- Texas Woman’s University, Kinesiology, Denton, TX, USA
Background: The purpose of this study was to conduct a systematic review of the literature to evaluate empirical support for the use of exercise as an evidence-based practice (EBP) for individuals with autism spectrum disorder (ASD), aged 1–21 years, using the Adapted Physical Activity Taxonomy (APAT) (1).
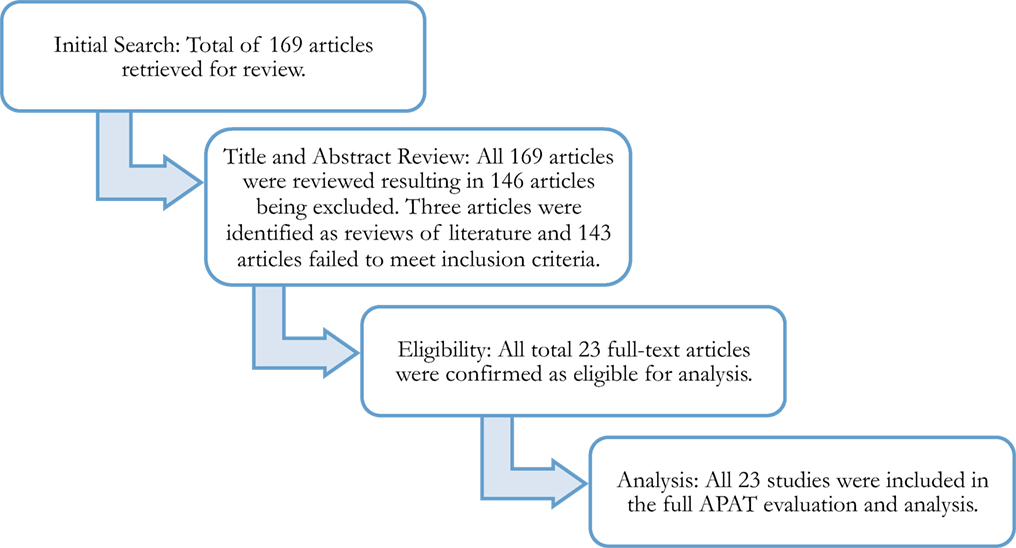
Method: A systematic review of research, published within the past 10 years and accessible in SPORTDiscus, ProQuest Nursing, Science Direct, ERIC, Ovid MEDLINE, and PsychINFO databases, was conducted following seven inclusion criteria. An initial 169 articles were identified of which 23 articles were found that met the inclusion criteria including implementation of an exercise intervention for participants diagnosed with ASD and utilization of an experimental/quasi experimental, correlational, single–subject, or qualitative research design. These 23 articles were evaluated using the APAT to determine the quality of the research and the strength of the recommendation in establishing exercise as an EBP.
Results: Of the 23 articles evaluated, 17 employed an experimental/quasi experimental design, 1 article employed a correlational design, and 5 articles employed a single-subject design. Only one article (2) was found to meet the minimum overall quality indicator of moderate (i.e., Level 2) when evaluated on the APAT. In total, 13 of the 23 articles (57%) had method sections evaluated as weak, and 17 of the 23 articles (74%) had results sections evaluated as weak.
Conclusion: From the findings of this systematic review, and in accordance with the Every Student Succeeds Act of 2015 (3) definition of an EBP, it appears that exercise can be considered an EBP for school-aged children with ASD. However, this recommendation is based solely on moderate evidence from one well-designed and well-implemented experimental study; therefore, generalization is still pending further similar findings. Recommendations for future research are offered.
Autism spectrum disorder (ASD) is defined by the American Psychiatric Association (APA) as a group of developmental disabilities causing significant delays in communication (e.g., limited expressive language) and social skills (e.g., difficulty with social reciprocity) and is associated with repetitive behavior (e.g., engages in hand-flapping) and stereotypical movements (e.g., body rocking) (4). Recent investigations of the motor and exercise patterns of individuals with ASD have also established motor development delays as an attribute of ASD (5–7). Individuals diagnosed with ASD will be categorized as one of three levels based on support needed: Level 1, requiring support; Level 2, requiring substantial support; and Level 3, requiring extreme support at all times (APA). These individual attributes and the levels of support needed by individuals with ASD may interfere with the development of age-appropriate motor skills and participation in exercise.
