Impact of incentives on COVID-19 vaccination; A systematic review
- 1Non-communicable Diseases Research Center, Alborz University of Medical Sciences, Karaj, Iran
- 2Student Research Committee, Alborz University of Medical Sciences, Karaj, Iran
- 3Development of Research and Technology Center, Deputy of Research and Technology, Ministry of Health and Medical Education, Tehran, Iran
- 4Pediatric Nephrology Research Center, Research Institute for Children's Health, Shahid Beheshti University of Medical Sciences, Tehran, Iran
Introduction: Although vaccination is the most effective way to limit and overcome the COVID-19 pandemic, a considerable fraction of them are not intended to get vaccinated. This study aims to investigate the existing research evidence and evaluate the effectiveness and consequences of all incentives provided for increasing the uptake of COVID-19 vaccination.
Methods: A systematic search in PubMed, Web of Science (WoS), and SCOPUS from 2020 until October 10, 2021, was conducted on experimental studies evaluating the effects of incentives including cash, lottery voucher, and persuasive messages on COVID-19 vaccination intention and uptake. The study selection process, data extraction, and quality assessment were conducted independently by two investigators using Consolidated Standards of Reporting Trials (CONSORT 2010) checklist.
Results: Twenty-four records were included in the qualitative analysis. Most of the included studies assessed the effect of financial incentives. In 14 studies (58%) the assessed outcome was vaccination uptake and in nine (37.5%) others it was vaccination intention. One study considered self-reported vaccination status as the outcome. This study shows that high financial incentives and the Vax-a-million lottery are attributed to a higher vaccination rate, while the low amount of financial incentives, other lotteries, and persuasive messages have small or non-significant effects.
Conclusion: Paying a considerable amount of cash and Vax-a-million lottery are attributed to a higher vaccination. Nevertheless, there is a controversy over the effect of other incentives including other lotteries, low amount of cash, and messages on vaccination. It is noteworthy that, inconsistency and imprecision of included studies should be considered.
Introduction
Coronavirus Disease 2019 (COVID-19) is expanded worldwide, causing a global concern in all group ages (1–3). Vaccination is the most effective controllable measurement to limit and overcome the COVID-19 pandemic. It is estimated that in the best-case scenario using a vaccine with 90% efficacy against, herd immunity will be achieved by vaccinating at least 66% of the population (4), although some studies are more pessimistic predicting that herd immunity may not be achievable (5). The vaccination speed is currently limited in many countries due to insufficient production capacities and affordability (6). However, even in countries with adequate supplies and evidence for sufficient efficacy, vaccine hesitancy remains a non-negligible barrier in mitigating the COVID-19 pandemic (7).
Vaccine hesitancy is defined as the delay in acceptance or refusal of vaccination despite available vaccination services (8) and was introduced in 2019 by the World Health Organization (WHO) as one of the top ten threats to global health (9). The COVID-19 era may be associated with even more catastrophic consequences due to the rapid progression of the COVID-19 pandemic and the ongoing development of vaccine-resistant variants of SARS-CoV-2 (10, 11). The main reasons for vaccine hesitancy include concerns about vaccine side effects, distrust in their efficacy, misleading information about the vaccine's necessity and benefit, and conspiracy beliefs (7, 12). Also, vaccine hesitancy is linked to a lack of trust in COVID-19 vaccine safety and science (13).
Notably, the majority of vaccine-hesitant people are also highly resistant to required proof of vaccination. A previous study showed that a small of vaccine-hesitant people approve of requiring vaccination proof for access to international travel, indoor activities, employment, and public schools. To put it simply, not only are vaccine-hesitant individuals, not willing to get vaccinated themselves, but also they resist the rules that force others to get vaccinated. This leads to a block in improving COVID-19 vaccination coverage going forward and generates substantial challenges for ongoing vaccination campaigns to succeed (13, 14).
Both positive reinforcements [e.g., providing certain liberties to vaccinated people, monetary incentives (cash, lotteries, gift cards, free foods), facilitated access] (15) and negative reinforcements (restricted access to entertainment venues, not allowed to work) (12, 16) are applied to combat vaccine hesitancy and increase vaccination adherence. However, incentives (particularly financial ones) may, on the other hand, lead to a false interpretation of uptake-increasing strategies, further increasing society's resistance to vaccinations (17).
Besides incentives, other practical approaches for increasing vaccination willingness are proposed by different studies, including governmental transparency in providing information about vaccine details and decision making, altruistic messages (reflecting the responsibility of an individual to contribute to herd immunity), and highlighting the burden of losses associated with vaccine avoidance (18, 19). However, the degree to which these approaches can affect the rate of vaccination is not precise. The purpose of the present systematic review is to investigate the existing research evidence and evaluate the effectiveness and consequences of all types of incentives provided for increasing uptake/intention of COVID-19 vaccination.
