- 1Department of Mental Health, Graduate School of Medicine, The University of Tokyo, Tokyo, Japan
- 2Department of Community Mental Health and Law, National Institute of Mental Health, National Center of Neurology and Psychiatry, Kodaira, Japan
- 3Department of Clinical Epidemiology, Translational Medical Center, National Center of Neurology and Psychiatry, Kodaira, Japan
- 4Kawasaki City Center for Mental Health and Welfare, Kawasaki, Japan
- 5Research Institute of Nursing Care for People and Community, University of Hyogo, Akashi, Japan
Psychotic experiences (PEs) may be associated with hikikomori. In the present study, we analyzed interview data from a community-based representative sample (N = 1,616) in Japan to know the association of PEs over a life time, as well as the two components, hallucinatory experiences (HEs) and delusional experiences (DEs), with lifetime experience of hikikomori (severe social withdrawal). Logistic regression analysis was used to estimate the association between any PE, any HE, and any DE; and hikikomori, adjusting for socio-demographics and other psychopathologies (mental disorder in the past 12 months or having autistic spectrum disorder trait). Any PE was significantly associated with hikikomori [odds ratio (OR) =3.44, 95% CI = 1.14–10.33] after adjustment for sociodemographic factors, although the association attenuated after adjusting for other psychopathologies. Any DE remained significantly associated with hikikomori, even after adjustment for all the covariates (OR = 10.50, 95% CI = 1.57–70.29). Any HE was not significantly associated with hikikomori. DEs may be associated with hikikomori. However, because the study sample was small and the temporal association between DEs and hikikomori was unclear, a future study is needed to examine a causal relationship between DEs and hikikomori.
Introduction
Hikikomori (severe social withdrawal) is a public mental health concern worldwide, as well as in Japan (1). Hikikomori is defined as withdrawing from all social engagement (e.g., education, employment, and friendships) for at least 6 months (2). The epidemiological research has shown the prevalence of hikikomori to be ~1% in Japan (3). Considerable concern has been growing about the potential societal and economic impact of hikikomori, such as a declining labor force, although the actual impact has yet to be examined (4–6). Meanwhile, it is important to understand its determinants and to develop preventive measures.
Previous studies investigated a variety of factors associated with the occurrence of hikikomori, including socio-cultural influences, e.g., the social structure, the school context, and family relationships (7–9). In addition, they identified a broad range of psychopathology, such as common mental disorders (3), Internet addiction (10), social phobic tendencies (11), and autistic spectrum disorders (12). Another previous study also reported a high prevalence of severe mental disorders among patients with hikikomori who sought help at community mental health centers: for instance, 5.3% of the cases were diagnosed as schizophrenia and other psychotic disorders (13). However, the sample may be biased because this previous study used only service users; the magnitude of the association between the disorder and hikikomori was unclear because no comparison was made with non-cases.
Psychotic experiences (PEs) refer to a broad spectrum of hallucinatory and delusional symptoms from clinical to subthreshold, that often are milder than symptoms of schizophrenia (14, 15). PEs are common in the general population: a previous meta-analysis reported a lifetime prevalence of 7.2% (16). This prevalence is much higher than that of schizophrenia (17). PEs have been recognized as a risk factor for developing psychotic disorders (18, 19), common mental disorders (20), and suicidality (21–23). Thus, PEs may be an important psychopathology that could affect various aspects of mental health and mental disorders. PEs also may be associated with the development of hikikomori. Previous studies revealed that PEs were associated with later poorer social functioning, and not participating in education, employment, or training (NEET) (24–26). Another previous study reported a high prevalence of schizophrenia, a severe form of PE, among cases with hikikomori (13). However, no previous study has investigated the association between PEs and hikikomori. Because PEs are milder psychotic symptoms common in the general population, studying the association between PEs and hikikomori would contribute to better understanding the psychopathology of hikikomori and developing effective early intervention measures.