The physical benefits of exercise reported for children with ASD include improvements in cardiorespiratory functioning (8–10), motor skill performance (11), and muscular strength (10, 12), as well as a reduction in body mass index (13). Along with physical benefits, behavioral and cognitive functioning improvements have been reported. Exercise, as an intervention, has also been shown to reduce maladaptive behaviors (14, 15) and stereotypic behaviors (16) as well as increase on-task behaviors (17) and academic responding (e.g., participating in instructional tasks, asking, and answering questions) (18). Exercise has also been shown to improve academic achievement (19) and social skills (20). However, the research studies cited above provide varying definitions of exercise, utilize different methods to determine levels of heart rate or energy expenditure, and examine differing health-related fitness components. These research studies also involve participants across a wide age range and participants who include, but may not be exclusive to, individuals with ASD. These factors contribute to the difficulties of establishing exercise as an evidence-based practice (EBP). Furthermore, to date, no systematic review has been completed that examines the quality of the research or the strength of the recommendation needed to establish exercise as an EBP.
Evidence-Based Practice
While the exact definition may vary between professions, EBP can generally be defined as an instructional strategy, intervention, or teaching program that is grounded in scientifically based research (21). Within legislation, the Individuals with Disability Education Improvement Act of 2004 lacks a definition but does imply that teachers use EBPs, mandating instructional interventions grounded in “scientifically based research,” when teaching students with disabilities (22). Conversely, the newly passed Every Student Succeeds Act of 2015 (ESSA) (3), after which the reauthorization of IDEA may be modeled, does clearly define evidence-based as:
an activity, strategy, or intervention that—(i) demonstrates a statistically significant effect on improving student outcomes or other relevant outcomes based on—(I) strong evidence from at least 1 well-designed and well-implemented experimental study; (II) moderate evidence from at least 1 well-designed and well-implemented quasi-experimental study; or (III) promising evidence from at least 1 well-designed and well-implemented correlational study with statistical controls for selection bias; or (ii) (I) demonstrates a rationale based on high-quality research findings or positive evaluation that such activity, strategy, or intervention is likely to improve student outcomes or other relevant outcomes; and (II) includes ongoing efforts to examine the effects of such activity, strategy, or intervention (22).
Prior to the Federal definition to guide educational practice, a number of organizations including the National Professional Development Center on Autism Spectrum Disorder (NPDC) and the National Autism Center (NAC) reported on EBPs used in school settings with children with ASD. Both organizations included exercise in their EBP reports but with differing results regarding the effectiveness of exercise, based on the taxonomies used for evaluation.
The NPDC defined EBP as interventions that have been proven through research to be effective and used their own criteria for evaluation when reviewing peer-reviewed research in scientific journals to reported on 27 EBPs for children with ASD (23). NPDC recognized exercise as an EBP and purported that exercise improves physical fitness, increases desired behaviors, and decreases inappropriate behaviors for children with ASD, aged 3–5 years (14, 18); and adolescents with ASD, aged 12 through 14 years (12, 24).
At the same time that the NPDC was releasing their report, the NAC released the National Standards Project: Phase 2 Report (25). For their report, the NAC adopted the definition of an EBP offered by Dr. David Sackett and his colleagues in Evidence-Based Medicine: How to Practice and Teach EBM (26) and systematically evaluated peer-reviewed research using a Scientific Merit Rating Scale and a Strength of Evidence Taxonomy. Within their National Standards Project: Phase 2 Report (25), the NAC identified 14 established EBPs, for children and young adults under the age of 22 years, but did not identify exercise within the established EBPs. Rather, the NAC identified exercise as an intervention with an emerging level of support and indicated that more high-quality studies were needed that consistently documents the effectiveness of exercise. The discrepancy between the conclusions drawn by the NPDC and the NAC, two leading organizations for research on children with ASD, makes the selection and implementation of EBPs problematic for teachers and researchers.
In order to gain scientific corroboration, there is a need to determine evidence for the establishment of exercise as an EBP for individuals with ASD. However, to date, no systematic review of the literature has been completed on exercise as an EBP using a taxonomy specific to the field of adapted physical activity or the discipline of kinesiology that educators could use to justify their use of exercise as an EBP. Therefore, the purpose of this study was to conduct a systematic review of the literature to evaluate empirical support for the use of exercise as an EBP for individuals with ASD, aged 1–21 years, using the Adapted Physical Activity Taxonomy (APAT) (1).
Method
Systematic Review Procedures
This systematic review of the literature (27) focused on the use of exercise as an intervention for children and youth with ASD. Prior to conducting the literature search, the reviewers unanimously agreed to (a) the operational definition for exercise for the study as “a subcategory of physical activity that is planned, structured, repetitive, and purposive to improve or maintain one’s physical fitness” (p. 250) (28) and (b) the minimum APAT (1) Quality of Study rating (i.e., Level 1 or Level 2) and Level of Recommendation (i.e., A or B) needed for the establishment of exercise as an EBP. These parameters, along with the inclusion criteria, guided the systematic review (see Figure 1 for an overview of the procedures).
