- 1Department of Psychiatry, Harvard Medical School, Boston, MA, USA
- 2Department of Psychiatry, Massachusetts General Hospital, Charlestown, MA, USA
Background: Posttraumatic stress related with the childbirth experience of full-term delivery with health outcomes has been recently documented in a growing body of studies. The magnitude of this condition and the factors that might put a woman at risk for developing childbirth-related postpartum posttraumatic stress disorder (PP-PTSD) symptoms are not fully understood.
Methods: In this systematic review of 36 articles representing quantitative studies of primarily community samples, we set to examine PP-PTSD prevalence rates and associated predictors with a focus on the role of prior PTSD and time since childbirth.
Results: A significant minority of women endorsed PP-PTSD following successful birth. Acute PP-PTSD rates were between 4.6 and 6.3%, and endorsement of clinically significant PP-PTSD symptoms was identified in up to 16.8% of women in community samples of high quality studies. Negative subjective experience of childbirth emerged as the most important predictor. Endorsement of PTSD before childbirth contributed to PP-PTSD; nevertheless, women without PTSD also exhibited PP-PTSD, with acute rates at 4.6%, signifying a new PTSD onset in the postpartum period.
Conclusion: Although the majority of women cope well, childbirth for some can be perceived as a highly stressful experience and even result in the development of PP-PTSD symptoms. More research is needed to understand postpartum adaption and childbirth-related posttraumatic stress outcomes.
Introduction
Many people think of childbirth as a uniformly happy event. This belief may be responsible for the paucity of research into its possible deleterious outcomes. As unpleasant as it may be to face this, such research as exists indicates that childbirth may have negative (as well as positive) psychological effects. Postpartum women may experience psychological distress, and some may even develop mental disorders. Although postpartum depression has been extensively described (O'Hara and McCabe, 2013), accumulating data suggests that new mothers may also exhibit a posttraumatic stress response induced by the childbirth experience and may even suffer from childbirth-related postpartum traumatic stress disorder (PP-PTSD) following successful birth (Olde et al., 2006; Grekin and O'Hara, 2014).
As many as a third of women rate their delivery as psychologically traumatic (Ayers and Pickering, 2001), and as many as one quarter report some component of clinically significant PP-PTSD symptoms (Czarnocka and Slade, 2000). Co-morbidity of PP-PTSD and postpartum depression is high, as evident in up to 72% of cases of women endorsing PP-PTSD (Yildiz et al., 2017), and some may also endorse suicide ideation, as evident in 23% of cases (Dekel et al., in preparation). PP-PTSD may impair maternal bonding and indirectly have adverse affects on infant health (Williams et al., 2016). Hence, PP-PTSD is a problem deserving of attention.
A stress-diathesis model has been proposed to understand the factors giving rising to PP-PTSD (Ayers, 2004). Accordingly, PP-PTSD is the outcome of the interplay between pre-birth vulnerability factors, risk factors in birth, and factors after birth (Ayers et al., 2016). Factors such as pre-existing maternal psychiatric problems, a negative birth experience, and lack of social support, have been consistently reported as commonly endorsed risk factors (e.g., Andersen et al., 2012). These risks are broadly comparable with factors associated with PTSD in relation to other stressors (Ozer et al., 2003).
Much less agreement concerns the estimates of the incidence of PP-PTSD. PP-PTSD rates are between 1 and 30%, too wide a range to be very useful (Andersen et al., 2012; Grekin and O'Hara, 2014). Partial PP-PTSD, i.e., PTSD symptoms occurring at a clinically significant level, has also been noted, but again with a similar pattern of widely estimated rates (Czarnocka and Slade, 2000; Soet et al., 2003; Polachek et al., 2012).
Several review studies have been conducted on the topic. Olde et al. (2006) groundbreaking qualitative review of 19 studies published between 1997 and 2003 identified PP-PTSD following successful birth in up to 5.6% of women at 6 weeks postpartum. A subsequent review by Andersen et al. (2012) of 31 studies between 2003 and 2010 utilized a study quality ranking. They noted PP-PTSD rates in high quality studies were up to 4.6% between three and 12 months postpartum. Recent reviews importantly targeted community in comparison to at-risks samples (Grekin and O'Hara, 2014). As might be expected, PP-PTSD rates were approximately fivefold higher (15.7%) in at-risk groups than in the community (3.1%). Yildiz et al. (2017) report similar results from reviewing 28 studies using a diagnostic measure of PTSD, documenting once again a wide PP-PTSD rate variability among the studies.
These reviews support the existence of PTSD following childbirth; however, some clarification remains. While earlier reviews reported on the prevalence of PTSD during the postpartum period, it is not clear whether the studies were limited to those reporting on PTSD induced by childbirth. To our knowledge, a review comparing PP-PTSD prevalence in the context of prior PTSD versus a first time onset in the postpartum period was not conducted to-date. Such analysis is important to fully grasp the magnitude of the childbirth stressor.
PP-PTSD can be conceptualized in at least two ways. PTSD related to the childbirth event may develop in the context of endorsement of existing posttraumatic stress syndrome before childbirth. An estimated lifetime prevalence of PTSD in women is 10.4% and those who develop symptoms are highly susceptible to PTSD endorsement in relation to subsequent traumatic events (Kessler et al., 1995). PTSD is associated with a negative appraisal of subsequent events (Ehlers and Clark, 2000). In accord with Ayers (2004) the vulnerability factor of prior PTSD is likely to interact with birth events to determine appraisal of birth as traumatic and development of a traumatic stress responses. Thus, prepartum PTSD symptoms may continue into the postpartum period and trigger PP-PTSD. In contrast, PP-PTSD may signify the occurrence of first-time posttraumatic stress syndrome onset. Having a difficult childbirth experience (subjective or objective) for some women might be extreme enough to result in PP-PTSD without having prior PTSD symptoms. The childbirth event would then be regarded as the index event of traumatic exposure, although other vulnerability factors are possible. Women with a history of trauma exposure, who do not exhibit prepartum PTSD, may be a special case. Trauma history may reduce the ability to cope with subsequent stressful events (Dekel et al., 2013a), as noted in a sensitization effect (Breslau et al., 1999; Dekel et al., 2013b). Thus, women with trauma history may exhibit a delayed PTSD response induced by childbirth.
