Drastic Reductions in Mental Well-Being Observed Globally During the COVID-19 Pandemic: Results From the ASAP Survey
- 1Department of Sports Medicine, Goethe University Frankfurt, Frankfurt, Germany
- 2Faculty of Medicine, Medical School Hamburg, Hamburg, Germany
- 3Department of Physical Medicine and Rehabilitation, Spaulding Rehabilitation Hospital and Harvard Medical School, Charlestown, MA, United States
- 4Inter-University Laboratory of Human Movement Science (LIBM EA 7424), University of Lyon, University Jean Monnet, Saint Etienne, France
- 5Department of Clinical and Exercise Physiology, Sports Medicine Unity, Faculty of Medicine, University Hospital of Saint-Etienne, Saint-Etienne, France
- 6Department of Movement, Human and Health Sciences, University of Rome “Foro Italico”, Rome, Italy
- 7ImFine Research Group, Department of Health and Human Performance, Universidad Politécnica de Madrid, Madrid, Spain
- 8Exercise is Medicine Spain, Madrid, Spain
- 9School of Physical Activity Sciences, University of Santiago de Chile, Santiago, Chile
- 10Fundación Instituto Superior de Ciencias de la Salud, Buenos Aires, Argentina
- 11Department of Sport and Exercise Medicine, Changi General Hospital, Singapore, Singapore
- 12Department of Basic Medical Sciences, Durban University of Technology, Durban, South Africa
- 13MOVE-IT Research Group, Department of Physical Education, Faculty of Education Sciences, University of Cádiz, Cádiz, Spain
- 14Institute of Human Movement Science, Sport and Health, University of Graz, Graz, Austria
- 15Department of Orthopedics, University Children's Hospital Basel, University of Basel, Basel, Switzerland
- 16School of Human Movement and Nutrition Sciences, The University of Queensland, Brisbane, QLD, Australia
- 17Institute of Biomechanics and Orthopaedics, German Sport University Cologne, Cologne, Germany
- 18Amsterdam Collaboration on Health and Safety in Sports, Department of Public and Occupational Health, Amsterdam Movement Sciences, Amsterdam UMC, University Medical Centers—Vrije Universiteit Amsterdam, Amsterdam, Netherlands
- 19Masters and Doctoral Programs in Physical Therapy, Universidade Cidade de São Paulo (UNICID), São Paulo, Brazil
Most countries affected by the COVID-19 pandemic have repeatedly restricted public life to control the contagion. However, the health impact of confinement measures is hitherto unclear. We performed a multinational survey investigating changes in mental and physical well-being (MWB/PWB) during the first wave of the pandemic. A total of 14,975 individuals from 14 countries provided valid responses. Compared to pre-restrictions, MWB, as measured by the WHO-5 questionnaire, decreased considerably during restrictions (68.1 ± 16.9 to 51.9 ± 21.0 points). Whereas 14.2% of the participants met the cutoff for depression screening pre-restrictions, this share tripled to 45.2% during restrictions. Factors associated with clinically relevant decreases in MWB were female sex (odds ratio/OR = 1.20, 95% CI: 1.11–1.29), high physical activity levels pre-restrictions (OR = 1.29, 95% CI 1.16–1.42), decreased vigorous physical activity during restrictions (OR = 1.14, 95% CI: 1.05–1.23), and working (partially) outside the home vs. working remotely (OR = 1.29, 95% CI: 1.16–1.44/OR = 1.35, 95% CI: 1.23–1.47). Reductions, although smaller, were also seen for PWB. Scores in the SF-36 bodily pain subscale decreased from 85.8 ± 18.7% pre-restrictions to 81.3 ± 21.9% during restrictions. Clinically relevant decrements of PWB were associated with female sex (OR = 1.62, 95% CI: 1.50–1.75), high levels of public life restrictions (OR = 1.26, 95% CI: 1.18–1.36), and young age (OR = 1.10, 95% CI: 1.03–1.19). Study findings suggest lockdowns instituted during the COVID-19 pandemic may have had substantial adverse public health effects. The development of interventions mitigating losses in MWB and PWB is, thus, paramount when preparing for forthcoming waves of COVID-19 or future public life restrictions.
Introduction
The pandemic associated with the novel coronavirus SARS-CoV2 (commonly referred to as COVID-19) has been managed using a variety of containment strategies. States with known cases instituted restrictions in public travel, school and business closures, stay-at-home orders, and quarantines. Despite their effectiveness in limiting virus transmission (1), lockdowns may have detrimental consequences for health. Even with no restrictions in place, social isolation results in a 29% higher mortality risk (2). Investigations of quarantine effects for previous pandemics (e.g., Ebola, MERS, and SARS) identified the occurrence of post-traumatic stress syndromes, confusion, anger, or symptoms of depression (3). In addition to reducing interpersonal contact, confinements rendered gyms, sports clubs, and public spaces inaccessible. This is of relevance because regular movement is associated with positive affect and life satisfaction (4). Furthermore, active individuals exhibit better nociceptive inhibition and have a lower risk of suffering from musculoskeletal disorders when compared with sedentary persons (5). In sum, it could be speculated that lockdowns cause decreases in both physical and mental well-being.
