Impact of age and comorbidity on survival in colorectal cancer
Introduction
Colorectal cancer is the third most occurring malignancy in the Netherlands with over 13,000 new cases in 2012. Seventy percent of these patients are above the age of 65 years, and 21% is even older than 80 years of age (1). Despite the high prevalence of colorectal cancer in the elderly population, the inclusion of this cohort in clinical trials is disproportionately low. In addition, inclusion is limited to patients with little comorbidity and a high performance score (2-4). Hence, it is questionable whether the evidence for treatment of colorectal cancer is valid in a large percentage of patients. As such, Dutch guidelines recommend individualised treatment and emphasize shared decision making in elderly patients with comorbidity (5).
A number of studies have been performed analysing the influence of age and comorbidity on outcomes as well as decisions by clinicians whether to treat patients with chemotherapy in adjuvant or palliative setting. A number of observational studies show survival benefit of chemotherapy treatment in elderly patients (6-9). Survival and the survival benefit of treatment are reduced with increasing age and comorbidity (10,11). Also, the percentage of patients treated with chemotherapy is inversely correlated with age and comorbidity (12).
Due to their retrospective nature, and the fact that standard treatment is withheld in a large portion of elderly patients based on their comorbidity and performance score, studies examining the relation between comorbidity and treatment efficacy suffer from selection bias. The present cross-sectional single centre study examines the effect of age and comorbidity on survival. In addition, cause of death was evaluated as colorectal cancer patients do not die exclusively because of cancer.
Methods
All consecutive patients diagnosed and treated for colorectal cancer within a specific timeframe [2002-2008] in the Zaans Medisch Centrum, the community hospital of the Zaanstreek region in the Netherlands, were included. An extensive chart review was performed for all these patients. Via detailed patient information transparency was increased, and bias in the assessment of the effect of comorbidity on outcomes could be minimised.
Evaluation was done on 1-1-2014. The review consisted of an examination of patient charts with medical history, pathology, radiology, and endoscopy reports as well as data from the department of pharmacy (13).
The well-known Charlson comorbidity score was used to estimate comorbidity. The diagnosis of colorectal cancer was excluded in the calculation of the Charlson index (14-16).
Overall survival was measured from date of diagnosis till date of death. The TNM7 classification was used to assess disease stage (17). A detailed description of all variables and exclusions are noted in the appendices.
Kaplan Meier curves for overall survival were calculated, separate for both age, categorized into four equally sized groups, and Charlson index, divided into three categories: 0 [1], 1-2 [2], and 3+ [3]. Uni- and multivariate cox regression analysis was used to assess hazard ratios (HR) of survival for age, comorbidity score and tumour characteristics. Poisson regression was used to determine the risk ratio (RR) of dying due to tumour progression relative to death from other causes. Separate analyses were performed for patients with rectal and colon cancer.
Statistical analyses were performed using IBM SPSS statistics software version 20.0 and Microsoft Office Excel 2010.
The study was approved by the ethical committee of the Zaans Medisch Centrum.
Results
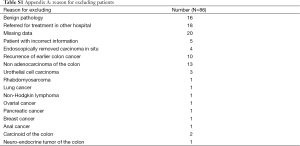
Six hundred twenty-one patients were diagnosed with colorectal cancer between 1-1-2002 and 31-12-2008. Eighty-six patients were excluded for various reasons. See Tables S1 and S2 for detailed descriptions of these exclusions. These patients were referred to a nearby University Hospital for treatment on their own requests. Follow-up data of all patients were present for a minimum of 5 years and a maximum of 13 years, depending on the year of inclusion, or until death.
