- Departamento de Psicologia, Pontifícia Universidade Católica do Rio de Janeiro, Rio de Janeiro, Brazil
The incidence of obesity has reached epidemic proportions, affecting 30% of the adult population globally. During the last decade, the rising rates of obesity in developing countries has been particularly striking. One potential consequence of obesity is a decline in quality of life (QoL). Thus, the objective of the present study was to investigate the possible relationship between obesity, defined by body mass index (BMI), and QoL, evaluated using the short version of the World Health Organization Quality of Life (WHOQOL) scale in a Brazilian population. The sample consisted of 30 men and 30 women, divided into three groups according to BMI: normal weight, obese, and morbidly obese. All of the subjects responded to the WHOQOL inventories. The results indicated that the groups with lower BMIs had better QoL than the groups with higher BMIs. Being overweight interfered with QoL equally in both sexes, with no difference found between men and women. The results indicate the necessity of multidisciplinary care of obese individuals.
Introduction
Obesity is characterized by the excessive accumulation of body fat relative to lean mass. Its prevalence reached important proportions (Ng et al., 2014), being one of the main problems that face public health in modern societies (Halpern and Mancini, 2003). During the last decade, studies showed that obesity has increased in developing countries (Friedrich, 2002; Popkin et al., 2012). Obesity increases the risk of several chronic diseases, such as diabetes mellitus, cardiovascular and cerebrovascular disease, coagulation alterations, degenerative articulation disease, neoplasias, and sleep apnea, among others (Dixon, 2010; Vucenik and Stains, 2012; Ojeda et al., 2014). Regarding the relationship between obesity and mortality, a recent study showed an increased risk only for patients with a higher grade of obesity (Flegal et al., 2013). However, most of the results published highlighted that obese patients have an increase in mortality (Must et al., 1999; Adams et al., 2006; Guh et al., 2009).
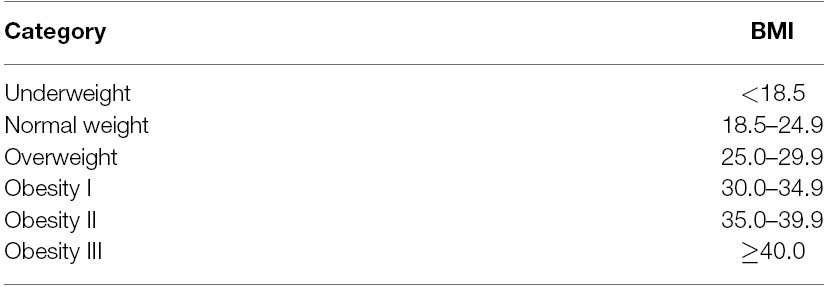
The most commonly used method to assess obesity in adults is the body mass index (BMI). BMI is calculated as body weight (in kilograms) divided by the square of height (in meters). BMI is highly correlated with body fat, but it does not directly measure the proportion of fat. Table 1 presents the classification of BMIs according to the World Health Organization. Subjects are considered obese, which is implicated in functional and health deficits, when they present a BMI between 30 and 40 kg/m2, a range that varies only in the degree of illness.
Obesity is considered as a multifactorial condition, implicating medical, psychiatric, and social aspects. According to Dobrow et al. (2002), obesity is a behavioral disorder that reflects excess food intake compared with energy expenditure; therefore, the genetic contribution to the initiation and maintenance of obesity needs to be considered.
The genetic predisposition to obesity can be expressed in different degrees, either higher or lower, but environmental factors also play a role (Silventoinen et al., 2010; Dubois et al., 2012; Blakemore and Buxton, 2014). The biological/environmental model rather than the psychological model best explains the behaviors that lead to obesity, although its consequences affect psychological variables. According to Dobrow et al. (2002), several studies have revealed high correlations between obesity, depression, and low self-esteem.
Regardless of the specific causes of obesity, its psychological aspects are important when considering the quality of life (QoL) of obese individuals. Studies showed that obese individuals are negatively impacted by judgments and direct and indirect criticisms from others (for review, see Puhl and Heuer, 2009). Thus, negative feelings about oneself and the world often occur, causing anxiety and depression. Negative personal beliefs about inferiority are common in obese individuals (Abilés et al., 2010; Luppino et al., 2010; Son and Kim, 2012). Additionally, excess body weight can cause muscle pain, articulation pain, and discomfort. Because the obese body is heavy and bulky, it expends more energy to move, consequently resulting in the need to rest more often.
