Published online Oct 18, 2019. doi: 10.5312/wjo.v10.i10.364
Peer-review started: June 4, 2019
First decision: July 31, 2019
Revised: August 8, 2019
Accepted: September 15, 2019
Article in press: September 15, 2019
Published online: October 18, 2019
Posterior ankle impingement syndrome (PAIS) is a cause of ankle pain due to pinching of bony or soft tissue structures in the hindfoot. The diagnosis is primarily made based on detailed history and accurate clinical examination. The delay in its diagnosis has not yet been described in the pediatric and adolescent population.
To identify and characterize misdiagnosed cases of PAIS in pediatric and adolescent patients.
This descriptive prospective study at a tertiary children’s hospital included patients ≤ 18 years who underwent posterior ankle arthroscopy after presenting with chronic posterior ankle pain after being diagnosed with PAIS. Collected data included: Demographics, prior diagnoses and treatments, providers seen, time to diagnosis from presentation, and prior imaging obtained. Visual Analogue Scale (VAS) for pain and American Orthopedic Foot Ankle Society (AOFAS) ankle-hindfoot scores were noted at initial presentation and follow-up.
35 patients (46 ankles) with average age of 13 years had an average 19 mo (range 0-60 mo) delay in diagnosis from initial presentation. 25 (71%) patients had previously seen multiple medical providers and were given multiple other diagnoses. All 46 (100%) ankles had tenderness to palpation over the posterior ankle joint. Radiographs were reported normal in 31/42 (72%) exams. In 32 ankles who underwent MRI, the most common findings included os trigonum (47%)/Stieda process (47%). Conservative treatment had already been attempted in all patients. Ankle impingement pathology was confirmed during arthroscopy in 46 (100%) ankles. At an average follow-up of 13.1 mo, there was an improvement of VAS (pre-op 7.0 to post-op 1.2) and AOFAS scores (pre-op 65.1 to post-op 94).
This is the first study which shows that PAIS is a clinically misdiagnosed cause of posterior ankle pain in pediatric and adolescent population; an increased awareness about this diagnosis is needed amongst providers treating young patients.
Core tip: Our prospective study included 35 patients under 18 years of age diagnosed with posterior ankle impingement syndrome (PAIS) who underwent arthroscopic treatment for failed conservative management. We found that there was an average of 19 mo delay in diagnosis from initial presentation to a medical provider. All patients had posterior ankle tenderness which was used to make the clinical diagnosis. The pain relief with arthroscopic debridement, as evidenced by improvement of Visual Analogue Scale and American Orthopedic Foot Ankle Society scores was used to confirm our clinical diagnosis of PAIS. Our study shows that there needs to be an increased awareness about PAIS is needed amongst providers treating young patients.
- Citation: Kushare I, Kastan K, Allahabadi S. Posterior ankle impingement–an underdiagnosed cause of ankle pain in pediatric patients. World J Orthop 2019; 10(10): 364-370
- URL: https://www.wjgnet.com/2218-5836/full/v10/i10/364.htm
- DOI: https://dx.doi.org/10.5312/wjo.v10.i10.364
Posterior ankle impingement syndrome (PAIS) is a common cause of posterior ankle pain that has been classically described in ballet dancers and soccer players[1-4]. It is caused by mechanical pinching of bony or soft tissue structures during terminal plantar-flexion in the posterior part of the ankle[1-5]. Even though it can present acutely, PAIS more commonly presents with chronic pain secondary to repetitive stresses in the posterior ankle with forced plantar-flexion activities. With several causes (soft tissue, bony, or both) and heterogenous pathological anatomic features, the diagnosis was coined as posterior ankle impingement “syndrome”[2,6]. This diagnosis is primarily made based on an accurate history and detailed clinical exam[2,3,7-9]. To our knowledge, there has not been any prior literature that highlights the delay in making this diagnosis in the pediatric and adolescent population. The aim of our study was to identify any delay in diagnosis and further characterize the misdiagnosed cases of posterior ankle impingement exclusively in the pediatric and adolescent population.