PEs have two components: hallucinatory experiences (HEs) and delusional experiences (DEs) (27). These two components differ in terms of their prevalence, demographic characteristics, and social functioning (27–30). For example, a lifetime prevalence was found to be much greater for HEs (5.2%) than for DEs (1.3%) (27). HEs are more common among women, but no gender difference was found for DEs; DEs are more common in the younger generation, but no age difference was observed for HEs (27). A metacognitive decline was more prominently associated with DEs than with HEs (28–30). These previous findings suggest that HEs and DEs each have unique etiology and clinical consequences. It would be interesting to investigate the association with hikikomori separately for HEs and DEs, which also would contribute to understanding the psychopathology of hikikomori.
This cross-sectional study aimed to preliminarily explore the association between lifetime experienes of PEs and hikikomori in a national sample of community-living adults in Japan, based on the World Mental Health Japan Second Survey [WMHJ2; (31)]. While the study could not specify the causal relationship between PEs and hikikomori, it would provide a useful insight into this research topic that was poorly studied previously.
Methods
Sample
We conducted the WMHJ2 Survey by using a two-stage random sampling method from 2013 to 2015 among community residents in Japan (31). The survey area was divided into 3 sections: (1) Kanto district (Tokyo Metropolitan area and surrounding areas); (2) Tokai, Hokuriku, Koshin'etsu, Tohoku, and Hokkaido (the eastern part of Japan except for Kanto); and (3) Kinki, Chugoku, Kyushu, Shikoku, and Okinawa (the western part of Japan). We recruited a sample of almost 5,000 representative individuals aged 20–75 years old in 129 municipalities. Of these, 2,450 individuals participated in the studies and the average response rate was 43.4%. A face-to-face interview survey and a self-administered questionnaire were carried out by trained interviewers who visited the homes of respondents and collected the data. The Japanese computerized edition of the World Health Organization Integrated International Diagnostic Interview (WHO-CIDI), version 3.0 was used for the interview survey (32, 33). The Research Ethics Committee of the Graduate School of Medicine, The University of Tokyo approved the protocols of this study [nos. 10131-(1), -(2), -(3), and -(4)].
Measures
Hikikomori
Hikikomori was measured by a single item, defined as a state of social withdrawal for more than 6 months, communicating only with family members and rarely leaving the house for work or school, measured by a module developed in a previous study. Participants were classified into those with or without any experience in the lifetime (yes/no; 3). Respondents were asked if they had ever experienced hikikomori [e.g., “Have you ever had a time when you stayed at home for more than 6 months without going to work or school or interacting with people other than your family (you may sometimes go shopping)?”].
Psychotic Experiences (PEs), any PE, any HE, any DE Over a Lifetime
The CIDI Psychosis Module was composed of six PE types. The six PE types consisted of two items related to HEs (visual hallucinations, auditory hallucinations) and four items related to DEs (thought insertion/withdrawal, mind control/passivity, ideas of reference, plot to harm/follow) (27, 32). Respondents were asked questions concerning PEs (see Appendix 1). Then, a probe question was asked to determine whether the reported PEs occurred when the patient was “not dreaming, not half asleep, and not under the influence of alcohol or drugs.” Only the latter type of responses were considered. We showed the prevalence estimates for any PE, any HE (with or without an associated DE) and any DE (with or without an associated HE) in this study.
Mental Disorder in the Past 12 Months
Mental disorder in the past 12 months was measured by using the WHO-CIDI 3.0 (31, 33). Mental disorders included 12 common mental disorders [generalized anxiety disorder, panic disorder, social phobia, agoraphobia, post-traumatic stress disorder, major depressive disorder, bipolar disorders (I and II), dysthymia, alcohol abuse and dependence, and drug abuse and dependence] which were diagnosed by using the Diagnostic and Statistical Manual of Mental Disorders, 4th edition (DSM-IV). Those reporting a common mental disorder in the past 12 months met the diagnostic criteria for any of these mental disorders. We measured autistic spectrum disorder (ASD) trait using the Japanese version of Autism Spectrum Quotient Short Form [AQ-J-10; (12, 34)]. AQ-J-10 is a 10-item self-administered questionnaire to screen adolescents and adults for current high-functioning pervasive developmental disorders. A total score of 7 or higher was defined as “having ASD trait” (34). The sensitivity and specificity of this cut-off point were 0.75 and 0.90, respectively (34).