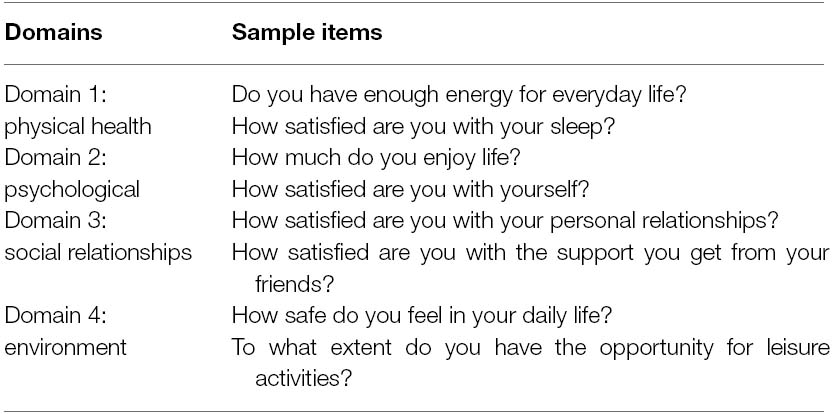
The World Health Organization defines QoL as an individual’s perception of his or her position in life within the context of the culture and value systems in which he or she lives and relative to his or her objectives, expectancies, patterns, and preoccupations. QoL encompasses (1) physical aspects, such as pain, fatigue, energy, sleep, and rest, (2) psychological aspects, such as self-esteem, memory, positive and negative feelings, and perceptions of body image and appearance, (3) social aspects that principally regard personal relationships, and (4) environmental aspects, such as security, finances, leisure, and information (World Health Organization, 1996; Table 2). Studies on obesity and QoL suggest a possible interaction between these two variables (Hlatky et al., 2010; Buttitta et al., 2014; McLaughlin and Hinyard, 2014), in which physical, medical, and cultural aspects that are related to obesity are directly reflected by scores on evaluations of QoL. Illnesses associated with being overweight, the difficulties and embarrassment that obese individuals often experience, and cultural beliefs about beauty, functionality, productivity, and personality attributes (e.g., self-control and perseverance) can negatively interfere with the way of life of obese people.
Even with some authors suggesting an influence of the cultural and ethnic context (Ritenbaugh, 1982; Perez and Warren, 2011; Cox et al., 2011), most studies demonstrating a relationship between QoL and obesity were conducted with North American and European populations. The few studies exploring this relationship in developing countries show contradictory results regarding the association between obesity and impaired QoL (e.g., Lee et al., 2012 in Malaysia; Boodai and Reilly, 2013 in Kuwait; Jalali-Farahani et al., 2013 in Iran). The discrepancy in findings was explained due to cultural differences in attitudes and stigma toward obesity, differences of social expectations for body size and differences regarding social norms. The few studies exploring the relationship between BMI and QoL in Brazil also had contradictory results. Adolescents (Turco et al., 2013) and women (Horta et al., 2013) with chronic non-communicable diseases experienced a similar impact of weight on QoL to samples in developing countries (QoL was negatively influenced by higher BMI). However, an interesting cross-cultural study involving Brazilian and Austrian women with Polycystic Ovary Syndrome demonstrated that for the Brazilian group, obesity was the factor having less impact on QoL, in contrast to the Austrian group, highlighting an influence of the cultural context on the obesity/QoL relationship (Hashimoto et al., 2003). The results of these studies show that the impact of weight on QoL is still unclear for the Brazilian population. Moreover, the specificity of the groups studied does not allow generalizing the results, highlighting the need for further exploration of the impact of BMI on QoL in the Brazilian population.
Gender has been shown to be another factor influencing the QoL burden of obesity. The existing literature indicates that the QoL of women and men is differentially impacted by excessive body weight, with a more impaired QoL in women than in men (Jia and Lubetkin, 2005; Bentley et al., 2011; Korhonen et al., 2014). Choo et al. (2014) showed similar results in a Korean population and suggested that sociocultural influences explained these findings. In fact, in various societies worldwide thinness is valued, resulting in pressure for individuals to monitor their body weight (for review see, Hesse-Biber et al., 2006).
The main objective of the present study was to investigate for the first time in an adult Brazilian population the relationship between QoL and obesity, testing the hypothesis that obesity would be associated with impaired QoL in this population differently in comparison to the results obtained in developed countries. The study also investigated the possible effect of gender on the relationship between obesity and QoL, testing the hypothesis that the influence of weight on QoL would differ between men and women.
Materials and Methods
Subjects
Sixty subjects, aged 20–60 years, were included in the study and divided into three groups (n = 20 per group; 10 men and 10 women) that were matched by age.
Weight and height were self-reported and used to calculate BMI, using the standard BMI formula of weight in kilos divided by height squared in meters (kg/height2). Subjects with BMIs between 18.5 and 24.9, which is considered normal, were included in the first group. The second group was composed of subjects who presented BMIs between 30.0 and 39.9, which are considered degrees I and II of obesity. The third group was composed of subjects with a BMI above 40.0, which is considered morbid obesity.
Tools
To evaluate the QoL for each participant, the World Health Organization Quality of Life-Brief (WHOQOL-Brief) instrument was used, which was translated into Portuguese and validated for the Brazilian population (Fleck et al., 2000). The WHOQOL-Brief consists of 26 questions (two general questions that evaluate QoL and 24 questions that represent specific items in the physical, psychological, social, and environmental domains). This instrument also has a cover page that collects general information about the participant, such as age, sex, weight and height (to calculate the BMI), and health problems.
Procedure
The participants were recruited at the Service of Applied Psychology of the Department of Psychology at PUC-Rio.
All subjects were informed about data confidentiality and anonymity before they responded to the questionnaire. The questionnaires were individually applied, and any doubts or questions about the study were clarified by the researcher.