This was a descriptive prospective study conducted at a tertiary children’s hospital after approval from the Institutional Review Board. The study included patients 18 years and younger from 2016 to 2019 who presented with posterior ankle pain, were diagnosed with posterior ankle impingement, and underwent arthroscopic debridement due to failure of conservative treatment. Informed written consent was obtained from all patients prior to enrollment in the study.
Collected data included the following: Age, gender, previous diagnoses and treatment received, prior specialists seen for ankle pain, time to diagnosis from initial presentation, and radiologic imaging obtained-including plain radiographs and magnetic resonance imaging (MRI). Diagnosis of PAIS was made based on history and clinical exam (posterior joint line tenderness, pain on forced plantar flexion) supplemented by radiographic imaging. Delay in diagnosis was defined as the time between initial presentation to a medical provider with ankle pain until the diagnosis of PAIS was made. Indication for arthroscopic debridement was failure of conservative treatment which included rest and immobilization, with or without physical therapy. Visual Analogue scale (VAS) for pain and American Orthopedic Foot Ankle Society (AOFAS) ankle-hindfoot scores at presentation pre-operatively and post-operative follow-up visits were compared using the paired t or Wilcoxon signed-rank tests with statistical significance set at P < 0.05. Descriptive statistical analyses were conducted and summarized as means with range values or frequencies with corresponding percentages.
Prospective data was collected in 35 patients (16 males, 19 females). A total of 46 ankles were included with a mean patient age of 13 years (range 8.6-17.9). 33 (94%) patients had a delay in the diagnosis of PAIS from the initial presentation with symptoms to a medical provider, the average delay being 19 mo (range 0-60). 22/35 (62%) patients were athletes, the most common sports included American football (4 patients), soccer and gymnastics (3 patients each). 25 (71%) patients had previously seen multiple health care professionals and specialists and were given multiple other diagnoses as a cause of their ankle pain (Table 1). All 46 (100%) ankles had specific tenderness to palpation over the posterior ankle joint which was located between the peroneal tendons and Achilles tendon. 42 (91%) ankles had at least one preoperative radiograph obtained (Figure 1), and 15 (43%) patients had multiple radiographs prior to actual diagnosis. The radiographs were reported “normal” with no significant findings by local radiologist in 31 (74%) exams. 30 (86%) patients (32 ankles) had an MRI study done, the most common findings of which were os trigonum (47%) (Figure 2) or Stieda process (47%). 22 of the 32 ankles (69%) with an MRI performed had osseous edema indicative of the inflammation seen in PAIS.
| Previous providers seen | Previous diagnoses given |
| Pediatricians | Sever’s apophysitis |
| Orthopedic surgeons | Peroneal tendon subluxation |
| Primary care sports physicians | Peroneal tendinopathy |
| Physical medicine and rehabilitation physicians | Achilles tendonitis |
| Podiatrists | Chronic regional pain syndrome |
| Physical therapists | Ankle sprain |
| Chiropractors | Sural neuralgia |
| Pain clinic | “Deconditioned ankle” |
All 35 (100%) patients had attempted and failed prolonged and exhaustive conservative management for several months. Conservative treatment included rest from sports and physical activities (including physical education at school), immobilization with boot, brace or cast, and/or physical therapy. One patient had a prior ankle corticosteroid injection. Pain typically subsided temporarily with conservative treatment but recurred with return to activity/sports. All 46 (100%) ankles had exquisite tenderness to palpation over posterior ankle joint, anterior to the Achilles tendon.