So far, the health impact of public life restrictions related to COVID-19 has mostly been examined in individual countries. For instance, reports from China (6, 7), Italy (8), and Greece (9) suggest considerable increases in anxiety and depression. As confinement measures affect an estimated minimum of 4 billion people worldwide (10), exploring changes in mental well-being on a multinational scale is an urgent need. The same applies to physical well-being. To the best of our knowledge, changes in the prevalence of musculoskeletal pain and related disability have not been studied. The present study, therefore, investigated the hypothesis that restricting public life to address the COVID-19 pandemic is globally associated with decreases in markers of psychological and physical health.
Materials and Methods
Ethics and Design
We report data from the Activity and Health during the SArs-CoV2 Pandemic (ASAP) survey (11), which was performed in April and May 2020. Ethics approval was obtained in each of the involved 14 countries (Australia, Austria, Argentina, Brazil, Chile, France, Germany, Italy, Netherlands, South Africa, Singapore, Switzerland, Spain, and the United States). Participants were 18 and older from countries with (1) official cases of SARS-CoV2 and (2) confinement measures limiting movement in public spaces. Recruitment strategies included social media promotion, mailing lists, and health-related organizations.
Assessment
The well-being section of the ASAP questionnaire consisted of three parts. The first used a Likert scale to gauge the overall impact of public life restrictions on (a) mental and (b) physical well-being. In the second part, mental well-being was assessed by means of the World Health Organization Well-Being Index (WHO-5) questionnaire. It retrospectively measures agreement with five statements (feeling cheerful and in good spirits, feeling calm and relaxed, feeling active and vigorous, waking up feeling fresh and relaxed, having a daily life being filled with things of interest). Each item is answered on a Likert scale (0 = at no time, 1 = some of the time, 2 = less than half of the time, 3 = more than half of the time, 4 = most of the time, 5 = all of the time). A total score is calculated by multiplying the sum of all item values by four. The instrument is available in multiple languages and has high reliability and validity as a screening tool for depression (12): A sum score of ≤50 has been shown to exhibit 86% sensitivity and 81% specificity for a “screening diagnosis” of depression (12). The WHO-5 was answered twice, once referring to a typical period before public life restrictions and once referring to the time during restrictions.
In the third part, physical well-being was measured using the bodily pain subscale of the SF-36 questionnaire (SF-36 BPS). The instrument asks two questions assessing musculoskeletal pain (6-point Likert scale from “none” to “very severe”) and the resulting disability (5-point Likert scale from “not at all” to “extreme”). For the composite score, the average of both items is calculated and translated to a 0–100 scale. The SF-36 BPS is cross-culturally adapted and has both high internal consistency and reliability (13). To complement the results from the SF-36 BPS, we examined locations of musculoskeletal pain by adapting a checklist from a consensus statement on the reporting of epidemiological injury data (14). Also, the SF-36 BPS and the pain location checklist were completed twice: once for the time period preceding and once for the period during public life restrictions.
In addition to the background variables assessed in the ASAP questionnaire (sex, age, physical activity, work mode, and work volume), the level of national public life restrictions during the assessment period was quantified by means of the Containment and Health Index (15). The instrument systematically evaluates the governmental measures taken to contain viral spread (e.g., business closures, contact restrictions/tracing). The resulting score ranges between 1 and 100 with higher values representing stronger restrictions.
Data Processing and Statistics
We conducted wave analyses to estimate the risk of nonresponse bias (16). Then, first, well-being changes from pre- to during restrictions were examined using Wilcoxon tests (Likert ratings of physical/mental well-being, subdimensions of the WHO-5 index) and paired t-tests for dependent samples (WHO-5 and SF-36 BPS scores), respectively. For the WHO-5, in addition to the sum score, the portion of participants below the cutoff for depression screening (≤50) pre- and during restrictions was determined.
In a second step, binary logistic regression (dependent variables: clinically relevant WHO-5 decrease of ≥10 (12) or minimally important SF-36 BPS decrease of ≥10 [13]) was used to calculate adjusted odds ratios (OR) including 95% confidence intervals for variables potentially moderating reductions in well-being. All data analyses were performed using SPSS 22 (SPSS Inc., Armonk, NY, USA). The significance level was set to α = 0.05.