Methods
Protocol
This study is a comprehensive systematic review of all available evidence on the association between incentives and COVID-19 vaccination. We followed a systematic review protocol that adheres to the PRISMA-P guidelines (20). All of the processes run based on details of the study protocol.
Search strategy
The main root of search strategies developed is based on two main components of “incentives of vaccinations” and “COVID-19.” We searched the electronic data sources including PubMed, Web of Science (WoS), and SCOPUS based on the search strategy described in Supplementary Table 1. We also searched bioRxiv and medRxiv to include related preprint articles.
Eligibility criteria
All relevant experimental studies [cross-sectional (CS), randomized trial (RT), factorial trial (FT), and quasi-experimental (QE)] have been included. All of the related review articles were evaluated for their references. There was no limitation in terms of the age and gender of the target groups and the time and language of the papers. All studies with duplicate citations were excluded. Moreover, other resources, related gray literature, publications' reference lists, and related key journals were searched for additional publications.
Screening
The searched papers were exported to Endnote software. Initially, the relevancy of papers was evaluated based on their titles and abstracts, followed by a full-text assessment.
Quality assessment
For remaining eligible studies, QA was conducted based on comprehensive recommended guidelines of the Consolidated Standards of Reporting Trials (CONSORT 2010) 25 item-checklist (21) by two independent research experts (SD and PM). Any disagreements resolve by another investigator (MQ).
Data extraction
The data were extracted using a checklist recording bibliographic characteristics (citation, publication year, study year, provenance of study), general and methodologic characteristics (type of study, sample size, type of intervention, and type of outcome), and the main findings of each study. All search and data extraction process was done by two independent research experts (ZEA and RK).
Ethical considerations
The present study was approved by the Ethical Committee of the Alborz University of Medical Sciences. All of the included studies are cited. Whenever we needed more information about a particular study, we contacted the corresponding author.
Results
Study selection process
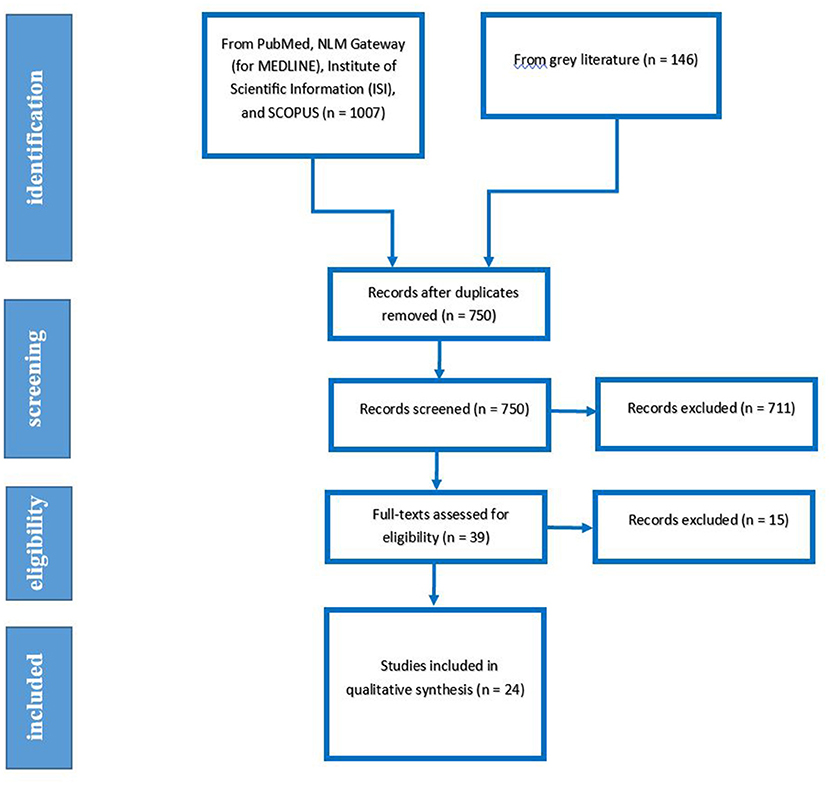
Our searches yielded 1,153 studies from previously mentioned databases and sources. After the rejection of duplicates, we screened 759 studies. We Excluded 601 and 110 papers after the title and abstract screening, respectively. After the full-text assessment, 24 studies were included in the qualitative synthesis. The detailed flow diagram is shown in Figure 1 (22–45).
