Acupuncture as Add-On Treatment of the Positive, Negative, and Cognitive Symptoms of Patients with Schizophrenia: A Systematic Review
Abstract
:1. Introduction
2. Materials and Methods
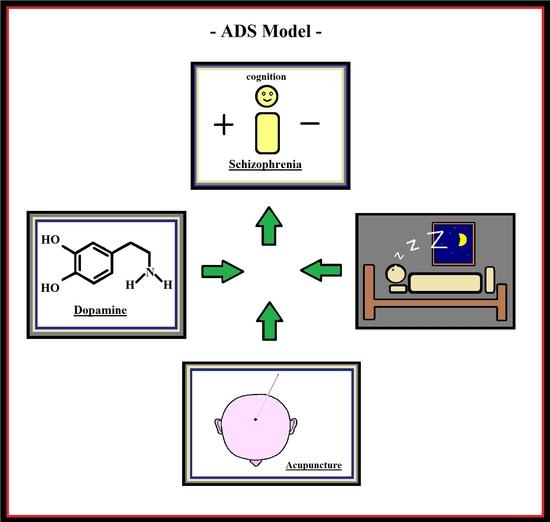
2.1. Search Strategies
2.2. Study Selection and Data extraction
3. Results
3.1. Safety Issue
3.2. Positive and Negative Symptoms
3.3. Cognitive Symptoms
3.4. Sleep Disorders
4. Discussion
5. Conclusions
Acknowledgments
Author Contributions
Conflicts of Interest
References
- Van Os, J.; Kapur, S. Schizophrenia. Lancet 2009, 374, 635–645. [Google Scholar] [CrossRef]
- Iacono, W.G.; Beiser, M. Are males more likely than females to develop schizophrenia? Am. J. Psychiatry 1992, 149, 1070–1074. [Google Scholar] [PubMed]
- McGrath, J.; Saha, S.; Welham, J.; El Saadi, O.; MacCauley, C.; Chant, D. A systematic review of the incidence of schizophrenia: The distribution of rates and the influence of sex, urbanicity, migrant status and methodology. BMC Med. 2004, 2, 13. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Picchioni, M.M.; Murray, R.M. Schizophrenia. BMJ 2007, 335, 91–95. [Google Scholar] [CrossRef] [PubMed]
- Castle, D.; Wessely, S.; Der, G.; Murray, R.M. The incidence of operationally defined schizophrenia in Camberwell, 1965–1984. Br. J. Psychiatry 1991, 159, 790–794. [Google Scholar] [CrossRef] [PubMed]
- Kelly, B.D.; O’Callaghan, E.; Waddington, J.L.; Feeney, L.; Browne, S.; Scully, P.J.; Clarke, M.; Quinn, J.F.; McTigue, O.; Morgan, M.G.; et al. Schizophrenia and the city: A review of literature and prospective study of psychosis and urbanicity in Ireland. Schizophr. Res. 2010, 116, 75–89. [Google Scholar] [CrossRef] [PubMed]
- Carbon, M.; Correll, C.U. Thinking and acting beyond the positive: The role of the cognitive and negative symptoms in schizophrenia. CNS Spectr. 2014, 19, 38–52. [Google Scholar] [CrossRef] [PubMed]
- Teeple, R.C.; Caplan, J.P.; Stern, T.A. Visual hallucinations: Differential diagnosis and treatment. Prim. Care Companion J. Clin. Psychiatry 2009, 11, 26–32. [Google Scholar] [CrossRef] [PubMed]
- Foussias, G.; Remington, G. Negative symptoms in schizophrenia: Avolition and Occam’s razor. Schizophr. Bull. 2010, 36, 359–369. [Google Scholar] [CrossRef] [PubMed]
- Orellana, G.; Slachevsky, A. Executive functioning in schizophrenia. Front. Psychiatry 2013, 4, 35. [Google Scholar] [CrossRef] [PubMed]
- Gruber, O.; Chadha Santuccione, A.; Aach, H. Magnetic resonance imaging in studying schizophrenia, negative symptoms, and the glutamate system. Front. Psychiatry 2014, 5, 32. [Google Scholar] [CrossRef] [PubMed]
- De Hert, M.; McKenzie, K.; Peuskens, J. Risk factors for suicide in young people suffering from schizophrenia: A long-term follow-up study. Schizophr. Res. 2001, 47, 127–134. [Google Scholar] [CrossRef]
- Kane, J.M.; Correll, C.U. Pharmacologic treatment of schizophrenia. Dialogues Clin. Neurosci. 2010, 12, 345–357. [Google Scholar] [CrossRef]
- Jaffe, A.B.; Levine, J. Efficacy and effectiveness of first- and second-generation antipsychotics in schizophrenia. J. Clin. Psychiatry 2003, 64, 3–6. [Google Scholar] [PubMed]
- Smith, M.; Hopkins, D.; Peveler, R.C.; Holt, R.I.; Woodward, M.; Ismail, K. First- v. second-generation antipsychotics and risk for diabetes in schizophrenia: Systematic review and meta-analysis. Br. J. Psychiatry 2008, 192, 406–411. [Google Scholar] [CrossRef] [PubMed]