Initial Search Procedure
Potential articles, published in the past 10 years, were initially located via online indexing system searches. The reference lists of the articles found through the online search were also manually searched for potential articles. The reviewers conducted an initial search of the literature using the indexing systems/research platforms of SPORTDiscus, ProQuest Nursing, Science Direct, ERIC, Ovid MEDLINE, and PsychINFO. Searches were conducted with search limiters of English language journals published within the last 10 years, and the keywords of exercise and ASD including the terms autism, Asperger’s syndrome, and PDD-NOS.
Criteria for Inclusion
The following seven inclusion criteria were selected by the five authors and required that articles be (a) published between January 2006 and April 2016; (b) published in English language journals; (c) located in periodical publications (i.e., books, unpublished papers, conference proceedings and book chapters were excluded); (d) involved implementation of an exercise intervention consistent with the adopted operational definition for exercise; (e) provided a clear description of the participants as individuals diagnosed with ASD, to include participants with autism, Asperger’s syndrome and Pervasive-Developmental Disorder—Not Otherwise Specified (i.e., studies with participants with ASD who were diagnosed with other/secondary disabilities were excluded); (f) included participants between the ages of 1 and 21 years; and (g) utilized an experimental/quasi experimental, correlational, single-subject, or qualitative research design (i.e., systematic reviews and meta-analyses were excluded). Only articles that met these criteria were eligible for evaluation.
Title and Abstract Review
Research studies, identified through the initial search procedure, were then evaluated using a three-step process. First, reviewers conducted a title and abstract review on the potential studies identified in the initial search to confirm studies met inclusion criteria. Articles identified as reviews of literature were excluded but the reference lists from these articles were examined for additional potential articles. In the second step, articles meeting the inclusion criteria were then independently evaluated by one of the authors using the APAT. Finally, the second author independently evaluated each article to confirm agreement on the evaluation of the article as a Level I, II, or III.