Results
Our sample consisted of 14,975 participants (38 ± 15 years, 58.1% females) from 14 countries. Levels of national public life restrictions were highest in Argentina, South Africa, and France and lowest in Brazil, Australia, and Switzerland (Table 1). Wave analyses yielded no indication of nonresponse bias (p < 0.05).
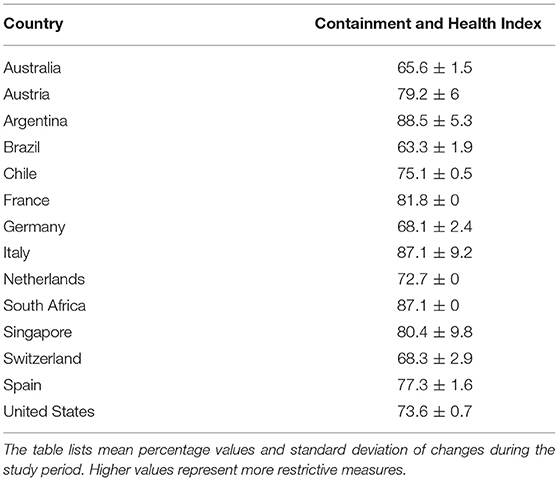
Table 1. Strength of governmental public life restrictions in the included countries as measured with the Containment and Health Index.
Changes in Mental Well-Being
On the Likert scale, 73.0% (n = 10,916) of the participants reported a reduction in overall mental well-being although an improvement was indicated by 14.2% (n = 2130). Like the global rating (p < 0.001), also the WHO-5 score declined significantly from 68.1 ± 16.9 to 51.9 ± 21.0 during restrictions (p < 0.001, Figure 1). In the vast majority of cases (80.6%), the observed reductions were clinically relevant. Decreases were found on all items of the WHO-5 with highest reductions in “feeling active and vigorous” and “having a life filled with interesting things” (p < 0.001, Table 2). Pre-restrictions, 14.2% (n = 2,133) of participants met the cutoff for depression screening. This portion increased to 45.2% (n = 6,765) during restrictions.
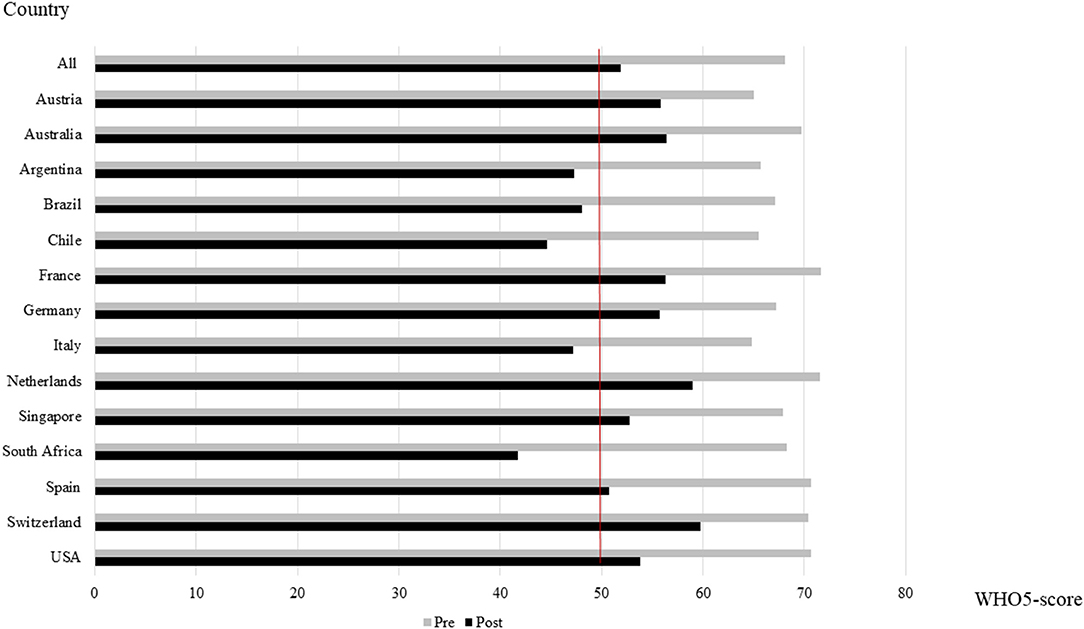
Figure 1. Mental well-being (mean WHO-5 sum score) pre- and during public life restrictions in all included countries. The red line indicates the cutoff score for depression screening (50%).