Another factor to consider in understanding incidences of PP-PTSD is the passage of time since childbirth. Although the majority of individuals endorse posttraumatic stress symptoms (i.e., PTS) in the immediate aftermath of trauma, symptoms subside for most survivors and a significant minority fails to recover (Bonanno et al., 2005; Shalev, 2009). Previous studies assessed rates of PP-PTSD at different time points ranging from the first days following childbirth to several months, which may account for the wide prevalence rates among the studies.
Thus, in the following systematic review, we examined the prevalence rates of PP-PTSD with a focus on the time period of symptoms endorsement following childbirth. We set to examine PP-PTSD in relation to the endorsement of new posttraumatic stress syndrome as well as in relation to prior PTSD. We also set to examine the risk factors involved in the development of PP-PTSD.
Methods
Study Criteria Selection
The search of literature targeted a wide range of studies, published from January 1980 until 1 August 2016. A search of PubMed and PsychInfo databases was performed using any combination of keywords: posttraumatic stress, posttraumatic stress disorder, traumatic stress with childbirth, PTSD, postpartum, or postnatal. Studies were also found through the “Related Citations” function on PubMed and through the reference lists of previously identified studies. Previous reviews on PTSD following childbirth were another basis to identify studies.
Studies included in our review were quantitative studies, published in English, and met the following criteria: (a) full-term successful births; (b) indication of prevalence of PP-PTSD, at a maximum initial assessment of 6 months postpartum; and (c) PP-PTSD stressor specified in relation to childbirth.
A total of 93 articles were identified via the search criteria. Of this total, 57 articles were removed either for failure to meet criteria or to avoid duplicate samples. The final review included 36 articles, with 32 representing community samples and four representing at-risk groups.
Study Rating System
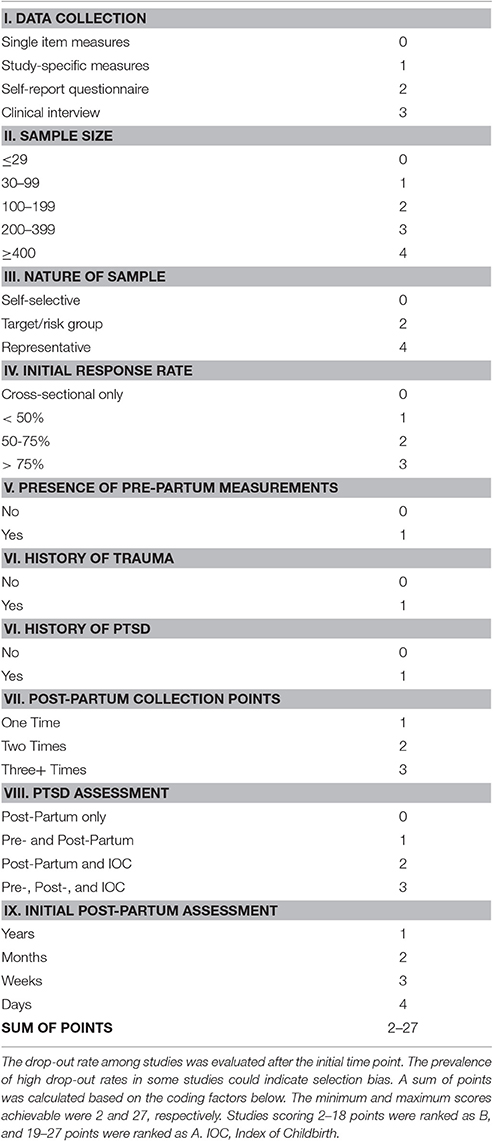
A quality rating system modeled off Andersen et al. (2012) was utilized to assess identified studies. This system is based in part upon the Meta-analysis of Observational Studies in Epidemiology (MOOSE) technique (Stroup et al., 2000). It is designed to assess study quality by accounting for methodological differences among the studies. In this review, several factors were assessed to determine study quality such as sample size, method of data collection, measurement used, etc. Table 1 indicates the full list of factors, their corresponding items, and the point value assigned to each item. For example, the factor Data Collection included four items: single-item measures, study-specific measures, self-report questionnaire, and clinical interview. Single-item measures were assigned a point value of one, leading up to clinical interview, which was assigned a point value of four. Thus, a study would be given a score ranging from one to four for data collection. The sum of each factor resulted in an overall study quality score, ranging from 2 to 27 points.
According to their study quality score, each study was ranked as either A or B. The A category included studies with the highest methodological ranking, and, for the relevance of this review, those that controlled for PTSD symptom endorsement before childbirth (“controlled studies”). The B category included studies that may have received a lower quality score due to smaller sample size, fewer postpartum time assessments, lack of perinatal assessments, etc., or due to less relevance to this review. All studies in B did not control for PTSD before childbirth (“uncontrolled studies”).
Two research assistants analyzed and rated the 36 identified articles. Inter-rater agreement between the research assistants was high and reached 92%. If disagreements in coding arose, the disagreement was discussed and resolved to reach a consensus.
In the next step, we calculated PTSD prevalence rates within studies in Groups A and B by taking into consideration the time of postpartum assessment. In accordance with PTSD DSM-4 (American Psychiatric Association, 2000), PP-PTSD assessed more than 1 month and up to 3 months postpartum was labeled “acute PP-PTSD,” and assessment more than 3 months and up to 6 months postpartum was labeled “chronic PP-PTSD.” In addition, PP-PTSD symptoms measured within 1 month postpartum were labeled postpartum posttraumatic stress, i.e., PP-PTS. PTSD rate for each time point was created by computing the mean PTSD value. We also computed the overall PP-PTSD rate assessed by averaging the time categories (PP-PTS + acute PTSD + chronic PTSD).
Risk Factor Analysis
Risk factors for PP-PTSD, if presented by the studies, were identified and analyzed. To be included in the analysis, risk factors had to be of statistical significance. Each identified risk factor was assigned a point value based on the group rank of the study. For example, a risk factor identified from a Group A study was assigned a point value of two. Risk factors identified from Group B were assigned a point value of one. If multiple studies reported the same risk factor, that risk factor received a summed score.
