- 1Department of Social Medicine and Health Management, Xiangya School of Public Health, Central South University, Changsha, China
- 2Chinese Evidence-Based Medicine Center, West China Hospital, Sichuan University, Chengdu, China
- 3Hunan Provincial Center for Disease Prevention and Control, Changsha, China
- 4Human Immunodeficiency Virus/Acquired Immunodeficiency Syndrome Research Institute, The First Hospital of Changsha, Changsha, China
- 5Furong District Center for Disease Prevention and Control, Changsha, China
Background: The Pittsburgh Sleep Quality Index (PSQI) has been a widely used instrument measuring sleep quality among people living with HIV (PLWH) in China while its psychometric properties have yet to be examined in this population. We aimed to assess the reliability and validity of the Chinese version of PSQI in PLWH and identify factors associated with sleep quality.
Methods: This study was based on a longitudinal study of newly diagnosed PLWH, among whom the PSQI was used to measure sleep quality 5 years after HIV diagnosis (n = 386). To evaluate internal consistency, Cronbach's alpha and corrected item-total correlation were calculated. To assess construct validity, Pearson's correlation coefficients were calculated between PSQI scores and depression, anxiety, stress, and health-related quality of life (HRQoL). Known group validity was evaluated by comparing PSQI scores between participants with probable depression and those without. Binary logistic regression was conducted to identify factors associated with sleep disturbances.
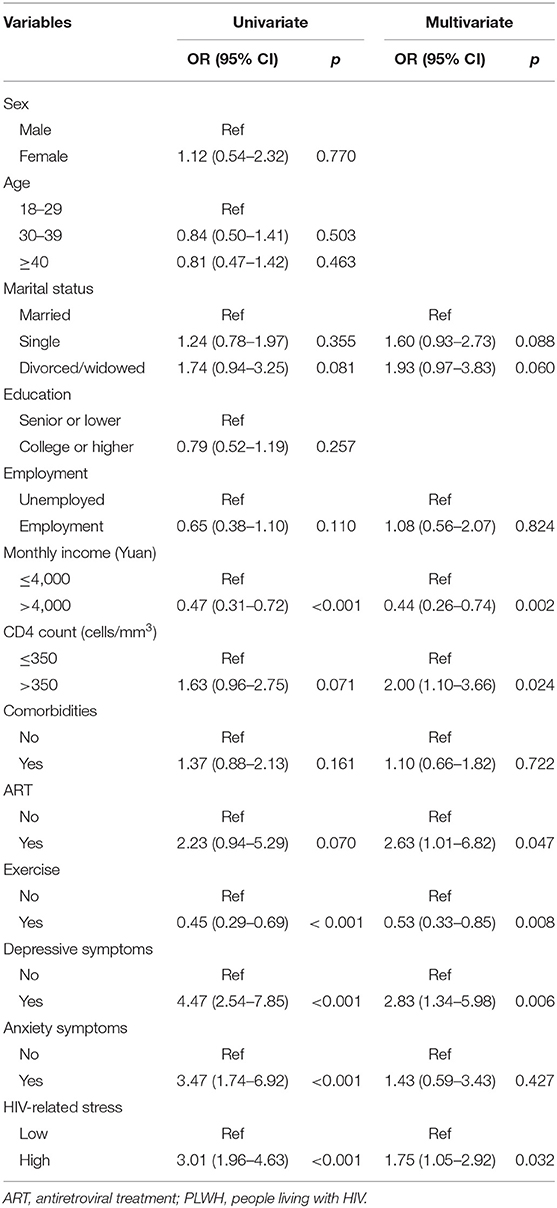
Results: The internal consistency Cronbach's alpha for the Chinese version of PSQI in PLWH was 0.713. Construct validity was established by significant relationships between PSQI and depression, anxiety, stress, and HRQoL. The PSQI scores in participants with probable depression were significantly higher than those without, indicating good known-group validity. Sleep disturbances were associated with less income, higher CD4 counts, antiretroviral treatment (ART) initiation, exercise, depression, and higher stress levels.
Conclusions: The Chinese version of PSQI is feasible for use among Chinese PLWH. Over a third of PLWH reported sleep disturbances. More attention should be given to individuals with less income and on ART. Intervention aimed at improving mental health or facilitating exercise may improve sleep quality.
Introduction
Receiving diagnosis of HIV infection is considered as an extremely stressful experience for most individuals, accompanied with considerable stressors such as stigma, disclosure, emotional distress, medication side effects, and declines in physical function (1, 2), which are known to be strong predictors of sleep disturbances among people living with HIV (PLWH) (3, 4). PLWH are, therefore, more likely to be vulnerable to sleep problems (5). A meta-analysis estimating the prevalence of self-reported sleep disturbances among PLWH found that approximately more than half of PLWH report sleep disturbances after diagnosis (5), while PLWH complaining of poor sleep quality have been shown to be less likely to adhere to recommended treatment and more likely to suffer multiple mental disorders (6, 7), which may negatively impact the immune and virologic responses (8), leading to treatment failure (9) and, ultimately, influencing the quality of life in this population (10).
