- 1BrainPark, Turner Institute for Brain and Mental Health, Monash University, Clayton, VIC, Australia
- 2Monash Business School, Monash University, Caulfield, VIC, Australia
- 3Department of Psychiatry, University of Southampton, Southampton, United Kingdom
- 4Department of Psychiatry and Behavioral Neuroscience, University of Chicago, Chicago, IL, United States
- 5Obsessive, Compulsive, and Anxiety Spectrum Research Program, Institute of Psychiatry, Federal University of Rio de Janeiro (UFRJ), D'Or Institute for Research and Education (IDOR), Rio de Janeiro, Brazil
- 6D'Or Institute for Research and Education, Rio de Janeiro, Brazil
Background: The COVID-19 pandemic has resulted in high levels of psychological distress worldwide, with experts expressing concern that this could result in corresponding increases in addictive behaviors as individuals seek to cope with their distress. Further, some individuals may be at greater risk than others for developing problematic addictive behaviors during times of high stress, such as individuals with high trait impulsivity and compulsivity. Despite the potential of such knowledge to inform early detection of risk, no study to date has examined the influence of trait impulsivity and compulsivity on addictive behaviors during COVID-19. Toward this aim, the current study examined the association between impulsive and compulsive traits and problematic addictive and compulsive behaviors during the first COVID-19 lockdown in Australia.
Methods: Eight hundred seventy-eight adults completed a cross-sectional online survey during the first lockdown, between late May to June 2020. Participants completed scales for addictive and compulsive behaviors for the period prior to and during lockdown for problematic eating, pornography, internet use, gambling, drinking, and obsessive-compulsive behaviors. Negative binomial regressions examined the associations between impulsivity, compulsivity, and their interaction with problematic behaviors during lockdown, controlling for age, gender, sample, psychological distress, exposure to COVID-related stressors, and pre-COVID problems.
Results: Greater trait compulsivity was associated with more problematic obsessive-compulsive behaviors (p < 0.001) and less problematic drinking (p = 0.038) during lockdown. Further, trait compulsivity interacted with trait impulsivity in relation to problematic eating behaviors (p = 0.014) such that greater trait compulsivity was associated with more problems among individuals with low impulsivity only (p = 0.030). Finally, psychological distress and/or exposure to COVID-related stressors were associated with greater problems across all addictive and compulsive behaviors, as was severity of pre-COVID problems.
Discussion: Trait compulsivity was associated with addictive and compulsive behaviors in different ways. Further, the finding that stress-related variables (psychological distress and COVID-related stressors) were associated with greater problems across all lockdown behaviors supports the idea that stress may facilitate, or otherwise be associated with, problematic behaviors. These findings highlight the need for interventions that enhance resilience to stress, which in turn may reduce risk for addictive and compulsive disorders.
Introduction
Stress is a well-known risk factor across addictive and compulsive behaviors (1, 2). This knowledge has led to the general expectation that such behaviors will increase during the COVID-19 pandemic (3–6), considered a stressful time worldwide due to health and financial concerns, lockdown-related social isolation, and life disruption. While studies suggest that some addictive and compulsive behaviors may have increased during COVID-19, including problematic internet use (7), drinking (8), and obsessive-compulsive behaviors (9), this has not been the case across the board. Particularly, reports of gambling-related harm suggest a decrease during lockdown (10, 11), and there have been mixed findings for obsessive-compulsive behaviors [e.g., (12)]. An emerging body of research suggests that lockdown-related changes in addictive and compulsive behaviors may be predicted by, or otherwise related to, behavior-specific factors, such as motives [e.g., (13)] and pre-existing severity (6, 10, 14). However, individual characteristics also play a role [e.g., (15)]. This pattern of findings is not unique to COVID-19; there is a wealth of past research showing that while stressful life events generally increase risk for addictive and compulsive behaviors (16–19), the extent to which they do is influenced by individual differences (20–22). As such, COVID-19 provides an invaluable context within which to better understand (and thereby address) individual-level risk factors for psychopathology.
It is generally accepted that, at least under non-pandemic circumstances, trait impulsivity is associated with risk across the spectrum of addictive and compulsive disorders (23–31). Briefly, impulsivity refers to the tendency to act without thinking, especially when the consequences of such action are inappropriate to the situation (32, 33). There is a large body of evidence showing that greater trait impulsivity is associated with more problematic addictive and compulsive behaviors, including for alcohol use, gambling, internet use, binge eating, pornography, as well as obsessive-compulsive behaviors (24, 30, 34–40). Another risk factor for addictive and compulsive behaviors is compulsivity, that is, the tendency to engage in repetitive, habitual behaviors that are difficult to control or interfere with current goals (27, 41–46). Indeed, higher levels of trait compulsivity have been found to be associated with addictive and compulsive behaviors, including problematic alcohol use, internet use, binge eating, gambling, and obsessive-compulsive behaviors (35, 37, 46, 47). Further, research suggests that impulsivity and compulsivity may interact such that individuals with high levels on both compulsive and impulsive traits are at greatest risk of problematic impulsive-compulsive behaviors (23, 29, 35). For instance, individuals characterized by high impulsivity and high compulsivity have been shown to have more severe obsessive-compulsive symptoms (29) and problematic eating (48). Similarly, this interaction is seen at the cognitive level, with higher levels of both impulsive and compulsive cognitive traits being associated with more problematic alcohol use and obsessive-compulsive behaviors (35).
Arguably, this risk profile (high impulsivity, high compulsivity) might contribute to more problematic addictive and compulsive behaviors during lockdown. For instance, while individuals with high impulsivity and low compulsivity might engage in impulsive behaviors during lockdown, they would not engage in the same impulsive behavior routinely. On the other hand, individuals with high compulsivity and low impulsivity might engage in certain behaviors routinely during lockdown but might be able to inhibit these newly adopted routine behaviors should they become maladaptive. However, when these traits are combined, an individual might engage in routine coping behaviors (due to compulsive tendencies) and have difficulty inhibiting these behaviors if they become maladaptive (due to the impaired response inhibition that characterizes impulsivity). Thus, individuals with high compulsivity and high impulsivity may be at greater risk of developing persistent, maladaptive coping behaviors during the current pandemic. This risk may further increase with time, as impulsive behaviors become coping strategies (through reinforcement) and routine behaviors become habits. Intervening early in the course of impulsive-compulsive behaviors, before behaviors become entrenched, is critical to curtailing progression to addictive and compulsive disorders (44).
Early detection of risk for impulsive-compulsive disorders may be especially important during the current pandemic as problematic behaviors may become entrenched more quickly under times of high stress. Specifically, stress may facilitate progression toward problematic compulsive behaviors by promoting a shift toward habit learning and/or otherwise supporting the maladaptive expression of learned behaviors (44, 49–54). Through facilitating these mechanisms, stress may effectively shorten the window of time that a behavioral pattern is malleable. Thus, early detection of risk during COVID-19 (a stressful period for many) is critical to enabling timely access to interventions, before addictive and compulsive behaviors become harder to modify. The current study therefore aimed to examine the potential of trait compulsivity and impulsivity as risk markers for problematic addictive and compulsive behaviors during the first lockdown of COVID-19. Specifically, this study examined the associations between trait compulsivity, impulsivity, and their interaction on problematic internet use, drinking, eating, pornography use, gambling, and obsessive-compulsive behaviors during COVID-19. Obsessive-compulsive behaviors were examined alongside addictive behaviors in line with transdiagnostic models of compulsive behaviors (42, 44, 55), as well as the recent conceptualization of OCD as a behavioral addiction (56). In line with the idea that impulsive and compulsive traits may pre-dispose individuals to developing problematic behaviors, especially during times of high stress, we hypothesized that impulsivity and compulsivity would interact in relation to problematic behaviors during lockdown. Specifically, we hypothesized that individuals with high compulsivity and high impulsivity would report the greatest increases in addictive and compulsive behaviors during lockdown.
Method
Participants
Participants included in the study were 992 adults (18 years and above). The current analyses exclude participants who did not complete all the general study measures (trait impulsivity and compulsivity, COVID events, and psychological distress), which were 114 in total. Thus, the resulting study sample includes 878 participants. Participants were recruited through two methods: (1) general advertisements on Facebook, twitter, and other social media platforms, and reimbursement was entry into a draw to win one of 50 $100 JB HiFi vouchers, and (2) Prolific online participant recruitment platform targeting individuals residing in Australia, and reimbursement was £7.50 per hour. The current study includes 214 community participants and 664 prolific participants.