Statistical Analysis
Group differences in the total scores on the WHOQOL-Brief and each of the domains were analyzed using two-way analysis of variance (ANOVA; 3 × 2). The first factor was BMI (normal, obese, or morbidly obese), and the second factor was gender (male or female). The focus of interest in the analysis is the comparison between weight categories (main effect of BMI), with the gender × weight interactions being secondary interests. The same analysis was performed for the number of illnesses reported by the subjects. In both analyses, significant results were followed up with post hoc comparisons using Student’s t-test.
Ethical Consideration
All participants provided informed consent before taking part in the study. The study was approved by the Ethical Review Board Committee from Pontifícia Universidade Católica from Rio de Janeiro and was conducted in accordance with the Declaration of Helsinki.
Results
Figure 1 presents the mean (±SEM) of the total score and score on each domain of the WHOQOL in men and women with normal weight, obesity, and morbid obesity.
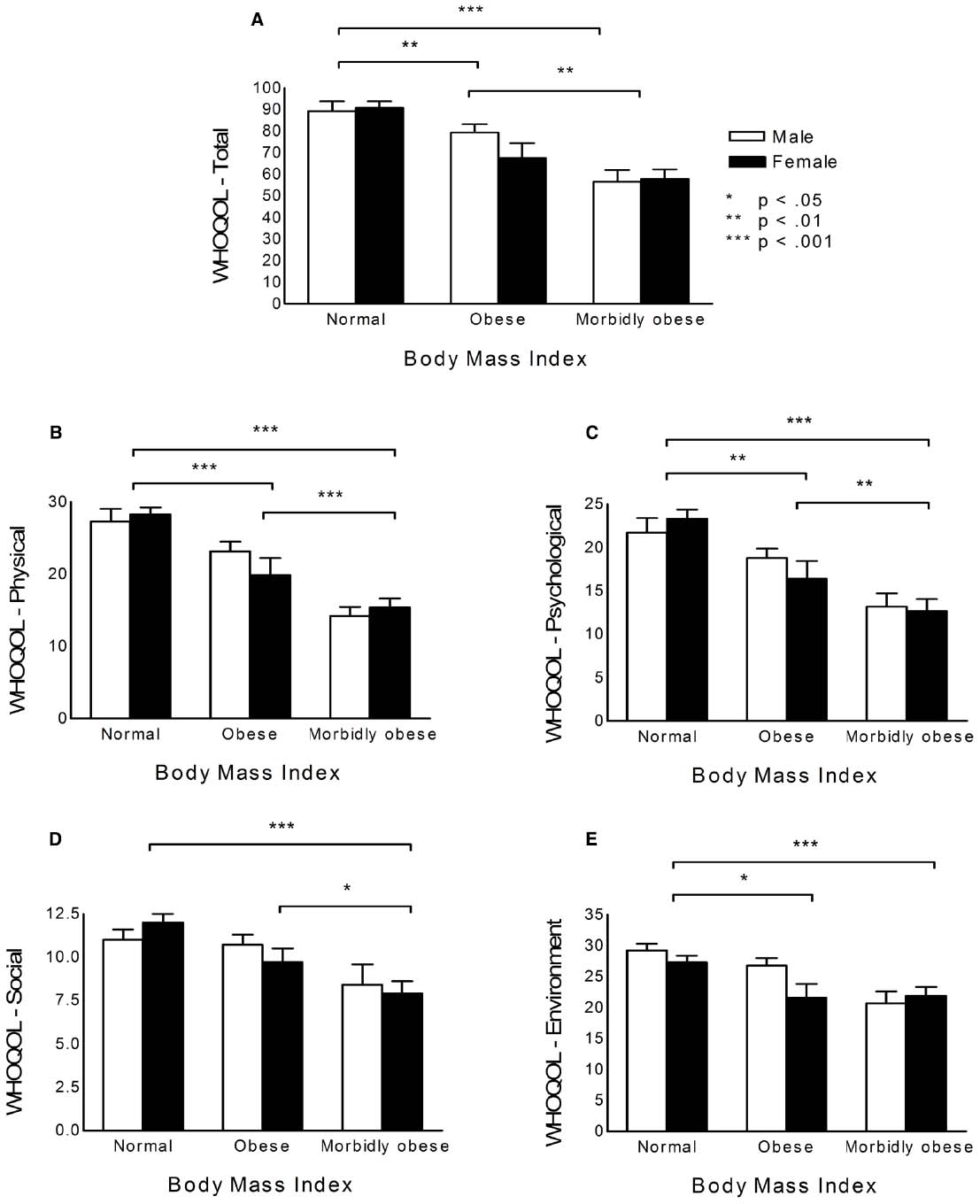
Figure 1. Quality of life according to BMI ranges and gender. (A) WHOQOL total scores. (B) Physical domain. (C) Psychological domain. (D) Social domain. (E) Environment domain.
The results were similar for the total scores and domain scores, revealing a main effect of BMI (total: F2,54 = 22.76, p < 0.001; physical: F2,54 = 35.22, p < 0.001; psychological: F2,54 = 19.93, p < 0.001; social: F2,54 = 9.70, p < 0.001; environmental: F2,54 = 10.24, p < 0.001), but no effect of gender (total: F1,54 = 0.53, p = 0.469; physical: F1,54 = 0.07, p = 0.793; psychological: F1,54 = 0.12, p = 0.727; social: F1,54 = 0.07, p = 0.791; environmental: F1,54 = 2.43, p = 0.124), and no interaction between factors (total: F2,54 = 1.25, p = 0.294, physical: F2,54 = 1.29, p = 0.285; psychological: F2,54 = 0.87, p = 0.423; social: F2,54 = 0.92, p = 0.404; environmental: F2,54 = 2.15, p = 0.126).