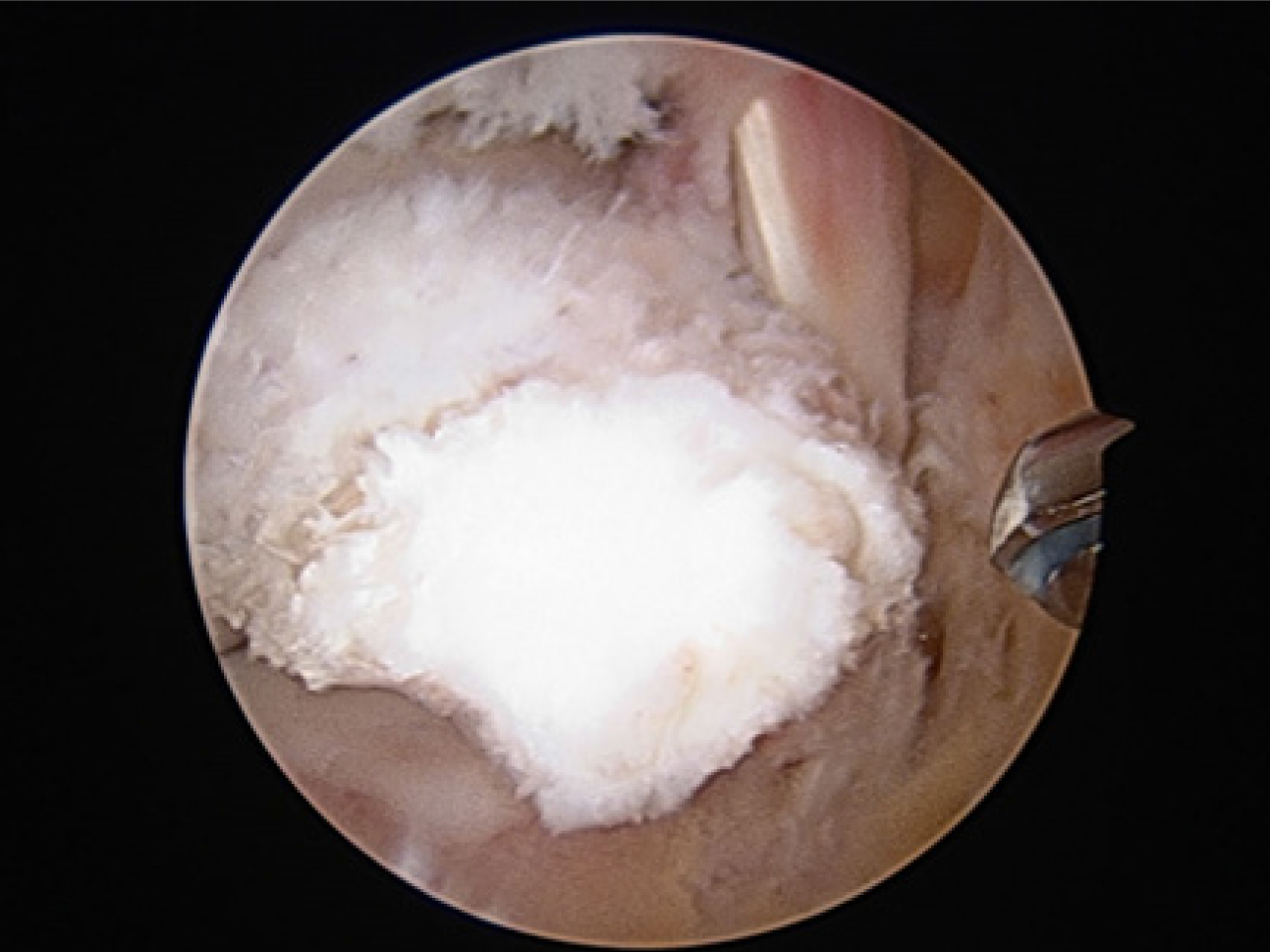
All 46 ankles had PAIS pathology, either soft tissue, bony, or a combination of both, confirmed during arthroscopic treatment, including os trigonum (Figure 3), Stieda process, hypertrophic ligaments and synovium–these three were the most common findings seen in majority (42/46) of the ankles. Uncommon findings were cysts of the flexor hallucis longus tendonitis (FHL) (2 cases), and a low-lying FHL muscle belly (2 cases). At an average follow-up of 13.1 mo, there was significant improvement of mean VAS pain scale (pre-op 7.0 to post-op 1.2, P < 0.001) and mean AOFAS ankle scores (pre-op 65.1 to post-op 94, P < 0.001). Three patients had inadequate documentation; the remaining 32 (91%) patients returned to their previous level of activity/sports at average 7.8 wk after treatment. None of the patients had recurrence of symptoms at their last follow-up which supports our diagnosis of PAIS.