Sociodemographic Factors
Age, gender, education, and income were examined as sociodemographic factors. Education was divided into four groups: junior high school graduates, high school graduates, some college, and university graduates or higher. Annual household income included the respondent's own earned income, spouse's income, income from others, social security income, and other income. We imputed the missing values of income by their age, sex, education, employment status and household size (35). However, we used those without missing values for other variables. Annual household income was divided into 4 groups: < 2.5 million yen, from 2.5 million yen to < 5 million yen, from 5 million yen to < 7.5 million yen, and 7.5 million yen or over.
Statistical Analysis
Logistic regression analysis was used to estimate the association between any PE and hikikomori, any HE and hikikomori, and any DE and hikikomori. Hikikomori was analyzed as a dependent variable. Sociodemographic variables were adjusted for in Model 1 and Mental disorder in the past 12 months and having ASD trait were additionally adjusted for in Model 2. Fisher's exact test was performed to examine the association between the proportions of PEs and the presence of hikikomori. SPSS (Windows version 26) was used for statistical analysis and a p < 0.05 was considered statistically significant.
Results
Demographic Characteristics and Prevalence of Hikikomori and PEs
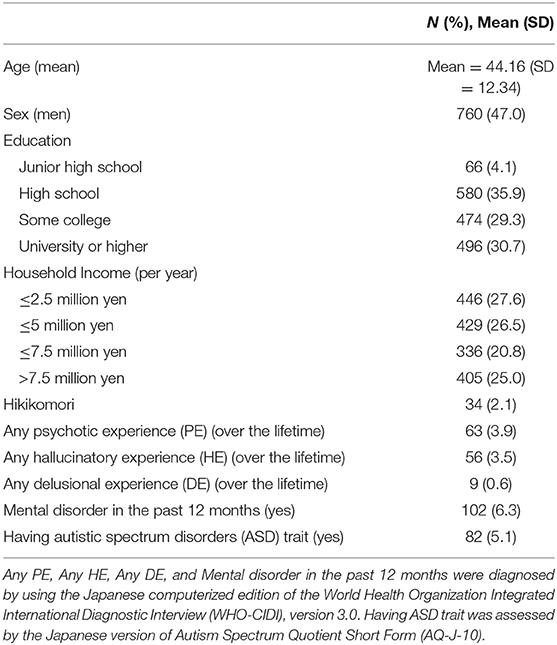
Among 2,450 total survey respondents, 1,775 answered the questionnaire on hikikomori. Some of these respondents had missing values on demographic variables (n = 6), PEs (n = 27), and ASD trait (n = 126); these respondents were excluded, which left an analytic sample of 1,616 respondents. Table 1 shows the demographic and psychosocial characteristics and the prevalence of hikikomori and PEs. For hikikomori, the average age in the survey was 37.38 (SD = 1.90), the average onset age was 27.53 (SD = 10.22), and the average hikikomori duration was 5.85 years (SD = 4.47). For PEs, the average age in the survey was 42.59 (SD = 1.50), and the average onset age was 24.21 (SD = 14.14). Thirty-four (2.1%) had experienced hikikomori and 1,582 had not. Among those who had experienced hikikomori, 4 had any PE, 2 had any HE, and 2 had any DE. Proportions with any PE (p = 0.04) and any DE (p = 0.01) among those who had experienced hikikomori were significantly higher than among those who had not experienced it, but the proportion with any HE was insignificant (p = 0.33). These p-values were obtained by Fisher's exact test.