Instrumentation
The APAT Quality of the Study and Letter of Recommendation (1) were used as the decision-making tool to rate the quality of each individual study and the strength of the recommendations for each of the identified articles. Designed to address four types of research designs (i.e., experimental/quasi experimental, single-subject, correlational, qualitative), the APAT contains five evaluation domains (i.e., introduction, method, results, discussion, and others) with quality indicators delineated within each domain. See Tables 1–3 for additional details regarding the content evaluated within each domain. These domains guide the evaluation of the article and provide an APAT Quality of the Study rating (i.e., Level 1 = strong; Level 2 = moderate; Level 3 = weak). The APAT also follows a standardized decision-making process to determine an APAT Level of Recommendation (i.e., A, B, and C Levels of Recommendation) for the research reported within the article. Articles evaluated as having a Level of Recommendation of A are those studies with outcomes that meet at least one of the following: (a) “result in significant value that can be applied to educational, recreational, and disability sport settings”; (b) have “consistent findings from at least two good-quality randomized controlled trials or a systematic review/meta-analysis”; or (c) have a “validated intervention decision relevant to a disability population” [APAT: Level of Recommendation (Part II)].
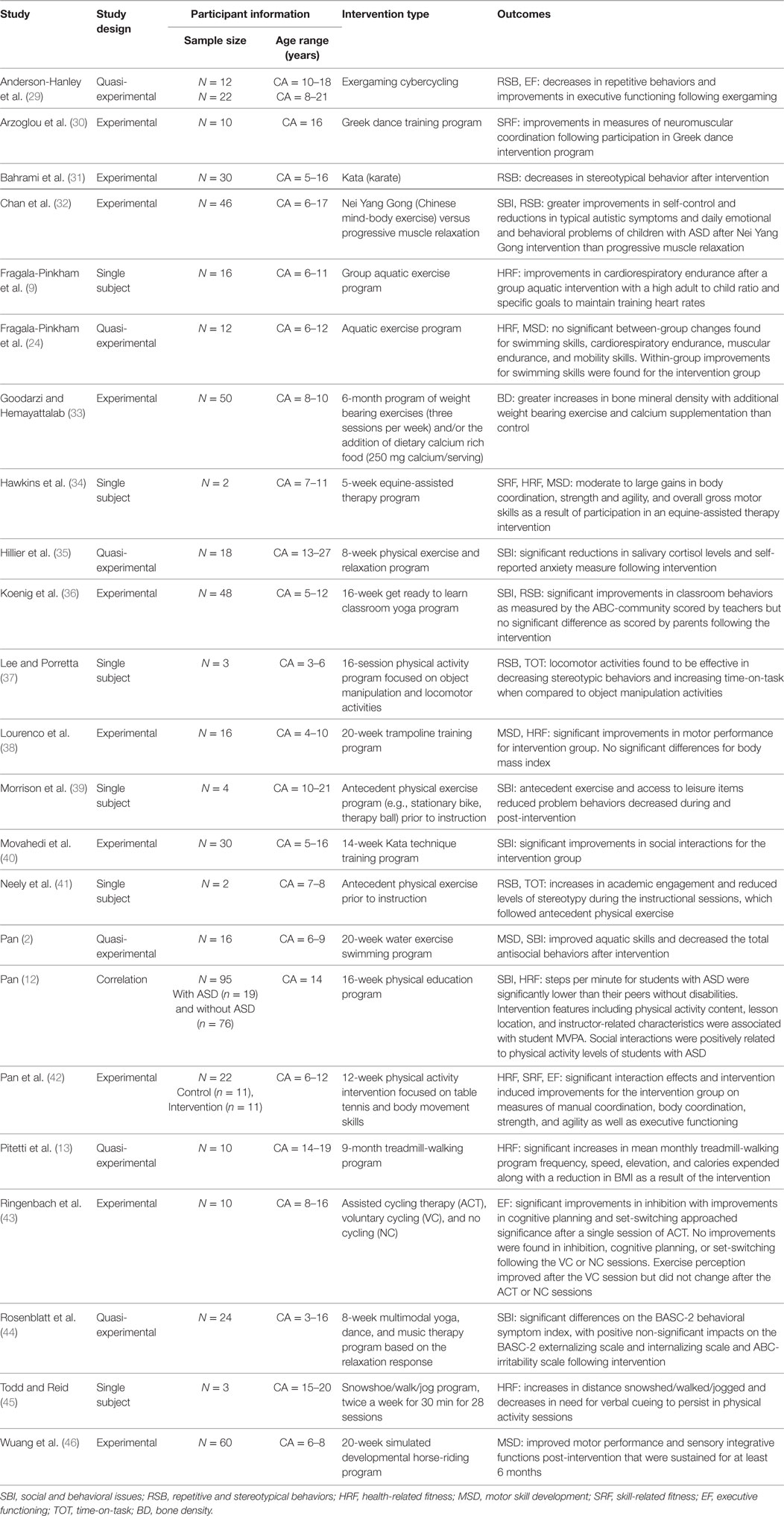
Table 1. Exercise intervention studies for individuals with autism spectrum disorder (ASD): study design, participant information, intervention type, and outcomes.
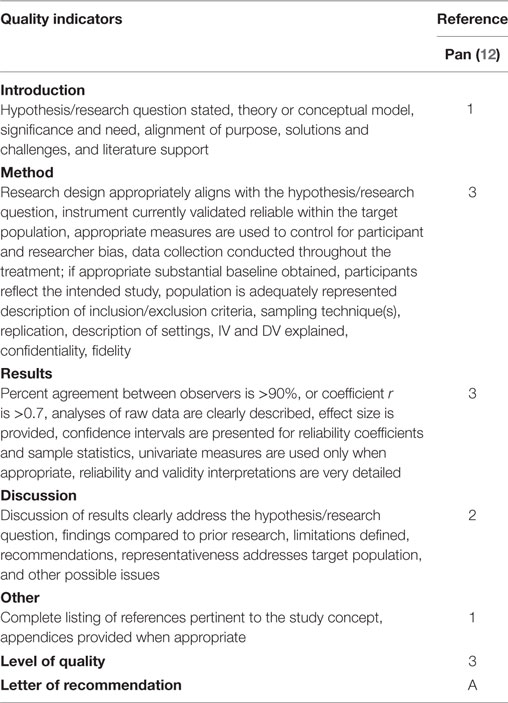
Table 2. Adapted Physical Activity Taxonomy quality indicator ratings for correlational research reviewed.
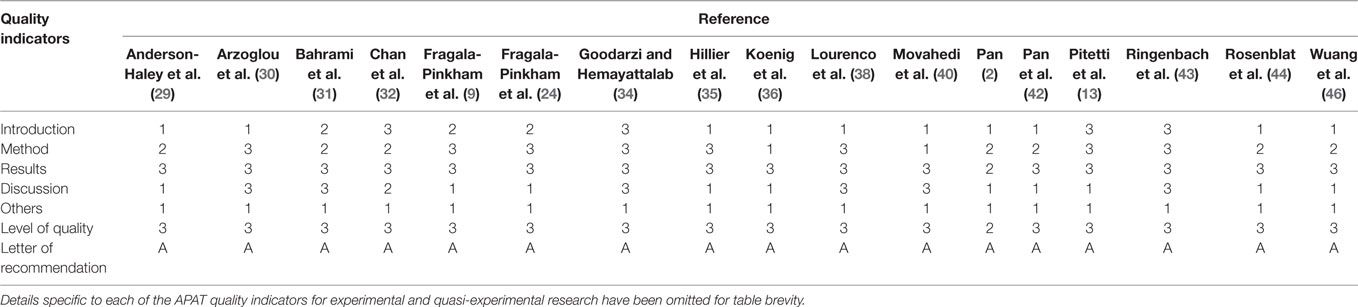
Table 3. Adapted Physical Activity Taxonomy (APAT) quality indicator ratings for experimental/quasi experimental research reviewed.