All study procedures were carried out in accordance with the Declaration of Helsinki. The Monash University Human Research Ethics Committee ethically reviewed and approved the study.
Measures
Demographic information such as age and gender was collected, and participants completed the following questionnaires:
Short UPPS-P Impulsivity Scale [S-UPPS-P; (57)]: This is a 20-item scale that measures impulsivity traits with five subscales: Negative Urgency, the tendency toward impulsive action when experiencing strong negative emotions (e.g., “When I am upset, I often act without thinking”); Positive Urgency, the tendency toward impulsive action when experiencing strong positive emotions; Lack of Perseverance; Lack of Premeditation; and Sensation Seeking. For each item, participants selected whether the extent to which they agreed or disagreed with statements describing ways in which people act and think (generally, i.e., no timeframe was specified). Response options were “strongly disagree,” “disagree somewhat,” “agree somewhat,” or “strongly agree,” scored as 1–4, respectively (or 4–1 for reverse items). The present study used total S-UPPS-P score as the measure of interest.
The Cambridge-Chicago Compulsivity Trait Scale [CHI-T; (47)]. This is a 15-item scale covering broad aspects of compulsivity including the need for completion or perfection, being stuck in a habit, reward-seeking, desire for high standards, and avoidance of situations that are hard to control. For each item, participants selected whether the statement applied to them (generally, i.e., no timeframe was specified) by selecting “strongly disagree,” “disagree,” “agree,” or “strongly agree,” scored as 0–3, respectively. The measure of interest was the total score.
COVID-related events: An 8-item checklist of COVID-related events was used to gauge exposure to stressors from the start of the pandemic. These eight items were taken from a measure of potentially stressful COVID-related events [COROTRAS; (58, 59)]. Specifically, these items asked about worsening of financial situation; reduced time in paid employment; being diagnosed with COVID-19; having a family member or significant other diagnosed with COVID-19; having experienced a cough or fever during the pandemic; being kept away from home (in another state or country) because of COVID-19; having family member or significant other share space with a suspected or confirmed case of COVID-19 or being in a position where they are exposed to lots of people; and having to work or be exposed against your wishes to any activity associated with a high risk of contracting COVID-19. The measure was in the form of a checklist (with a score of 1 given for each event experienced) the total score was used in the present study (i.e., total number of events experienced).
K10 (60): This is a 10-item scale designed to measure past month psychological distress. Each item is rated on a 5-point scale as follows: None of the time (1); A little of the time (2); Some of the time (3); Most of the time (4); or All of the time (5). The measure of interest was the total score. We adjusted for psychological distress given research showing that it is associated with increases in addictive behaviors during COVID-19 (61) as well as its elevation during COVID-19 (62, 63). The total score was used in the present study.
Problematic Behavior Scales
Modified Yale Food Addiction Scale 2.0 [mYFAS2.0; (64)]: This scale is a 13-item scale designed to measure addiction-like eating behaviors in accordance with the DSM5 diagnostic criteria for addictive disorders, with additional items asking about distress and interference as a result of the eating behaviors. All participants completed the mYFAS 2.0. The scale was modified to cover a month timeframe and response options were modified as follows: Never (1); 1–3 times/month (2); 1–3 times/week; (3); 4+ times/week (4). Further, each scale item was asked in relation to both (a) the month prior to the onset of the first COVID-19 restrictions and (b) the past month, during COVID-19 restrictions. The current study used total scores for each timeframe (pre-COVID and lockdown) as the measures of interest.
Young's Internet Addiction Test, Short Version [IAT; (65)]: This is a 12-item version of Young's IAT developed to measure Problematic Usage of the Internet. Only participants who reported excessive use of the internet in the past 3 months were asked to complete the IAT. Each scale item was asked in relation to both (a) the month prior to the onset of the first COVID-19 restrictions and (b) the past month, during COVID-19 restrictions. Item response options were as follows: Never (0); Rarely (1); Sometimes; (2); Often (3); and Very often (4). The current study used total scores for each timeframe (pre-COVID and lockdown) as the measures of interest.
Short Version of the Problematic Pornography Consumption Scale [PPCS-6; (40)]: This is a 6-item scale designed to measure problematic pornography use. Only participants who reported watching pornography in the past 3 months were asked to complete the PPCS-6. Each scale item was asked in relation to both (a) the month prior to the onset of the first COVID-19 restrictions and (b) the past month, during COVID-19 restrictions. Item response options were as follows: Never (1); Sometimes; (2); Often (3); and Very often (4). The current study used total scores for each timeframe (pre-COVID and lockdown) as the measures of interest.
Problem Gambling Severity Index [PGSI; derived from the 31-item Canadian Problem Gambling Index, (66)]. This is a 9-item measure of gambling harm severity. Only participants who reported gambling in the past 3 months were asked to complete the PGSI. Each scale item was asked in relation to both (a) the month prior to the onset of the first COVID-19 restrictions and (b) the past month, during COVID-19 restrictions. Item response options were as follows: Never (0); Sometimes; (1); Almost always (2); and Always (3). The current study used total scores for each timeframe (pre-COVID and lockdown) as the measures of interest.
Alcohol Use Disorders Identification Test [AUDIT; (67)]. The AUDIT is a 10-item self-report measure that assesses hazardous/risky alcohol consumption. Only participants who reported drinking in the past 3 months were asked to complete the AUDIT. Each scale item was asked in relation to both (a) the month prior to the onset of the first COVID-19 restrictions and (b) the past month, during COVID-19 restrictions. Response options were modified to suit the 1-month timeframe needed for the current study. For questions 1, response options were: Never (0); Once a month (1); 2–4 times/month (2); 2–3 times/week (3); 4+ times/week. For questions 3–8, response options were: Never (0); Monthly (1); Weekly (2); Daily or almost daily (3). For questions 9 and 10, participants were asked to answer yes (2) or no (0) in relation to the timeframe in question. The current study used total scores for each timeframe (pre-COVID and lockdown) as the measures of interest.
Obsessive-Compulsive Inventory Revised [OCI-R; (68)]. This is an 18-item scale enquiring about OC-related experiences. All participants were asked to complete the OCI-R. Each scale item was asked in relation to both (a) the month prior to the onset of the first COVID-19 restrictions and (b) the past month, during COVID-19 restrictions. For each scale item the individual rated how distressed or bothered they had been by this over the specified timeframe, with response options as follows: Not at all (0), A little (1), Moderately (2), A lot (3), or Extremely (4). The current study used total scores for each timeframe (pre-COVID and lockdown) as the measures of interest.
Statistical Analyses
The data were examined for outliers (based on Z scores >3.29), which were then winsorized. Descriptive statistics compared pre-COVID to lockdown problematic behaviors using Wilcoxon Signed Ranks Test (Table 1), and examined correlations across compulsivity, impulsivity, and all problematic behaviors during lockdown (Table 2). Six negative binomial regressions examined whether trait impulsivity (S-UPPS-P score), trait compulsivity (CHIT score), and their interaction were associated with each of the following problematic behaviors during lockdown; eating, internet use, pornography use, drinking, gambling, and obsessive-compulsive behaviors. Compulsivity scores and impulsivity scores were mean-centered according to the respective outcome group, and interaction terms calculated accordingly. All regression models adjusted for corresponding pre-COVID problematic behavior score, age, gender, sample, COVID-related events, and psychological distress (K10).