Given the significantly negative consequence of the poor sleep quality among PLWH, providing a reliable estimate of the prevalence of sleep disturbances has been increasingly important. Sleep quality is evaluated either by self-reported or interviewer-rated scales or objective measures (such as polysomnography and actigraphy) (11). Empirical evidence showed that self-reported measures are user-friendly, reliable, and sensitive to change in sleep pattern and quality (12). Of the different measures on sleep quality, the Pittsburgh Sleep Quality Index (PSQI) is the most widely used (5). The Chinese version of the PQSI was translated in 1996 by Liu et al. and have been subsequently examined in different populations including the civil servants, college students, and rural elderly (13), all indicating the Chinese version PSQI is a reliable and valid instrument for evaluating sleep quality (14–16).
Although previous studies have explored various psychometric properties of the Chinese-version PSQI across different clinical and non-clinical groups, its application in PLWH has yet to be examined. This study aimed to (1) examine the reliability and validity of the Chinese version of the PQSI in PLWH, and (2) assess the prevalence of poor sleep quality using PQSI and identify the factors associated with poor sleep quality among PLWH.
Methods
Participants
Participants were HIV-infected patients enrolled since 2013 in a longitudinal study designed to evaluate mental health challenges, among people with newly diagnosed HIV infection. Relevant description on the study design is available in elsewhere (17). Briefly, individuals with newly diagnosed HIV were consecutively recruited from the Changsha Center for Disease Control and Prevention, Hunan Province, China. Individuals were eligible if they were (1) receiving HIV diagnosis for less than 1 month (newly diagnosed with HIV), (2) more than 18 years of age, and (3) having lived in Changsha city for more than 6 months. This study was approved by the Ethics Committee of Xiangya School of Public Health Central South University (ZYGW-2018-055). Written informed consent was obtained from each participant before participation.
A total of 855 people newly diagnosed with HIV met the inclusion criteria, among which 557 participants completed the baseline survey between March 1, 2013 and September 30, 2014. After 1 year, 410 participants continued to participate in the follow-up survey. Among the 557 individuals who completed the baseline survey, 386 agreed to participate in the 5-year follow-up survey which was conducted between August 1, 2018 and March 29, 2019. This study was based on data from 5-year follow-up survey in which the sleep quality was added as a new variable of interest.
Measures
Socio-Demographic Information
Demographic information included gender, age (18–29, 30–39, or ≥40), marriage status (single, married, or divorced/widowed), education (senior or below, college or above), employment (employed or unemployed), monthly income (≤ 4,000 Yuan or >4,000 Yuan), and exercise behavior (yes or no).
Sleep Quality
Sleep quality was assessed by the Chinese version of PSQI, which was translated and validated by Liu et al. in 1996 (13). The original scale was designed by Buysse et al. which was used to measure the sleep quality and disturbances over the past month (12). It includes 18 items consisting of seven components: subjective quality of sleep, sleep latency, sleep duration, habitual sleep efficiency, sleep disturbance, use of sleep medication, and daytime dysfunction. Each item is scored from 0 (not during the past month) to 3 (three or more times a week), with total score ranging from 0 to 21. A higher score suggests poorer sleep quality. A cut-off score of 5 has been recommended to screen for sleep disturbance by Buysse et al. (12).
Clinical Information
Clinical information including CD4 counts and antiretroviral treatment (ART) status were obtained from the Chinese HIV/AIDS Comprehensive Response Information Management System. In addition, participants were asked in questionnaire whether they had any other disease (except for HIV infection).
Depression
Depression was assessed by the 9-item Patient Health Questionnaire Depression Scale (PHQ-9) (18). Participants responded on a 4-point Likert-type scale ranging from 0 (not at all) to 3 (nearly every day). The total score of scare ranges from 0 to 27, with a score ≥10 being considered a cut-off screening for significant depressive symptoms (19). The Chinese version of the PHQ-9 shows good reliability and validity with a Cronbach's α coefficient of 0.86 (20).
Anxiety
Anxiety was measured by the 7-item Generalized Anxiety Disorder questionnaire (GAD-7) (21). Each item was rated on a 4-point Likert scale ranging from 0 (not at all) to 3 (nearly every day). The total score of scale ranges from 0 to 21. A score of 10 points or higher was usually used as cut-off to identify significant anxiety symptoms (22). The Chinese version of GAD-7 shows good reliability and validity with a Cronbach's α coefficient of 0.88 (23).
Stress
The Chinese version of HIV/AIDS Stress Scale (CSS-HIV) was used to assess HIV-related stress (23). It was first developed by Pakenham et al. (24), and Niu et al. later translated it into Chinese version. This scale consists of three subscales: social stress, instrumental stress, and emotional stress. Participants were asked how much stress they had endured in the past month on a 5-point Likert-type scale. A higher score indicates higher levels of stress. In this study, the median score of the CSS-HIV (P50 = 13) was used as the cut-off to divide low and high stress. The CSS-HIV has good validity and reliability, with an overall Cronbach's α coefficient of 0.906 (23).