Studies and participants' characteristics
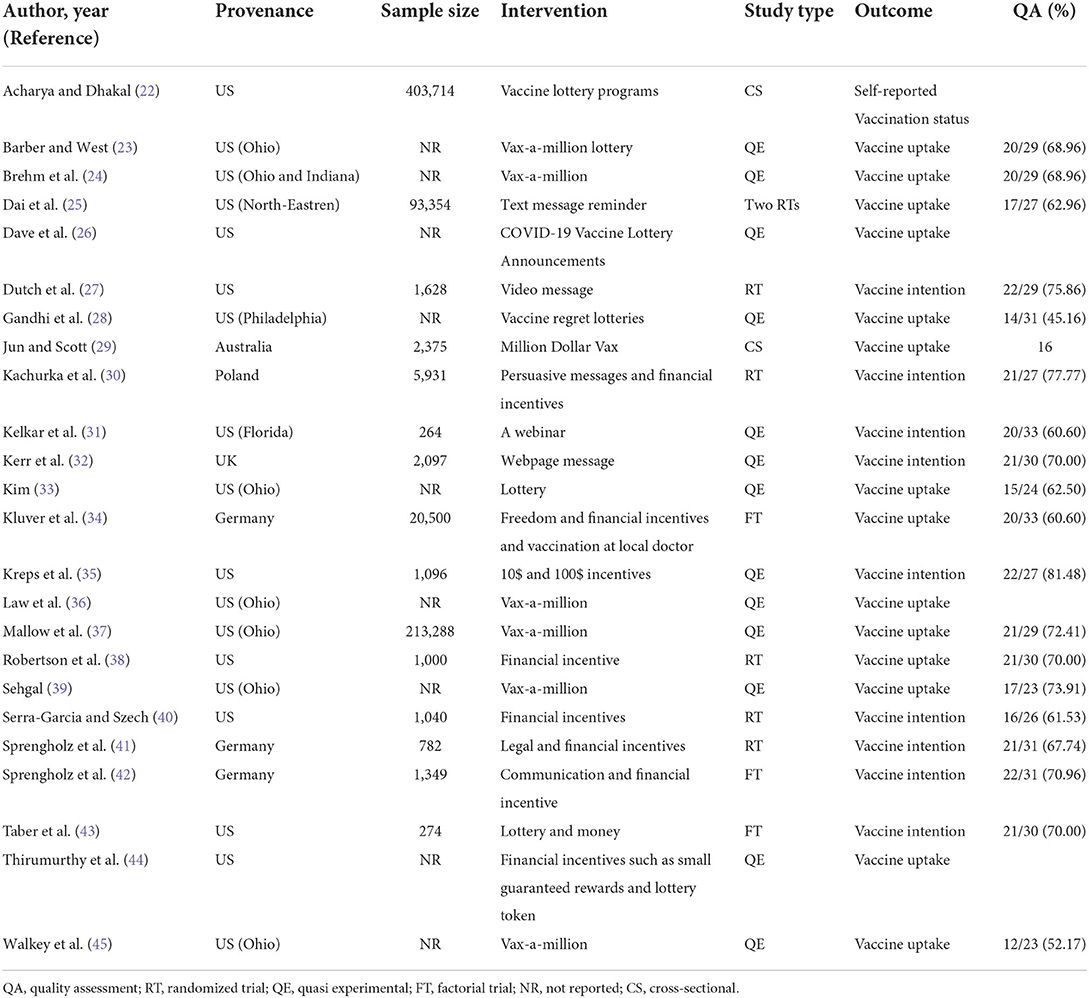
Among 24 included studies the design of 13 studies were QE, two studies were CS, six studies were RT and three studies were FT. Nine studies assessed the effect of financial incentives. In 14 studies (58%) the assessed outcome was vaccination uptake and in nine (37.5%) others it was vaccination intention. One study considered self-reported vaccination status as the outcome. Nineteen studies originated from the United States, followed by three papers that originated from Germany. The bibliographic and general characteristics of included studies are summarized in Table 1. Supplementary Table 2 provides details of the QA of included studies.