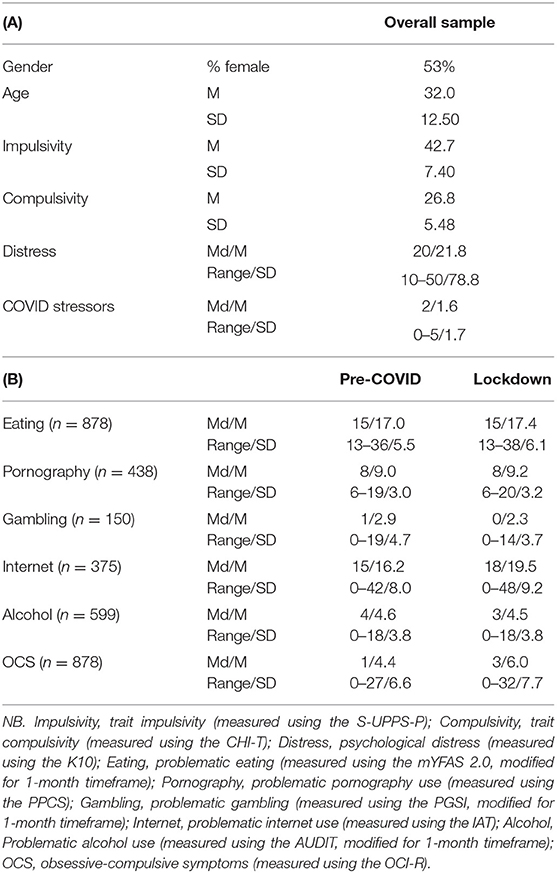
Table 1. (A) Sample descriptives (N = 878) and (B) Pre-COVID and lockdown problematic behavior scale scores.
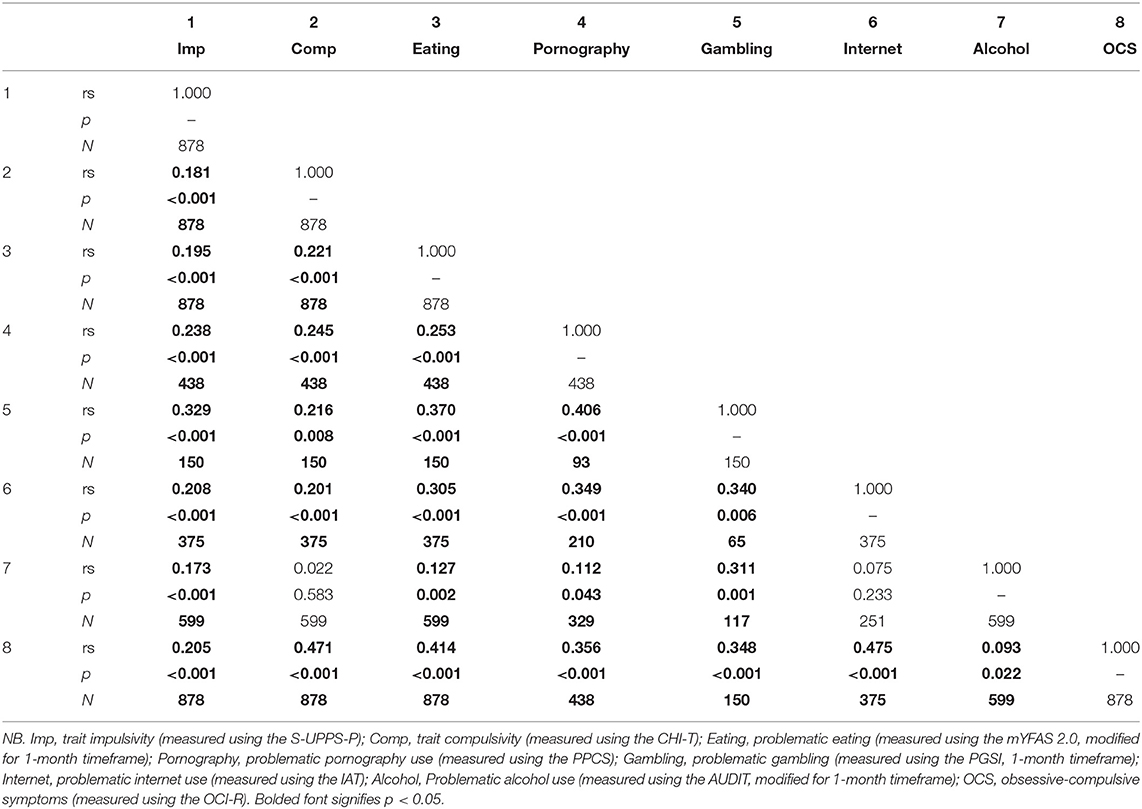
Table 2. Spearman's correlation across impulsivity, compulsivity, and problematic behaviors during lockdown.
Significant and trend-level interactions were followed up by dividing the sample into high and low trait impulsivity groups (by median split, according to corresponding outcome group) and running a negative binomial regression with trait compulsivity as the predictor, lockdown score of behavior in question as the dependent variable, and adjusting for the pre-COVID scale score.
Further, to provide an illustration of significant interactions, we graphed change scores (calculated as lockdown minus pre-COVID score) by high and low impulsivity and compulsivity groups (median split). This is shown in the Supplementary Figure 1. Finally, to support interpretation of study findings, pre-COVID behaviors were analyzed to examine their relationship with trait impulsivity and compulsivity. These analyses are also presented in the Supplementary Materials.
Results
Participants were 878 adults (466 females; age M = 32.0 years, SD = 12.5, range 18–84). Prolific participants were younger than community participants [mean diff. = 2.5, t(876) = 2.5, p = 0.012]. The community sample had relatively more females (71 vs. 47%) than the prolific sample, X2 = 36.6, p < 0.001. The community sample also reported higher lockdown obsessive-compulsive symptoms scores than the prolific sample, Z = −2.5, p = 0.012. No other differences were found between the two samples.
As shown in Table 1, problematic internet use, Z = 12.0, p < 0.001, dCohen = 0.98, pornography use, Z = 3.5, p < 0.001, dCohen = 0.24, eating, Z = 5.5, p < 0.001, dCohen = 0.27, and obsessive-compulsive symptoms, Z = 15.0, p < 0.001, dCohen = 0.77, increased from pre-COVID to lockdown. In contrast, problematic gambling score decreased from pre-COVID to lockdown, Z = −2.6, p = 0.011, dCohen = 0.30. No differences were found for problematic drinking. As shown in Table 2, trait compulsivity and impulsivity were significantly correlated with all lockdown behaviors, except for problematic drinking, which did not show a significant correlation with trait compulsivity.
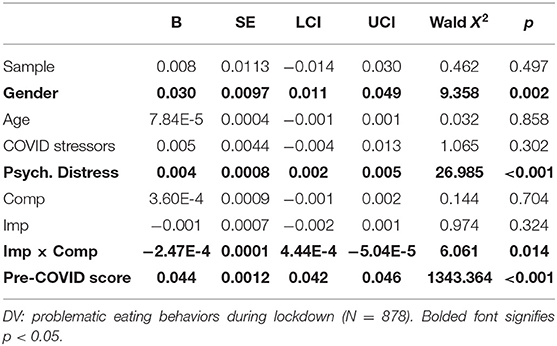
Problematic Eating During Lockdown
Results of the regression on lockdown problematic eating are shown in Table 3. Female gender was associated with increased problematic eating during lockdown (Wald X2 = 9.7, p = 0.002), as was greater psychological distress (Wald X2 = 27.0, p < 0.001), and higher pre-COVID problematic eating score (Wald X2 = 1,343.4, p < 0.001). The interaction between trait compulsivity and impulsivity was also significant (Wald X2 = 6.3, p = 0.014). Follow-up of this interaction found that while the association between compulsivity scores and lockdown eating was significant for the low impulsivity group (Wald X2 = 4.7, p = 0.030, n = 423), it was not significant in the high impulsivity group (Wald X2 = 0.61, p = 0.434, n = 455). Supplementary Figure 1 shows change scores (calculated as lockdown minus pre-COVID score) by high and low impulsivity and compulsivity groups (median split), to aid interpretation of the above interaction.
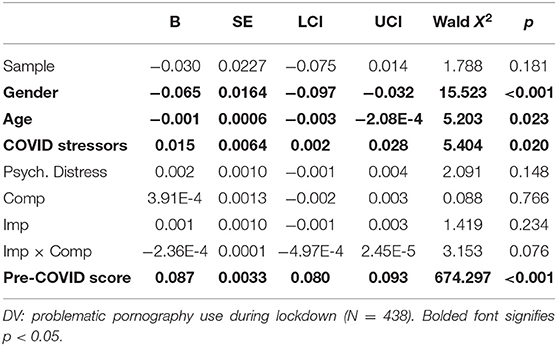
Problematic Pornography Use During Lockdown
Results of the regression on lockdown problematic pornography use are shown in Table 4. Female gender was associated with lower lockdown problematic pornography use (Wald X2 = 15.5, p < 0.001). Younger age (Wald X2 = 5.2, p = 0.023), a higher number of COVID events (Wald X2 = 5.4, p = 0.020), and greater pre-COVID problematic pornography use (Wald X2 = 674.3, p < 0.001) were associated with higher lockdown problematic pornography use. Finally, there was a trend-level interaction (Wald X2 = 3.2, p = 0.076), which follow-up analyses revealed was driven by a trend-level association between compulsivity and lockdown pornography use in the low impulsivity group (Wald X2 = 3.2, p = 0.072, n = 224) which was not seen in the high impulsivity group (Wald X2 = 0.48, p = 0.488, n = 214).