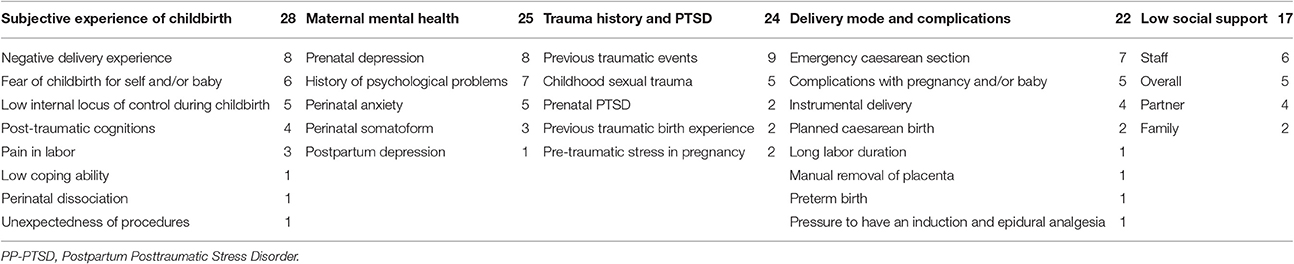
Risk factors of similar nature were then grouped into categories. For example, risk factors such as prenatal depression and perinatal anxiety were grouped under the category “Maternal Mental Health.” Five categories were created. The category score was the sum of the individual risk factors, and was above 15 for each category. A miscellaneous category was added to account for risk factors that did not fall within the five identified categories.
Results
Study Classification
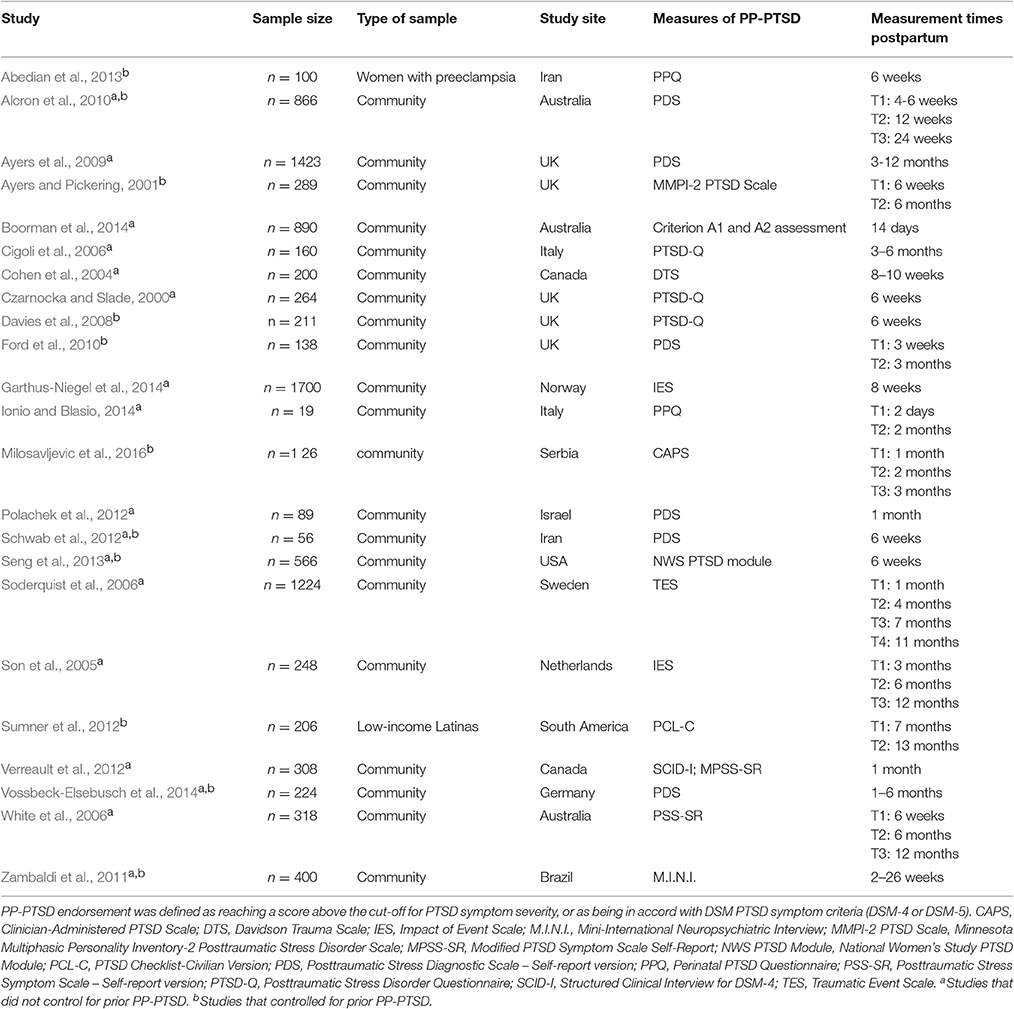
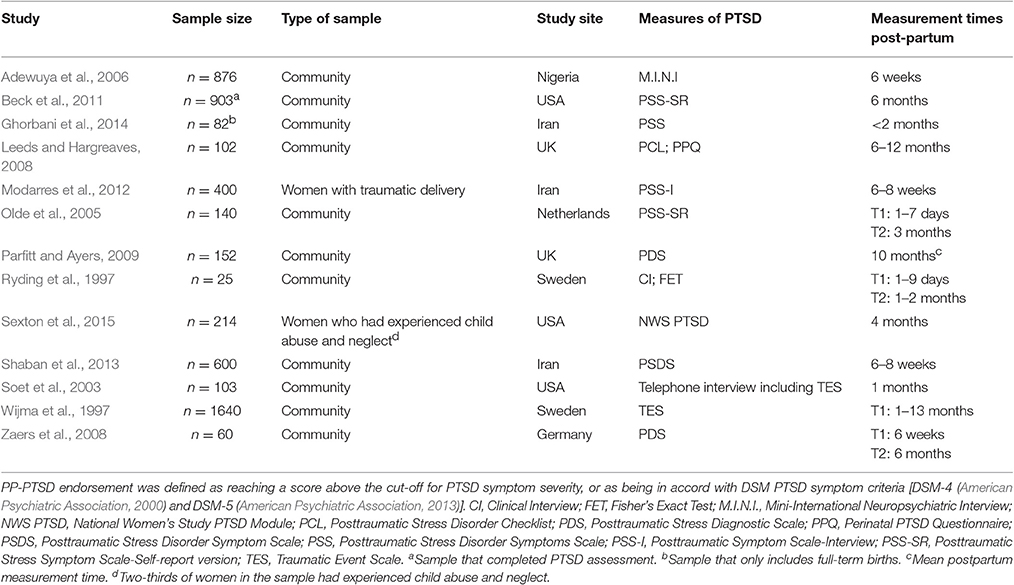
The identified 36 articles meeting inclusion criteria were categorized into groups A and B in accordance with the proposed coding system. Group A included 23 studies which were categorized according to whether they controlled for endorsement of PTSD prior to childbirth (controlled) or not (uncontrolled) (See Table 2). Group B included 13 studies (See Table 3).