Qualitative synthesis
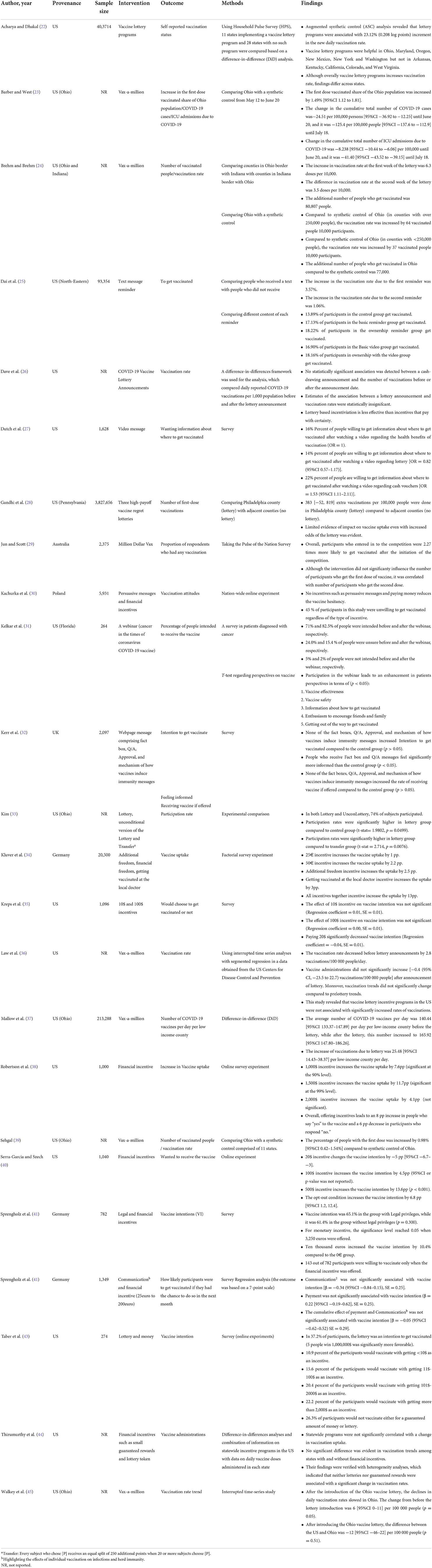
Table 2 not merely summarizes the effects of different incentives on indices related to vaccine uptake and intention but also shows how the surge in vaccine uptake as a result of incentives can prevent COVID-19 infection and its outcomes.
Thirteen of included studies revealed the effects of the lottery on vaccination uptake or intention. Vax-a-million lottery in Ohio, United States, was attributed to a significant increase ranging from 0.98% (39) to 1.49% (23) in the percentage of the first dose vaccinated people compared to synthetic control. This intervention not only slowed the decline in vaccination rate (37) but also led to the vaccination of additional 77,000 Ohioans compared to synthetic control (24). Nevertheless, some other studies revealed insignificant or negligible findings regarding the lotteries in the US (36). Included studies also revealed contradictory findings for other lotteries. While most studies showed limited or no evidence of impact (22, 26, 28, 29, 44), others demonstrated that lottery should be considered as a motivation for vaccination in a significant fraction of participants (33, 43).
Similarly, most studies revealed non-significant effects of persuasive messages and communication in incrementing the general population's intention to get vaccinated (21, 23, 31). Nevertheless, this intervention significantly enhances the intentions and perspectives of patients diagnosed with cancer (31). It should be noted that text messages and first reminders lead to a higher vaccination intention than video messages and second reminders, respectively (25).
When paid in high amounts, financial incentives significantly increase the participants' intention to vaccination (40, 42, 43). Conversely, studies included in this review showed that not merely the effects of the low amount of financial incentives are non-significant (30), but also that these incentives can lead to a decreased vaccination intention (40).
Discussion
The present study was performed to systematically review the effect of some interventions, such as lotteries, persuasive messages, and financial incentives, and a series of other variables such as legal incentives on getting vaccinated or people's intention to get vaccinated. The lottery has driven minor changes in vaccination share among people. Messages' effects are generally non-significant; however, they may be beneficial in a particular group of people. Conversely, most studies have shown that financial incentives can effectively increase the vaccination rate.
Various incentives and behavioral nudges have been applied to abrogate vaccine hesitancy and increase vaccination coverage. On May 13, 2021, Ohio announced the Vax-a-Million, a free weekly lottery, which ran from May 26 to June 23 for Ohioans who had received at least one COVID-19 vaccine. By June 20, the end of the lottery registration period, nearly 3.5 million adults and 155,000 children had registered for the free lottery (39). Several studies have examined the effect of this incentive program. Overall, the results showed that the first dose vaccinated share of the population, vaccination rate, and the number of vaccinated people increased. Furthermore, the cumulative total number of COVID-19 cases and the total number of ICU admissions due to COVID-19 decreased after the beginning of the lottery. As mentioned earlier, these changes have been enough to be considered meaningful, although evidence on lotteries other than Vax-a-Million is limited (28).