- Miller, D.D.; Caroff, S.N.; Davis, S.M.; Rosenheck, R.A.; McEvoy, J.P.; Saltz, B.L.; Riggio, S.; Chakos, M.H.; Swartz, M.S.; Keefe, R.S.; et al. Extrapyramidal side-effects of antipsychotics in a randomised trial. Br. J. Psychiatry 2008, 193, 279–288. [Google Scholar] [CrossRef] [PubMed]
- Correll, C.U.; Schenk, E.M. Tardive dyskinesia and new antipsychotics. Curr. Opin. Psychiatry 2008, 21, 151–156. [Google Scholar] [CrossRef] [PubMed]
- Krebs, M.; Leopold, K.; Hinzpeter, A.; Schaefer, M. Current schizophrenia drugs: Efficacy and side effects. Expert Opin. Pharmacother. 2006, 7, 1005–1016. [Google Scholar] [CrossRef] [PubMed]
- Lieberman, J.A. Metabolic changes associated with antipsychotic use. Prim. Care Companion J. Clin. Psychiatry 2004, 6, 8–13. [Google Scholar] [PubMed]
- Kemmler, G.; Hummer, M.; Widschwendter, C.; Fleischhacker, W.W. Dropout rates in placebo-controlled and active-control clinical trials of antipsychotic drugs: A meta-analysis. Arch. Gen. Psychiatry 2005, 62, 1305–1312. [Google Scholar] [CrossRef] [PubMed]
- Zhang, J.P.; Malhotra, A.K. Pharmacogenetics and antipsychotics: Therapeutic efficacy and side effects prediction. Expert Opin. Drug Metab. Toxicol. 2011, 7, 9–37. [Google Scholar] [CrossRef] [PubMed]
- Dickerson, F.B.; Lehman, A.F. Evidence-based psychotherapy for schizophrenia. J. Nerv. Ment. Dis. 2006, 194, 3–9. [Google Scholar] [CrossRef] [PubMed]
- Kopelowicz, A.; Liberman, R.P.; Zarate, R. Recent advances in social skills training for schizophrenia. Schizophr. Bull. 2006, 32, 12–23. [Google Scholar] [CrossRef] [PubMed]
- Waite, F.; Myers, E.; Harvey, A.G.; Espie, C.A.; Startup, H.; Sheaves, B.; Freeman, D. Treating sleep problems in patients with schizophrenia. Behav. Cogn. Psychother. 2016, 44, 273–287. [Google Scholar] [CrossRef] [PubMed]
- Caqueo-Urízar, A.; Rus-Calafell, M.; Urzúa, A.; Escudero, J.; Gutiérrez-Maldonado, J. The role of family therapy in the management of schizophrenia: Challenges and solutions. Neuropsychiatr. Dis. Treat. 2015, 11, 145–151. [Google Scholar] [PubMed]
- Twamley, E.W.; Jeste, D.V.; Lehman, A.F. Vocational rehabilitation in schizophrenia and other psychotic disorders: A literature review and meta-analysis of randomized controlled trials. J. Nerv. Ment. Dis. 2003, 191, 515–523. [Google Scholar] [CrossRef] [PubMed]
- Dey, T. Soothing the Troubled Mind: Acupuncture and Moxibustion in the Treatment and Prevention of Schizophrenia; Paradigm: Brookline, MA, USA, 1999; pp. 1–168. ISBN 13-978-0912111605. [Google Scholar]
- Moher, D.; Liberati, A.; Tetzlaff, J.; Altman, D.G.; The PRISMA Group. Preferred reporting items for systematic reviews and meta-analyses: The PRISMA statement. BMJ 2009, 339, eb2535. [Google Scholar] [CrossRef] [PubMed]
- Cheng, J.; Wang, G.; Xiao, L.; Wang, H.; Wang, X.; Li, C. Electro-acupuncture versus sham electro-acupuncture for auditory hallucinations in patients with schizophrenia: A randomized controlled trial. Clin. Rehabil. 2009, 23, 579–588. [Google Scholar] [CrossRef] [PubMed]
- Zhang, B. A controlled study of clinical therapeutic effects of laser acupuncture for schizophrenia. Zhonghua Shen Jing Jing Shen Ke Za Zhi 1991, 24, 81–83. [Google Scholar] [PubMed]