Health-Related Quality of Life
The health-related quality of life was measured using the Medical Outcomes Study HIV Survey (MOS-HIV) (25). The MOS-HIV includes 35 items with 11 dimensions containing general health, physical function, role function, cognitive function, pain, mental health, health distress, energy/fatigue, social function, overall quality of life, and health transition. Based on standard scoring procedures, a physical health summary score and a mental health summary score could be calculated. The Chinese version of the MOS-HIV has shown good validity and reliability among PLWH (26).
Statistical Analysis
The continuous variables were described as median with interquartile ranges (IQRs) and categorical variables were described as numbers with percentages. To evaluate the internal consistency, we calculated Cronbach's alpha for overall scale and corrected item-total correlation, with Cronbach's α ≥0.70 and corrected correlations ≥0.30 indicating adequate internal consistency (27). To evaluate construct validity, Pearson's correlation coefficients were calculated between PSQI scores and other theoretically related constructs, i.e., depression, anxiety, stress, and HRQoL. Known group validity was evaluated by comparing each component scores of PSQI between participants with probable depression (PHQ-9 ≥ 10) and without depression (PHQ-9 < 17) using independent sample t test. We hypothesized that depression is negatively associated with poor sleep quality. To identify the factors associated with sleep disturbances (defined as PSQI > 5), univariate logistical regression was conducted, with experiencing sleep disturbance or not as dependent variable, and sex, age, marital status, education, employment, monthly income, CD4 count, comorbidities, ART status, exercise, HIV-related stress, depressive, and anxiety symptoms as independent variables. Variables that were statistically associated with sleep disturbances with a p ≤ 0.2 in the univariate logistic regression were further selected into the multiple logistic regression model. Odds ratios (OR) and 95% CIs were presented. All analyses were conducted using SPSS 22.0 (SPSS Inc., Chicago, IL, USA) with two-tailed p < 0.05 considered statistically significant.
Results
Sample Characteristics
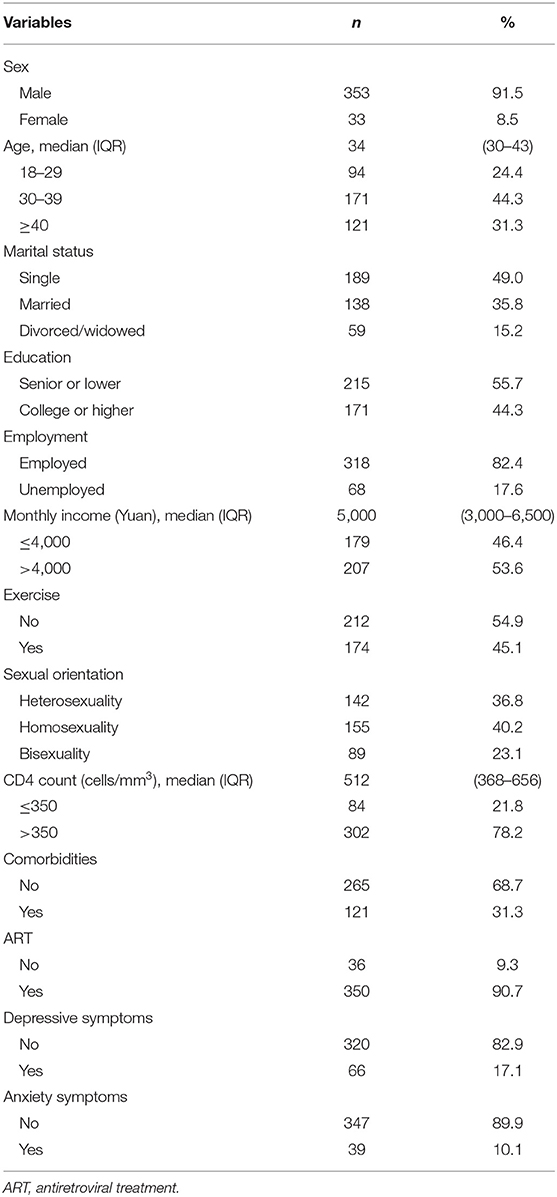
Of the 386 participants who completed the 5-year follow-up survey after diagnosis, 353 (91.5%) were male, with a median age of 34 (IQR: 30–43). The majority were single, employed, and had a monthly income of more than 4,000 Yuan. Nearly two-thirds of participants self-reported as homosexual or bisexual. The median CD4 counts 5 years after diagnosis were 512 cells/mm3 (IQR: 368–656). Over one-third of individuals reported the presence of other disease except for HIV infection (Table 1).
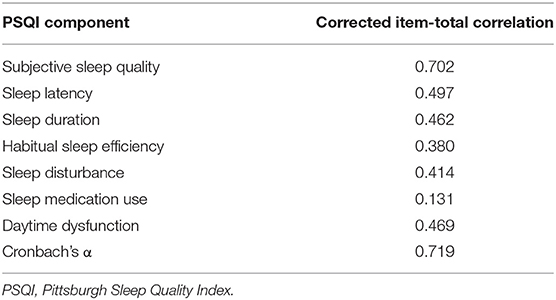
Reliability
The corrected item-total correlation ranged from 0.131 for the use of sleep medication component to 0.702 for the subjective sleep quality component. The overall Cronbach's α was 0.719 and increased to 0.734 after excluding the use of sleep medication component (Table 2).