For total scores and physical and psychological domain scores, the post hoc comparisons revealed that the participants with normal weight displayed higher QoL compared with obese individuals (total: p = 0.001; physical: p < 0.001; psychological: p = 0.002) and morbidly obese individuals (total: p < 0.001; physical: p < 0.001; psychological: p < 0.001), and obese individuals displayed higher QoL compared with morbidly obese individuals (total: p = 0.001; physical: p < 0.001; psychological: p = 0.003). For the social domain, morbidly obese individuals displayed lower QoL compared with normal weight individuals (p < 0.001) and obese individuals (p = 0.010), but the latter two groups did not differ from each other (p = 0.096). For the environmental domain, individuals with normal weight displayed better QoL compared with obese individuals (p = 0.011) and morbidly obese individuals (p < 0.001). The latter two groups did not differ from each other (p = 0.065). These results are shown in Figure 1.
The ANOVA for number of illnesses revealed significant effects of BMI (F2,54 = 12.19, p < 0.001) and gender (F1,54 = 4.57, p = 0.037) but no interaction between these factors (F2,54 = 0.30, p = 0.740). The post hoc comparisons indicated a greater number of illnesses in women than in men (p = 0.037) and a smaller number of illnesses in individuals with normal weight compared with obese (p = 0.002) and morbidly obese (p < 0.001) individuals.
Discussion
The results indicated an association between an increase in BMI and a decrease in QoL in all domains of the WHOQOL-Brief. For total scores and scores on the physical and psychological domains, the results suggested a linear reduction of QoL with an increase in BMI. The analysis also suggested an increase in the number of comorbidities with an increase in BMI.
The findings with global scores on the WHOQOL-Brief supported previous studies that reported a negative linear relationship between QoL and elevated BMI (Kushner and Foster, 2000; Taylor et al., 2013; Ul-Haq et al., 2013; for review, see Kolotkin et al., 2001). However, these results are in contrast with our hypothesis of cultural differences. These findings can be explained by recent changes observed regarding body image in Brazil. In fact, esthetic ideals in the Brazilian society have been through a progressive transition from a curvier to a thinner body shape, closer to the beauty ideal of European and North American societies (Goldenberg, 2010; Forbes et al., 2012). Following these changes regarding beauty ideal, the stigma toward obesity increased, with greater valorization of thinness (Oliveira and Hutz, 2010). This sociocultural context can explain the negative impact of BMI on QoL.
In contrast to previous studies (Garner et al., 2012; Choo et al., 2014; Korhonen et al., 2014), there was no effect of gender on this relationship. This discrepancy may be explained by sociocultural differences, such as the specific values of the Brazilian culture regarding body image, given that the role of these contextual variables has already been suggested in the relationships among gender, BMI, and QoL (Choo et al., 2014). Studies in the last decade highlighted that Brazilian men are also subject of a sociocultural pressure regarding body image (Oliveira and Hutz, 2010). Kakeshita and Almeida (2008) highlighted the impact of this form of social pressure on men, indicating that both men and women were dissatisfied with their body size and desired leaner bodies.
The results with regard to the different domains also indicated a relationship between elevated BMI and poor QoL. The physical aspect of QoL was negatively correlated with BMI. This domain considers such characteristics as pain, sleep, and the capacity to perform daily activities. Stone and Broderick (2012) reported that BMI and pain were positively correlated, and others reported an association between obesity and sleep disorders (Lam et al., 2012; Ryan et al., 2014). In a recent review of the literature, Backholer et al. (2012) concluded that greater difficulties in daily activities were related to weight gain.
The results with regard to the psychological domain (i.e., self-esteem, body image, and negative and positive feelings) indicated that QoL declined with an increase in weight, which is consistent with previous studies (Kushner and Foster, 2000; Taylor et al., 2013). As highlighted by Wee et al. (2013), the stigma associated with obesity has an impact on various dimensions of QoL. The influence of obesity on psychological aspects, including self-esteem, body image, and emotional state, has been reported in the literature. These factors are influenced by the stigma associated with being overweight and obesity (Friedman et al., 2005; Thomas et al., 2010; Puhl and King, 2013). The stigma associated with obesity also appears to be an important factor in the decline of the social aspect of QoL of obese individuals (Wee et al., 2013). The social domain data revealed that self-evaluations of relationships and social support are negatively influenced by an increase in weight. These results can be explained by the marginalization of people who are overweight or obese. Different socio-epidemiological studies have highlighted the importance of social support for the well-being of individuals (Cummins et al., 2005; Poortinga, 2006). In fact, because of the stigma associated with obesity, people who are overweight or obese have difficulty maintaining social and professional relationships (Morris, 2007) and friendships (Ali et al., 2012). Social norms of body weight changed in Brazil during the last decades, closer to a European and North American body ideal, increasing the stigma toward obesity and influencing the impact of BMI on QoL.