Any PE, any HE, any DE, and Hikikomori
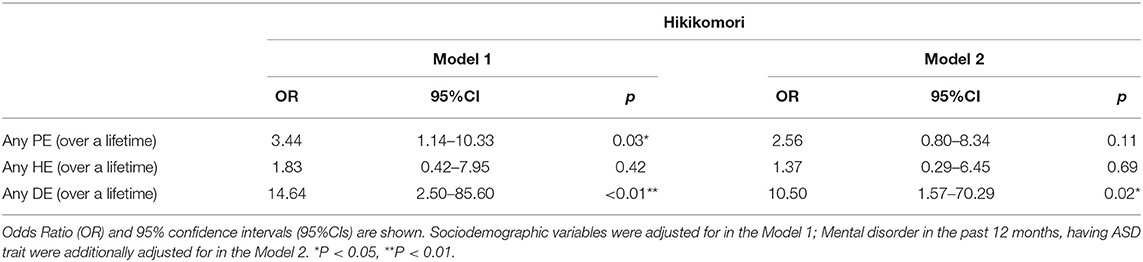
As is seen in Table 2, any PE was significantly and positively associated with hikikomori after adjusting for socio-demographic variables (Model 1: OR = 3.44, 95% CI = 1.14–10.33). However, no significant associations were seen after adjusting for mental disorder in the past 12 months and ASD trait (Model 2: OR = 2.56, 95% CI = 0.80–8.34). In the sensitivity analyses, any HE was not significantly associated with hikikomori after adjusting for both Model 1 and Model 2 (OR = 1.83, 95% CI = 0.42–7.95; OR = 1.37, 95% CI = 0.29–6.45). On the other hand, any DE was significantly and positively associated with hikikomori after adjusting for both Model 1 and Model 2 (OR = 14.64, 95% CI = 2.50–85.60; OR = 10.50, 95% CI = 1.57–70.29).
Discussion
Main Findings
To our knowledge, this is the first study to describe the association between PEs and hikikomori. Any PE and any DE were significantly and positively associated with hikikomori, while any HE was not significantly associated with hikikomori. Only any DE had a significant relation with hikikomori when adjusting for both sociodemographics and psychopathology. However, because this study was cross-sectional, we could not specify the temporal association between these two conditions. It was unclear if PE led to hikikomori, hikikomori led to PE, or PE and hikikomori co-occurred. In addition, because of the small sample size and low prevalence of PEs and hikikomori, the statistical power of the study, and the generalization of the findings may be limited.
Comparing to the Previous Findings
Previous studies revealed that PEs were associated with later poorer social functioning and participation (24, 25). In addition, a previous survey revealed that hikikomori showed a wide coexistence with psychiatric disorders, including schizophrenia, mood disorders, anxiety disorders, personality disorders, and pervasive developmental disorder (36). Our results were consistent with the previous studies, and also found that any PE, particularly any DE, could also be one of the determinants for hikikomori.
Potential Mechanisms
The possible mechanisms for the relationship between PEs and hikikomori is that PEs could be a determinant for hikikomori. Hikikomori was often observed in prodromal-stage cases of psychosis (37). Hallucinations and delusions might cause frightening experiences when outside and lead to hikikomori.
The reason that any DE, but not any HE, was significantly associated with hikikomori may be explained by the hypothesis that a DE could have mediated metacognitive decline and hikikomori. A previous study indicated that metacognitive decline could be associated with hikikomori (38). In addition, the metacognitive decline was reported to be less associated with hallucinations but more related to delusions (28–30). Therefore, it is possible that hikikomori could be caused by metacognitive decline mediated by delusion. That is why only any DE had a significant association with hikikomori.
Strengths and Limitations
The strengths of this study are as follows. First, this study used a nationally representative sample using a two-stage random sampling method. Second, the study measured PEs, hikikomori and mental disorders diagnosed by a structured interview, WHO-CIDI 3.0.