Posterior ankle impingement syndrome has been well-described in the literature, particularly in dancers and soccer players[1,2,4]. PAIS is due to the mechanical pinching of structures in the posterior ankle, which may be secondary to bony or soft tissue causes, or a combination of both[1,2]. An average delay of over one and a half years (19 mo) from the time of initial symptomatic presentation to making the diagnosis in a high percentage (94%) of patients indicates that PAIS is usually not on the radar of physicians treating ankle pain in the pediatric and adolescent population.
The diagnosis of PAIS is primarily based on an accurate history and clinical examination[1-3]. The classic etiologic activities that have been described are dance (especially ballet), soccer, downhill running, and additional forced plantar-flexion activities[1-4]. The pain is aggravated by the aforementioned activities and is typically relieved by rest. The ankle pain is described as consistent, sharp, dull and deep; it is usually difficult for patients to indicate the exact location of the pain in the hindfoot[10,11]. On examination there is posterior joint line tenderness, and more specifically it is typically between the Achilles and peroneal tendons[2,4], which is important to help differentiate it from other causes of posterior foot and ankle pain such as Sever’s apophysitis and ankle sprain. The clinical exam finding of posterior joint line tenderness was seen in all of the ankles in our study; we suggest that this examination should be included in the evaluation of all patients presenting with ankle pain so that the diagnosis of posterior ankle impingement is not missed. A diagnostic local infiltration may also be performed to confirm the diagnosis, which can be guided by ultrasound[2].
History and clinical examination are most important in diagnosing PAIS and they can be supported by imaging findings. Standard lateral plain radiographs can identify bony pathology in the form of os trigonum (Figure 1) or Stieda process[12]. However, in young patients with open physes, os trigonum can very well be small or cartilaginous[4] and radiographs could often be reported as “normal”. Entrapment, hypertrophy and inflammation of soft tissues, FHL are common pathologies seen in posterior ankle impingement, but the fact that these are not well-visualized on radiographs can lead to delay in treatment and more expensive imaging[13]. Many of our patients had multiple radiographic imaging procedures performed of the painful ankle; and normal reported radiographs which likely contributed to the delayed diagnosis of PAIS. MRI is considered a useful diagnostic modality for assessment of the pathology in ankle impingement[6,14]. However, MRI has been shown to be an insensitive modality for ankle imaging in the pediatric population[15]. The most common MRI findings in our study included the presence of an os trigonum or Stieda process, with associated osseous and soft tissue edema which is similar to what prior studies in the literature have reported[6,12,14,16].
The most common treatment for posterior ankle impingement is conservative management which includes rest and immobilization of the ankle (with brace/boot/cast) to aid in decreasing the inflammation. This can be supplemented with physical therapy. Corticosteroid injections in the ankle have been described in literature, and are more typically used in athletes to help them complete a season[5]. Prolonged conservative treatment for several months was already attempted in all our patients, which lead to temporary pain relief but persisted/recurred with return to activity/sports. Persistent pain with activity despite conservative management was likely the reason why a high percentage (71%) of our patients saw multiple medical providers for treatment. Return of ankle pain with activity is commonly seen in ankle impingement as the pinching of structures in the hindfoot typically occurs with plantar flexion of the ankle causing recurrence of inflammation and pain[3,9,17,18].