The environmental aspects of QoL focus on physical safety with regard to access to transportation, leisure activities, and the availability of medico-social care. The present study corroborates the results in the literature, demonstrating a negative impact of elevated BMI on the perception of environmental characteristics (Poortinga, 2006). With regard to the social and environmental domains of QoL, the results did not show a linear relationship with BMI and may reflect a “dose-response effect.” According to McLaughlin and Hinyard (2014), when QoL is significantly reduced because of obesity, additional weight gain has little influence on the individual’s perceptions.
The present study also explored the presence of comorbidities in obese patients. We found that the number of illnesses was accentuated by increases in weight, regardless of gender. This result is consistent with recent studies on the relationship between obesity and other physical illnesses, which have reported that the number of pathologies presented by people who are overweight or obese increases with BMI (Dixon, 2010; Vucenik and Stains, 2012; Ojeda et al., 2014). The results also showed that women presented more illnesses than men. The difference between men and women in the number of health problems can be explained by the global disparity between genders with regard to health, suggesting that women are more prone to develop illnesses than men because of social, cultural, and economic reasons (World Health Organization, 2009).
The present study has some limitations. Similar to the majority of such studies (Yan et al., 2004), the groups included individuals with varying ages. Ideally, age would be included as an independent variable, with different groups according to age, but this would impact recruitment and study feasibility. Future studies that examine the link between obesity and QoL in young adults compared with older adults should be conducted to explore possible age factors. Additionally, BMI was calculated based on self-reported information, which, according to Stommel and Schoenborn (2009), can cause differences between the calculated BMI and real BMI. Future studies that use BMI should directly obtain the information that is necessary to calculate BMI. The lack of an overweight category can also be seen as a limitation of the study. However, previous studies showed small differences in QoL between this group and normal weight people (Hassan et al., 2003; Jia and Lubetkin, 2005). Another limitation of this study is the sample size. Nevertheless, the sample was sufficiently large to find group differences.
The present study is the first exploring the relationship between QoL and obesity in the adult population in Brazil. Only two studies exploring this relationship in Brazil have been published. Turco et al. (2013) compared obese and eutrophic adolescents using the PedsQL (Varni et al., 1999, Brazilian version by Klatchoian et al., 2008). They highlighted that obese adolescents had worse QoL compared to the eutrophic group across all domains evaluated. Horta et al. (2013) explored overweighed adult and elderly women with chronic non-communicable disease, using the WHOQOL-brief and showed that the “social relationship” domain is the one that contributed the most to QoL, followed by the “physical” domain. Our study replicated the results obtained by these two publications, extending the conclusions to another population (adult men and women).
This study is also one of the few exploring the relationship between QoL in a developing country. This relationship has already been extensively demonstrated in North American and European populations, but our results allow us to affirm that this relationship remains the same in a different social and cultural context. Additionally, the results suggest the possible influence of the sociocultural context on the relationship between weight, QoL and gender. Future studies that utilize a cross-cultural design may help to understand the contextual factors that are involved in the impact of obesity on QoL in relation to other variables, such as gender. We also suggest further explorations of the correlation between demographic information, such as socio-economic status, and the relationship between obesity/QoL, in particular for studies conducted in countries with higher inequality.
Our results indicate that an elevated BMI is associated with a reduction of overall QoL and reductions in various domains (i.e., physical, psychological, environmental, and social) in Brazilian men and women. Thus, the care and treatment of obese patients should be approached in a multidisciplinary way. In fact, obesity is a multifaceted condition impacting QoL in different ways, depending on the cultural context and, possibly, gender. The treatment of obesity is a difficult and complex process and, as recommended by the American National Institute of Health, a therapeutic approach emphasizing an increase in QoL on physical, psychological, environmental and social domains may facilitate loss of weight and a healthier lifestyle.
Author Contributions
HS and JL-F conceived the study design. FP collected the data and drafted the manuscript. DM performed the data analysis. Critical revisions were contributed by DM and EB. All authors discussed the results, implications, and literature, and approved the final version of the manuscript for submission.