However, there are many limitations in this study. Thus, caution should be used in interpretation of the results. First, as we stated earlier, this study was cross-sectional, which could not show a causality between PEs and hikikomori. We could not specify the temporal association between these two conditions because data were limited in this study. The alternative explanation was that hikikomori could affect PEs. Sensory deprivation has been linked to psychotic symptoms for decades, even in otherwise normal individuals (37). The sensory deprivation experienced by hikikomori who stay for extended periods in their room could increase PEs. Another explanation was the social defeat (SD) hypothesis, which is that long-term exposure to the experience of SD may lead to sensitization of the mesolimbic dopamine system and thereby increase the risk for schizophrenia (39, 40). People with hikikomori could have felt SD, which would increase the potential for PEs. However, to clarify the potential mechanism, longitudinal studies should be conducted in the future. Second, the number of cases with PEs and hikikomori was small as a proportion of our overall sample size. The sample may include selected participants that limit the generalizability. We may have overlooked some important associations. Third, the response rate of the WMHJ2 survey was not high overall, which could cause selection bias, although a previous study of the prevalence of common mental disorders suggested that response rate might not have a strong effect on the prevalence estimates of mental disorders in a community-based survey (41). Fourth, information bias may have been present if respondents with PEs were more aware of problems related to hikikomori and therefore more hesitant to report such problems in the survey. Fifth, other covariates may confound the association; for instance, psychotic disorders such as schizophrenia, which was not measured in this study, may partly explain the association between PEs and hikikomori. We did not measure negative symptoms that are often observed among people with chronic schizophrenia, which could also be an important psychopathology leading to social withdrawal. Sixth, our definition of “hikikomori” following that in a previous study (42) was based on only the behavioral patterns and did not consider the etiology or psychopathology of hikikomori. Hikikomori may consist of multiple psychopathologies. The association between subtypes of hikikomori and PE needs to be investigated in future research.
Implications
While the findings are largely limited by the small number of hikikomori cases and PE cases, some clinical implications can be drawn. Some Hikikomori cases may develop due to or at least be comorbid with PEs. Thus, psychiatric assessment of these cases would be important. By sharing with health professionals the finding that PEs could be a determinant of hikikomori, early intervention for PEs with careful assessment, frequent monitoring and, if necessary, outreach visits to homes could be a good practice. In addition, it could be useful if health professionals would provide sufficient information to the public about the known risks of PEs and enhance the consultation support system for people with PEs and their families. Carrying out these efforts may decrease the future risk for hikikomori in the population.
Conclusions
Any PE, particularly any DE, might be associated with hikikomori in this general population sample. The findings obtained in the current study inform our understanding of the relationship between PEs and hikikomori. Future population-based studies with longitudinal data are needed to better understand the etiology and prevention of hikikomori in the context of PEs.
Data Availability Statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Ethics Statement
The studies involving human participants were reviewed and approved by The Research Ethics Committees of the Graduate School of Medicine/Faculty of Medicine, The University of Tokyo [nos. 10131-(1), -(2), -(3), and -(4)] approved the aims and procedures of this study before it began. The patients/participants provided their written informed consent to participate in this study.
Author Contributions
NY was the principal investigator who conceptualized and designed the study, analyzed data, and drafted the article. KW, DN, HI, HT, TT, MU, and NK made a critical revision of the article and gave final approval for the version to be published. All authors contributed to the article and approved the submitted version.
Funding
The authors declare that this study received funding from the Japan Ministry of Health, Labour, and Welfare (Grant Number H25-SEISHIN-IPPAN006) and the Japan Agency for Medical Research and Development (Grant Number 15dk0310020h0003). The overall WMHS was supported by the US National Institute of Mental Health (Grant Number R01 MH070884), the MacArthur Foundation (Grant Number R13-MH066849), the Pfizer Foundation (Grant Number R01-MH069864), the US Public Health Service (Grant Number R01 DA016558), the Fogarty International Center (Grant Number R03-TW006481), and the Pan American Health Organization, Eli Lilly and Company, Ortho-McNeil Pharmaceutical Inc., GlaxoSmithKline, Bristol-Myers Squibb, and Shire. The funders were not involved in the study design, collection, analysis, interpretation of data, the writing of this article or the decision to submit it for publication.