PP-PTSD Prevalence
All 36 articles included in this review reported the prevalence of childbirth-related PP-PTSD, with 18 studies also reporting the prevalence of partial PP-PTSD.
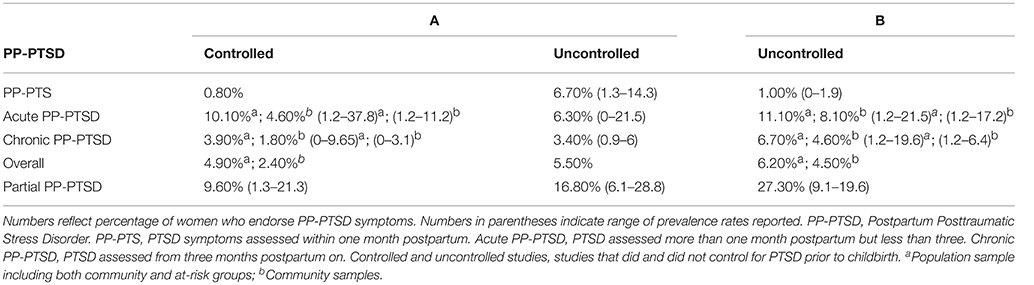
Table 4 presents PP-PTSD prevalence according to group classification (A and B), time of postpartum assessment, and type of sample (community vs. at-risk). As indicated previously: “PP-PTS” noted was for symptoms ≤1 month postpartum; “acute PP-PTSD” for symptoms >1month postpartum but <3 months postpartum; and “chronic PP-PTSD” for symptoms >3 months and ≤6 months. Overall, PP-PTSD and partial PTSD referred to symptoms across time points.
For “Controlled” studies in Group A, the overall PP-PTSD prevalence was 4.9%, including at-risk samples. Though PP-PTS rates were 0.8%, acute PP-PTSD rates were much higher, with 4.6% in community samples and 10.1% including at-risk. Chronic PP-PTSD rates were 1.8% in the community sample and 3.9% including at-risk samples, suggesting a decline in PP-PTSD endorsement. Overall partial PP-PTSD was 9.6%. For example, a controlled community study (N = 211 of primi- and multiparas women who underwent various modes of delivery with healthy outcomes) reported rates of full and partial PP-PTSD at 3.8 and 21.3%, respectively, at 6 weeks postpartum (Davies et al., 2008).
For “Uncontrolled” studies in Group A, the overall PP-PTSD prevalence was 5.5%. Rates of PP-PTS and acute PP-PTSD were similar, at 6.7 and 6.3%, respectively. Again, chronic PP-PTSD rates were lower at 3.4%. The overall partial PP-PTSD rate, as might be expected, was much higher, at 16.8%; three times higher than the rates for overall PP-PTSD. For example, a uncontrolled study (N = 308 of community sample) reported partial and full PP-PTSD rates of 7.6 and 16.6%, respectively, at 1 month (Verreault et al., 2012).
In Group B, the overall PP-PTSD prevalence including at-risk samples was 6.2%. The prevalence rates also varied according to time of assessment, with lowest rates found for PP-PTS and highest for acute PP-PTSD. PP-PTS prevalence was 1.0%, whereas acute PP-PTSD was 8.1% in the community sample and 11.1% when including at-risk groups. Chronic PP-PTSD prevalence was lower than acute, with rates of 4.6% in community samples and 6.7% including at-risk samples. Rates of partial PP-PTSD were highest at 27.3%.
PP-PTSD Risk Factors
Five categories of risk factors were identified: negative perception of childbirth, maternal mental health, trauma history, and PTSD, delivery mode and complications, and low social support. Table 5 presents the categories and their risk factors.
Factors relating to negative subjective experience of childbirth received the highest weighted score of 28 points, and were thus identified as the most potent predictors of PP-PTSD. The most significant risk factor, reported by five studies, was negative delivery experience (Wijma et al., 1997; Son et al., 2005; Zaers et al., 2008; Verreault et al., 2012; Garthus-Niegel et al., 2014). Fear of childbirth for the self and/or baby and low internal locus of control during childbirth were also significant factors noted in this category, and were reported by several studies (Czarnocka and Slade, 2000; Soet et al., 2003; Adewuya et al., 2006; Soderquist et al., 2006; Leeds and Hargreaves, 2008; Garthus-Niegel et al., 2014).
The next most significant group of risk factors included those pertaining to maternal mental health. This group received a weighted score of 25 points. The presence of prenatal depression was the most commonly noted factor within this group, as documented in five studies (Cohen et al., 2004; Soderquist et al., 2006; Leeds and Hargreaves, 2008; Sumner et al., 2012; Shaban et al., 2013). Having a history of psychological problems prior to pregnancy was found to significantly contribute to the endorsement of PP-PTSD as well (Soderquist et al., 2006; Leeds and Hargreaves, 2008; Zaers et al., 2008; Zambaldi et al., 2011; Boorman et al., 2014). Perinatal somatoform and anxiety were also significant factors cited by six studies (Soet et al., 2003; Olde et al., 2005; Zaers et al., 2008; Zambaldi et al., 2011; Verreault et al., 2012; Shaban et al., 2013). Finally, acute postpartum depression symptoms were found to predict later PP-PTSD (Beck et al., 2011).