Conflict of Interest Statement
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
Abilés, V., Rodríguez-Ruiz, S., Abilés, J., Mellado, C., García, A., Perez de la Cruz, A., et al. (2010). Psychological characteristics of morbidly obese candidates for bariatric surgery. Obes. Surg. 20, 161–167. doi: 10.1007/s11695-008-9726-1
Adams, K. F., Schatzkin, A., Harris, T. B., Kipnis, V., Mouw, T., Ballard-Barbash, R., et al. (2006). Overweight, obesity, and mortality in a large prospective cohort of persons 50 to 71 years old. N. Engl. J. Med. 355, 763–778. doi: 10.1056/NEJMoa055643
Ali, M. M., Amialchuk, A., and Rizzo, J. A. (2012). The influence of body weight on social network ties among adolescents. Econ. Hum. Biol. 10, 20–34. doi: 10.1016/j.ehb.2011.10.001
Backholer, K., Wong, E., Freak-Poli, R., Walls, H. L., and Peeters, A. (2012). Increasing body weight and risk of limitations in activities of daily living: a systematic review and meta-analysis. Obes. Rev. 13, 456–468. doi: 10.1111/j.1467-789X.2011.00970.x
Blakemore, A. I. F., and Buxton, J. L. (2014). Obesity, genetic risk, and environment. Br. Med. J. 348, g1900. doi: 10.1136/bmj.g1900
Bentley, T. G. K., Palta, M., Paulsen, A. J., Cherepanov, D., Dunham, N. C., Feeny, D., et al. (2011). Race and gender associations between obesity and nine health-related quality-of-life measures. Qual. Life Res. 20, 665–674. doi: 10.1007/s11136-011-9878-7
Boodai, S. A., and Reilly, J. J. (2013). Health related quality of life of obese adolescents in Kuwait. BMC Pediatr. 13, 105. doi: 10.1186/1471-2431-13-105
Buttitta, M., Iliescu, C., Rousseau, A., and Guerrien, A. (2014). Quality of life in overweight and obese children and adolescents: a literature review. Qual. Life Res. 23, 1117–1139. doi: 10.1007/s11136-013-0568-5
Choo, J., Jeon, S., and Lee, J. (2014). Gender differences in health-related quality of life associated with abdominal obesity in a Korean population. BMJ Open 4, e003954. doi: 10.1136/bmjopen-2013-003954
Cox, T. L., Ard, J. D., Beasley, T. M., Fernandez, J. R., Howard, V. J., Kolotkin, R. L., et al. (2011). Examining the Association Between Body Mass Index and Weight Related Quality of Life in Black and White Women. Appl. Res. Qual. Life. 7, 309–322. doi: 10.1007/s11482-011-9160-8
Cummins, S., Stafford, M., Macintyre, S., Marmot, M., and Ellaway, A. (2005). Neighbourhood environment and its association with self rated health: evidence from Scotland and England. J. Epidemiol. Community Health 59, 207–213. doi: 10.1136/jech.2003.016147
Dixon, J. B. (2010). The effect of obesity on health outcomes. Mol. Cell. Endocrinol. 316, 104–108. doi: 10.1016/j.mce.2009.07.008
Dobrow, I. J., Kamenetz, C., and Devlin, M. J. (2002). Psychiatric aspects of obesity. Rev. Bras. Psiquiatr. 24, 63–67. doi: 10.1590/S1516-44462002000700014
Dubois, L., Ohm Kyvik, K., Girard, M., Tatone-Tokuda, F., Pérusse, D., Hjelmborg, J., et al. (2012). Genetic and environmental contributions to weight, height, and BMI from birth to 19 years of age: an international study of over 12,000 twin pairs. PLoS ONE 7:e30153. doi: 10.1371/journal.pone.0030153
Fleck, M. P., Louzada, S., Xavier, M., Chachamovich, E., Vieira, G., Santos, L., et al. (2000). Application of the Portuguese version of the abbreviated instrument of quality life WHOQOL-bref. Rev. Saúde Pública 34, 178–183. doi: 10.1590/S0034-89102000000200012
Flegal, K. M., Kit, B. K., Orpana, H., and Graubard, B. I. (2013). Association of all-cause mortality with overweight and obesity using standard body mass index categories: a systematic review and meta-analysis. JAMA 309, 71–82. doi: 10.1001/jama.2012.113905
Forbes, G. B., Jung, J., Vaamonde, J. D., Omar, A., Paris, L., and Formiga, N. S. (2012). Body Dissatisfaction and Disordered Eating in Three Cultures: Argentina, Brazil, and the U.S. Sex Roles 66, 677–694. doi: 10.1007/s11199-011-0105-3
Friedman, K. E., Reichmann, S. K., Costanzo, P. R., Zelli, A., Ashmore, J. A., and Musante, G. J. (2005). Weight stigmatization and ideological beliefs: relation to psychological functioning in obese adults. Obes. Res. 13, 907–916. doi: 10.1038/oby.2005.105
Friedrich, M. J. (2002). Epidemic of obesity expands its spread to developing countries. JAMA 287, 1382–1386. doi: 10.1001/jama.287.11.1382-JMN0320-2-1
Garner, R. E., Feeny, D. H., Thompson, A., Bernier, J., McFarland, B. H., Huguet, N., et al. (2012). Bodyweight, gender, and quality of life: a population-based longitudinal study. Qual. Life Res. 21, 813–825. doi: 10.1007/s11136-011-9989-1
Guh, D. P., Zhang, W., Bansback, N., Amarsi, Z., Birmingham, C. L., and Anis, A. H. (2009). The incidence of co-morbidities related to obesity and overweight: a systematic review and meta-analysis. BMC Public Health 9:88. doi: 10.1186/1471-2458-9-88
Halpern, A., and Mancini, M. C. (2003). Treatment of obesity: an update on anti-obesity medications. Obes. Rev. 4, 25–42. doi: 10.1046/j.1467-789X.2003.00083.x
Hashimoto, D. M., Schmid, J., Martins, F. M., Fonseca, A. M., Andrade, L. H., Kirchengast, S., et al. (2003). The impact of the weight status on subjective symptomatology of the Polycystic Ovary Syndrome: a cross-cultural comparison between Brazilian and Austrian women. Anthropol. Anz. 61, 297–310.