Validity
Construct Validity
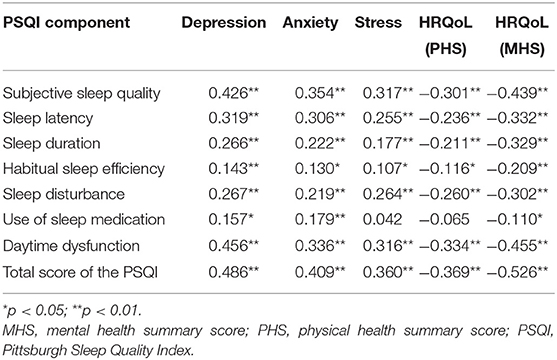
Correlations between the PSQI scores and relevant variables are presented in Table 3. Theoretical related constructs such as depression, anxiety, stress, and HRQoL were all significantly correlated with the total score of the PSQI (r ≥ |0.360|). Each component scores of the PSQI were significantly correlated with the depression, anxiety, and mental health summary scores of HRQoL (|r| = 0.110–0.526, p < 0.05). In addition, all components of the PSQI were correlated with the scores of stress the physical health summary scores of HRQoL (|r| = 0.107–0.369, p < 0.05), except for the component of sleeping medication use (|r| = 0.042–0.065, p > 0.05).
Known Group Validity
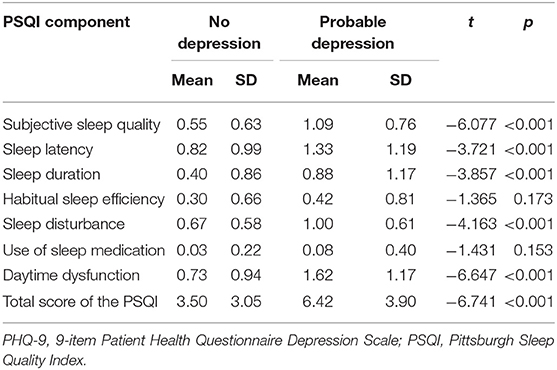
As hypothesized, the total score of the PSQI in individuals with probable depression (PHQ-9 ≥ 10, n = 66; mean = 6.42, SD = 3.90) was significantly higher than that in normal individuals with no depression (PHQ-9 <10, n = 320; mean = 3.50, SD = 3.50) with p < 0.001 (Table 4). All of the PSQI components, except for two components, sleep efficiency and use of sleep medication, were significantly correlated with the depression (p < 0.001).
Sleep Quality Among PLWH
Prevalence and Severity of Symptoms
The global PSQI score for the 386 participants ranged from 0 to 18, with a median of 3 (IQR: 1–6). The overall prevalence rate of poor sleep quality was 37.0%, using a cut-off point of 5, as suggested by Buysse et al. (12).
Factors Associated With Sleep Quality in PLWH
In the multivariate regression analysis, we found participants with less income (p = 0.002), CD4 >350 cells/mm3 (p = 0.024), ART initiation (p = 0.047), exercise behavior (p = 0.008), depressive symptoms (p = 0.006), and higher stress levels (p = 0.032) were more likely to experience sleep disturbances (Table 5).
Discussion
Although the PSQI has been frequently used in the studies of PLWH in China, the reliability and validity of the Chinese version in this population has yet to be examined. This is the first study to examine the psychometric efficiency of the PSQI among Chinese PLWH. We found that the Chinese version of the PSQI has adequate reliability and validity in PLWH. Over a third of PLWH reported sleep disturbances (defined as PSQI >5) in this study. Individuals who had a lower income, higher CD4 counts, ART initiation, exercise behavior, presence of depressive symptoms, and higher stress levels were more likely to experience sleep disturbances.
The reliability of PSQI in this study was supported by high internal consistency (Cronbach's α = 0.719), which was close to the result from studies by Buysse et al. (12). The component on sleep medication use had an item-total correlation <0.3 in this study, indicating poor correlations for this component in the PSQI framework. After deleting the component on sleep medication use, the Cronbach's α coefficient of PSQI increased from 0.719 to 0.734. Such a result is consistent with several published studies (28, 29). Of note, removing the medication use component was based on psychometrical methods, whereas the best possible psychometrics may not always be the highest consideration.
The validity of PSQI was supported by good construct validity and known-group validity. Significant correlations between PSQI and theoretical related constructs such as depression, anxiety, stress, and HRQoL were found in this study. In addition, the total score of PSQI in individuals with probable depression (PHQ-9 ≥ 10) was found to be significantly higher than that of individuals with no depression (PHQ-9 <10), compatible with our hypothesis that individuals with depression are more likely to experience poor sleep quality. The reliability and validity analyses of PSQI in this study suggest that the Chinese version of PSQI is a suitable and acceptable instrument for use in assessing sleep quality among Chinese PLWH.