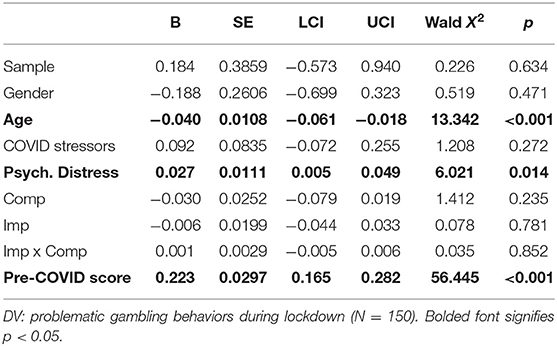
Problematic Gambling During Lockdown
Results of the regression on lockdown problematic gambling scores are shown in Table 5. Younger age (Wald X2 = 13.3, p < 0.001), greater psychological distress (Wald X2 = 6.0, p = 0.014), and greater pre-COVID problematic gambling (Wald X2 = 56.4, p < 0.001) were associated with more problematic gambling during lockdown.
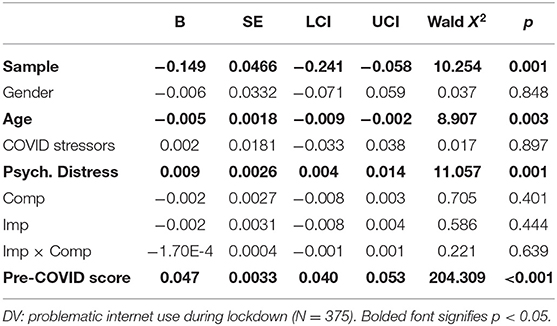
Problematic Internet Use During Lockdown
Results of the regression on lockdown problematic internet use are shown in Table 6. Younger age (Wald X2 = 8.9, p = 0.003), community sample status (Wald X2 = 10.3, p = 0.001), greater K10 (Wald X2 = 11.1, p = 0.001), and greater pre-COVID problematic internet use (Wald X2 = 204.3, p < 0.001), were associated with more problematic internet use during lockdown.
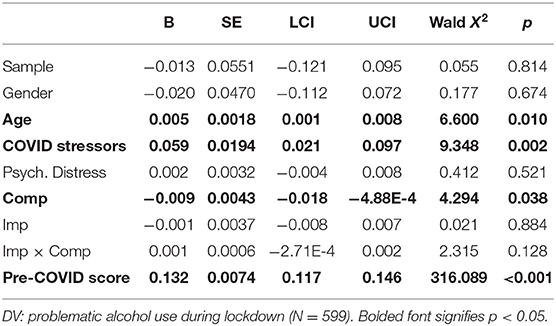
Problematic Drinking During Lockdown
Results of the regression on lockdown problematic drinking scores are shown in Table 7. Older age (Wald X2 = 6.6, p = 0.010), greater COVID-related events (Wald X2 = 9.3, p = 0.002), lower trait compulsivity (Wald X2 = 4.3, p = 0.038), and greater pre-COVID drinking problems (Wald X2 = 316.1, p < 0.001) were associated with more problematic drinking during lockdown.
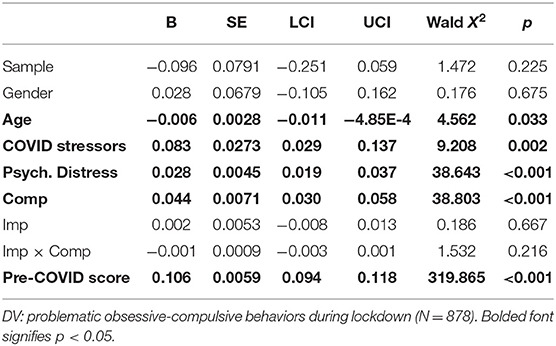
Problematic Obsessive-Compulsive Behaviors During Lockdown
Results of the regression on problematic obsessive-compulsive behaviors during lockdown are shown in Table 8. Younger age (Wald X2 = 4.5, p = 0.033), greater COVID-related events (Wald X2 =9.2, p = 0.002), greater psychological distress (Wald X2 = 38.6, p < 0.001), greater trait compulsivity (Wald X2 = 38.8, p < 0.001), and greater pre-COVD obsessive-compulsive behaviors (Wald X2 = 319.9, p < 0.001) were associated with more problematic obsessive-compulsive behaviors during lockdown.
Supplementary Analyses on Pre-COVID Problematic Behaviors
Higher trait impulsivity and/or compulsivity, or their interaction were significantly associated with all pre-COVID problematic behaviors. Please see Supplementary Materials for details.
Discussion
The current study examined whether two transdiagnostic risk factors, trait impulsivity and compulsivity, and their interaction, were associated with problematic addictive and compulsive behaviors during lockdown. First, the current study found that participants reported increased problematic behaviors during lockdown, compared to pre-COVID levels, except for alcohol use and gambling. In fact, participants reported reduced gambling during lockdown. However, with the exception of reported changes (from pre-COVID to lockdown) in obsessive-compulsive symptoms and internet use, which were large in effect size, reported changes in problematic behaviors were small in effect size. Second, trait impulsivity and compulsivity were significantly correlated with all lockdown problematic behaviors (except compulsivity with alcohol use). These correlations were small to medium in effect size and generally in line with past research in non-clinical populations (35, 36, 38). However, these relationships changed considerably once examined within regression models, which controlled for pre-COVID levels of problematic behaviors. These analyses found that greater trait compulsivity was associated with greater lockdown obsessive-compulsive behaviors, as well as lower levels of lockdown problematic drinking. Further, trait compulsivity interacted with impulsivity in relation to problematic eating and (at trend level) pornography use. Follow-up of these interactions found that greater trait compulsivity was associated with greater problematic eating and (at trend-level) pornography use during lockdown among individuals with low trait impulsivity only. It must be noted however that the effect sizes of these interactions are very small, as may be seen from Tables 3, 4 (interaction term Bs). Psychological distress and/or exposure to COVID-related stressors were associated with greater problems across all addictive and compulsive lockdown behaviors as were pre-COVID levels of the behavior in question.
The finding that greater trait compulsivity was associated with more problematic obsessive-compulsive behaviors during lockdown, after adjusting for psychological distress, COVID-related stressors, and pre-COVID obsessive-compulsive behaviors highlights its role as a key risk marker for OCD. While the nature of its role in driving risk has yet to be identified, the current findings suggest that these traits, or what they reflect, interact with environmental factors to promote the expression of compulsive symptoms. Critically, while greater compulsivity was associated with obsessive-compulsive behaviors during lockdown, it was not associated with pre-COVID obsessive-compulsive behaviors (expect through interaction with impulsivity; see Supplementary Table 6 for details). Notably, trait compulsivity is associated with family history of obsessive-compulsive and addictive behaviors (46). Thus, these traits may reflect a genetic predisposition toward compulsivity that is influenced by environmental factors (69). As the nature of COVID-19 stressors directly support OCD symptomatology (e.g., contamination concerns), this pre-disposition (which is reflected in trait compulsivity) might then be expected to be associated with greater obsessive-compulsive symptoms during lockdown, more so than with other compulsive and addictive behaviors during lockdown. Finally, this finding adds to the growing literature supporting the CHI-T scale as a measure that is sensitive to OCD-related risk in the general population (28, 46, 47), and may be especially useful to detect at-risk individuals who might benefit from early intervention during the pandemic to minimize progression and entrenchment of problematic behaviors.