By considering the additional number of people who have been encouraged to get vaccinated because of the Ohio Vax-a-million, Barber and West (23) showed that the cost of the Vax-a-million scheme was less than one-tenth of the potential costs incurred in the absence of the lottery, which indicates the value of such schemes. Furthermore, recent evidence suggests that a lottery is more cost-effective than a lump-sum transfer payment (33). The budget allocated to Ohio's Vax-a-million was $75 for each additional injected dose, much more cost-effective than paying to everyone.
In contrast to lotteries, text message reminders for vaccination do not seem to considerably affect vaccine hesitancy. Although a slight increment in the vaccination rate was observed after the first message reminder, the second text message reminder had a meaningless influence. It is worth noting that video messages had a more negligible effect on the vaccination rate than text messages (25). On the other hand, messages regarding cash vouchers raised people's willingness to get information about vaccination; however, it is unclear how much this intervention will actually lead to getting vaccinated (27).
Unlike the general population, webinars on cancer and COVID-19 vaccination represented promising results. The percentage of patients with cancer who intended to receive the vaccine increased, and patients' perspectives in terms of vaccine effectiveness, vaccine safety, information about how to get vaccinated, enthusiasm to encourage friends and family, and getting out of the way to get vaccinated were notably improved (31). Therefore, measurements to increase awareness among target populations with special conditions can be taken to address their doubts about vaccination.
Among the interventions we reviewed, financial incentives (paying cash) generally had higher levels of significance. However, determining the amount of money paid should be considered thoroughly because it has been shown that small amounts of money as an incentive can be ineffective or even have reverse effects (35, 40). In other words, some studies demonstrated that offering little payment often signals to individuals that a particular behavior is unpredictable, hazardous, or risky, which may in turn lead to lower vaccination uptake (46). But paying higher amounts, such as 1,000 or $1,500, has significant effects on people's willingness to get vaccinated (38, 40). It can be conjectured that economically vulnerable populations are more likely to get vaccinated by financial incentives. Nonetheless, other factors such as young age, psychological antecedent (less confidence about vaccine safety, more complacency about no necessity of vaccination) (42), and belonging to specific political groups (democrats and independents vs. republicans) (38) seem to contribute to the higher responsiveness to monetary incentives. It is important to note that the correlation between the size of incentive and vaccine uptake is not linear, as one study showed that huge financial incentives ($2,000) appear to be less effective than moderately sized incentives ($1,500) and even maybe counter-productive is some ethnic groups (Black and Latino Americans) (38). This finding may somehow decrease concerns regarding the possibility of disturbing autonomous vaccination decisions in those of limited means.
There is controversy over whether it is ethical to encourage people to get vaccinated through financial incentives. Some experts believe that paying cash and giving lottery vouchers undermines the moral spirit of performing tasks such as maintaining and promoting the personal community's public health and contributing to the mitigation of pandemics. In addition, they state that many people are willing to get vaccinated even without the need to receive money, which leads to the unnecessary waste of substantial financial resources (46).
Conversely, other studies point to the history of such schemes, arguing that these incentives can reduce the burden of COVID-19 in general. Also, upgrading and increasing vaccination can provide better safety for disadvantaged individuals (47, 48). In addition, these incentives create a double motivation. They can at least make people get vaccinated in a reduced timetable, which eventually leads to decreased number of infected patients and declined mortality rate (17, 39). To sum up, similar to Brewer et al. research, our findings suggest that vaccine incentives are more effective when they are delivered immediately, recipients value them, and more importantly, their receipt is certain (49).
Limitations
This study had several limitations; First, the inclusion criteria and experimental setting of the studies we have mentioned for incentives may not cover a wide range of people, and this limitation may change the results of this study in reality. Second, Most studies reviewed in this paper originated from the United States and Europe. Prior to extending the results of this study to other countries, considerations should be taken into account according to the demographic, cultural, and structural features. Third, most of the included experimental studies suffered from a lack of a well-defined control group which may have affected the results. Fourth, the findings of this study could be affected by, inconsistency and imprecision of included studies.
Implications
It is estimated that the threshold of 60–70% of the population gaining immunity is essential to achieve COVID-19 herd immunity (4). As a result of high vaccine hesitancy, this threshold is probably impossible to achieve without vaccine incentives. This study assists policymakers around the globe to opt for the most effective incentive to boost COVID-19 vaccination in their countries. Governments should keep in mind that although vaccination incentives were introduced as practical tools in accelerating the vaccination, more experimental studies in variable geographical regions and different ethnic groups concerning each country's specifications are still needed.
Conclusion
This review showed that participants were more likely to get vaccinated when incentivized by a high amount of cash. Moreover, while Vax-a-million significantly increases the uptake of the COVID-19 vaccine, the effects of other lotteries and persuasive messages were non-significant or marginally significant.