Factors falling within the trauma history and PTSD category comprised the third highest weighted score of 24 points. A history of trauma exposure of any type was the most commonly reported risk factor as noted in three studies (White et al., 2006; Zaers et al., 2008; Ayers et al., 2009). Childhood sexual trauma in particular was found to be a highly cited factor, as well as pre-traumatic stress in pregnancy (Soderquist et al., 2006; Lev-Wiesel and Daphna-Tekoah, 2010; Verreault et al., 2012; Sexton et al., 2015). As might be expected, the endorsement of PTSD during pregnancy was a strong predictor of PP-PTSD (Seng et al., 2013). Trauma related to interpersonal violence and having a previous traumatic birth experience were other frequently reported factors (Polachek et al., 2012; Sumner et al., 2012).
Risk factors related to delivery mode and complications constituted the fourth highest weighted category of 22 points. Emergency cesarean section and complications with the pregnancy and/or baby were the most cited risk factors in this category, reported by seven studies total (Cohen et al., 2004; Adewuya et al., 2006; Zambaldi et al., 2011; Modarres et al., 2012; Boorman et al., 2014; Vossbeck-Elsebusch et al., 2014; Milosavljevic et al., 2016). Two studies also noted instrumental deliveries as a significant risk factor (Adewuya et al., 2006; Milosavljevic et al., 2016).
The final category pertained to low levels of social support, and received a weighted score of 17 points. Three studies referred to low levels of social support in general as a risk factor (Soet et al., 2003; Ford et al., 2010; Sumner et al., 2012). The remaining studies were more specific in regards to the support group, with one study reporting low family support, three studies reporting low staff support, and three studies reporting low partner support (Czarnocka and Slade, 2000; Cigoli et al., 2006; Parfitt and Ayers, 2009; Beck et al., 2011; Ford and Ayers, 2011). Previous counseling related to childbirth or pregnancy was also a contributing factor (Soderquist et al., 2006).
Finally, we identified common risk factors that did not fit into the noted risk factors categories. These factors largely pertain to demographics and included the risk factors such as young age, low income, primiparity, and multiparity (Zambaldi et al., 2011; Abedian et al., 2013; Boorman et al., 2014; Vossbeck-Elsebusch et al., 2014).
Discussion
Posttraumatic stress syndrome related with the childbirth experience has been largely overlooked. That a mostly voluntary event implicated in reproduction can trigger PP-PTSD does not reconcile with the positive notion of childbirth. Yet, childbirth involves drastic physiological changes of hormonal imbalance, blood and body weight loss, increased cardiac output, and is often accompanied by acute bodily pain and sleep deprivation. Not surprisingly, a full-term delivery with healthy outcomes may nonetheless be associated with threat on bodily integrity and a sense of fear and loss of control.
There are two competing theories on childbirth-related PTSD. First, PP-PTSD signifies amplification of pre-existing traumatic stress symptoms. Second, PP-PTSD indicates a new PTSD onset induced by the childbirth experience rather than continuation of perinatal PTSD. We explored predictions from these theories by analyzing 36 articles reporting the rates of PP-PTSD symptoms associated with the experience of healthy, full-term birth.
Overall, the prevalence rates of PP-PTSD, in its acute form (between 1 and 3 months postpartum) were 5–8% in community samples. The prevalence of clinically significant symptoms of PP-PTSD, was higher, and ranged between 9.6 and 27.3%. It is estimated that four million babies are born in the States each year. While our results suggest that at a minimum only 5 out of 100 women will experience a sort of PP-PTSD, when translated to the larger sample of four million, this is roughly two hundred thousand mothers at-risk.
New PTSD onset following childbirth was noted in the studies reviewed here, suggesting that for some women childbirth can be perceived as a highly stressful experience capable of triggering PTSD without having prior PTSD. In fact, rates of new PTSD onset evident in samples of women without PTSD before childbirth were slightly lower than in samples including women with or without PTSD history, 4.6 vs. 6.3% for acute PP-PTSD in studies of high quality. Although these findings may be attributed to differences in the nature of the samples, we applied a quality approach to compare between the studies. Alternatively, the findings may suggest that for a significant sub-group of women, PTSD symptoms do not carry on from pregnancy to childbirth but rather develop for the first time in the immediate postpartum period. Although several reviews have been conducted on PTSD in relation to childbirth, this is the first attempt to distinguish between syndromes of new and prior PTSD endorsement.
Various risk factors were also reviewed and identified as potentially predictive of the development of PP-PTSD, mainly pre-trauma related factors and peritraumatic aspects related to the childbirth. Although predisposing mental health conditions and prior trauma were associated with subsequent PP-PTSD, peritraumatic factors and early emotional symptoms emerged as the strongest predictor. Obstetrical factors and related complications, which may entail threat to life of mother and/or baby, were ranked as less important. These findings accord with the previous reviews (Andersen et al., 2012) and are also in line with the literature of PTSD in relation to other stressors (Ozer et al., 2003). It has been documented that the subjective experience of the traumatic event is a more important factor in predicting PTSD than its objective stressor severity (Bowman, 1999; Dekel et al., 2016a). Subjective negative childbirth experience, as our data reveals, pertains to having a negative appraisal of the event (primary appraisal) and of one's ability to cope with the stressor (secondary appraisal) (Lazarus, 1981). These kinds of negative appraisals have been linked with the development and endurance of PTSD following traumatic experiences (Dunmore et al., 2001).
Several limitations in this review should be noted. Although identified studies used well-validated measures of PP-PTSD symptoms, whether participants had clinically diagnosed PP-PTSD was assessed by some studies but not in all. While we identified common risk factors for PP-PTSD, the interplay between the factors was not assessed, and there might be other unknown factors that have not been studied yet. Analysis of quantitative studies allowed for study comparison; however, qualitative studies may have offered important information as well. We applied a quality rating to compare and integrate studies, but might have overlooked factors that may bias the results. Although we mainly reviewed community samples, important confounding factors such as age, medical issues during birth, mode of delivery, and peripartum anxiety, were not taken into account when reporting PP-PTSD rates. We included samples derived from different world regions, which offers a broad perspective on PP-PTSD but might create wide variations in prevalence rates. Ideally, we would have targeted large, prospective, longitudinal studies to clarify childbirth-related PTSD with/without PTSD or trauma history and the moderating factor of culture (Dekel et al., 2016b). Future studies are warranted to examine the various pathways for the development of PP-PTSD and its symptom trajectory.