Higher trait compulsivity was also associated with more problematic eating behaviors during lockdown, albeit among individuals with low impulsivity only. Among individuals with high impulsivity, trait compulsivity was not associated with problematic lockdown eating behaviors. This pattern of findings may reflect the high impulsivity group having higher levels of pre-existing problematic eating (see Supplementary Table 1), which was itself associated with greater problematic eating during lockdown. In contrast, the lower levels of baseline eating problems among individuals with low impulsivity may have allowed for other influences on lockdown behavior to be revealed, such as trait compulsivity. This pattern of findings was also seen at trend-level for problematic pornography use and may be interpreted similarly. Finally, greater trait compulsivity was associated with lower problematic alcohol use during lockdown. This finding may be best understood in the context of lockdown-related closures of public venues where drinking was common prior to COVID-19. For individuals who drank at these venues regularly, these places provided a wide range of cues (people, situation, etc.) and routines that supported drinking. Individuals high on trait compulsivity are habit- and routine-oriented (47, 70), and strongly influenced by cues (46). Thus, with the closure of public drinking venues, compulsive individuals who drank there lost the cues and routines that previously promoted their drinking. According to this account, without such routines and cues to promote drinking, compulsive individuals may drink less during lockdown than previously, at least, until new drinking habits and routines set in.
The finding that higher psychological distress was associated with greater problematic behaviors during lockdown is in line with emerging findings across addictive and compulsive behaviors (8, 10, 61, 71), as well as a large body of literature suggesting that stress facilitates habit-driven behavior and/or otherwise promotes the maladaptive expression of learned behaviors (44, 49–53). Problematic obsessive-compulsive behaviors were associated with both COVID-related events and psychological distress, in line with a recent study using a COVID events checklist (from which the current items were taken) in relation to obsessive-compulsive and related disorders (59). These findings may be explained in various ways. For instance, for people with obsessive-compulsive tendencies, COVID-related events might be more salient, which may in turn increase reporting of them. Supporting this interpretation, pre-COVID obsessive-compulsive behaviors were the only pre-COVID problematic behavior (of all addictive and compulsive behaviors) associated with exposure to COVID-19 events (see Supplementary Table 6). Further, as several COVID-related events involve potential harm to others and/or contamination, exposure to these events may further promote compulsive behaviors through triggering obsession-related concerns.
In line with other COVID-19 studies, greater pre-COVID levels of problematic behaviors predicted greater problematic behaviors during lockdown across all problematic behaviors. This provides important context for interpreting the current findings in relation to trait impulsivity and compulsivity and their role in driving risk during the current pandemic. That is, while their relationship with addictive and compulsive behaviors is evident from past research (24, 25, 46), as well as current findings (see Supplementary Tables), they may have limited influence on behavior during the current pandemic at this early stage, at least, over and above stress-related influences and pre-COVID levels of the behavior in question. It is likely that the influence of trait impulsivity and compulsivity will become clearer over time, as patterns of behavior become established and differences emerge in relation to how people adapt their behaviors as problems arise. In any case, the current findings highlight the need to better understand the different roles that individual risk factors might play during life as usual vs. during COVID-19, and how these traits might interact with environmental factors to influence disorder-specific expressions.
The current study has several limitations, such as its cross-sectional design, which limits the ability to draw conclusions about the direction of the findings. For instance, while we interpreted the association between compulsivity and problematic eating as indicating that compulsivity increases risk for problematic eating (in those with low impulsivity), an alternative explanation might be that engaging in excessive, unhealthy eating may result in cognitive impairments that in turn drive inflexible, compulsive behaviors (72, 73). Longitudinal research is needed to better understand the direction of the relationship between the trait impulsivity and compulsivity and how they are related to problematic behaviors over the course of this pandemic. Other limitations include the self-reporting of problematic behaviors, including comparisons of behaviors at different timepoints, which is subject to bias and random error. However, previous studies have found self-reported addictive and obsessive-compulsive behavior measures to be generally valid and reliable (74, 75). Also, the current study did not control for important confounding variables such as current mental health diagnosis, trauma, psychiatric medication, illicit drug use, or IQ. Such variables have been shown to be associated with addictive and compulsive behaviors (76–80) as well as impulsivity and/or compulsivity (81–83). Future studies are needed to confirm the present findings taking these confounding variables into account. Finally, participants in this study were recruited through social media and may therefore not be representative of individuals in the general population.
A clear implication of the current findings is the need for interventions that increase resilience to stress to protect against its effects on addictive and compulsive behaviors. Such interventions may include promoting adaptive coping skills and/or healthy lifestyle patterns. For instance, engaging in exercise has been shown to reduce stress levels acutely (84) and regular exercise has been shown to increase resilience to stress generally (85) and has been linked to greater resilience during COVID-19 (63, 86, 87). Further, maintaining a healthy diet (88) and having strong social support (89) have also been linked to increased resilience to stress generally, as well as during COVID-19 (61, 87, 90). Through enhancing resilience to stress, lifestyle interventions and the use of adaptive coping strategies may in turn reduce the risk for addictive and compulsive behaviors during the COVID-19 pandemic.
In conclusion, the current study found that the influence of trait impulsivity and compulsivity on addictive and compulsive behaviors during lockdown differed according to the behavior in question. These behavior-specific findings suggest that traits may interact with situational factors to influence whether pre-existing behaviors continue, increase, or decrease during major life disruptions. In contrast, stress-related variables, i.e., psychological distress and/or exposure to COVID-related stressors, were associated with greater problems across all addictive and compulsive behaviors. The current study adds to the growing literature supporting the need for interventions that enhance resilience to stress during the current pandemic, which in turn could reduce risk for addictive and compulsive disorders.
Contribution to the Field
The COVID-19 pandemic has resulted in high levels of psychological distress worldwide, with experts expressing concern that this could result in corresponding increases in addictive behaviors as individuals seek to cope with their distress. People with high levels of impulsive and compulsive traits may be especially prone to developing problematic coping behaviors during COVID-19. Not only do these traits heighten risk generally, but their influence on risk may be accelerated during times of stress. Thus, early detection of risk is critical as the timeframe for early intervention may be shortened by stress. The current study thus examined the potential of impulsive and compulsive traits to serve as risk markers for addictive and compulsive behaviors during COVID-19. The findings suggest that while impulsive-compulsive traits were associated with all problematic pre-COVID behaviors examined, their influence was limited to a few problematic behaviors during COVID-19. In contrast, stress-related variables were associated with all problematic behaviors during COVID-19, as was severity of pre-COVID problems. These findings suggest that the influence of impulsive and compulsive traits on addictive behaviors during COVID-19 might be largely indirect, mediated through pre-COVID problems. Further, these findings also highlight the impact of stress-related factors across addictive and compulsive behaviors and the need for interventions aimed at enhancing resilience to stress, which in turn may reduce risk for addictive and compulsive disorders.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by Monash Human Research Ethics Committee. The patients/participants provided their consent to participate in this study.
Author Contributions
LA wrote first draft of this manuscript. LA, MY, KRo, and RS designed the major components of the study. LA, KRo, EC, M-EB, AL, and KRi contributed critically to data collection for this study. All authors contributed to revising subsequent versions of the paper. All authors contributed to the selection of study measures.