The indication of arthroscopy in our patient population was persistent symptoms despite prolonged conservative management as mentioned above. Arthroscopic treatment is now an established modality of treatment for patients who fail conservative management[19-21]. Arthroscopic visualization of the ankle and hindfoot during surgery is also a reliable way to confirm the correct diagnosis[22]. Various pathologies which have already been well-described as sources of bony and/or soft tissue causes of posterior ankle impingement were encountered during arthroscopic treatment of our cohort, including os trigonum, Stieda process, hypertrophic ligaments and synovium, cysts of the FHL, and a low-lying FHL muscle belly[2,6,16,18,22-24]. The pain relief after treatment as indicated by improvement in VAS and AOFAS scores, along with return to prior level of sports and activity in our patient cohort supports the clinical diagnosis of posterior ankle impingement.
Weaknesses of our study include data collected at a single institution, small sample size, and no comparative non-operative cohort. The patients referred to a tertiary center like ours may not be representative of the whole population, and the referral could possibly increase the delay. The mean follow-up of 13.1 mo is relatively short; however, the focus of this study is on the delay in clinical diagnosis of PAIS, and not on the surgical outcomes. We have included the arthroscopic findings and treatment outcomes primarily to supplement our clinical diagnosis of PAIS. The strength of our study is the prospective nature of data collection and consecutive enrollment of pediatric patients, both of which help minimize biases that could result from a retrospective study. Collecting long-term multi-center data and including non-operatively treated patients for comparison are recommended for future studies. To conclude, posterior ankle impingement syndrome can be misdiagnosed in young patients presenting with posterior ankle pain, thus leading to a delay in diagnosis. This prospective study in the pediatric population is the first study which highlights the need for increased awareness about this condition and its clinical diagnosis amongst pediatric orthopedic surgeons, pediatricians, primary care sports doctors, and other physicians involved in treating young athletes to avoid delay in treatment.
Posterior ankle impingement is a known cause of ankle pain which has been well described in adults but not as much in the pediatric literature.
The diagnosis of posterior ankle impingement syndrome (PAIS) is made based on detailed history and clinical findings. We came across patients with missed diagnosis of PAIS in clinic and realized that without adequate awareness, this diagnosis can possibly be missed in pediatric and adolescent patients.
The purpose of our study was to identify and characterize the delay in making the diagnosis of PAIS in the young patient population.
We started a prospective study to enroll patients under 18 years of age who were diagnosed with PAIS and underwent arthroscopic treatment after failed conservative management. Data collection was done to try and identify any delay in making this diagnosis by the previous treating medical providers. Pre and post treatment pain and American Orthopedic Foot Ankle Society (AOFAS) scores were also noted and compared.
35 patients (46 ankles) with average age of 13 years had an average 19 mo (range 0-60 mo) delay in diagnosis from initial presentation to a medical provider. 25 (71%) patients had previously seen multiple medical providers. All 46 (100%) ankles had tenderness to palpation over the posterior ankle joint. Radiographs were reported normal in 31/42 (72%) exams. In 32 ankles who underwent MRI, the most common findings included os trigonum (47%)/Stieda process (47%). At an average follow-up of 13.1 mo after treatment, there was significant improvement of VAS (pre-op 7.0 to post-op 1.2) and AOFAS scores (pre-op 65.1 to post-op 93.4) (P < 0.001).
The study concludes that PAIS is a misdiagnosed condition in the pediatric population.
It was shown that a variety of medical providers (pediatricians, orthopedic surgeons, sports physicians, etc.) missed this diagnosis. There needs to be increased awareness about this condition among medical providers treating young patients.
The study makes us aware about the delayed diagnosis if PAIS which can be prevented by detailed history taking and examination. This research can be potentially improved in the future by collecting multi-center data to include larger cohort of patients.