Within the context of these limitations, the current review provides important evidence for the endorsement of PTSD related with childbirth. Although there has been controversy regarding whether PTSD could be induced by childbirth, our findings indicate that a significant sub-group of women with and without prior PTSD may develop PP-PTSD of an enduring nature. The development of PTSD in relation to a relatively predicted event (i.e., birth) during routine clinical care offers the opportunity to potentially identify women at high risk for PP-PTSD and provide specific preventive interventions, both of which are currently lacking. As this study demonstrates, having a negative childbirth experience is an important factor implicated in PP-PTSD. Childbirth accounts may be a useful tool to identify at-risk women in the immediate peripartum period and to intervene accordingly. At a broader level, our findings suggest that by nature women are resilient and cope well with the childbirth experience. Childbirth is not inevitably appraised as traumatic. Examining biological factors underlining positive adaptation and posttraumatic stress reactions is likely to provide insight into this under-researched scientific territory.
Author Contributions
SD supervised coding of articles and data analysis and headed manuscript writing. CS identified and coded articles, completed data analysis, and contributed to manuscript writing. GD identified and coded articles.
Funding
This work was supported by MGH ECOR Claflin Distinguished Scholar Award and the Brain and Behavior Research Foundation (NARSAD) Grant awarded to SD.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Acknowledgments
We thank Ms. Olivia Lanman for assisting with the coding of the reviewed studies.
References
Abedian, Z., Narges, S., Mokhber, N., and Esmaily, H. (2013). Comparing post-traumatic stress disorder in primiparous and multiparous women with preeclampsia. J. Midwifery Reprod. Health 1, 13–18. doi: 10.22038/jmrh.2013.755
Adewuya, A. O., Ologun, Y. A., and Ibigbami, O. S. (2006). Post-traumatic stress disorder after childbirth in Nigerian women: prevalence and risk factors. BJOG 113, 284–288. doi: 10.1111/j.1471-0528.2006.00861.x
Alcron, K. L., O'Donovan, A., Patrick, J. C., Creedy, D., and Devilly, G. J. (2010). A prospective longitudinal study of the prevalence of post-traumatic stress disorder resulting from childbirth events. Psychol. Med. 40, 1849–1859. doi: 10.1017/S0033291709992224
American Psychiatric Association. (2000). Diagnostic and Statistical Manual of Mental Disorders, 4th Edn. Washington, DC: Author.
American Psychiatric Association. (2013). Diagnostic and Statistical Manual of Mental Disorders, 5th Edn. Arlington, VA: Author.
Andersen, L. B., Melvaer, L. B., Videbech, P., Lamont, R. F., and Joergensen, J. S. (2012). Risk factors for developing post-traumatic stress disorder following childbirth: a systematic review. Acta Obstet. Gynecol. Scand. 91, 1261–1272. doi: 10.1111/j.1600-0412.2012.01476.x
Ayers, S. (2004). Delivery as a traumatic event: prevalence, risk factors, and treatment for postnatal posttraumatic stress disorder. Clin. Obstet. Gynecol. 47, 552–567. doi: 10.1097/01.grf.0000129919.00756.9c
Ayers, S., Bond, R., Bertullies, S., and Wijma, K. (2016). The aetiology of post-traumatic stress following childbirth: a meta-analysis and theoretical framework. Psychol. Med. 46, 1121–1134. doi: 10.1017/S0033291715002706
Ayers, S., Harris, R., Sawyer, A., Parfitt, Y., and Ford, E. (2009). Posttraumatic stress disorder after childbirth: analysis of symptom presentation and sampling. J. Affect. Disord. 119, 200–204. doi: 10.1016/j.jad.2009.02.029
Ayers, S., and Pickering, A. D. (2001). Do women get posttraumatic stress disorder as a result of childbirth? A prospective study of incidence. Birth 28, 111–118. doi: 10.1046/j.1523-536X.2001.00111.x
Beck, C. T., Gable, R. K., Sakala, C., and Declercq, E. R. (2011). Posttraumatic stress disorder in new mothers: results from a two-stage U.S. national survey. Birth 38, 216–227. doi: 10.1111/j.1523-536X.2011.00475.x
Bonanno, G. A., Rennicke, C., and Dekel, S. (2005). Self-enhancement among high-exposure survivors of the September 11th terrorist attack: resilience or social maladjustment? J. Pers. Soc. Psychol. 88, 984–998. doi: 10.1037/0022-3514.88.6.984
Boorman, R. J., Devilly, G. J., Gamble, J., Creedy, D. K., and Fenwick, J. (2014). Childbirth and criteria for traumatic events. Midwifery 30, 255–261. doi: 10.1016/j.midw.2013.03.001
Bowman, M. L. (1999). Individual differences in posttraumatic distress: problems with the DSM-IV model. Can. J. Psychiatry 44, 21–33. doi: 10.1177/070674379904400103
Breslau, N., Chilcoat, H. D., Kessler, R. C., and Davis, G. C. (1999). Previous exposure to trauma and PTSD effects of subsequent trauma: results from the detroit area survey of trauma. Am. J. Psychiatry 156, 902–907. doi: 10.1176/ajp.156.6.902
Cigoli, V., Gilli, G., and Saita, E. (2006). Relational factors in psychopathological responses to childbirth. J. Psychosom. Obstet. Gynaecol. 27, 91–97. doi: 10.1080/01674820600714566
Cohen, M. M., Ansara, D., Schei, B., Stuckless, N., and Stewart, D. E. (2004). Posttraumatic stress disorder after pregnancy, labor, and delivery. J. Womens Health (Larchmt). 13, 315–324. doi: 10.1089/154099904323016473
Czarnocka, J., and Slade, P. (2000). Prevalence and predictors of post-traumatic stress symptoms following childbirth. Br. J. Clin. Psychol. 39(Pt 1), 35–51. doi: 10.1348/014466500163095