Data availability statement
The raw data supporting the conclusions of this article will be made available by the authors, without undue reservation.
Author contributions
RK and ZE: data extraction. PM, SD, and MQ: systematic search and quality assessment. PM: drafting. MQ and MJ: revision. MQ: supervision. All authors read and approved final version of manuscript.
Conflict of interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
Publisher's note
All claims expressed in this article are solely those of the authors and do not necessarily represent those of their affiliated organizations, or those of the publisher, the editors and the reviewers. Any product that may be evaluated in this article, or claim that may be made by its manufacturer, is not guaranteed or endorsed by the publisher.
Supplementary material
The Supplementary Material for this article can be found online at: https://www.frontiersin.org/articles/10.3389/fmed.2022.810323/full#supplementary-material
References
1. Hasani H, Mardi S, Shakerian S, Taherzadeh-Ghahfarokhi N, Mardi P. The novel coronavirus disease (COVID-19): a PRISMA systematic review and meta-analysis of clinical and paraclinical characteristics. Biomed Res Int. (2020) 2020:3149020. doi: 10.1101/2020.04.19.20071456
2. Mardi P, Esmaeili M, Iravani P, Abdar ME, Pourrostami K, Qorbani M. Characteristics of children with kawasaki disease-like signs in COVID-19 pandemic: a systematic review. Front Pediatr. (2021) 9:625377. doi: 10.3389/fped.2021.625377
3. Mardi P, Shojaeian S, Taherzadeh-Ghahfarokhi N, Molaverdi G, Amiri Roudy M, Salahshour A, et al. SARS-CoV-2 and COVID-19, evidence from a literature review: review article. Tehran Univ Med J. (2021) 78:712–25. Available online at: http://tumj.tums.ac.ir/article-1-11034-en.html
4. MacIntyre CR, Costantino V, Trent M. Modelling of COVID-19 vaccination strategies and herd immunity, in scenarios of limited and full vaccine supply in NSW, Australia. Vaccine. (2022) 40:2506–13. doi: 10.1016/j.vaccine.2021.04.042
5. Kadkhoda K. Herd immunity to COVID-19: alluring and elusive. Am J Clin Pathol. (2021) 155:471–2. doi: 10.1093/ajcp/aqaa272
6. Wouters OJ, Shadlen KC, Salcher-Konrad M, Pollard AJ, Larson HJ, Teerawattananon Y, et al. Challenges in ensuring global access to COVID-19 vaccines: production, affordability, allocation, and deployment. Lancet. (2021) 397:1023–34. doi: 10.1016/S0140-6736(21)00306-8
7. Štěpánek L, Janošíková M, Nakládalová M, Štěpánek L, Boriková A, Vildová H. Motivation to COVID-19 vaccination and reasons for hesitancy in employees of a czech tertiary care hospital: a cross-sectional survey. Vaccines. (2021) 9:863. doi: 10.3390/vaccines9080863
8. MacDonald NE. Vaccine hesitancy: definition, scope and determinants. Vaccine. (2015) 33:4161–4. doi: 10.1016/j.vaccine.2015.04.036
9. WHO. Ten Threats to Global Health in 2019. (2019). Available online at: www.who.int/news-room/spotlight/ten-threats-to-global-health-in-2019 (accessed August 2, 2021).