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Supplementary Material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fpsyt.2020.602678/full#supplementary-material
References
1. Kato TA, Shinfuku N, Sartorius N, Kanba S. Are Japan's hikikomori and depression in young people spreading abroad? Lancet. (2011) 378:1070. doi: 10.1016/S0140-6736(11)61475-X
2. Watts J. Public health experts concerned about “hikikomori.” Lancet. (2002) 359:1131. doi: 10.1016/S0140-6736(02)08186-2
3. Koyama A, Miyake Y, Kawakami N, Tsuchiya M, Tachimori H, Takeshima T. World Mental Health Japan Survey Group 2002-2006. Lifetime prevalence, psychiatric comorbidity and demographic correlates of “hikikomori” in a community population in Japan. Psychiatry Res. (2010) 176:69–74. doi: 10.1016/j.psychres.2008.10.019
4. Kato TA, Kanba S, Teo AR. Hikikomori: experience in Japan and international relevance. World Psychiatry. (2018) 17:105–6. doi: 10.1002/wps.20497
5. Li TM, Wong PW. Youth social withdrawal behavior (hikikomori): a systematic review of qualitative and quantitative studies. Aust N Z J Psychiatry. (2015) 49:595–609. doi: 10.1177/0004867415581179
6. Wong J, Wan M, Kroneman L, Kato TA, Lo TW, Wong PW, et al. Hikikomori phenomenon in East Asia: regional perspectives, challenges, and opportunities for social health agencies. Front Psychiatry. (2019) 10:512. doi: 10.3389/fpsyt.2019.00512
7. Kato TA, Tateno M, Shinfuku N, Fujisawa D, Teo AR, Sartorius N, et al. Does the 'hikikomori' syndrome of social withdrawal exist outside Japan? A preliminary international investigation. Soc Psychiatry Psychiatr Epidemiol. (2012) 47:1061–75. doi: 10.1007/s00127-011-0411-7
8. Pozza A, Coluccia A, Kato T, Gaetani M, Ferretti F. The 'Hikikomori' syndrome: worldwide prevalence and co-occurring major psychiatric disorders: a systematic review and meta-analysis protocol. BMJ Open. (2019) 9:e025213. doi: 10.1136/bmjopen-2018-025213
9. Teo AR, Gaw AC. Hikikomori, a Japanese culture-bound syndrome of social withdrawal?: A proposal for DSM-5. J Nerv Ment Dis. (2010) 198:444–9. doi: 10.1097/NMD.0b013e3181e086b1
10. Tateno M, Teo AR, Ukai W, Kanazawa J, Katsuki R, Kubo H, et al. Internet addiction, smartphone addiction, and hikikomori trait in Japanese young adult: social isolation and social network. Front Psychiatry. (2019) 10:455. doi: 10.3389/fpsyt.2019.00455
11. Yong R, Nomura K. Hikikomori is most associated with interpersonal relationships, followed by suicide risks: a secondary analysis of a national cross-sectional study. Front Psychiatry. (2019) 10:247. doi: 10.3389/fpsyt.2019.00247
12. Umeda M, Shimoda H, Miyamoto K, Ishikawa H, Tachimori H, Takeshima T, et al. Comorbidity and sociodemographic characteristics of adult autism spectrum disorder and attention deficit hyperactivity disorder: epidemiological investigation in the World Mental Health Japan 2nd Survey. Int J Dev Disabil. (2019) 65:1–9. doi: 10.1080/20473869.2019.1576409
13. Kondo N, Sakai M, Kuroda Y, Kiyota Y, Kitabata Y, Kurosawa M. General condition of hikikomori (prolonged social withdrawal) in Japan: psychiatric diagnosis and outcome in mental health welfare centres. Int J Soc Psychiatry. (2013) 59:79–86. doi: 10.1177/0020764011423611
14. Healy C, Brannigan R, Dooley N, Coughlan H, Clarke M, Kelleher I, et al. Childhood and adolescent psychotic experiences and risk of mental disorder: a systematic review and meta-analysis. Psychol Med. (2019) 49:1589–99. doi: 10.1017/S0033291719000485
15. Kaymaz N, Drukker M, Lieb R, Wittchen HU, Werbeloff N, Weiser M, et al. Do subthreshold psychotic experiences predict clinical outcomes in unselected non-help-seeking population-based samples? A systematic review and meta-analysis, enriched with new results. Psychol Med. (2012) 42:2239–53. doi: 10.1017/S0033291711002911