Poor sleep quality was observed in 37% of participants in this study, which is much higher than that of the general population survey in China where the rate of sleep disturbances was found to be about 10% (30). This result, however, was lower than the rate of 43.1% reported by another study conducted among 4,103 HIV-infected individuals at 20 AIDS clinics across China (31). The different lengths of time since diagnosis may partially explain the discrepancy between the two studies. The median duration of diagnosis was 2.25 years in that study and 5 years in our sample, while the length of time since diagnosis has been associated with sleep disturbances, with shorter duration from diagnosis being associated with poor sleep quality (31). Nevertheless, the prevalence of sleep disturbances remains high even 5 years after diagnosis. Routinely assessing sleep quality over the course of the HIV infection should be taken into consideration. In accordance, identifying factors associated with sleep disturbances among PLWH is critical to inform strategies to improve sleep quality among this population.
In this study, PLWH on ART were more likely to report sleep disturbances. It is well-known that the morbidity and mortality rates among PLWH have declined dramatically with the scale-up of ART (32). However, side effects associated with ART have also been frequently reported by patients on ART, with sleep disturbances as a common side effect of treatment (33). A previous study investigating factors influencing adherence to ART mentioned that 56.4% of patients regarded insomnia as an adverse effect of ART, which further contribute to the non-adherence and discontinuation of treatment (34). Some antiretroviral medications (e.g., efavirenz) have been linked to adverse sleep effects, especially at higher plasma levels (35). Regularly monitoring adverse reactions to ART should be an important consideration in the management of HIV.
Our study found that individuals with higher CD4 counts (>350 cells/mm3) have a higher rate of sleep disturbances when compared with those with lower CD4 counts (≤ 350 cells/mm3). Conversely, findings from most HIV studies suggested higher CD4 counts were associated with better sleep quality (36, 37). It seems a more likely scenario as it would be expected that as patients decrease their viral load and improve their CD4 counts, their overall health would improve, together with sleep. However, a study in South Africa where 79% of the participants were women also reported a similar relationship between higher CD4 counts and poor sleep quality, arguing this may be related to an underlying immune activation (38). In addition, a cross-sectional study conducted in France found that patients with CD4 count <500 cells/mm3 were more likely to be long sleepers and less likely to experience insomnia. Insomnia and impaired sleep quality seem to be highly prevalent in well-controlled PLWH (39). Further investigation is needed to explore the relationship between CD4 counts and sleep quality.
5Poor immune function, serious symptoms, and antiretroviral side effects in the 1990s were broadly considered as the contributors of sleep disturbances in PLWH (40, 41), while even in the context of improved antiretroviral therapy and optimally controlled viral replication, PLWH still struggle with sleep disturbances, indicating that sleep disturbances among PLWH may be caused by additional factors related to psychosocial status other than HIV disease. Individuals would suffer from a myriad of stressors related to HIV after being diagnosed, such as disclosure concerns and infection-related stigma (2), which may make individuals with HIV infection be burdened further by depression and sleep disturbances (42, 43). Consistent with previous studies that depression is a major factor influencing sleep quality among PLWH (44, 45), we found that individuals with depression were more likely to experience sleep disturbances than those without. Considering the possible bidirectional association between sleep and depression (46), alleviating depressive symptoms among PLWH may improve sleep quality and vice versa.
In our study, less income was significantly associated with increased risk of sleep disturbances, and this variable is known to be an important factor associated with sleep whatever the medical condition (47). In addition, the beneficial effect of exercise on sleep has been commonly demonstrated among the general population or patients with other disease such as cancer survivors, and people with rheumatoid arthritis and mental illness (48–51), while less attention has been paid to PLWH. In this study, we found PLWH with exercise behavior were less likely to report sleep disturbances. Further research should investigate which type of exercise and exercise intensity is more effective for the sleep quality of PLWH.
Several limitations of this study should be acknowledged. First, consecutive sampling was used in this study to recruit participants, which may limit the generalizability of the findings. Second, other factors that may influence sleep quality were not included in this study, e.g., pain, alcohol assumption, smoking, and body mass index (BMI). These variables should be considered in future studies. Another limitation is that the sleep quality among PLWH in this study was based on one-time point assessment. Longitudinal studies tracking sleep disturbances among PLWH throughout the course of the disease could be valuable to characterize the impact of HIV infection on sleep.
Conclusions
The findings from this study supported the feasibility of the PSQI for use among Chinese PLWH. Over a third of PLWH reported sleep disturbances in this study, and participants with less income, higher CD4 counts, ART, exercise behavior, depressive symptoms, and higher stress levels were more likely to experience sleep disturbances. More attention should be given to the screening and treatment for sleep disturbances experienced by PLWH.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
This study was approved by the Ethics Committee of Xiangya School of Public Health Central South University (ZYGW-2018-055). Written informed consent was obtained from each participant before participation.