Funding
MY has received funding from Monash University, the National Health and Medical Research Council (NHMRC; including Fellowship #APP1117188), the Australian Research Council (ARC), Australian Defense Science and Technology (DST), and the Department of Industry, Innovation and Science (DIIS). He has also received philanthropic donations from the David Winston Turner Endowment Fund, Wilson Foundation, as well as payment from law firms in relation to court and/or expert witness reports. SC consults for Promentis; and receives a stipend from Elsevier for editorial work. SC's role in this study was funded by a Wellcome Trust Clinical Fellowship (110049/Z/15/Z). RL was funded by a National Health and Medical Research Council project grant (APP1162031). JG has received research grants from Biohaven, Promentis, and Otsuka Pharmaceuticals. JG receives yearly compensation from Springer Publishing for acting as Editor-in-Chief of the Journal of Gambling Studies and has received royalties from Oxford University Press, American Psychiatric Publishing, Inc., Norton Press, and McGraw Hill.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2021.634583/full#supplementary-material
References
1. Goeders NE. The impact of stress on addiction. Eur Neuropsychopharmacol. (2003) 13:435–41. doi: 10.1016/j.euroneuro.2003.08.004
2. Sinha R. Chronic stress, drug use, and vulnerability to addiction. Ann NY Acad Sci. (2008) 1141:105. doi: 10.1196/annals.1441.030
3. Király O, Potenza MN, Stein DJ, King DL, Hodgins DC, Saunders JB, et al. Preventing problematic internet use during the COVID-19 pandemic: consensus guidance. Compr Psychiatry. (2020) 100:152180. doi: 10.1016/j.comppsych.2020.152180
4. Columb D, Hussain R, O'Gara C. Addiction psychiatry and COVID-19: impact on patients and service provision. Ir J Psycholo Med. (2020) 37:1–5. doi: 10.1017/ipm.2020.47
5. Fontenelle LF, Miguel EC. The impact of COVID-19 in the diagnosis and treatment of obsessive-compulsive disorder. Depress Anxiety. (2020) 37:510–1. doi: 10.1002/da.23037
6. Dubey MJ, Ghosh R, Chatterjee S, Biswas P, Chatterjee S, Dubey S. COVID-19 and addiction. Diab Metab Syndr. (2020) 14:817–23. doi: 10.1016/j.dsx.2020.06.008
7. Sun Y, Li Y, Bao Y, Meng S, Sun Y, Schumann G, et al. Brief report: increased addictive internet and substance use behavior during the COVID-19 pandemic in China. Am J Addict. (2020) 29:268–70. doi: 10.1111/ajad.13066
8. Koopmann A, Georgiadou E, Kiefer F, Hillemacher T. Did the general population in Germany drink more alcohol during the COVID-19 pandemic lockdown? Alcohol Alcohol. (2020) 55:698–9. doi: 10.1093/alcalc/agaa058
9. Benatti B, Albert U, Maina G, Fiorillo A, Celebre L, Girone N, et al. What happened to patients with obsessive compulsive disorder during the COVID-19 pandemic? A multicentre report from tertiary clinics in Northern Italy. Front Psychiatry. (2020) 11:720. doi: 10.3389/fpsyt.2020.00720
10. Håkansson A. Changes in gambling behavior during the COVID-19 pandemic-A web survey study in Sweden. Int J Environ Res Public Health. (2020) 17:4013. doi: 10.3390/ijerph17114013
11. Livingstone C, Myles D, Albertella L, de Lacy-Vawdon C, Carter A, Yucel M. When Pokies Stop: Gambling Behaviour During Restriction of Terrestrial Gambling. School of Public Health and Preventative Medicine, Monash University (2020).
12. Chakraborty A, Karmakar S. Impact of COVID-19 on obsessive compulsive disorder (OCD). Ir J Psychiatry. (2020) 15:256–9. doi: 10.18502/ijps.v15i3.3820
13. Price A. Online gambling in the midst of COVID-19: a nexus of mental health concerns, substance use and financial stress. Int J Ment Health Addict. (2020). doi: 10.1007/s11469-020-00366-1. [Epub ahead of print].
14. Sidor A, Rzymski P. Dietary choices and habits during COVID-19 lockdown: experience from Poland. Nutrients. (2020) 12:1657. doi: 10.3390/nu12061657
15. Rahman MA, Hoque N, Alif SM, Salehin M, Islam SMS, Banik B, et al. Factors Associated With Psychological Distress, Fear and Coping Strategies During the COVID-19 Pandemic in Australia. Global Health. (2020) 16:95. doi: 10.1186/s12992-020-00624-w
16. Miller ML, Brock RL. The effect of trauma on the severity of obsessive-compulsive spectrum symptoms: a meta-analysis. J Anxiety Disord. (2017) 47:29–44. doi: 10.1016/j.janxdis.2017.02.005
17. Garami J, Valikhani A, Parkes D, Haber P, Mahlberg J, Misiak B, et al. Examining perceived stress, childhood trauma and interpersonal trauma in individuals with drug addiction. Psychol Rep. (2019) 122:433–50. doi: 10.1177/0033294118764918
18. Mason SM, Flint AJ, Roberts AL, Agnew-Blais J, Koenen KC, Rich-Edwards JW. Posttraumatic stress disorder symptoms and food addiction in women by timing and type of trauma exposure. JAMA Psychiatry. (2014) 71:1271–8. doi: 10.1001/jamapsychiatry.2014.1208
19. Flory K, Hankin BL, Kloos B, Cheely C, Turecki G. Alcohol and cigarette use and misuse among Hurricane Katrina survivors: psychosocial risk and protective factors. Subst Use Misuse. (2009) 44:1711–24. doi: 10.3109/10826080902962128
20. Ceschi G, Billieux J, Hearn M, Fürst G, Van der Linden M. Trauma exposure interacts with impulsivity in predicting emotion regulation and depressive mood. Eur J Psychotraumatol. (2014) 5:24104. doi: 10.3402/ejpt.v5.24104
21. Daskalakis NP, Bagot RC, Parker KJ, Vinkers CH, de Kloet ER. The three-hit concept of vulnerability and resilience: toward understanding adaptation to early-life adversity outcome. Psychoneuroendocrinology. (2013) 38:1858–73. doi: 10.1016/j.psyneuen.2013.06.008
22. Helen C F, Keri L B, Peihua G, Rajita S. Interactive effects of cumulative stress and impulsivity on alcohol consumption. Alcohol Clin Exp Res. (2010) 34:1376–85. doi: 10.1111/j.1530-0277.2010.01221.x
23. Tiego J, Oostermeijer S, Prochazkova L, Parkes L, Dawson A, Youssef G, et al. Overlapping dimensional phenotypes of impulsivity and compulsivity explain co-occurrence of addictive and related behaviors. CNS Spectr. (2019) 24:426–40. doi: 10.1017/S1092852918001244
24. Fontenelle LF, Oostermeijer S, Harrison BJ, Pantelis C, Yücel M. Obsessive-compulsive disorder, impulse control disorders and drug addiction. Drugs. (2011) 71:827–40. doi: 10.2165/11591790-000000000-00000
25. Chamberlain SR, Stochl J, Redden SA, Grant JE. Latent traits of impulsivity and compulsivity: toward dimensional psychiatry. Psychol Med. (2018) 48:810–21. doi: 10.1017/S0033291717002185
26. Verdejo-García A, Lawrence AJ, Clark L. Impulsivity as a vulnerability marker for substance-use disorders: review of findings from high-risk research, problem gamblers and genetic association studies. Neuroscie Biobehavi Rev. (2008) 32:777–810. doi: 10.1016/j.neubiorev.2007.11.003
27. Robbins TW, Gillan CM, Smith DG, de Wit S, Ersche KD. Neurocognitive endophenotypes of impulsivity and compulsivity: towards dimensional psychiatry. Trends Cogn Sci. (2012) 16:81–91. doi: 10.1016/j.tics.2011.11.009
28. Hook RW, Grant JE, Ioannidis K, Tiego J, Yücel M, Wilkinson P, et al. Trans-diagnostic measurement of impulsivity and compulsivity: a review of self-report tools. Neurosci Biobehav Rev. (2020) 120:455–69. doi: 10.1016/j.neubiorev.2020.10.007
29. Prochazkova L, Parkes L, Dawson A, Youssef G, Ferreira GM, Lorenzetti V, et al. Unpacking the role of self-reported compulsivity and impulsivity in obsessive-compulsive disorder. CNS Spectr. (2018) 23:51–8. doi: 10.1017/S1092852917000244
30. Boisseau CL, Thompson-Brenner H, Caldwell-Harris C, Pratt E, Farchione T, Barlow DH. Behavioral and cognitive impulsivity in obsessive–compulsive disorder and eating disorders. Psychiatry Res. (2012) 200:1062–6. doi: 10.1016/j.psychres.2012.06.010
31. Guo K, Youssef GJ, Dawson A, Parkes L, Oostermeijer S, López-Solà C, et al. A psychometric validation study of the Impulsive-Compulsive Behaviours Checklist: a transdiagnostic tool for addictive and compulsive behaviours. Addict Behav. (2017) 67:26–33. doi: 10.1016/j.addbeh.2016.11.021
32. Whiteside SP, Lynam DR. The five factor model and impulsivity: using a structural model of personality to understand impulsivity. Personal Individ Differ. (2001) 30:669–89. doi: 10.1016/S0191-8869(00)00064-7
33. Evenden JL. Varieties of impulsivity. Psychopharmacology. (1999) 146:348–61. doi: 10.1007/PL00005481
34. Zermatten A, Van der Linden M. Impulsivity in non-clinical persons with obsessive-compulsive symptoms. Personal Individ Differ. (2008) 44:1824–30. doi: 10.1016/j.paid.2008.01.025
35. Albertella L, Le Pelley ME, Chamberlain SR, Westbrook F, Fontenelle L, Grant J, et al. Reward-related attentional capture and cognitive inflexibility interact to determine problematic compulsive behaviors. J Behav Ther Exp Psychiatry. (2020) 69:101580. doi: 10.1016/j.jbtep.2020.101580
36. Coskunpinar A, Dir AL, Cyders MA. Multidimensionality in impulsivity and alcohol use: a meta-analysis using the UPPS model of impulsivity. Alcohol Clin Exp Res. (2013) 37:1441–50. doi: 10.1111/acer.12131
37. Grant JE, Lust K, Christenson GA, Redden SA, Chamberlain SR. Gambling and its clinical correlates in university students. Int J Psychiatry Clin Pract. (2019) 23:33–9. doi: 10.1080/13651501.2018.1436715
38. Dalbudak E, Evren C, Topcu M, Aldemir S, Coskun KS, Bozkurt M, et al. Relationship of Internet addiction with impulsivity and severity of psychopathology among Turkish university students. Psychiatry Res. (2013) 210:1086–91. doi: 10.1016/j.psychres.2013.08.014
39. Schag K, Schönleber J, Teufel M, Zipfel S, Giel K. Food-related impulsivity in obesity and Binge Eating Disorder–a systematic review. Obes Rev. (2013) 14:477–95. doi: 10.1111/obr.12017
40. Bothe B, Tóth-Király I, Demetrovics Z, Orosz G. The short version of the Problematic Pornography Consumption Scale (PPCS-6): a reliable and valid measure in general and treatment-seeking populations. J Sex Res. (2020). doi: 10.1080/00224499.2020.1716205. [Epub ahead of print].