Full table

Full table
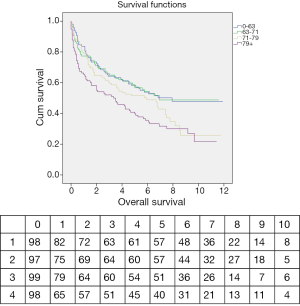
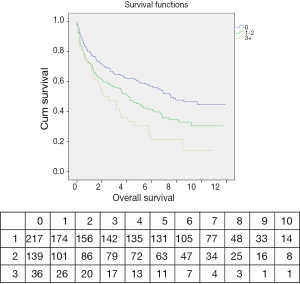
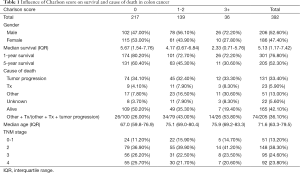
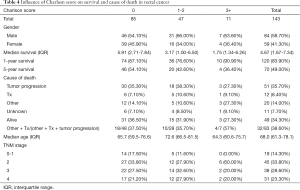
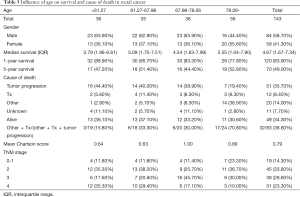
Colon
Three hundred ninety-two patients were diagnosed with colon cancer. Median follow-up was 5.13 years, interquartile range (IQR) 1.17-7.42. One hundred sixty-five patients (42.1%) were alive at the end of follow-up. One hundred thirty-one patients (33.4%) died from tumour progression, 23 patients (5.9%) experienced treatment related adverse events with fatal outcome and 51 patients (13.0%) died from other causes. Median age at diagnosis was 71.6 years, IQR 63.3-79.5. Mean Charlson index was 0.82, range 0-7 (Tables 1,2).
Full table
Full table
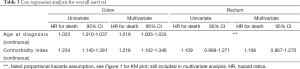
Age at the time of diagnosis and Charlson comorbidity index were significant predictors of survival in uni- and multivariate cox regression analysis (P<0.05). Hazard ratio (HR) of death in multivariate analysis for age was 1.019 per year increase. For comorbidity the HR was 1.218 per point increase on Charlson score (Table 3, Figures 2,3).
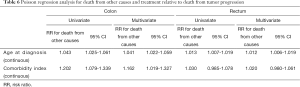
Full table
Age and comorbidity index were also significant predictors of death from causes other than tumour progression in multivariate analysis. RR for death from other causes was 1.041 per year of age. The RR increased 1.162 per point increase in Charlson score (Tables 4,5).
Full table
Full table
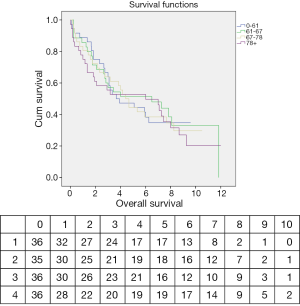
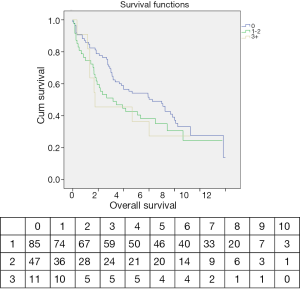
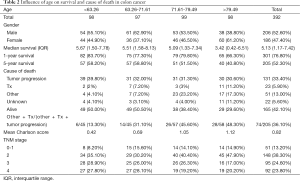
Rectum
One hundred forty-three patients were diagnosed with rectal cancer. Median follow-up was 4.51 years, IQR 1.67-7.26. Forty-nine patients (34.3%) were alive at the end of follow-up. Fifty-one patients (35.7%) died from tumour progression, 12 patients (8.4%) experienced treatment related adverse events with a fatal outcome, and 20 patients (14.0%) died from other causes. Median age at diagnosis was 68.0, IQR 61.3-78.1. Mean Charlson index was 0.79, range 0-8 (Tables 4,5).
There was a trend towards increased risk of death per point increase in comorbidity score, HR 1.108 (95% CI, 0.967-1.270). HR’s determined for age at diagnosis was not valid as the proportional hazards assumption was not met. This is most likely due to a small effect size (Figures 1,4, Table 3).
Age at diagnosis was a significant predictor of cause of death in multivariate analysis with a RR of 1.012 per year of age to die from causes other than tumour progression. The comorbidity index was not a significant predictor of cause of death (Table 6).
Full table
Discussion
This study deals with the impact of age and comorbidity on overall survival and cause of death in patients diagnosed with colorectal cancer in normal daily practice.