- Ching, H.Y.; Wu, S.L.; Chen, W.C.; Hsieh, C.L. Effects of auricular acupressure on body weight parameters in patients with chronic schizophrenia. Evid. Based Complement. Altern. Med. 2012, 2012, 151737. [Google Scholar] [CrossRef] [PubMed]
- Bosch, P.; van Luijtelaar, G.; van den Noort, M.; Lim, S.; Egger, J.; Coenen, A. Sleep ameliorating effects of acupuncture in a psychiatric population. Evid. Based Complement. Altern. Med. 2013, 2013, 969032. [Google Scholar] [CrossRef] [PubMed]
- Bosch, P.; van den Noort, M.; Yeo, S.; Lim, S.; Coenen, A.; van Luijtelaar, G. The effect of acupuncture on mood and working memory in patients with depression and schizophrenia. J. Integr. Med. 2015, 13, 380–390. [Google Scholar] [CrossRef]
- Bouhlel, S.; El-Hechmi, S.; Ghanmi, L.; Ghaouar, M.; Besbes, C.; Khaled, M.; Melki, W.; El-Hechmi, Z. Effectiveness of acupuncture in treating schizophrenia: A clinical randomized trial of 31 patients. Tunis Med. 2011, 89, 774–778. [Google Scholar] [PubMed]
- Huang, Y.; Zheng, Y. Sleep disorder of schizophrenia treated with shallow needling: A randomized controlled trial. Zhongguo Zhen Jiu 2015, 35, 869–873. [Google Scholar] [PubMed]
- Xu, T.C.; Su, J.; Wang, W.N. Effect of three-step acupuncture combined with small dosage antipsychotic in treating incipient schizophrenia. Zhongguo Zhong Xi Yi Jie He Za Zhi 2010, 30, 1138–1141. [Google Scholar] [PubMed]
- Bosch, P.; de Rover, P.; Staudte, H.; Lim, S.; van den Noort, M. Schizophrenia, depression, and sleep disorders: Their traditional Oriental medicine equivalents. J. Acupunct. Meridian Stud. 2015, 8, 17–22. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Bosch, P.; van den Noort, M.; Staudte, H.; Lim, S.; Yeo, S.; Coenen, A.; van Luijtelaar, G. Sleep disorders in patients with depression or schizophrenia: A randomized controlled trial using acupuncture treatment. Eur. J. Integr. Med. 2016, 8, 789–796. [Google Scholar] [CrossRef]
- Shi, Z.X.; Tan, M.Z. An analysis of the therapeutic effect of acupuncture treatment in 500 cases of schizophrenia. J. Tradit. Chin. Med. 1986, 6, 99–104. [Google Scholar] [PubMed]
- Zhang, M.J. Treatment of 296 cases of hallucination with scalp-acupuncture. J. Tradit. Chin. Med. 1988, 8, 193–194. [Google Scholar] [PubMed]
- Shi, Z.X. Observation on the therapeutic effect of 120 cases of hallucination treated with auricular acupuncture. J. Tradit. Chin. Med. 1988, 8, 263–264. [Google Scholar] [PubMed]
- Shi, Z.X. Observation on the curative effect of 120 cases of auditory hallucination treated with auricular acupuncture. J. Tradit. Chin. Med. 1989, 9, 176–178. [Google Scholar] [PubMed]
- Bosch, P.; Staudte, H.; van den Noort, M.; Lim, S. A case study on acupuncture in the treatment of schizophrenia. Acupunct. Med. 2014, 32, 286–289. [Google Scholar] [CrossRef] [PubMed]
- Bosch, P.; Lim, S.; Yeo, S.; Lee, S.H.; Staudte, H.; van den Noort, M. Acupuncture in the treatment of a female patient suffering from chronic schizophrenia and sleep disorders. Case Rep. Psychiatry 2016, 2016, 6745618. [Google Scholar] [CrossRef] [PubMed]
- Bosch, P.; Staudte, H.; Yeo, S.; Lee, S.H.; Lim, S.; van den Noort, M. Acupuncture treatment of a male patient suffering from long-term schizophrenia and sleep disorders. J. Tradit. Chin. Med. 2017, 37, 862–867. [Google Scholar] [CrossRef]