Inter-Rater Agreement
The authors of this article independently assessed all the titles and abstracts to determine whether the studies met the criteria for inclusion using a dichotomous scale (yes or no). In instances of disagreement, articles were re-assessed until an inter-rater agreement of 100% was reached. All of the articles were also independently evaluated by at least two of the current authors using the APAT. There were no instances of disagreement during the evaluation using the APAT; hence, there was 100% inter-rater consensus.
Results
The initial search of the literature identified 169 exercise-based intervention studies targeting individuals with ASD, aged 1–21 years (see Figure 1). Of the 169 articles identified through the initial search, 146 articles were excluded from further analysis as a result of failing to meet 1 of the 7 inclusion criteria. Three of the 146 articles were excluded because they were identified as reviews of literature in the title and abstract review. The references for these articles were examined for additional articles. None of the potential articles found on the reference list met the publication year inclusion criteria. See Figure 1 for a summary of the systematic review process.
The resulting 23 articles remained for analysis and were evaluated using the APAT, with 17 articles evaluated as experimental/quasi experimental, 1 article as correlational, and 5 articles as single-subject designs. Table 1 presents a summary of each article reviewed including the study design, participant information, intervention type, and study outcomes. The studies evaluated employed fitness-focused exercise (n = 8), aquatics (n = 3), karate and martial arts training (n = 3), motor skills programming (n = 3), yoga (n = 2), dance (n = 2), equine-assisted programming (n = 2), relaxation training (n = 2), and exergaming (n = 1) interventions. These exercise interventions implemented attempted to address ASD-related issues including social and behavioral issues (n = 8), repetitive and stereotypical behaviors (n = 5), health-related fitness (n = 4), skill development (n = 4), skill-related fitness (n = 3), cognitive functioning (n = 2), and time-on-task (n = 2). While the interventions were implemented with participants with ASD from 4 to 27 years of age, a majority of the studies (74%) targeted adolescents with ASD as participants.
In addition to the descriptive summary table, a summary of the APAT evaluation ratings for the 23 articles reviewed are presented, by research design, in Tables 2–4. A closer examination of the articles presented in Tables 2–4 reveals that 13 of the 23 articles (57%) had method sections evaluated as weak (i.e., Level 3 rating), and 17 of the 23 articles (74%) had results sections evaluated as weak. This weak rating is problematic as the method and results sections provide details essential to quality design and study replication as well as the research findings. Additionally, 10 of the 23 articles (43%) were published without a clearly stated hypothesis or theory.
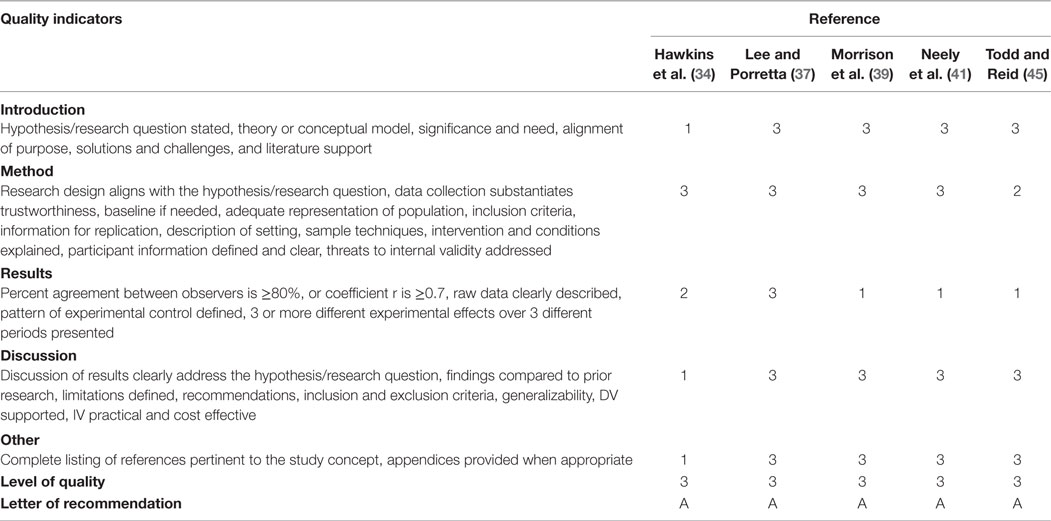
Table 4. Adapted Physical Activity Taxonomy quality indicator ratings for single-subject design research reviewed.