Eighteen patients were referred to a tertiary centre for treatment mostly at their own request. A possible limitation of the present study is the relatively small sample size when comparing it to others in its field using large patient registries. However, the strength of the present study is the introduction of cause of death in the analysis.
This study has a long follow-up period, with (near) perfect follow-up for the first 5 years. In addition, since all consecutive patients were included, this study accurately represents the population of colorectal cancer patients in a developed country in normal daily practice. Furthermore, patient and tumour characteristics are extensively documented. To our knowledge this is the first study to include causes of death, tumour characteristics and a comorbidity measure in a study of colorectal cancer survival.
In colon cancer patients, age and comorbidity are predictors of survival. This solidifies the notion that despite the morbidity and mortality associated with a colon cancer diagnosis; baseline patient characteristics still largely predict a patient’s primary outcome. This underlines the need to treat patients holistically.
Age is also significantly associated with cause of death, with a difference of 35% (48% vs. 13%) in ratio between death from tumour progression and other causes. This is primarily caused by an increase in death from other causes as the percentage of patients dying due to tumour progression remains constant. However, one should take into account that with increasing age, overall survival, and thus follow-up, decreases, as does the intensity of cancer treatment (18,19). This has also been observed for adjuvant therapy in this cohort (13).
The observation that cancer related mortality does not decrease with increasing age exemplifies the idea that, although elderly patients have a shorter life expectancy based on their age and pre-existent conditions, they do still benefit from cancer treatment. However, this survival benefit is hard to quantify. The present study does not take associated morbidity and quality of life into account. Therefore a shared decision making model when treating elderly patients with colon cancer is advocated.
In this study, rectal cancer patients’ age and comorbidity did not significantly influence survival or the cause of death. The explanation could be that cancer related mortality in this cohort was very high, implicating that all patients should be treated according to standard guidelines irrespective of age or pre-existent conditions.
However, the validity of these findings is questionable. First off, the findings do not correspond with previous large cohort studies that did find an inverse relationship between age and comorbidity, and survival (20,21). The tumour related mortality in our rectal cancer is almost identical to that of colon cancer in our cohort [33.4% (colon) vs. 35.7% (rectum)]. The median survival of 4.67 years of rectum cancer patients is also similar to that of the colon cancer patients in this cohort and corresponds with the 5 years survival rate of approximately 50% observed in the study by Ostenfeld et al. in the same time period (11).
Thus, one could conclude that the non-significant effect of the Charlson score on survival likely represents a small sample size and a type 2 error as the Charlson score has been validated to predict overall survival in many much larger cohorts (22,23), and, as just established, it is unlikely that the effect of comorbidity is negated by a higher cancer related mortality in this cohort.
In conclusion, age and comorbidity are significant predictors of overall survival, reflecting the importance of optimizing patients beyond their cancer treatment, and cause of death. This represents possible treatment bias and a reduced survival benefit of treatment with increasing age. In rectal cancer patients neither comorbidity nor age was a predictor of overall survival. This could be explained if rectal cancer was the prognosis defining illness in the majority of cases, however this is contradicted by the observed median survival and the percentage of cancer related deaths. As such, the validity of these outcomes can be questioned.
We recommend further study of the benefit of cancer treatment in the elderly, and advocate inclusion of this patient group in clinical trials.
Acknowledgements
None.
Footnote
Conflicts of Interest: The authors have no conflicts of interest to declare.