- Ronan, P.; Robinson, N.; Harbinson, D.; MaxInnes, D. A case study exploration of the value of acupuncture as an adjunct treatment for patients diagnosed with schizophrenia: Results and future study design. Zhong Xi Yi Jie He Xue Bao 2011, 9, 503–514. [Google Scholar] [CrossRef] [PubMed]
- Tani, M.; Suzuki, T.; Takada, A.; Yagyu, T.; Kinoshita, T. Effect of acupuncture treatment for a patient with severe axial dystonia appearing during treatment for schizophrenia. Seishin Shinkeigaku Zasshi 2005, 107, 802–810. [Google Scholar] [PubMed]
- Kane, J.; Di Scipio, W.J. Acupuncture treatment of schizophrenia: Report on three cases. Am. J. Psychiatry 1979, 136, 297–302. [Google Scholar] [PubMed]
- Wu, Y.; Bi, S. Combined use of acupuncture and pharmacotherapy for treatment of auditory hallucination. J. Tradit. Chin. Med. 2004, 24, 180–181. [Google Scholar] [PubMed]
- Reshev, A.; Bloch, B.; Vadas, L.; Ravid, S.; Kremer, I.; Haimov, I. The effects of acupuncture treatment on sleep quality and on emotional measures among individuals living with schizophrenia: A pilot study. Sleep Disord. 2013, 2013, 327820. [Google Scholar] [CrossRef]
- Bloch, B.; Ravid, S.; Vadas, L.; Reshev, A.; Schiff, E.; Kremer, I.; Haimov, I. The acupuncture treatment of schizophrenia: A review with case studies. J. Chin. Med. 2010, 93, 57–63. [Google Scholar]
- Beecroft, N.; Rampes, H. Review of acupuncture for schizophrenia. Acupunct. Med. 1997, 15, 91–94. [Google Scholar] [CrossRef]
- Bosch, P.; van den Noort, M.; Staudte, H.; Lim, S. Schizophrenia and depression: A systematic review of the effectiveness and the working mechanisms behind acupuncture. Explore 2015, 11, 281–291. [Google Scholar] [CrossRef] [PubMed]
- Rathbone, J.; Xia, J. Acupuncture for schizophrenia. Cochrane Database Syst. Rev. 2005, 4, CD005475. [Google Scholar]
- Lee, M.S.; Shin, B.C.; Ronan, P.; Ernst, E. Acupuncture for schizophrenia: A systematic review and meta-analysis. Int. J. Clin. Pract. 2009, 63, 1622–1633. [Google Scholar] [CrossRef] [PubMed]
- Shen, X.; Xia, J.; Adams, C.E. Acupuncture for schizophrenia. Cochrane Database Syst. Rev. 2014, 10, CD005475. [Google Scholar]
- Shen, X.; Xia, J.; Adams, C. Acupuncture for schizophrenia. Schizophr. Bull. 2014, 40, 1198–1199. [Google Scholar] [CrossRef] [PubMed]
- Maeda, Y.; Kim, H.; Kettner, N.; Kim, J.; Cina, S.; Malatesta, C.; Gerber, J.; McManus, C.; Ong-Sutherland, R.; Mezzacappa, P.; et al. Rewiring the primary somatosensory cortex in carpal tunnel syndrome with acupuncture. Brain 2017, 140, 914–927. [Google Scholar] [CrossRef] [PubMed]
- Han, J.S.; Ho, Y.S. Global trends and performances of acupuncture research. Neurosci. Biobehav. Rev. 2011, 35, 680–687. [Google Scholar] [CrossRef] [PubMed]
- Viron, M.; Baggett, T.; Hill, M.; Freudenreich, O. Schizophrenia for primary care providers: How to contribute to the care of a vulnerable patient population. Am. J. Med. 2012, 125, 223–230. [Google Scholar] [CrossRef] [PubMed]
- American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 5th ed.; American Psychiatric Publishing: Arlington, VA, USA, 2013; pp. 87–122. ISBN 139780890425558. [Google Scholar]
- MacPherson, H.; Thomas, K.; Walters, S.; Fitter, M. The York acupuncture safety study: Prospective survey of 34,000 treatments by traditional acupuncturists. BMJ 2001, 323, 486–487. [Google Scholar] [CrossRef] [PubMed]