Author Contributions
D-QY: investigation, data curation, formal analysis, visualization, writing—original draft, writing—review and editing. Y-XH: investigation, data curation, formal analysis, visualization, writing—original draft, writing—review and editing, supervision. DL: conceptualization, methodology, project administration, funding acquisition, writing—review and editing, supervision. XC: methodology, writing—review, and editing. MW and JL: methodology, writing—review and editing. All authors contributed to the article and approved the submitted version.
Funding
This work was supported by the Natural Science Foundation of Hunan Province (2019JJ40401), Development and Reform Commission of Hunan Province ([2019]875), and the National Natural Science Foundation of China (81202290).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Martinez J, Lemos D, Hosek S. Stressors and sources of support: the perceptions and experiences of newly diagnosed Latino youth living with HIV. AIDS Patient Care STDS. (2012) 26:281–90. doi: 10.1089/apc.2011.0317
2. Huang Y, Luo D, Chen X, Zhang D, Huang Z, Xiao S. HIV-related stress experienced by newly diagnosed people living with HIV in China: a 1-year longitudinal study. Int J Environ Res Public Health. (2020) 17:2687. doi: 10.3390/ijerph17082681
3. Zimbardo PG, Pickren WE. The Psychology Journal: From Shamanism to Cutting-Edge Neuroscience, 250 Milestones in the History of Psychology (2014).
4. Littlewood D, Kyle SD, Pratt D, Peters S, Gooding P. Examining the role of psychological factors in the relationship between sleep problems and suicide. Clin Psychol Rev. (2017) 54:1–16. doi: 10.1016/j.cpr.2017.03.009
5. Wu J, Wu H, Lu C, Guo L, Li P. Self-reported sleep disturbances in HIV-infected people: a meta-analysis of prevalence and moderators. Sleep Med. (2015) 16:901–7. doi: 10.1016/j.sleep.2015.03.027
6. Phillips KD, Mock KS, Bopp CM, Dudgeon WA, Hand GA. Spiritual well-being, sleep disturbance, and mental and physical health status in HIV-infected individuals. Issues Ment Health Nurs. (2006) 27:125–39. doi: 10.1080/01612840500436917
7. Phillips KD, Moneyham L, Murdaugh C, Boyd MR, Tavakoli A, Jackson K, et al. Sleep disturbance and depression as barriers to adherence. Clin Nurs Res. (2005) 14:273–93. doi: 10.1177/1054773805275122
8. Gifford L, Bormann JE, Shively MJ, Wright BC, Richman DD, Bozzette SA. Predictors of self-reported adherence and plasma HIV concentrations in patients on multidrug antiretroviral regimens. J Acquir Immune Defic Syndr. (2000) 23:386–95. doi: 10.1097/00126334-200004150-00005
9. Paterson DL, Swindells S, Mohr J, Brester M, Vergis EN, Squier C, et al. Adherence to protease inhibitor therapy and outcomes in patients with HIV infection. Ann Intern Med. (2000) 133:21–30. doi: 10.7326/0003-4819-133-1-200007040-00004
10. Phillips KD, Sowell RL, Boyd M, Dudgeon WD, Hand GA. Sleep quality and health-related quality of life in HIV-infected African-American women of childbearing age. Qual Life Res. (2005) 14:959–70. doi: 10.1007/s11136-004-2574-0
11. Abad VC, Guilleminault C. Diagnosis and treatment of sleep disorders: a brief review for clinicians. Dialogues Clin Neurosci. (2003) 5:371–88. doi: 10.31887/DCNS.2003.5.4/vabad
12. Buysse DJ, Reynolds CF III, Monk TH, Berman SR, Kupfer DJ. The Pittsburgh Sleep Quality Index: a new instrument for psychiatric practice and research. Psychiatry Res. (1989) 28:193–213. doi: 10.1016/0165-1781(89)90047-4
13. Liu XC, Tang MQ. Reliability and validity of the Pittsburgh sleep quality index. Chinese J Psychiatry. (1996) 29:29103–7.
14. Zheng B, Li M, Wang KL, Lv J. Analysis of the reliability and validity of the Chinese version of Pittsburgh sleep quality index among medical college students. Beijing Da Xue Xue Bao Yi Xue Ban. (2016) 48:424–8.
15. Spira AP, Beaudreau SA, Stone KL, Kezirian EJ, Lui L-Y, Redline S, et al. Reliability and validity of the Pittsburgh sleep quality index in older adults in rural area. Modern Prevent Med. (2016) 43:1835–8.