Manuscript source: Unsolicited manuscript
Specialty type: Orthopedics
Country of origin: United States
Peer-review report classification
Grade A (Excellent): 0
Grade B (Very good): B
Grade C (Good): 0
Grade D (Fair): D
Grade E (Poor): 0
P-Reviewer: Doets HC, van Bergen CJA S-Editor: Wang J L-Editor: A E-Editor: Liu MY
| 1. | Russell JA, Kruse DW, Koutedakis Y, McEwan IM, Wyon MA. Pathoanatomy of posterior ankle impingement in ballet dancers. Clin Anat. 2010;23:613-621. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 45] [Article Influence: 3.2] [Reference Citation Analysis (0)] |
| 2. | Giannini S, Buda R, Mosca M, Parma A, Di Caprio F. Posterior ankle impingement. Foot Ankle Int. 2013;34:459-465. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 40] [Cited by in F6Publishing: 41] [Article Influence: 3.7] [Reference Citation Analysis (0)] |
| 3. | Roche AJ, Calder JD, Lloyd Williams R. Posterior ankle impingement in dancers and athletes. Foot Ankle Clin. 2013;18:301-318. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 19] [Cited by in F6Publishing: 22] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 4. | Nault ML, Kocher MS, Micheli LJ. Os trigonum syndrome. J Am Acad Orthop Surg. 2014;22:545-553. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 50] [Cited by in F6Publishing: 39] [Article Influence: 3.9] [Reference Citation Analysis (0)] |
| 5. | Kudaş G, Dönmez MS, Işık Ç, Çelebi M, Çay N, Bozkurt M. Posterior ankle impingement syndrome in football players: Case series of 26 elite athletes. Acta Orthopaedica et Traumatologica Turcica. 2016;50:649-654. [DOI] [Cited in This Article: ] [Cited by in Crossref: 14] [Cited by in F6Publishing: 13] [Article Influence: 1.6] [Reference Citation Analysis (0)] |
| 6. | Peace KA, Hillier JC, Hulme A, Healy JC. MRI features of posterior ankle impingement syndrome in ballet dancers: a review of 25 cases. Clin Radiol. 2004;59:1025-1033. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 109] [Cited by in F6Publishing: 67] [Article Influence: 3.4] [Reference Citation Analysis (0)] |
| 7. | Maquirriain J. Posterior ankle impingement syndrome. J Am Acad Orthop Surg. 2005;13:365-371. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 82] [Cited by in F6Publishing: 81] [Article Influence: 4.3] [Reference Citation Analysis (0)] |
| 8. | Smyth NA, Zwiers R, Wiegerinck JI, Hannon CP, Murawski CD, van Dijk CN, Kennedy JG. Posterior hindfoot arthroscopy: a review. Am J Sports Med. 2014;42:225-234. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 63] [Cited by in F6Publishing: 65] [Article Influence: 6.5] [Reference Citation Analysis (0)] |
| 9. | Bojanić I, Janjić T, Dimnjaković D, Križan S, Smoljanović T. [Posterior ankle impingement syndrome]. Lijec Vjesn. 2015;137:109-115. [PubMed] [Cited in This Article: ] |
| 10. | Yasui Y, Hannon CP, Hurley E, Kennedy JG. Posterior ankle impingement syndrome: A systematic four-stage approach. World J Orthop. 2016;7:657-663. [PubMed] [DOI] [Cited in This Article: ] [Cited by in CrossRef: 25] [Cited by in F6Publishing: 21] [Article Influence: 2.6] [Reference Citation Analysis (1)] |
| 11. | Coetzee JC, Seybold JD, Moser BR, Stone RM. Management of Posterior Impingement in the Ankle in Athletes and Dancers. Foot Ankle Int. 2015;36:988-994. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 17] [Article Influence: 1.9] [Reference Citation Analysis (0)] |
| 12. | Al-Riyami AM, Tan HK, Peh WCG. Imaging of Ankle Impingement Syndromes. Can Assoc Radiol J. 2017;68:431-437. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 4] [Cited by in F6Publishing: 4] [Article Influence: 0.6] [Reference Citation Analysis (0)] |