- MacPherson, H.; Thomas, K.; Walters, S.; Fitter, M. A prospective survey of adverse events and treatment reactions following 34,000 consultations with professional acupuncturists. Acupunct. Med. 2001, 19, 93–102. [Google Scholar] [CrossRef] [PubMed]
- MacPherson, H.; Scullion, A.; Thomas, K.J.; Walters, S. Patient reports of adverse events associated with acupuncture treatment: A prospective national survey. Qual. Saf. Health Care 2004, 13, 349–355. [Google Scholar] [CrossRef] [PubMed]
- Kang, J.M.; Park, H.J.; Choi, Y.G.; Choe, I.H.; Park, J.H.; Kim, Y.S.; Lim, S. Acupuncture inhibits microglial activation and inflammatory events in the MPTP-induced mouse model. Brain Res. 2007, 1131, 211–219. [Google Scholar] [CrossRef] [PubMed]
- González, S.; Moreno-Delgado, D.; Moreno, E.; Pérez-Capote, K.; Franco, R.; Mallol, J.; Cortés, A.; Casadó, V.; Lluís, C.; Ortiz, J.; et al. Circadian-related heteromerization of adrenergic and dopamine D4 receptors modulates melatonin synthesis and release in the pineal gland. PLoS Biol. 2012, 10, e1001347. [Google Scholar] [CrossRef] [PubMed] [Green Version]
- Seeman, P.; Kapur, S. Schizophrenia: More dopamine, more D2 receptors. Proc. Natl. Acad. Sci. USA 2000, 97, 7673–7675. [Google Scholar] [CrossRef] [PubMed]
- Howes, O.D.; Kapur, S. The dopamine hypothesis of schizophrenia: Version III—The final common pathway. Schizophr. Bull. 2009, 35, 549–562. [Google Scholar] [CrossRef] [PubMed]
- Chan, Y.Y.; Lo, W.Y.; Yang, S.N.; Chen, Y.H.; Lin, J.G. The benefit of combined acupuncture and antidepressant medication for depression: A systematic review and meta-analysis. J. Affect. Disord. 2015, 176, 106–117. [Google Scholar] [CrossRef] [PubMed]
- Wang, H.; Qi, H.; Wang, B.S.; Cui, Y.Y.; Zhu, L.; Rong, Z.X.; Chen, H.Z. Is acupuncture beneficial in depression: A meta-analysis of 8 randomized controlled trials? J. Affect. Disord. 2008, 111, 125–134. [Google Scholar] [CrossRef] [PubMed]
- Lim, M.M.; Xu, J.; Holtzman, D.M.; Mach, R.H. Sleep deprivation differentially affects dopamine receptor subtypes in mouse striatum. Neuroreport 2011, 22, 489–493. [Google Scholar] [CrossRef] [PubMed]
- Rung, J.P.; Carlsson, A.; Markinhuhta, K.R.; Carlsson, M.L. The dopaminergic stabilizers (−)-OSU6162 and ACR16 reverse (+)-MK-801-induced social withdrawal in rats. Prog. Neuropsychopharmacol. Biol. Psychiatry 2005, 29, 833–839. [Google Scholar] [CrossRef] [PubMed]
- Van den Noort, M.; Staudte, H.; Perriard, B.; Yeo, S.; Lim, S.; Bosch, P. Schizophrenia and comorbid sleep disorders. Neuroimmunol. Neuroinflamm. 2016, 3, 225–227. [Google Scholar] [CrossRef]
- Ren, X.S.; Kazis, L.E.; Lee, A.F.; Hamed, A.; Huang, Y.H.; Cunningham, F.; Miller, D.R. Patient characteristics and prescription patterns of atypical antipsychotics among patients with schizophrenia. J. Clin. Pharm. Ther. 2002, 27, 441–451. [Google Scholar] [CrossRef] [PubMed]
- Tsutsumi, C.; Uchida, H.; Suzuki, T.; Watanabe, K.; Takeuchi, H.; Nakajima, S.; Kimura, Y.; Tsutsumi, Y.; Ishii, K.; Imasaka, Y.; et al. The evolution of antipsychotic switch and polypharmacy in natural practice: A longitudinal perspective. Schizophr. Res. 2011, 130, 40–46. [Google Scholar] [CrossRef] [PubMed]