16. Zhao X, Lan M, Li H, Yang J. Study on reliability and validity of Pittsburgh sleep quality index in civil servants of Tianjin. Tianjin Med J. (2012) 40:316–9. doi: 10.1016/j.sleep.2020.05.021
17. Niu L, Luo D, Chen X, Wang M, Zhou W, Zhang D, et al. Longitudinal trajectories of emotional problems and unmet mental health needs among people newly diagnosed with HIV in China. J Int AIDS Soc. (2019) 22:e25332. doi: 10.1002/jia2.25332
18. Kroenke K, Spitzer RL, Williams JB. The PHQ-9: validity of a brief depression severity measure. J Gen Intern Med. (2001) 16:606–13. doi: 10.1046/j.1525-1497.2001.016009606.x
19. Manea L, Gilbody S, McMillan D. A diagnostic meta-analysis of the Patient Health Questionnaire-9 (PHQ-9) algorithm scoring method as a screen for depression. Gen Hosp Psychiatry. (2015) 37:67–75. doi: 10.1016/j.genhosppsych.2014.09.009
20. Wang W, Bian Q, Zhao Y, Li X, Wang W, Du J, et al. Reliability and validity of the Chinese version of the Patient Health Questionnaire (PHQ-9) in the general population. Gen Hosp Psychiatry. (2014) 36:539–44. doi: 10.1016/j.genhosppsych.2014.05.021
21. Spitzer RL, Kroenke K, Williams JB, Lowe B. A brief measure for assessing generalized anxiety disorder: the GAD-7. Arch Intern Med. (2006) 166:1092–7. doi: 10.1001/archinte.166.10.1092
22. Tong X, An D, McGonigal A, Park SP, Zhou D. Validation of the generalized anxiety disorder-7 (GAD-7) among Chinese people with epilepsy. Epilepsy Res. (2016) 120:31–6. doi: 10.1016/j.eplepsyres.2015.11.019
23. Niu L, Qiu Y, Luo D, Chen X, Wang M, Pakenham KI, et al. Cross-culture validation of the HIV/AIDS Stress Scale: the development of a revised Chinese version. PLoS ONE. (2016) 11:e0152990. doi: 10.1371/journal.pone.0152990
24. Pakenham K, Rinaldis M. Development of the HIV/AIDS Stress Scale. Psychol Health. (2002) 17:203–19. doi: 10.1080/08870440290013680
25. Wu W, Revicki DA, Jacobson D, Malitz FE. Evidence for reliability, validity and usefulness of the Medical Outcomes Study HIV Health Survey (MOS-HIV). Qual Life Res. (1997) 6:481–93. doi: 10.1023/a:1018451930750
26. Huang ZJ, Tian M, Dai SY, Ye DQ. Feasibility, reliability and validity of the Chinese simplified version of the MOS-HIV health survey among AIDS patients in China. Qual Life Res. (2013) 22:403–7. doi: 10.1007/s11136-012-0148-0
27. Cho E, Kim S. Cronbach's coefficient alpha: well-known but poorly understood. Organ Res Methods. (2015) 18:207–30. doi: 10.1177/1094428114555994
28. Zhang C, Zhang H, Zhao M, Li Z, Cook CE, Buysse DJ, et al. Reliability, validity, and factor structure of pittsburgh sleep quality index in community-based centenarians. Front Psychiatry. (2020) 11:573530. doi: 10.3389/fpsyt.2020.573530
29. Spira P, Beaudreau SA, Stone KL, Kezirian EJ, Lui LY, Redline S, et al. Reliability and validity of the Pittsburgh Sleep Quality Index and the Epworth Sleepiness Scale in older men. J Gerontol A Biol Sci Med Sci. (2012) 67:433–9. doi: 10.1093/gerona/glr172
30. Xiang YT, Ma X, Cai ZJ, Li SR, Xiang YQ, Guo HL, et al. The prevalence of insomnia, its socio-demographic and clinical correlates, and treatment in rural and urban regions of Beijing, China: a general population-based survey. Sleep. (2008) 31:1655–62. doi: 10.1093/sleep/31.12.1655
31. Huang X, Li H, Meyers K, Xia W, Meng Z, Li C, et al. Burden of sleep disturbances and associated risk factors: a cross-sectional survey among HIV-infected persons on antiretroviral therapy across China. Sci Rep. (2017) 7:3657. doi: 10.1038/s41598-017-03968-3
32. Michaels SH, Clark R, Kissinger P. Declining morbidity and mortality among patients with advanced human immunodeficiency virus infection. N Engl J Med. (1998) 339:405–6. doi: 10.1056/NEJM199808063390612
33. Clifford DB, Evans S, Yang Y, Acosta EP, Ribaudo H, Gulick RM. Long-term impact of efavirenz on neuropsychological performance and symptoms in HIV-infected individuals (ACTG 5097s). HIV Clin Trials. (2009) 10:343–55. doi: 10.1310/hct1006-343
34. Naidoo P. Factors influencing HAART adherence among private health care sector patients in a suburb of the Ethekwini Metro. Afr J Prim Health Care Fam Med. (2009) 1:12. doi: 10.4102/phcfm.v1i1.12
35. Gallego L, Barreiro P, Del RR, Gonzalez DRD, Rodriguez-Albarino A, Gonzalez-Lahoz J, et al. Analyzing sleep abnormalities in HIV-infected patients treated with Efavirenz. Clin Infect Dis. (2004) 38:430–2. doi: 10.1086/380791