16. Linscott RJ, van Os J. An updated and conservative systematic review and meta-analysis of epidemiological evidence on psychotic experiences in children and adults: on the pathway from proneness to persistence to dimensional expression across mental disorders. Psychol Med. (2013) 43:1133–49. doi: 10.1017/S0033291712001626
17. Saha S, Chant D, Welham J, McGrath J. A systematic review of the prevalence of schizophrenia. PLoS Med. (2005) 2:e141. doi: 10.1371/journal.pmed.0020141
18. DeVylder JE, Burnette D, Yang LH. Co-occurrence of psychotic experiences and common mental health conditions across four racially and ethnically diverse population samples. Psychol Med. (2014) 44:3503–13. doi: 10.1017/S0033291714000944
19. Nordgaard J, Buch-Pedersen M, Hastrup LH, Haahr UH, Simonsen E. Measuring psychotic-like experiences in the general population. Psychopathology. (2019) 52:240–7. doi: 10.1159/000502048
20. Kelleher I, Keeley H, Corcoran P, Lynch F, Fitzpatrick C, Devlin N, et al. Clinicopathological significance of psychotic experiences in non-psychotic young people: evidence from four population-based studies. Br J Psychiatry. (2012) 201:26–32. doi: 10.1192/bjp.bp.111.101543
21. Honings S, Drukker M, Groen R, van Os J. Psychotic experiences and risk of self-injurious behaviour in the general population: a systematic review and meta-analysis. Psychol. Med. (2016) 46:237–51. doi: 10.1017/S0033291715001841
22. Yates K, Lång U, Cederlöf M, Boland F, Taylor P, Cannon M, et al. Association of psychotic experiences with subsequent risk of suicidal ideation, suicide attempts, and suicide deaths: a systematic review and meta-analysis of longitudinal population studies. JAMA psychiatry. (2019) 76:180–9. doi: 10.1001/jamapsychiatry.2018.3514
23. Narita Z, Wilcox HC, DeVylder J. Psychotic experiences and suicidal outcomes in a general population sample. Schizophr Res. (2020) 215:223–8. doi: 10.1016/j.schres.2019.10.024
24. Rössler W, Riecher-Rössler A, Angst J, Murray R, Gamma A, Eich D, et al. Psychotic experiences in the general population: a twenty-year prospective community study. Schizophr Res. (2007) 92:1–14. doi: 10.1016/j.schres.2007.01.002
25. Trotta A, Arseneault L, Caspi A, Moffitt TE, Danese A, Pariante C, et al. Mental health and functional outcomes in young adulthood of children with psychotic symptoms: a longitudinal cohort study. Schizophr Bull. (2020) 46:261–71. doi: 10.1093/schbul/sbz069
26. Davies J, Sullivan S, Zammit S. Adverse life outcomes associated with adolescent psychotic experiences and depressive symptoms. Soc Psychiatry Psychiatr Epidemiol. (2018) 53:497–507. doi: 10.1007/s00127-018-1496-z
27. McGrath JJ, Saha S, Al-Hamzawi A, Alonso J, Bromet EJ, Bruffaerts R, et al. Psychotic experiences in the general population: a cross-national analysis based on 31,261 respondents from 18 countries. JAMA Psychiatry. (2015) 72:697–705. doi: 10.1001/jamapsychiatry.2015.0575
28. Goldstone E, Farhall J, Thomas N, Ong B. The role of metacognitive beliefs in the proneness to hallucinations and delusions: an analysis across clinical and non-clinical populations. Br J Health Psychol. (2013) 52:330–46. doi: 10.1111/bjc.12020
29. Sun X, Zhu C, So S. Dysfunctional metacognition across psychopathologies: a meta-analytic review. Eur Psychiatry. (2017) 45:139–53. doi: 10.1016/j.eurpsy.2017.05.029
30. Varese F, Bentall RP. The metacognitive beliefs account of hallucinatory experiences: a literature review and meta-analysis. Clin Psychol Rev. (2011) 31:850–64. doi: 10.1016/j.cpr.2010.12.001