10. Kabir K, Taherinia A, Ashourloo D, Khosravi A, Karim H, Salehi Shahrabi H, et al. Epidemic size, trend and spatiotemporal mapping of SARS-CoV-2 using geographical information system in Alborz Province, Iran. BMC Infect Dis. (2021) 21:1185. doi: 10.1186/s12879-021-06870-6
11. Tian D, Sun Y, Xu H, Ye Q. The emergence and epidemic characteristics of the highly mutated SARS-CoV-2 Omicron variant. J Med Virol. (2022) 94:2376–83. doi: 10.1002/jmv.27643
12. Burke PF, Masters D, Massey G. Enablers and barriers to COVID-19 vaccine uptake: an international study of perceptions and intentions. Vaccine. (2021) 39:5116–28. doi: 10.1016/j.vaccine.2021.07.056
13. Lazarus JV, Wyka K, White TM, Picchio CA, Rabin K, Ratzan SC, et al. Revisiting COVID-19 vaccine hesitancy around the world using data from 23 countries in 2021. Nat Commun. (2022) 13:3801. doi: 10.1038/s41467-022-31441-x
14. Finney Rutten LJ, Zhu X, Leppin AL, Ridgeway JL, Swift MD, Griffin JM, et al. Evidence-based strategies for clinical organizations to address COVID-19 vaccine hesitancy. Mayo Clin Proc. (2021) 96:699–707. doi: 10.1016/j.mayocp.2020.12.024
15. Arezki R. Cash payments in Africa could boost vaccine uptake. Nature. (2021) 596:9. doi: 10.1038/d41586-021-02086-5
16. Saban M, Myers V, Ben Shetrit S, Wilf-Miron R. Issues surrounding incentives and penalties for COVID-19 vaccination: the Israeli experience. Prev Med. (2021) 153:106763. doi: 10.1016/j.ypmed.2021.106763
17. Volpp KG, Cannuscio CC. Incentives for immunity — strategies for increasing COVID-19 vaccine uptake. N Engl J Med. (2021) 385:e1. doi: 10.1056/NEJMp2107719
18. Giuliani M, Ichino A, Bonomi A, Martoni R, Cammino S, Gorini A. Who is willing to get vaccinated? a study into the psychological, socio-demographic, and cultural determinants of COVID-19 vaccination intentions. Vaccines. (2021) 9:810. doi: 10.3390/vaccines9080810
19. Gong Z, Tang Z, Li J. What strategy is better for promoting COVID-19 vaccination? a comparison between gain-framed, loss-framed, altruistic messages. Ann Behav Med. (2021) 56:25–331. doi: 10.1093/abm/kaab070
20. Liberati A, Altman DG, Tetzlaff J, Mulrow C, Gøtzsche PC, Ioannidis JP, et al. The PRISMA statement for reporting systematic reviews and meta-analyses of studies that evaluate health care interventions: explanation and elaboration. J Clin Epidemiol. (2009) 62:e1–34. doi: 10.1016/j.jclinepi.2009.06.006
21. Schulz KF, Altman DG, Moher D. CONSORT 2010 statement: updated guidelines for reporting parallel group randomised trials. Int J Surg. (2011) 9:672–7. doi: 10.1016/j.ijsu.2011.09.004
22. Acharya B, Dhakal C. Implementation of state vaccine incentive lottery programs and uptake of COVID-19 vaccinations in the United States. JAMA Net Open. (2021) 4:e2138238. doi: 10.1001/jamanetworkopen.2021.38238
23. Barber A, West J. Conditional cash lotteries increase COVID-19 vaccination rates. J Health Econ. (2022) 81:102578. doi: 10.1016/j.jhealeco.2021.102578
24. Brehm ME, Brehm PA, Saavedra M. The Ohio vaccine lottery and starting vaccination rates. Am J Health Econ. (2022) 8:387–411. doi: 10.1086/718512
25. Dai H, Saccardo S, Han MA, Roh L, Raja N, Vangala S, et al. Behavioural nudges increase COVID-19 vaccinations. Nature. (2021) 597:404–9. doi: 10.1038/s41586-021-03843-2
26. Dave D, Friedson AI, Hansen B, Sabia JJ. Association between statewide COVID-19 lottery announcements and vaccinations. JAMA Health Forum. (2021). doi: 10.1001/jamahealthforum.2021.3117
27. Duch RM, Barnett A, Filipek M, Roope L, Violato M, Clarke P. Cash versus lotteries: COVID-19 vaccine incentives experiment. medRxiv [Preprint]. (2021). p. 1–29. doi: 10.1101/2021.07.26.21250865
28. Gandhi L, Milkman K, Ellis S, Graci H, Gromet D, Mobarak R, et al. An experiment evaluating the impact of large-scale, high-payoff vaccine regret lotteries. SSRN Electron J. (2021). doi: 10.2139/ssrn.3904365
29. Jun D, Scott A. An observational study of the association between COVID-19 vaccination rates and entry into the Australian ‘million dollar vax' competition. medRxiv [Preprint]. (2022). p. 1–27. doi: 10.1101/2022.03.02.22271734