36. Oshinaike O, Akinbami A, Ojelabi O, Dada A, Dosunmu A, John OS. Quality of sleep in an HIV population on Antiretroviral Therapy at an Urban Tertiary Centre in Lagos, Nigeria. Neurol Res Int. (2014) 2014:298703. doi: 10.1155/2014/298703
37. Seay JS, McIntosh R, Fekete EM, Fletcher MA, Kumar M, Schneiderman N, et al. Self-reported sleep disturbance is associated with lower CD4 count and 24-h urinary dopamine levels in ethnic minority women living with HIV. Psychoneuroendocrino. (2013) 38:2647–53. doi: 10.1016/j.psyneuen.2013.06.022
38. Redman KN, Karstaedt AS, Scheuermaier K. Increased CD4 counts, pain and depression are correlates of lower sleep quality in treated HIV positive patients with low baseline CD4 counts. Brain Behav Immun. (2018) 69:548–55. doi: 10.1016/j.bbi.2018.02.002
39. Faraut B, Malmartel A, Ghosn J, Duracinsky M, Leger D, Grabar S, et al. Sleep disturbance and total sleep time in persons living with HIV: a cross-sectional study. AIDS Behav. (2018) 22:2877–87. doi: 10.1007/s10461-018-2179-1
40. Norman SE, Chediak AD, Kiel M, Cohn MA. Sleep disturbances in HIV-infected homosexual men. AIDS. (1990) 4:775–81. doi: 10.1097/00002030-199008000-00009
41. Grandner MA, Patel NP, Gehrman PR, Xie D, Sha D, Weaver T, et al. Who gets the best sleep? Ethnic and socioeconomic factors related to sleep complaints. Sleep Med. (2010) 11:470–8. doi: 10.1016/j.sleep.2009.10.006
42. Garrido-Hernansaiz H, Alonso-Tapia J. Associations among resilience, posttraumatic growth, anxiety, and depression and their prediction from stress in newly diagnosed people living with HIV. J Assoc Nurses AIDS Care. (2017) 28:289–94. doi: 10.1016/j.jana.2016.12.005
43. Vosvick M, Gore-Felton C, Ashton E, Koopman C, Fluery T, Israelski D, et al. Sleep disturbances among HIV-positive adults. J Psychosom Res. (2004) 57:459–63. doi: 10.1016/j.jpsychores.2004.03.003
44. Ren J, Zhao M, Liu B, Wu Q, Hao Y, Jiao M, et al. Factors associated with sleep quality in HIV. J Assoc Nurses AIDS Care. (2018) 29:924–31. doi: 10.1016/j.jana.2018.04.006
45. Allavena C, Guimard T, Billaud E, De la Tullaye S, Reliquet V, Pineau S, et al. Prevalence and risk factors of sleep disturbance in a large HIV-infected adult population. AIDS Behav. (2016) 20:339–44. doi: 10.1007/s10461-015-1160-5
46. Ford DE, Kamerow DB. Epidemiologic study of sleep disturbances and psychiatric disorders. An opportunity for prevention? JAMA. (1989) 262:1479–84. doi: 10.1001/jama.1989.03430110069030
47. Stamatakis KA, Kaplan GA, Roberts RE. Short sleep duration across income, education, and race/ethnic groups: population prevalence and growing disparities during 34 years of follow-up. Ann Epidemiol. (2007) 17:948–55. doi: 10.1016/j.annepidem.2007.07.096
48. Bennie JA, De Cocker K, Duncan MJ. Associations of muscle-strengthening and aerobic exercise with self-reported components of sleep health among a nationally representative sample of 47,564 US adults. Sleep Health. (2021) 7:281–8. doi: 10.1016/j.sleh.2020.08.004
49. Lederman O, Ward PB, Firth J, Maloney C, Carney R, Vancampfort D, et al. Does exercise improve sleep quality in individuals with mental illness? A systematic review and meta-analysis. J Psychiatr Res. (2019) 109:96–106. doi: 10.1016/j.jpsychires.2018.11.004
50. Hidde MC, Leach HJ, Marker RJ, Peters JC, Purcell WT. Effects of a clinic-based exercise program on sleep disturbance among cancer survivors. Integr Cancer Ther. (2020) 19:1534735420975852. doi: 10.1177/1534735420975852
Keywords: pittsburgh sleep quality index, reliability, validity, HIV, sleep disturbances, China
Citation: Yan D-Q, Huang Y-X, Chen X, Wang M, Li J and Luo D (2021) Application of the Chinese Version of the Pittsburgh Sleep Quality Index in People Living With HIV: Preliminary Reliability and Validity. Front. Psychiatry 12:676022. doi: 10.3389/fpsyt.2021.676022
Received: 04 March 2021; Accepted: 24 May 2021;
Published: 06 July 2021.
Edited by:
Seog Ju Kim, Sungkyunkwan University, South KoreaReviewed by:
Daniela Adamo, University of Naples Federico II, ItalyLorenzo Tonetti, University of Bologna, Italy
Copyright © 2021 Yan, Huang, Chen, Wang, Li and Luo. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Dan Luo, luodan_csu_2011@126.com
†These authors have contributed equally to this work
 Dong-Qin Yan
Dong-Qin Yan Yun-Xiang Huang1,2†
Yun-Xiang Huang1,2† Min Wang
Min Wang Dan Luo
Dan Luo