As can be observed from the aforementioned tables, only 1 article (2) from the 23 articles reviewed was found to meet the minimum overall quality indicator of Level 2 when evaluated on the APAT. In his research, Pan (2) examined the effects of a water exercise swimming program on the aquatic skills and social behaviors of children, aged 6–9 years, diagnosed with ASD. The participants were split into two groups, Group A (n = 8) and Group B (n = 8). Group A received water exercise swimming program in the first 10-week phase followed by a week break and then a 10-week phase of baseline treatment/activity. Group B received treatments in reverse order. Pan (2) found improved aquatic skills as well as a decrease in the frequency of antisocial behaviors (e.g., spinning, rocking, and delayed echolalia) in children with ASD. While Pan (2) was able to report significant improvements in aquatic skills, sustainability of improvements, and significant decreases all antisocial behaviors, the research article as a whole was evaluated as having only moderate strength of quality. More specifically, when evaluated via the APAT, the Pan article (2) was strong (i.e., Level 1) in the introduction, discussion, and other section but only moderate in the method section (e.g., sampling technique described but not replicable), and the results section (e.g., reliability and validity interpretation lacked detail) producing a moderate overall rating.
Discussion
The purpose of the current study was to conduct a systematic review of the literature to evaluate empirical support for the use of exercise as an EBP for individuals with ASD, aged 1–21 years. A total of 23 articles were evaluated. Based on the findings of this systematic review, and utilizing the newly enacted ESSA (2016) definition of an EBP, it appears that exercise can be considered an EBP for school-aged children with ASD. However, this recommendation is based solely on moderate evidence from one well-designed and well-implemented experimental study (2), therefore, generalization is still pending further similar findings. These current systematic review findings are consistent with that of Lang et al. (47) who reported a limited literature base and called for additional high-quality research, especially studies using a strong experimental design, which could assist educators in developing effective programing for individuals with ASD.
As researchers move forward with designing and conducting the research to further establish the evidence base, they need to be mindful of the research-to-practice gap. It has been established that interventions that are too narrowly focused, complex, difficult to implement or costly; or interventions that do not meet the perceived needs of the community (48) perpetuate the gap and impede the process of converting empirically supported discoveries into routine educational practices. For example, within his study, Pan implemented a 10-week water exercise swimming program with multiple swimming instructors (i.e., a one instructor-to-two student instructional setting) and two 90-min instructional sessions per week. This design, while ideal for research purposes, is not easily implemented in PK-12 settings where instructional sessions are often shorter, staff ratios higher, and pools present in only some of the schools. Furthermore, researchers must take care to report all of the information critical to their research design and findings, such as those quality indicators outlined in the APAT (1), in order to improve the quality of the study and strengthen the resulting recommendations. We recognize that this can be a daunting task, but it is essential if exercise, or any other instructional strategy, intervention, or teaching program is to be firmly established as an EBP (21) for use with children and youth with ASD.
Author Contributions
The first author, SD, was responsible for designing and guiding the systematic review and was responsible for the preparation/writing of the manuscript. The remaining authors (DA, LG, SM, and MB) were involved in the systematic review of the literature including the evaluation of the 23 articles using the Adapted Physical Activity Taxonomy. The second (DA) and third (LG) authors provided significant assistance to the first author in the development of the manuscript. The fourth (SM) and fifth (MB) authors also provided editorial assistance in the development of the manuscript but to a lesser extent than the second and third authors.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Carano SL. Development of a Research Taxonomy for Adapted Physical Activity [Dissertation]. Ann Arbor: Texas Woman’s University (2014).
2. Pan C. Effects of water exercise swimming program on aquatic skills and social behaviors in children with autism spectrum disorders. Autism (2010) 14(1):9–28. doi: 10.1177/1362361309339496
4. American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders. 5th ed. Washington, DC: American Psychiatric Association (2013).