Hassan, M. K., Joshi, A. V., Madhavan, S. S., and Amonkar, M. M. (2003). Obesity and health-related quality of life: a cross-sectional analysis of the US population. Int. J. Obes. 27, 1227–1232. doi: 10.1038/sj.ijo.0802396
Hesse-Biber, S., Leavy, P., Quinn, C. E., and Zoino, J. (2006). The mass marketing of disordered eating and Eating Disorders: The social psychology of women, thinness and culture. Womens. Stud. Int. Forum. 29, 208–224. doi: 10.1016/j.wsif.2006.03.007
Hlatky, M. A., Chung, S. C., Escobedo, J., Hillegass, W. B., Melsop, K., Rogers, W., et al. (2010). The effect of obesity on quality of life in patients with diabetes and coronary artery disease. Am. Heart J. 159, 292–300. doi: 10.1016/j.ahj.2009.11.004
Horta, P. M., Cardoso, A. H., Lopes, A. C. S., and dos Santos, L. C. (2013). Qualidade de vida entre mulheres com excesso de peso e doenças crônicas não transmissíveis. Rev. Gaúcha Enferm. 34, 121–129. doi: 10.1590/S1983-14472013000400016
Jalali-Farahani, S., Chin, Y. S., Amiri, P., and Mohd Taib, M. N. (2013). Body mass index (BMI)-for-age and health-related quality of life (HRQOL) among high school students in Tehran. Child: Care. Health Dev. 40, 731–739. doi: 10.1111/cch.12103
Jia, H., and Lubetkin, E. I. (2005). The impact of obesity on health-related quality-of-life in the general adult US population. J. Public Health 27, 156–164. doi: 10.1093/pubmed/fdi025
Kakeshita, I. S., and Almeida, S. S. (2008). The relationship between body mass index and body image in Brazilian adults. Psychol. Neurosci. 1, 103–107. doi: 10.3922/j.psns.2008.2.003
Klatchoian, D. A., Len, C. A., Terreri, M. T. R. A., Silva, M., Itamoto, C., Ciconelli, R. M., et al. (2008). Quality of life of children and adolescents from São Paulo: reliability and validity of the Brazilian version of the Pediatric Quality of Life Inventory™ version 4.0 Generic Core Scales. J. Pediatr. 84, 308–315. doi: 10.1590/S0021-75572008000400005
Kolotkin, R. L., Meter, K., and Williams, G. R. (2001). Quality of life and obesity. Obes. Rev. 2, 219–229. doi: 10.1046/j.1467-789X.2001.00040.x
Korhonen, P. E., Seppälä, T., Järvenpää, S., and Kautiainen, H. (2014). Body mass index and health-related quality of life in apparently healthy individuals. Qual. Life Res. 23, 67–74. doi: 10.1007/s11136-013-0433-6
Kushner, R. F., and Foster, G. D. (2000). Obesity and quality of life. Nutrition 16, 947–952. doi: 10.1016/S0899-9007(00)00404-4
Lam, J. C. M., Mak, J. C. W., and Ip, M. S. M. (2012). Obesity, obstructive sleep apnoea and metabolic syndrome. Respirology 17, 223–236. doi: 10.1111/j.1440-1843.2011.02081.x
Lee, D. W., Kim, S., and Cho, D. Y. (2012). Obesity-Related Quality of Life and Distorted Self-Body Image in Adults. Appl. Res. Qual. Life. 8, 87–100. doi: 10.1007/s11482-012-9174-x
Luppino, F. S., de Wit, L. M., Bouvy, P. F., Stijnen, T., Cuijpers, P., Penninx, B. W., et al. (2010). Overweight, obesity, and depression: a systematic review and meta-analysis of longitudinal studies. Arch. Gen. Psychiatry 67, 220–229. doi: 10.1001/archgenpsychiatry.2010.2
McLaughlin, L., and Hinyard, L. J. (2014). The relationship between health-related quality of life and body mass index. West. J. Nurs. Res. 36, 989–1001. doi: 10.1177/0193945913520415
Morris, S. (2007). The impact of obesity on employment. Labour Econ. 14, 413–433. doi: 10.1016/j.labeco.2006.02.008
Must, A., Spadano, J., Coakley, E. H., Field, A. E., Colditz, G., and Dietz, W. H. (1999). The disease burden associated with overweight and obesity. J. Am. Med. Assoc. 282, 1523–1529. doi: 10.1001/jama.282.16.1523
Ng, M., Fleming, T., Robinson, M., Thomson, B., Graetz, N., Margono, C., et al. (2014). Global, regional, and national prevalence of overweight and obesity in children and adults during 1980–2013: a systematic analysis for the Global Burden of Disease Study 2013. Lancet 384, 766–781. doi: 10.1016/S0140-6736(14)60460-8
Ojeda, E., Lopez, S., Rodriguez, P., Moran, L., Rodriguez, J. M., and Delucas, P. (2014). Prevalence of sleep apnea syndrome in morbidly obese patients. Chest 145(3 Suppl.), 601A. doi: 10.1378/chest.1781090
Oliveira, L. L., and Hutz, C. S. (2010). Transtornos Alimentares: O Papel Dos Aspectos Culturais No Mundo Contemporâneo. Psicol. Em Estud. 15, 575–82. doi: 10.1590/S1413-73722010000300015
Perez, M., and Warren, C. S. (2011). The relationship between quality of life, binge-eating disorder, and obesity status in an ethnically diverse sample. Obesity (Silver Spring, Md.) 20, 879–885. doi: 10.1038/oby.2011.89