Davies, J., Slade, P., Wright, I., and Stewart, P. (2008). Posttraumatic stress symptoms following childbirth and mothers' perceptions of their infants. Infant Ment. Health J. 29, 537–554. doi: 10.1002/imhj.20197
Dekel, S., Mandl, C., and Solomon, Z. (2013b). Is the Holocaust implicated in posttraumatic growth in second-generation Holocaust survivors? A prospective study. J. Trauma. Stress 26, 530–533. doi: 10.1002/jts.21836
Dekel, S., Solomon, Z., and Ein-Dor, T. (2016a). PTSD symptoms lead to modification in the memory of the trauma: a prospective study of former prisoners of war. J. Clin. Psychiatry 77, e290–e296. doi: 10.4088/JCP.14m09114
Dekel, S., Solomon, Z., and Rozenstreich, E. (2013a). Secondary salutogenic effects in veterans whose parents were Holocaust survivors? J. Psychiatr. Res. 47, 266–271. doi: 10.1016/j.jpsychires.2012.10.013
Dekel, S., Stanger, V., Georgakopoulos, E. R., Stuebe, C. M., and Dishy, G. A. (2016b). Peripartum depression, traditional culture, and Israeli society. J. Clin. Psychol. 72, 784–794. doi: 10.1002/jclp.22360
Dunmore, E., Clark, D. M., and Ehlers, A. (2001). A prospective investigation of the role of cognitive factors in persistent posttraumatic stress disorder (PTSD) after physical or sexual assault. Behav. Res. Ther. 39, 1063–1084. doi: 10.1016/S0005-7967(00)00088-7
Ehlers, A., and Clark, D. M. (2000). A cognitive model of posttraumatic stress disorder. Behav. Res. Ther. 38, 319–345. doi: 10.1016/S0005-7967(99)00123-0
Ford, E., and Ayers, S. (2011). Support during birth interacts with prior trauma and birth intervention to predict postnatal post-traumatic stress symptoms. Psychol. Health 26, 1553–1570. doi: 10.1080/08870446.2010.533770
Ford, E., Ayers, S., and Bradley, R. (2010). Exploration of a cognitive model to predict post-traumatic stress symptoms following childbirth. J. Anxiety Disord. 24, 353–359. doi: 10.1016/j.janxdis.2010.01.008
Garthus-Niegel, S., von Soest, T., Knoph, C., Simonsen, T. B., Torgersen, L., and Eberhard-Gran, M. (2014). The influence of women's preferences and actual mode of delivery on post-traumatic stress symptoms following childbirth: a population-based, longitudinal study. BMC Pregnancy Childbirth 14:191. doi: 10.1186/1471-2393-14-191
Ghorbani, M., Dolatian, M., Shams, J., and Alavi-Majd, H. (2014). Anxiety, post-traumatic stress disorder and social supports among parents of premature and full-term infants. Iran. Red Cresecent Med. J. 16:e13461. doi: 10.5812/ircmj.13461
Grekin, R., and O'Hara, M. W. (2014). Prevalence and risk factors of postpartum posttraumatic stress disorder: a meta-analysis. Clin. Psychol. Rev. 34, 389–401. doi: 10.1016/j.cpr.2014.05.003
Ionio, C., and Blasio, P. D. (2014). Post-traumatic stress symptoms after childbirth and early mother—child interactions: an exploratory study. J. Reprod. Infant Psychol. 32, 163–181. doi: 10.1080/02646838.2013.841880
Kessler, R. C., Sonnega, A., Bromet, E., Hughes, M., and Nelson, C. B. (1995). Posttraumatic stress disorder in the National Comorbidity Survey. Arch. Gen. Psychiatry 52, 1048–1060. doi: 10.1001/archpsyc.1995.03950240066012
Lazarus, R. S. (1981). “The stress and coping paradigm,” in Models for Clinical Psychopathology, eds C. C. D. Eisdorfer, A. Kleinman, and P. Maxim (New York, NY: Spectrum), 177–214.
Leeds, L., and Hargreaves, I. (2008). The psychological consequences of childbirth. J. Reprod. Infant Psychol. 26, 108–122. doi: 10.1080/02646830701688299
Lev-Wiesel, R., and Daphna-Tekoah, S. (2010). The role of peripartum dissociation as a predictor of posttraumatic stress symptoms following childbirth in Israeli Jewish women. J. Trauma Dissociation 11, 266–283. doi: 10.1080/15299731003780887
Milosavljevic, M., Lecic Tosevski, D., Soldatovic, I., Vukovic, O., Miljevic, C., Peljto, A., et al. (2016). Posttraumatic stress disorder after vaginal delivery at primiparous women. Sci. Rep. 6:27554. doi: 10.1038/srep27554
Modarres, M. A., Afrasiabi, S., Rahnama, P., and Montazeri, A. (2012). Prevalence and risk factors of childbirth-related post-traumatic stress symptoms. BMC Pregnancy Childbirth 12:88. doi: 10.1186/1471-2393-12-88
O'Hara, M. W., and McCabe, J. E. (2013). Postpartum depression: current status and future directions. Annu. Rev. Clin. Psychol. 9, 379–407. doi: 10.1146/annurev-clinpsy-050212-185612
Olde, E., van der Hart, O., Kleber, R. J., van Son, M. J., Wijnen, H. A., and Pop, V. J. (2005). Peritraumatic dissociation and emotions as predictors of PTSD symptoms following childbirth. J. Trauma Dissociation 6, 125–142. doi: 10.1300/J229v06n03_06
Olde, E., van der Hart, O., Kleber, R., and van Son, M. (2006). Posttraumatic stress following childbirth: a review. Clin. Psychol. Rev. 26, 1–16. doi: 10.1016/j.cpr.2005.07.002
Ozer, E. J., Best, S. R., Lipsey, T. L., and Weiss, D. S. (2003). Predictors of posttraumatic stress disorder and symptoms in adults: a meta-analysis. Psychol. Bull. 129, 52–73. doi: 10.1037/0033-2909.129.1.52
Parfitt, Y., and Ayers, S. (2009). The effect of post-natal symptoms of post-traumatic stress and depression on the couple's relationship and parent-baby bond. J. Reprod. Infant Psychol. 27, 127–142. doi: 10.1080/02646830802350831
Polachek, I. S., Harari, L. H., Baum, M., and Strous, R. D. (2012). Postpartum post-traumatic stress disorder symptoms: the uninvited birth companion. Isr. Med. Assoc. J. 14, 347–353.