References
- Integraal kanker centrum Nederland, 2014. Accessed December, 2014. Available online: www.cijfersoverkanker.nl
- Townsley CA, Selby R, Siu LL. Systematic review of barriers to the recruitment of older patients with cancer onto clinical trials. J Clin Oncol 2005;23:3112-24. [PubMed]
- Trimble EL, Carter CL, Cain D, et al. Representation of older patients in cancer treatment trials. Cancer 1994;74:2208-14. [PubMed]
- Murthy VH, Krumholz HM, Gross CP. Participation in cancer clinical trials: race-, sex-, and age-based disparities. JAMA 2004;291:2720-6. [PubMed]
- Dutch guideline for the diagnosis and treatment of colorectal cancer, 2014. Accessed December, 2014. Available online: www.oncoline.org
- van Steenbergen LN, Lemmens VE, Rutten HJ, et al. Increased adjuvant treatment and improved survival in elderly stage III colon cancer patients in The Netherlands. Ann Oncol 2012;23:2805-11. [PubMed]
- Wildes TM, Kallogjeri D, Powers B, et al. The Benefit of Adjuvant Chemotherapy in Elderly Patients with Stage III Colorectal Cancer is Independent of Age and Comorbidity. J Geriatr Oncol 2010;1:48-56. [PubMed]
- Abraham A, Habermann EB, Rothenberger DA, et al. Adjuvant chemotherapy for stage III colon cancer in the oldest old: results beyond clinical guidelines. Cancer 2013;119:395-403. [PubMed]
- Venderbosch S, Doornebal J, Teerenstra S, et al. Outcome of first line systemic treatment in elderly compared to younger patients with metastatic colorectal cancer: a retrospective analysis of the CAIRO and CAIRO2 studies of the Dutch Colorectal Cancer Group (DCCG). Acta Oncol 2012;51:831-9. [PubMed]
- Tong L, Ahn C, Symanski E, et al. Effects of newly developed chemotherapy regimens, comorbidities, chemotherapy-related toxicities on the changing patterns of the leading causes of death in elderly patients with colorectal cancer. Ann Oncol 2014;25:1234-42. [PubMed]
- Ostenfeld EB, Nørgaard M, Thomsen RW, et al. Comorbidity and survival of Danish patients with colon and rectal cancer from 2000-2011: a population-based cohort study. Clin Epidemiol 2013;5:65-74. [PubMed]
- Kahn KL, Adams JL, Weeks JC, et al. Adjuvant chemotherapy use and adverse events among older patients with stage III colon cancer. JAMA 2010;303:1037-45. [PubMed]
- van Eeghen E, Bakker S, van Bochove A, et al. High risk stage 2 and stage 3 colon cancer, predictors of recurrence and effect of adjuvant therapy in a non-selected population. Int Sch Res Notices 2015;2015:790186-95.
- Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987;40:373-83. [PubMed]
- Ouellette JR, Small DG, Termuhlen PM. Evaluation of Charlson-Age Comorbidity Index as predictor of morbidity and mortality in patients with colorectal carcinoma. J Gastrointest Surg 2004;8:1061-7. [PubMed]
- Marventano S, Grosso G, Mistretta A, et al. Evaluation of four comorbidity indices and Charlson comorbidity index adjustment for colorectal cancer patients. Int J Colorectal Dis 2014;29:1159-69. [PubMed]
- Edge SB, Compton CC. The American Joint Committee on Cancer: the 7th edition of the AJCC cancer staging manual and the future of TNM. Ann Surg Oncol 2010;17:1471-4.
- Sanoff HK, Carpenter WR, Stürmer T, et al. Effect of adjuvant chemotherapy on survival of patients with stage III colon cancer diagnosed after age 75 years. J Clin Oncol 2012;30:2624-34. [PubMed]
- Doat S, Thiébaut A, Samson S, et al. Elderly patients with colorectal cancer: treatment modalities and survival in France. National data from the ThInDiT cohort study. Eur J Cancer 2014;50:1276-83. [PubMed]
- Shack LG, Shah A, Lambert PC, et al. Cure by age and stage at diagnosis for colorectal cancer patients in North West England, 1997-2004: a population-based study. Cancer Epidemiol 2012;36:548-53. [PubMed]
- Steele SR, Park GE, Johnson EK, et al. The impact of age on colorectal cancer incidence, treatment, and outcomes in an equal-access health care system. Dis Colon Rectum 2014;57:303-10. [PubMed]
- Frenkel WJ, Jongerius EJ, Mandjes-van Uitert MJ, et al. Validation of the Charlson Comorbidity Index in acutely hospitalized elderly adults: a prospective cohort study. J Am Geriatr Soc 2014;62:342-6. [PubMed]
- Hall WH, Ramachandran R, Narayan S, et al. An electronic application for rapidly calculating Charlson comorbidity score. BMC Cancer 2004;4:94. [PubMed]