31. Ishikawa H, Tachimori H, Takeshima T, Umeda M, Miyamoto K, Shimoda H, et al. Prevalence, treatment, and the correlates of common mental disorders in the mid 2010's in Japan: the results of the world mental health Japan 2nd survey. J Affect Disord. (2018) 241:554–62. doi: 10.1016/j.jad.2018.08.050
32. Haro JM, Arbabzadeh-Bouchez S, Brugha TS, de Girolamo G, Guyer ME, Jin R, et al. Concordance of the composite international diagnostic interview version 3.0 (CIDI 3.0) with standardized clinical assessments in the WHO World Mental Health surveys. Int J Methods Psychiatr Res. (2006) 15:167–80. doi: 10.1002/mpr.196
33. Kawakami N, Takeshima T, Ono Y, Uda H, Hata Y, Nakane Y, et al. Twelve-month prevalence, severity, and treatment of common mental disorders in communities in Japan: preliminary finding from the World Mental Health Japan Survey 2002-2003. Psychiatry Clin Neurosci. (2005) 59:441–52. doi: 10.1111/j.1440-1819.2005.01397.x
34. Kurita H, Koyama T, Osada H. Autism-Spectrum Quotient-Japanese version and its short forms for screening normally intelligent persons with pervasive developmental disorders. Psychiatry Clin Neurosci. (2005) 59:490–6. doi: 10.1111/j.1440-1819.2005.01403.x
35. Kawakami N, Abdulghani EA, Alonso J, Bromet EJ, Bruffaerts R, Caldas-de-Almeida JM, et al. Early-life mental disorders and adult household income in the World Mental Health Surveys. Biol Psychiatry. (2012) 72:228–37. doi: 10.1016/j.biopsych.2012.03.009
36. Kato TA, Kanba S, Teo AR. Hikikomori : multidimensional understanding, assessment, and future international perspectives. Psychiatry Clin Neurosci. (2019) 73:427–40. doi: 10.1111/pcn.12895
37. Stip E, Thibault A, Beauchamp-Chatel A, Kisely S. Internet addiction, hikikomori syndrome, and the prodromal phase of psychosis. Front Psychiatry. (2016) 7:6. doi: 10.3389/fpsyt.2016.00006
38. Gkika S, Wittkowski A, Wells A. Social cognition and metacognition in social anxiety: a systematic review. Clin Psychol Psychother. (2018) 25:10–30. doi: 10.1002/cpp.2127
39. Selten JP, Cantor-Graae E. Social defeat: risk factor for schizophrenia? Br J Psychiatry. (2005) 187:101–2. doi: 10.1192/bjp.187.2.101
40. Selten JP, van der Ven E, Rutten BP, Cantor-Graae E. The social defeat hypothesis of schizophrenia: an update. Schizophr Bull. (2013) 39:1180–6. doi: 10.1093/schbul/sbt134
41. Kawakami N, Yasuma N, Watanabe K, Ishikawa H, Tachimori H, Takeshima T, et al. Association of response rate and prevalence estimates of common mental disorders across 129 areas in a nationally representative survey of adults in Japan. Soc Psychiatry Psychiatr Epidemiol. (2020) 55:1373–82. doi: 10.1007/s00127-020-01847-3
Keywords: hikikomori, social withdrawal, psychotic experiences, hallucinatory experiences, delusional experiences
Citation: Yasuma N, Watanabe K, Nishi D, Ishikawa H, Tachimori H, Takeshima T, Umeda M and Kawakami N (2021) Psychotic Experiences and Hikikomori in a Nationally Representative Sample of Adult Community Residents in Japan: A Cross-Sectional Study. Front. Psychiatry 11:602678. doi: 10.3389/fpsyt.2020.602678
Received: 04 September 2020; Accepted: 08 December 2020;
Published: 29 January 2021.
Edited by:
Wulf Rössler, Charité—Universitätsmedizin Berlin, GermanyReviewed by:
Mary Cannon, Royal College of Surgeons in Ireland, IrelandMarjan Drukker, Maastricht University, Netherlands
Copyright © 2021 Yasuma, Watanabe, Nishi, Ishikawa, Tachimori, Takeshima, Umeda and Kawakami. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Norito Kawakami, nkawakami@m.u-tokyo.ac.jp
 Naonori Yasuma1,2
Naonori Yasuma1,2 Kazuhiro Watanabe
Kazuhiro Watanabe Hisateru Tachimori
Hisateru Tachimori Tadashi Takeshima
Tadashi Takeshima Norito Kawakami
Norito Kawakami