Ryding, E. L., Wijma, B., and Wijma, K. (1997). Posttraumatic stress reactions after emergency cesarean section. Acta Obstet. Gynecol. Scand. 76, 856–861.
Schwab, W., Marth, C., and Bergant, A. M. (2012). Post-traumatic stress disorder post partum: the impact of birth on the prevalence of post-traumatic stress disorder (PTSD) in multiparous women. Geburtshilfe Frauenheilkd. 72, 56–63. doi: 10.1055/s-0031-1280408
Seng, J. S., Sperlich, M., Low, L. K., Ronis, D. L., Muzik, M., and Liberzon, I. (2013). Childhood abuse history, posttraumatic stress disorder, postpartum mental health, and bonding: a prospective cohort study. J. Midwifery Womens Health 58, 57–68. doi: 10.1111/j.1542-2011.2012.00237.x
Sexton, M. B., Hamilton, L., McGinnis, E. W., Rosenblum, K. L., and Muzik, M. (2015). The roles of resilience and childhood trauma history: main and moderating effects on postpartum maternal mental health and functioning. J. Affect. Disord. 174, 562–568. doi: 10.1016/j.jad.2014.12.036
Shaban, Z., Dolatian, M., Shams, J., Alavi-Majd, H., Mahmoodi, Z., and Sajjadi, H. (2013). Post-traumatic stress disorder (PTSD) following childbirth: prevalence and contributing factors. Iran. Red Crescent Med. J. 15, 177–182. doi: 10.5812/ircmj.2312
Shalev, A. (2009). Posttraumatic stress disorder and stress-related disorders. Psychiatr. Clin. North Am. 32, 687–704. doi: 10.1016/j.psc.2009.06.001
Soderquist, J., Wijma, B., and Wijma, K. (2006). The longitudinal course of post-traumatic stress after childbirth. J. Psychosom. Obstet. Gynaecol. 27, 113–119. doi: 10.1080/01674820600712172
Soet, J. E., Brack, G. A., and DiIorio, C. (2003). Prevalence and predictors of women's experience of psychological trauma during childbirth. Birth 30, 36–46. doi: 10.1046/j.1523-536X.2003.00215.x
Son, M. V., Verkerk, G., Hart, O. V. D., Komproe, I., and Pop, V. (2005). Prenatal depression, mode of delivery and perinatal dissociation as predictors of postpartum posttraumatic sress: an empirical study. Clin. Psychol. Psychother. 12, 297–312. doi: 10.1002/cpp.446
Stroup, D. F., Berlin, J. A., Morton, S. C., Olkin, I., Williamson, G. D., Rennie, D., et al. (2000). Meta-analysis of observational studies in epidemiology: a proposal for reporting. Meta-analysis Of Observational Studies in Epidemiology (MOOSE) group. JAMA 283, 2008–2012. doi: 10.1001/jama.283.15.2008
Sumner, L. A., Wong, L., Schetter, C. D., Myers, H. F., and Rodriguez, M. (2012). Predictors of posttraumatic stress disorder symptoms among low-income latinas during pregnancy and postpartum. Psychol. Trauma 4, 196–203. doi: 10.1037/a0023538
Verreault, N., Da Costa, D., Marchand, A., Ireland, K., Banack, H., Dritsa, M., et al. (2012). PTSD following childbirth: a prospective study of incidence and risk factors in Canadian women. J. Psychosom. Res. 73, 257–263. doi: 10.1016/j.jpsychores.2012.07.010
Vossbeck-Elsebusch, A. N., Freisfeld, C., and Ehring, T. (2014). Predictors of posttraumatic stress symptoms following childbirth. BMC Psychiatry 14:200. doi: 10.1186/1471-244X-14-200
White, T., Matthey, S., Boyd, K., and Barnett, B. (2006). Postnatal depression and post-traumatic stress after childbirth: prevalence, course and co-occurrence. J. Reprod. Infant Psychol. 24, 107–120. doi: 10.1080/02646830600643874
Wijma, K., Soderquist, J., and Wijma, B. (1997). Posttraumatic stress disorder after childbirth: a cross sectional study. J. Anxiety Disord. 11, 587–597. doi: 10.1016/S0887-6185(97)00041-8
Williams, C., Patricia Taylor, E., and Schwannauer, M. (2016). A web-based survey of mother-infant bond, attachment experiences, and metacognition in posttraumatic stress following childbirth. Infant Ment. Health J. 37, 259–273. doi: 10.1002/imhj.21564
Yildiz, P. D., Ayers, S., and Phillips, L. (2017). The prevalence of posttraumatic stress disorder in pregnancy and after birth: a systematic review and meta-analysis. J. Affect. Disord. 208, 634–645. doi: 10.1016/j.jad.2016.10.009
Zaers, S., Waschke, M., and Ehlert, U. (2008). Depressive symptoms and symptoms of post-traumatic stress disorder in women after childbirth. J. Psychosom. Obstet. Gynaecol. 29, 61–71. doi: 10.1080/01674820701804324
Keywords: postpartum PTSD, childbirth, systematic review, posttraumatic stress, delivery, obstetrics, psychopathology, resilience
Citation: Dekel S, Stuebe C and Dishy G (2017) Childbirth Induced Posttraumatic Stress Syndrome: A Systematic Review of Prevalence and Risk Factors. Front. Psychol. 8:560. doi: 10.3389/fpsyg.2017.00560
Received: 23 November 2016; Accepted: 27 March 2017;
Published: 11 April 2017.
Edited by:
Alessandra Simonelli, University of Padua, ItalyReviewed by:
Ana Lúcia R. Moreira, Centro Hospitalar do Oeste, PortugalSerge Brand, University of Basel, Switzerland
Copyright © 2017 Dekel, Stuebe and Dishy. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Sharon Dekel, sdekel@mgh.harvard.edu
 Sharon Dekel
Sharon Dekel Caren Stuebe
Caren Stuebe Gabriella Dishy
Gabriella Dishy