- McGrath, J. Dissecting the heterogeneity of schizophrenia outcomes. Schizophr. Bull. 2008, 34, 247–248. [Google Scholar] [CrossRef] [PubMed]
- Jablensky, A. Schizophrenia or schizophrenias? The challenge of genetic parsing of a complex disorder. Am. J. Psychiatry 2015, 172, 105–107. [Google Scholar] [CrossRef] [PubMed]
- World Health Organization. The ICD-10 Classification of Mental and Behavioural Disorders: Clinical Descriptions and Diagnostic Guidelines; World Health Organization Press: Geneva, Switzerland, 1992; pp. 1–374. [Google Scholar]
- Bosch, P.; de Rover, P.; Yeo, S.; Lee, S.H.; Lim, S.; van den Noort, M. Traditional Chinese medicine in psychiatry: The fruit-basket-problem. J. Integr. Med. 2016, 14, 239–240. [Google Scholar] [CrossRef]
- Kay, S.R.; Fiszbein, A.; Opler, L.A. The positive and negative syndrome scale (PANSS) for schizophrenia. Schizophr. Bull. 1987, 13, 261–276. [Google Scholar] [CrossRef] [PubMed]
- Buysse, D.J.; Reynolds, C.F., III; Monk, T.H.; Berman, S.R.; Kupfer, D.J. The Pittsburgh Sleep Quality Index: A new instrument for psychiatric practice and research. Psychiatry Res. 1989, 28, 193–213. [Google Scholar] [CrossRef]
- Johns, M.W. A new method for measuring daytime sleepiness: The Epworth sleepiness scale. Sleep 1991, 14, 540–545. [Google Scholar] [CrossRef] [PubMed]
- Rahman, S.A.; Kayumov, L.; Tchmoutina, E.A.; Shapiro, C.M. Clinical efficacy of dim light melatonin onset testing in diagnosing delayed sleep phase syndrome. Sleep Med. 2009, 10, 549–555. [Google Scholar] [CrossRef] [PubMed]
- Lee, S.H.; van den Noort, M.; Bosch, P.; Lim, S. Sex differences in acupuncture effectiveness in animal models of Parkinson’s disease: A systematic review. BMC Complement. Altern. Med. 2016, 16, 430. [Google Scholar] [CrossRef] [PubMed]
- Yeo, S.; Rosen, B.; Bosch, P.; van den Noort, M.; Lim, S. Gender differences in the neural response to acupuncture: Clinical implications. Acupunct. Med. 2016, 34, 364–372. [Google Scholar] [CrossRef] [PubMed]
- Litscher, D.; Wang, J.; Litscher, G.; Li, G.; Bosch, P.; van den Noort, M.; Wang, L. Gender differences in laser-acupuncture results of a crossover study with green and yellow laser at the ear point Shenmen. Medicines 2018, 5, 24. [Google Scholar] [CrossRef] [PubMed]


© 2018 by the authors. Licensee MDPI, Basel, Switzerland. This article is an open access article distributed under the terms and conditions of the Creative Commons Attribution (CC BY) license (http://creativecommons.org/licenses/by/4.0/).
Share and Cite
Van den Noort, M.; Yeo, S.; Lim, S.; Lee, S.-H.; Staudte, H.; Bosch, P. Acupuncture as Add-On Treatment of the Positive, Negative, and Cognitive Symptoms of Patients with Schizophrenia: A Systematic Review. Medicines 2018, 5, 29. https://doi.org/10.3390/medicines5020029
Van den Noort M, Yeo S, Lim S, Lee S-H, Staudte H, Bosch P. Acupuncture as Add-On Treatment of the Positive, Negative, and Cognitive Symptoms of Patients with Schizophrenia: A Systematic Review. Medicines. 2018; 5(2):29. https://doi.org/10.3390/medicines5020029
Chicago/Turabian StyleVan den Noort, Maurits, Sujung Yeo, Sabina Lim, Sook-Hyun Lee, Heike Staudte, and Peggy Bosch. 2018. "Acupuncture as Add-On Treatment of the Positive, Negative, and Cognitive Symptoms of Patients with Schizophrenia: A Systematic Review" Medicines 5, no. 2: 29. https://doi.org/10.3390/medicines5020029