30. Kachurka R, Krawczyk M, Rachubik J. Persuasive messages will not increase COVID-19 vaccine acceptance: evidence from a nationwide online experiment. Vaccines. (2021) 9:1113. doi: 10.3390/vaccines9101113
31. Kelkar AH, Blake JA, Cherabuddi K, Cornett H, McKee BL, Cogle CR. Vaccine enthusiasm and hesitancy in cancer patients and the impact of a webinar. Healthcare. (2021) 9:351. doi: 10.3390/healthcare9030351
32. Kerr JR, Freeman ALJ, Marteau TM, van der Linden S. Effect of information about COVID-19 vaccine effectiveness and side effects on behavioural intentions: two online experiments. Vaccines. (2021) 9:379. doi: 10.3390/vaccines9040379
34. Klüver H, Hartmann F, Humphreys M, Geissler F, Giesecke J. Incentives can spur COVID-19 vaccination uptake. Proc Nat Acad Sci. (2021) 118:e2109543118. doi: 10.1073/pnas.2109543118
35. Kreps S, Dasgupta N, Brownstein JS, Hswen Y, Kriner DL. Public attitudes toward COVID-19 vaccination: the role of vaccine attributes, incentives, and misinformation. npj Vaccines. (2021) 6:73. doi: 10.1038/s41541-021-00335-2
36. Law AC, Peterson D, Walkey AJ, Bosch NA. Lottery-based incentives and COVID-19 vaccination rates in the US. JAMA Intern Med. (2022) 182:235–7. doi: 10.1001/jamainternmed.2021.7052
37. Mallow PJ, Enis A, Wackler M, Hooker EA. COVID-19 financial lottery effect on vaccine hesitant areas: results from Ohio's vax-a-million program. Am J Emerg Med. (2022) 56:316–7. doi: 10.1016/j.ajem.2021.08.053
38. Robertson C, Scheitrum D, Schaefer A, Malone T, McFadden BR, Messer KD, et al. Paying Americans to take the vaccine—would it help or backfire? J Law Biosci. (2021) 8:lsab027. doi: 10.1093/jlb/lsab027
39. Sehgal NKR. Impact of vax-a-million lottery on COVID-19 vaccination rates in ohio. Am J Med. (2021) 134:1424–6. doi: 10.1016/j.amjmed.2021.06.032
40. Serra-Garci M. nd test demand. SSRN Electron J. CESifo Working Paper No. 9003. (2021). Available online at: https://ssrn.com/abstract=3827616
41. Sprengholz P, Eitze S, Felgendreff L, Korn L, Betsch C. Money is not everything: experimental evidence that payments do not increase willingness to be vaccinated against COVID-19. J Med Ethics. (2021) 47:547. doi: 10.1136/medethics-2020-107122
42. Sprengholz P, Henkel L, Betsch C. Payments and freedoms: effects of monetary and legal incentives on COVID-19 vaccination intentions in Germany. PLoS ONE. (2022) 17:e0268911. doi: 10.1371/journal.pone.0268911
43. Taber JM, Thompson CA, Sidney PG, O'Brien A, Updegraff J. Promoting vaccination with lottery incentives. PsyArXiv [Preprint]. (2021). doi: 10.31234/osf.io/ux73h
44. Thirumurthy H, Milkman KL, Volpp KG, Buttenheim AM, Pope DG. Association between statewide financial incentive programs and COVID-19 vaccination rates. PLoS ONE. (2022) 17:e0263425. doi: 10.1371/journal.pone.0263425
45. Walkey AJ, Law A, Bosch NA. Lottery-based incentive in Ohio and COVID-19 vaccination rates. JAMA. (2021) 326:766–7. doi: 10.1001/jama.2021.11048
46. Largent EA, Miller FG. Problems with paying people to be vaccinated against COVID-19. JAMA. (2021) 325:534–5. doi: 10.1001/jama.2020.27121
47. Persad G, Emanuel EJ. Ethical considerations of offering benefits to COVID-19 vaccine recipients. JAMA. (2021) 326:221–2. doi: 10.1001/jama.2021.11045
48. Salali GD, Uysal MS. Effective incentives for increasing COVID-19 vaccine uptake. Psychol Med. (2021) 1–3. doi: 10.1017/S0033291721004013
Keywords: COVID-19, vaccination, incentive, lottery, cash
Citation: Mardi P, Djalalinia S, Kargar R, Jamee M, Esmaeili Abdar Z and Qorbani M (2022) Impact of incentives on COVID-19 vaccination; A systematic review. Front. Med. 9:810323. doi: 10.3389/fmed.2022.810323
Received: 06 November 2021; Accepted: 09 August 2022;
Published: 08 September 2022.
Edited by:
Sara Manti, University of Catania, ItalyReviewed by:
Chandra Dhakal, CDC Foundation, United StatesNaser Piri, Hamedan University of Medical Sciences, Iran
Copyright © 2022 Mardi, Djalalinia, Kargar, Jamee, Esmaeili Abdar and Qorbani. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Mostafa Qorbani, mqorbani1379@yahoo.com
 Parham Mardi
Parham Mardi Shirin Djalalinia
Shirin Djalalinia Reza Kargar
Reza Kargar Mahnaz Jamee
Mahnaz Jamee Zahra Esmaeili Abdar1
Zahra Esmaeili Abdar1  Mostafa Qorbani
Mostafa Qorbani