Poortinga, W. (2006). Perceptions of the environment, physical activity, and obesity. Soc. Sci. Med. 63, 2835–2846. doi: 10.1016/j.socscimed.2006.07.018
Popkin, B. M., Adair, L. S., and Ng, S. W. (2012). Global nutrition transition and the pandemic of obesity in developing countries. Nutr. Rev. 70, 3–21. doi: 10.1111/j.1753-4887.2011.00456.x
Puhl, R. M., and Heuer, C. A. (2009). The stigma of obesity: a review and update. Obesity 17, 941–964. doi: 10.1038/oby.2008.636
Puhl, R. M., and King, K. M. (2013). Weight discrimination and bullying. Best Pract. Res. Clin. Endocrinol. Metab. 27, 117–127. doi: 10.1016/j.beem.2012.12.002
Ryan, S., Crinion, S. J., and McNicholas, W. T. (2014). Obesity and sleep-disordered breathing: when two “bad guys” meet. Q. J. Med. 107, 949–954. doi: 10.1093/qjmed/hcu029
Silventoinen, K., Rokholm, B., Kaprio, J., and Sørensen, T. I. A. (2010). The genetic and environmental influences on childhood obesity: a systematic review of twin and adoption studies. Int. J. Obes. 34, 29–40. doi: 10.1038/ijo.2009.177
Son, Y. J., and Kim, G. (2012). The relationship between obesity, self-esteem and depressive symptoms of adult women in Korea. Korean J. Obes. 21, 89. doi: 10.7570/kjo.2012.21.2.89
Stommel, M., and Schoenborn, C. A. (2009). Accuracy and usefulness of BMI measures based on self-reported weight and height: findings from the NHANES & NHIS 2001–2006. BMC Public Health 9:421. doi: 10.1186/1471-2458-9-421
Stone, A. A., and Broderick, J. E. (2012). Obesity and pain are associated in the United States. Obesity 20, 1491–1495. doi: 10.1038/oby.2011.397
Taylor, V. H., Forhan, M., Vigod, S. N., McIntyre, R. S., and Morrison, K. M. (2013). The impact of obesity on quality of life. Best Pract. Res. Clin. Endocrinol. Metab. 27, 139–146. doi: 10.1016/j.beem.2013.04.004
Thomas, S., Karunaratne, A., Lewis, S., Castle, D., Knoesen, N., Honigman, R., et al. (2010). “Just bloody fat!”: a qualitative study of body image, self-esteem and coping in obese adults. Int. J. Mental Health Promot. 12, 39–49. doi: 10.1080/14623730.2010.9721805
Turco, G., Bobbio, T., Reimão, R., Rossini, S., Pereira, H., and Barros Filho, A. (2013). Qualidade de vida e do sono de adolescentes obesos. Arq. Neuropsiquiatr. 71, 78–82. doi: 10.1590/S0004-282X2013005000008
Ul-Haq, Z., Mackay, D. F., Fenwick, E., and Pell, J. P. (2013). Meta-analysis of the association between body mass index and health-related quality of life among adults, assessed by the SF-36. Obesity 21, E322–E327. doi: 10.1002/oby.20107
Varni, J. W., Seid, M., and Rode, C. A. (1999). The PedsQL: measurement model for the pediatric quality of life inventory. Med. Care. 37, 126–139.
Vucenik, I., and Stains, J. P. (2012). Obesity and cancer risk: evidence, mechanisms, and recommendations. Ann. N. Y. Acad. Sci. 1271, 37–43. doi: 10.1111/j.1749-6632.2012.06750.x
Wee, C. C., Davis, R. B., Huskey, K. W., Jones, D. B., and Hamel, M. B. (2013). Quality of life among obese patients seeking weight loss surgery: the importance of obesity-related social stigma and functional status. J. Gen. Intern. Med. 28, 231–238. doi: 10.1007/s11606-012-2188-0
World Health Organization. (1996). What quality of life? The WHOQOL Group. World Health Organization Quality of Life Assessment. World Health Forum 17, 354–356.
World Health Organization. (2009). Women and Health: Today’s Evidence, Tomorrow’s Agenda. Geneva: World Health Organization.
Keywords: obesity, adults, quality of life, BMI, World Health Organization Quality of Life
Citation: Pimenta FBC, Bertrand E, Mograbi DC, Shinohara H and Landeira-Fernandez J (2015) The relationship between obesity and quality of life in Brazilian adults. Front. Psychol. 6:966. doi: 10.3389/fpsyg.2015.00966
Received: 11 November 2014; Accepted: 28 June 2015;
Published: 14 July 2015.
Edited by:
Alix Timko, Children’s Hospital of Philadelphia, USACopyright © 2015 Pimenta, Bertrand, Mograbi, Shinohara and Landeira-Fernandez. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) or licensor are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Elodie Bertrand, Departamento de Psicologia, Pontifícia Universidade Católica do Rio de Janeiro, Rua Marquês de São Vicente, 225, Gávea, Edifício Cardeal Leme, sala 201, Rio de Janeiro, RJ 22453-900, Brasil, elodie.bertrand1@gmail.com
 Fernanda B. C. Pimenta
Fernanda B. C. Pimenta