41. Figee M, Pattij T, Willuhn I, Luigjes J, van den Brink W, Goudriaan A, et al. Compulsivity in obsessive–compulsive disorder and addictions. Eur Neuropsychopharmacol. (2016) 26:856–68. doi: 10.1016/j.euroneuro.2015.12.003
42. Voon V, Derbyshire K, Rück C, Irvine MA, Worbe Y, Enander J, et al. Disorders of compulsivity: a common bias towards learning habits. Mol Psychiatry. (2015) 20:345. doi: 10.1038/mp.2014.44
43. Luigjes J, Lorenzetti V, de Haan S, Youssef GJ, Murawski C, Sjoerds Z, et al. Defining compulsive behavior. Neuropsychol Rev. (2019) 29:4–13. doi: 10.1007/s11065-019-09404-9
44. Gillan CM, Robbins TW, Sahakian BJ, van den Heuvel OA, van Wingen G. The role of habit in compulsivity. Eur Neuropsychopharmacol. (2016) 26:828–40. doi: 10.1016/j.euroneuro.2015.12.033
45. Yücel M, Oldenhof E, Ahmed SH, Belin D, Billieux J, Bowden-Jones H, et al. A transdiagnostic dimensional approach towards a neuropsychological assessment for addiction: an international Delphi consensus study. Addiction. (2019) 114:1095–109. doi: 10.1111/add.14424
46. Albertella L, Chamberlain SR, Le Pelley ME, Greenwood L-M, Lee RS, Den Ouden L, et al. Compulsivity is measurable across distinct psychiatric symptom domains and is associated with familial risk and reward-related attentional capture. CNS Spectr. (2020) 25:519–26. doi: 10.1017/S1092852919001330
47. Chamberlain SR, Grant JE. Initial validation of a transdiagnostic compulsivity questionnaire: the Cambridge–Chicago Compulsivity Trait Scale. CNS Spectr. (2018) 23:340–6. doi: 10.1017/S1092852918000810
48. Engel SG, Corneliussen SJ, Wonderlich SA, Crosby RD, Le Grange D, Crow S, et al. Impulsivity and compulsivity in bulimia nervosa. Int J Eating Disord. (2005) 38:244–51. doi: 10.1002/eat.20169
49. Schwabe L, Wolf OT. Stress prompts habit behavior in humans. J Neurosci. (2009) 29:7191–8. doi: 10.1523/JNEUROSCI.0979-09.2009
50. van der Straten A, van Leeuwen W, Denys D, van Marle H, van Wingen G. The effect of distress on the balance between goal-directed and habit networks in obsessive-compulsive disorder. Transl Psychiatry. (2020) 10:1–10. doi: 10.1038/s41398-020-0744-7
51. Wirz L, Bogdanov M, Schwabe L. Habits under stress: mechanistic insights across different types of learning. Curr Opin Behav Sci. (2018) 20:9–16. doi: 10.1016/j.cobeha.2017.08.009
52. Sharp B. Basolateral amygdala and stress-induced hyperexcitability affect motivated behaviors and addiction. Transl Psychiatry. (2017) 7:e1194-e. doi: 10.1038/tp.2017.161
53. Koob GF, Schulkin J. Addiction and stress: an allostatic view. Neurosci Biobehav Rev. (2019) 106:245–62. doi: 10.1016/j.neubiorev.2018.09.008
54. Den Ouden L, Tiego J, Lee RS, Albertella L, Greenwood L-M, Fontenelle L, et al. The role of Experiential Avoidance in transdiagnostic compulsive behavior: a structural model analysis. Addict Behav. (2020) 108:106464. doi: 10.1016/j.addbeh.2020.106464
55. Fontenelle LF, Oldenhof E, Eduarda Moreira-de-Oliveira M, Abramowitz JS, Antony MM, Cath D, et al. A transdiagnostic perspective of constructs underlying obsessive-compulsive and related disorders: an international Delphi consensus study. Aust New Zealand J Psychiatry. (2020) 54:0004867420912327. doi: 10.1177/0004867420912327
56. Grassi G, Pallanti S, Righi L, Figee M, Mantione M, Denys D, et al. Think twice: impulsivity and decision making in obsessive–compulsive disorder. J Behav Addict. (2015) 4:263–72. doi: 10.1556/2006.4.2015.039
57. Cyders MA, Littlefield AK, Coffey S, Karyadi KA. Examination of a short English version of the UPPS-P Impulsive Behavior Scale. Addict Behav. (2014) 39(9):1372-6. doi: 10.1016/j.addbeh.2014.02.013
58. Fontenelle L, Muhlbauer JE, Albertella L, Eppingstall J. The Impact of Coronavirus on Hoarding. School of Psychological Sciences, Monash University (2020).
59. Fontenelle L, Brierley ME, Destree L, Thompson E, Chamberlain SR, Albertella L, et al. Correlates of Obsessive-Compulsive and Related Disorders Symptom Severity During the COVID-19 Pandemic. School of Psychological Sciences, Monash University (2020).
60. Kessler RC, Andrews G, Colpe LJ, Hiripi E, Mroczek DK, Normand S-L, et al. Short screening scales to monitor population prevalences and trends in non-specific psychological distress. Psychological Med. (2002) 32:959–76. doi: 10.1017/S0033291702006074
61. Lechner WV, Laurene KR, Patel S, Anderson M, Grega C, Kenne DR. Changes in alcohol use as a function of psychological distress and social support following COVID-19 related University closings. Addict Behav. (2020) 110:106527. doi: 10.1016/j.addbeh.2020.106527
62. Dawel A, Shou Y, Smithson M, Cherbuin N, Banfield M, Calear AL, et al. The effect of COVID-19 on mental health and wellbeing in a representative sample of Australian adults. Front Psychiatry. (2020) 11:579985. doi: 10.3389/fpsyt.2020.579985
63. Shanahan L, Steinhoff A, Bechtiger L, Murray AL, Nivette A, Hepp U, et al. Emotional distress in young adults during the COVID-19 pandemic: evidence of risk and resilience from a longitudinal cohort study. Psychol Med. (2020). doi: 10.1017/S003329172000241X. [Epub ahead of print].