5. Green D, Charman T, Pickles A, Chandler S, Loucas T, Simonoff E, et al. Impairment in movement skills of children with autistic spectrum disorders. Dev Med Child Neurol (2009) 51(4):311–6. doi:10.1111/j.1469-8749.2008.03242.x
7. Lloyd M, MacDonald M, Lord C. Motor skills of toddlers with autism spectrum disorders. Autism (2013) 17:133–46. doi:10.1177/1362361311402230
8. Yilmaz I, Yanarda M, Birkan B, Bumin G. Effects of swimming training on physical fitness and water orientation in autism. Pediatr Int (2004) 46(5):624–6. doi:10.1111/j.1442-200x.2004.01938.x
9. Fragala-Pinkham M, Haley S, O’Neil M. Group aquatic aerobic exercise for children with disabilities. Dev Med Child Neurol (2008) 50(11):822–7. doi:10.1111/j.1469-8749.2008.03086.x
10. Lochbaum M, Crews D. Viability of cardiorespiratory and muscular strength programs for the adolescent with autism. Comp Health Prac Rev (2003) 8(3):225–33. doi:10.1177/1076167503252917
11. Rogers L, Hemmeter ML, Wolery M. Using a constant time delay procedure to teach foundational swimming skills to children with autism. Top Early Child Spec Educ (2010) 30(2):102–11. doi:10.1177/0271121410369708
12. Pan C. The efficacy of an aquatic program on physical fitness and aquatic skills in children with and without autism spectrum disorders. Res Autism Spectr Disord (2011) 5(1):657–65. doi:10.1016/j.rasd.2010.08.001
13. Pitetti KH, Rendoff AD, Grover T, Beets MW. The efficacy of a 9-month treadmill walking program on the exercise capacity and weight reduction for adolescents with severe autism. J Autism Dev Disord (2007) 37(6):997–1006. doi:10.1007/s10803-006-0238-3
14. Celiberti DA, Bobo HE, Kelly KS, Harris SL, Handleman JS. The differential and temporal effects of antecedent exercise on the self-stimulatory behavior of a child with autism. Res Dev Disabil (1997) 18(2):139–50. doi:10.1016/S0891-4222(96)00032-7
15. Elliott RO, Dobbin AR, Rose GD, Soper HV. Vigorous, aerobic exercise versus general motor training activities: effects on maladaptive and stereotypic behaviors of adults with both autism and mental retardation. J Autism Dev Disord (1994) 24(5):565–76. doi:10.1007/BF02172138
16. Levinson L. The Effects of Exercise Intensity on the Stereotypic Behaviours of Individuals with Autism. Ann Arbor: McGill University (Canada) (1991).
17. Mahar MT, Murphy SK, Rowe DA, Golden J, Shields AT, Raedeke TD. Effects of a classroom-based program on physical activity and on-task behavior. Med Sci Sports Exerc (2006) 38(12):2086–94. doi:10.1249/01.mss.0000235359.16685.a3
18. Oriel KN, George CL, Peckus R, Semon A. The effects of aerobic exercise on academic engagement in young children with autism spectrum disorder. Pediatr Phys Ther (2011) 23(2):187–93. doi:10.1097/PEP.0b013e318218f149
19. Nicholson H, Kehle T, Bray M, Heest J. The effects of antecedent physical activity on the academic engagement of children with autism spectrum disorder. Psychol Sch (2011) 48(2):198–213. doi:10.1002/pits.20537
20. Bass MM, Duchowny CA, Llabre MM. The effect of therapeutic horseback riding on social functioning in children with autism. J Autism Dev Disord (2009) 39(9):1261–7. doi:10.1007/s10803-009-0734-3
21. Mesibov G, Shea V. Evidence-based practices and autism. Autism (2010) 15(1):114–33. doi:10.1177/1362361309348070
23. National Professional Development Center on Autism Spectrum Disorder. What Criteria Determined Whether an Intervention Was Effective? (2015). Available from: http://autismpdc.fpg.unc.edu/what-criteria-determined-if-intervention-was-effective
24. Fragala-Pinkham M, Haley SM, O’Neil ME. Group swimming and aquatic exercise programme for children with autism spectrum disorders: a pilot study. Dev Neurorehabil (2011) 14(4):230–41. doi:10.3109/17518423.2011.575438
25. National Autism Center. National Standards Project-Addressing the Need for Evidence-Based Practice Guidelines for Autism Spectrum Disorders. Randolph, MA: The Institute (2009).
26. Sackett DL, Richardson WS, Rosenburg WM, Haynes RB. Evidence-Based Medicine: How to Practice and Teach EBM. New York, NY: Churchill Livingstone (1997). p. 1–11.
27. Grant MJ, Booth A. A typology of reviews: an analysis of 14 review types and associated methodologies. Health Info Libr J (2009) 26(2):91–108. doi:10.1111/j.1471-1842.2009.00848.x
28. Rimmer JH, Chen M, McCubbin JA, Drum C, Peterson J. Exercise intervention research on persons with disabilities: what we know and where we need to go. Am J Phys Med Rehabil (2010) 89(3):249–63. doi:10.1097/PHM.0b013e3181c9fa9d
29. Anderson-Hanley C, Tureck K, Schneiderman RL. Autism and exergaming: effects on repetitive behaviors and cognition. Psychol Res Behav Manag (2011) 4:129–37. doi:10.2147/PRBM.S24016
30. Arzoglou D, Tsimaras V, Kotsikas G, Fotiadou E, Sidiropoulou M, Proios M, et al. The effect of a traditional dance training program on neuromuscular coordination of individuals with autism. J PE Sport (2013) 13(4):563–9. doi:10.7752/jpes.2013.04088
31. Bahrami F, Movahedi A, Marandi SM, Abedi A. Kata techniques training consistently decreases stereotypy in children with autism spectrum disorder. Res Dev Disabil (2012) 33(4):1183–93. doi:10.1016/j.ridd.2012.01.018
32. Chan AS, Sze SL, Siu NY, Lau EM, Cheung MA. Chinese mind-body exercise improves self-control of children with autism: a randomized controlled trial. PLoS One (2013) 8(7):e68184. doi:10.1371/journal.pone.0068184
33. Goodarzi M, Hemayattalab R. Bone mineral density accrual in students with autism spectrum disorders: effects of calcium intake and physical training. Res Autism Spectr Disord (2012) 6(2):690–5. doi:10.1016/j.rasd.2011.02.015
34. Hawkins BL, Ryan JB, Cory AL, Donaldson MC. Effects of equine-assisted therapy on gross motor skills of two children with autism spectrum disorder: a single-subject research study. Ther Recreation J (2014) 48(2):135–49.