| 13. | Wiegerinck JI, Vroemen JC, van Dongen TH, Sierevelt IN, Maas M, van Dijk CN. The posterior impingement view: an alternative conventional projection to detect bony posterior ankle impingement. Arthroscopy. 2014;30:1311-1316. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 20] [Cited by in F6Publishing: 21] [Article Influence: 2.1] [Reference Citation Analysis (0)] |
| 14. | Wong, GNL, Tan TJ. MR imaging as a problem solving tool in posterior ankle pain: A review. Eur J Radiol. 2016;85:2238-2256. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 16] [Cited by in F6Publishing: 16] [Article Influence: 2.0] [Reference Citation Analysis (0)] |
| 15. | Vasukutty NV, Akrawi H, Theruvil B, Uglow M. Ankle arthroscopy in children. Ann R Coll Surg Engl. 2011;93:232-235. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 9] [Cited by in F6Publishing: 9] [Article Influence: 0.7] [Reference Citation Analysis (0)] |
| 16. | Sellon E, Robinson P. MR Imaging of Impingement and Entrapment Syndromes of the Foot and Ankle. Magn Reson Imaging Clin N Am. 2017;25:145-158. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 8] [Cited by in F6Publishing: 8] [Article Influence: 1.1] [Reference Citation Analysis (0)] |
| 17. | Luk P, Thordarson D, Charlton T. Evaluation and management of posterior ankle pain in dancers. J Dance Med Sci. 2013;17:79-83. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 23] [Cited by in F6Publishing: 24] [Article Influence: 2.2] [Reference Citation Analysis (0)] |
| 18. | Hayashi D, Roemer FW, D'Hooghe P, Guermazi A. Posterior ankle impingement in athletes: Pathogenesis, imaging features and differential diagnoses. Eur J Radiol. 2015;84:2231-2241. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 28] [Article Influence: 3.1] [Reference Citation Analysis (0)] |
| 19. | Carreira DS, Vora AM, Hearne KL, Kozy J. Outcome of Arthroscopic Treatment of Posterior Impingement of the Ankle. Foot Ankle Int. 2016;37:394-400. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 23] [Article Influence: 2.9] [Reference Citation Analysis (0)] |
| 20. | Theodoulou MH, Bohman L. Arthroscopic Approach to Posterior Ankle Impingement. Clin Podiatr Med Surg. 2016;33:531-543. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 3] [Cited by in F6Publishing: 3] [Article Influence: 0.4] [Reference Citation Analysis (0)] |
| 21. | Miyamoto W, Miki S, Kawano H, Takao M. Surgical outcome of posterior ankle impingement syndrome with concomitant ankle disorders treated simultaneously in patient engaged in athletic activity. J Orthop Sci. 2017;22:463-467. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 11] [Cited by in F6Publishing: 12] [Article Influence: 1.7] [Reference Citation Analysis (0)] |
| 22. | Miyamoto W, Takao M, Matsushita T. Hindfoot endoscopy for posterior ankle impingement syndrome and flexor hallucis longus tendon disorders. Foot Ankle Clin. 2015;20:139-147. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 21] [Cited by in F6Publishing: 22] [Article Influence: 2.4] [Reference Citation Analysis (0)] |
| 23. | Hopper MA, Robinson P. Ankle impingement syndromes. Radiol Clin North Am. 2008;46:957-971, v. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 39] [Cited by in F6Publishing: 39] [Article Influence: 2.6] [Reference Citation Analysis (0)] |
| 24. | Rungprai C, Tennant JN, Phisitkul P. Disorders of the Flexor Hallucis Longus and Os Trigonum. Clin Sports Med. 2015;34:741-759. [PubMed] [DOI] [Cited in This Article: ] [Cited by in Crossref: 26] [Cited by in F6Publishing: 26] [Article Influence: 2.9] [Reference Citation Analysis (0)] |