64. Schulte EM, Gearhardt AN. Development of the modified Yale food addiction scale version 2.0. Eur Eating Disord Rev. (2017) 25:302–8. doi: 10.1002/erv.2515
65. Pawlikowski M, Altstotter-Gleich C, Brand M. Validation and psychometric properties of a short version of Young's Internet Addiction Test. Comput Human Behav. (2013) 29:1212–23. doi: 10.1016/j.chb.2012.10.014
66. Ferris JA, Wynne HJ. The Canadian Problem Gambling Index. Ottawa, ON: Canadian Centre on Substance Abuse (2001).
67. Saunders JB, Aasland OG, Babor TF, De la Fuente JR, Grant M. Development of the alcohol use disorders identification test (AUDIT): WHO collaborative project on early detection of persons with harmful alcohol consumption-II. Addiction. (1993) 88:791–804. doi: 10.1111/j.1360-0443.1993.tb02093.x
68. Foa EB, Huppert JD, Leiberg S, Langner R, Kichic R, Hajcak G, et al. The obsessive-compulsive inventory: development and validation of a short version. Psychol Assess. (2002) 14:485. doi: 10.1037/1040-3590.14.4.485
69. Tiego J, Chamberlain SR, Harrison BJ, Dawson A, Albertella L, Youssef GJ, et al. Heritability of overlapping impulsivity and compulsivity dimensional phenotypes. Sci Rep. (2020) 10:1–17. doi: 10.1038/s41598-020-71013-x
70. Ersche KD, Ward LH, Lim T-V, Lumsden RJ, Sawiak SJ, Robbins TW, et al. Impulsivity and compulsivity are differentially associated with automaticity and routine on the Creature of Habit Scale. Pers Individ Diff . (2019) 150:109493. doi: 10.1016/j.paid.2019.07.003
71. Dong H, Yang F, Lu X, Hao W. Internet addiction and related psychological factors among children and adolescents in china during the coronavirus disease 2019 (COVID-19) epidemic. Front Psychiatry. (2020) 11:751. doi: 10.3389/fpsyt.2020.00751
72. Magnusson K, Hauck L, Jeffrey B, Elias V, Humphrey A, Nath R, et al. Relationships between diet-related changes in the gut microbiome and cognitive flexibility. Neuroscience. (2015) 300:128–40. doi: 10.1016/j.neuroscience.2015.05.016
73. Kanoski SE, Davidson TL. Western diet consumption and cognitive impairment: links to hippocampal dysfunction and obesity. Physiol Behav. (2011) 103:59–68. doi: 10.1016/j.physbeh.2010.12.003
74. Hesselbrock M, Babor TF, Hesselbrock V, Meyer RE, Workman K. “Never believe an alcoholic”? On the validity of self-report measures of alcohol dependence and related constructs. Int J Addict. (1983) 18:593–609. doi: 10.3109/10826088309027359
75. Steketee G, Frost R, Bogart K. The Yale-Brown obsessive compulsive scale: interview versus self-report. Behav Res Ther. (1996) 34:675–84. doi: 10.1016/0005-7967(96)00036-8
76. Sjölund S, Hemmingsson T, Allebeck P. IQ and level of alcohol consumption—findings from a national survey of Swedish conscripts. Alcohol Clin Exp Res. (2015) 39:548–55. doi: 10.1111/acer.12656
77. Fontanesi L, Marchetti D, Limoncin E, Rossi R, Nimbi FM, Mollaioli D, et al. Hypersexuality and trauma: a mediation and moderation model from psychopathology to problematic sexual behavior. J Affect Disord. (2020) 281:631–7. doi: 10.1016/j.jad.2020.11.100
78. Pilver CE, Libby DJ, Hoff RA, Potenza MN. Problem gambling severity and the incidence of Axis I psychopathology among older adults in the general population. J Psychiatr Res. (2013) 47:534–41. doi: 10.1016/j.jpsychires.2012.12.013
79. Stiles-Shields C, Bogue C, Grange DL, Yohanna D. An examination of adults on antipsychotic medication at risk for metabolic syndrome: a comparison with obese and eating disorder populations. Eur Eating Disord Rev. (2013) 21:165–9. doi: 10.1002/erv.2200
80. Destrée L, Albertella L, Torres AR, Ferrão YA, Shavitt RG, Miguel EC, et al. Social losses predict a faster onset and greater severity of obsessive-compulsive disorder. J Psychiatr Res. (2020) 130:187–93. doi: 10.1016/j.jpsychires.2020.07.027
81. de Wit H, Flory JD, Acheson A, McCloskey M, Manuck SB. IQ and nonplanning impulsivity are independently associated with delay discounting in middle-aged adults. Personal Individ Diff . (2007) 42:111–21. doi: 10.1016/j.paid.2006.06.026
82. Corstorphine E, Waller G, Lawson R, Ganis C. Trauma and multi-impulsivity in the eating disorders. Eating Behav. (2007) 8:23–30. doi: 10.1016/j.eatbeh.2004.08.009
83. Reddy LF, Lee J, Davis MC, Altshuler L, Glahn DC, Miklowitz DJ, et al. Impulsivity and risk taking in bipolar disorder and schizophrenia. Neuropsychopharmacology. (2014) 39:456–63. doi: 10.1038/npp.2013.218
84. Basso JC, Suzuki WA. The effects of acute exercise on mood, cognition, neurophysiology, and neurochemical pathways: a review. Brain Plast. (2017) 2:127–52. doi: 10.3233/BPL-160040
85. Childs E, de Wit H. Regular exercise is associated with emotional resilience to acute stress in healthy adults. Front Physiol. (2014) 5:161. doi: 10.3389/fphys.2014.00161
86. Maugeri G, Castrogiovanni P, Battaglia G, Pippi R, D'Agata V, Palma A, et al. The impact of physical activity on psychological health during Covid-19 pandemic in Italy. Heliyon. (2020) 6:e04315. doi: 10.1016/j.heliyon.2020.e04315
87. Ingram J, Maciejewski G, Hand CJ. Changes in diet, sleep, and physical activity are associated with differences in negative mood during COVID-19 lockdown. Front Psychol. (2020) 11:2328. doi: 10.3389/fpsyg.2020.605118
88. Shively CA, Appt SE, Chen H, Day SM, Frye BM, Shaltout HA, et al. Mediterranean diet, stress resilience, and aging in nonhuman primates. Neurobiol Stress. (2020) 13:100254. doi: 10.1016/j.ynstr.2020.100254
89. Ozbay F, Johnson DC, Dimoulas E, Morgan C III, Charney D, Southwick S. Social support and resilience to stress: from neurobiology to clinical practice. Psychiatry. (2007) 4:35.
Keywords: compulsivity, impulsivity, addiction, OCD, COVID-19
Citation: Albertella L, Rotaru K, Christensen E, Lowe A, Brierley M-E, Richardson K, Chamberlain SR, Lee RSC, Kayayan E, Grant JE, Schluter-Hughes S, Ince C, Fontenelle LF, Segrave R and Yücel M (2021) The Influence of Trait Compulsivity and Impulsivity on Addictive and Compulsive Behaviors During COVID-19. Front. Psychiatry 12:634583. doi: 10.3389/fpsyt.2021.634583
Received: 28 November 2020; Accepted: 29 January 2021;
Published: 23 February 2021.
Edited by:
Ornella Corazza, University of Hertfordshire, United KingdomReviewed by:
Christie Burton, Hospital for Sick Children, CanadaAlessio Simonetti, Baylor College of Medicine, United States
Copyright © 2021 Albertella, Rotaru, Christensen, Lowe, Brierley, Richardson, Chamberlain, Lee, Kayayan, Grant, Schluter-Hughes, Ince, Fontenelle, Segrave and Yücel. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Lucy Albertella, lucy.albertella@monash.edu
†These authors share senior authorship
 Lucy Albertella
Lucy Albertella Kristian Rotaru
Kristian Rotaru Erynn Christensen
Erynn Christensen Amelia Lowe1
Amelia Lowe1 Karyn Richardson
Karyn Richardson Rico S. C. Lee
Rico S. C. Lee Edouard Kayayan
Edouard Kayayan Sam Schluter-Hughes
Sam Schluter-Hughes Campbell Ince
Campbell Ince Leonardo F. Fontenelle
Leonardo F. Fontenelle Rebecca Segrave
Rebecca Segrave Murat Yücel
Murat Yücel