35. Hillier A, Murphy D, Ferrara C. A pilot study: short-term reduction in salivary cortisol following low level physical exercise and relaxation among adolescents and young adults on the autism spectrum. Stress Health (2011) 27:395–402. doi:10.1002/smi.1391
36. Koenig KP, Buckley-Reen A, Garg S. Efficacy of the get ready to learn yoga program among children with autism spectrum disorders: a pretest-posttest control group design. Am J Occup Ther (2012) 66(5):538–46. doi:10.5014/ajot.2012.004390
37. Lee J, Porretta DL. Physical activity on stereotypic behaviors and task engagement in autism. Res Q Exerc Sport (2014) 85:A76–7.
38. Lourenco C, Esteves D, Corredeira R, Seabra A. Children with autism spectrum disorder and trampoline training. Paleastra (2015) 29(4):20.
39. Morrison H, Roscoe EM, Atwell A. An evaluation of antecedent exercise on behavior maintained by automatic reinforcement using a three-component multiple schedule. J Appl Behav Anal (2011) 44(3):523–41. doi:10.1901/jaba.2011.44-523
40. Movahedi A, Bahrami F, Marandi SM, Abedi A. Improvement in social dysfunction of children with autism spectrum disorder following long term Kata techniques training. Res Autism Spectr Disord (2013) 7(9):1054–61. doi:10.1016/j.rasd.2013.04.012
41. Neely L, Rispoli M, Gerow S, Ninci J. Effects of antecedent exercise on academic engagement and stereotypy during instruction. Behav Modif (2015) 39(1):98–116. doi:10.1177/0145445514552891
42. Pan C, Chu C, Tsai C, Sung M, Huang C, Ma W. The impacts of physical activity intervention on physical and cognitive outcomes in children with autism spectrum disorder. Autism (2017) 21(2):190–202. doi:10.1177/1362361316633562
43. Ringenbach S, Lichtsinn K, Holzapfel S. Assisted Cycling Therapy (ACT) improves inhibition in adolescents with autism spectrum disorder. J Intellect Dev Disabil (2015) 40(4):376–87. doi:10.3109/13668250.2015.1080352
44. Rosenblatt LE, Gorantla S, Torres JA, Yarmush RS, Rao S, Park ER, et al. Relaxation response-based yoga improves functioning in young children with autism: a pilot study. J Altern Complement Med (2011) 17(11):1029–35. doi:10.1089/acm.2010.0834
45. Todd T, Reid G. Increasing physical activity in individuals with autism. Focus Autism Other Dev Disabil (2006) 21(3):167–76. doi:10.1177/10883576060210030501
46. Wuang Y, Wang C, Huang M, Su C. The effectiveness of simulated developmental horse-riding program in children with autism. Adapt Phys Activ Q (2010) 27(2):113–26. doi:10.1123/apaq.27.2.113
47. Lang R, Koegel LK, Ashbaugh K, Regester A, Ence W, Smith W. Physical exercise and individuals with autism spectrum disorders: a systematic review. Res Autism Spect Dis (2010) 4:565–76. doi:10.1016/j.rasd.2010.01.006
Keywords: evidence-based practice, exercise, autism spectrum disorder, systematic review, adapted physical education
Citation: Dillon SR, Adams D, Goudy L, Bittner M and McNamara S (2017) Evaluating Exercise as Evidence-Based Practice for Individuals with Autism Spectrum Disorder. Front. Public Health 4:290. doi: 10.3389/fpubh.2016.00290
Received: 13 September 2016; Accepted: 20 December 2016;
Published: 07 February 2017
Edited by:
Megan MacDonald, Oregon State University, USACopyright: © 2017 Dillon, Adams, Goudy, Bittner and McNamara. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Suzanna R. Dillon, sdillon@twu.edu
 Suzanna R. Dillon
Suzanna R. Dillon David Adams
David Adams Leah Goudy
Leah Goudy Melissa Bittner
Melissa Bittner Scott McNamara
Scott McNamara