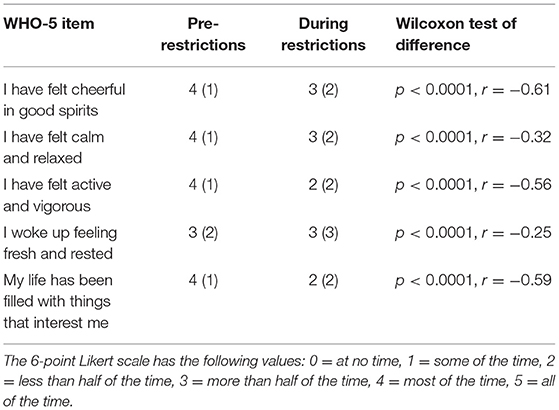
Table 2. Subdimensions of the WHO-5 index before and during public life restrictions (median and interquartile range).
Clinically relevant reductions of the WHO-5 score were associated with high physical activity levels pre-restrictions (OR = 1.29, 95% CI: 1.16–1.42), decreased vigorous physical activity during restrictions (OR = 1.14, 95% CI: 1.05–1.23), female sex (OR = 1.20, 95% CI: 1.11–1.29), working outside the home vs. working remotely (OR = 1.29, 95% CI: 1.16–1.44), and the combination of both vs. working remotely (OR = 1.35, 95% CI: 1.23–1.47). No associations were found for work volume (p = 0.42), age (p = 0.27), level of national public restrictions (p = 0.54), and changes in total physical activity during restrictions (p = 0.77).
Changes in Physical Well-Being
Almost two thirds (64.2%; n = 9,594) of the participants reported a reduction in overall physical well-being although an improvement was indicated by 20.0% (n = 2,985) of the surveyed individuals. Values on the SF-36 BPS decreased from 85.8 ± 18.7 to 81.3 ± 21.9% (p < 0.001). Regarding individual items, score reductions were higher for musculoskeletal pain (−7.1%) than for resulting disability (−3.8%). Prevalence of pain (Figure 2) increased in all body locations with the highest increments in the lower back (+8.4%), neck (+8.1%), and thoracic spine (+5.3%).
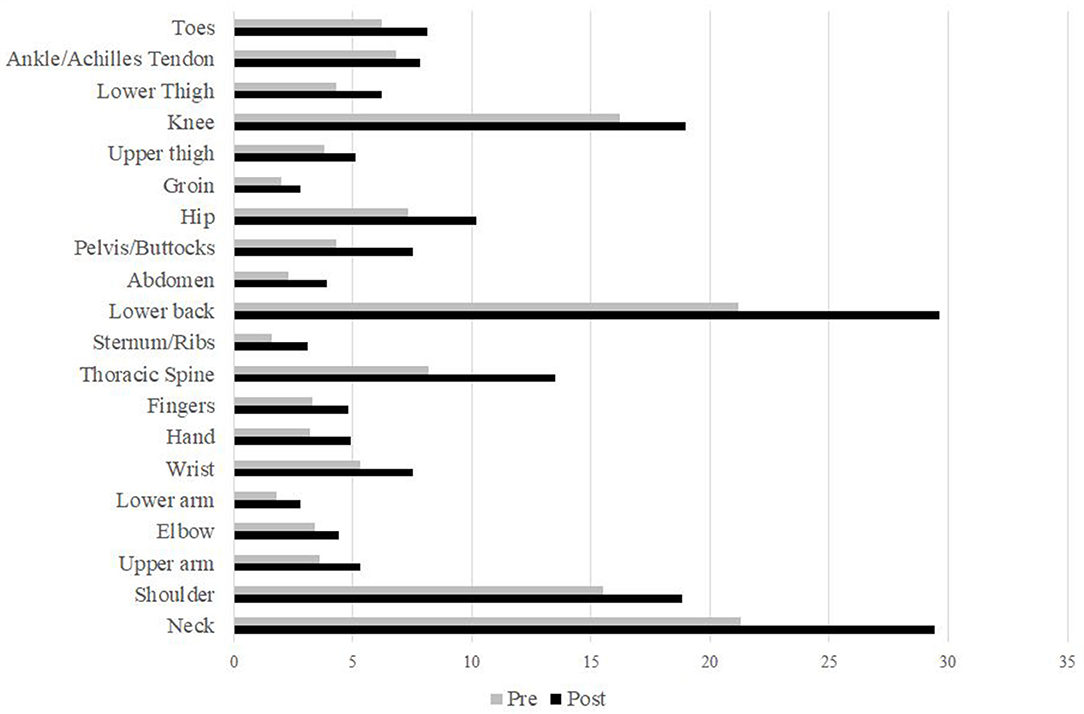
Figure 2. Prevalence [%] of musculoskeletal pain pre- and during public life restrictions stratified by body locations.
Clinically relevant decrements in physical well-being were associated with female sex (OR = 1.62, 95% CI: 1.50–1.75), high levels of national public life restrictions (OR = 1.26, 95% CI: 1.18–1.36), and young age (OR = 1.10, 95% CI: 1.03–1.19). No associations were found for work mode (p = 0.76), work volume (p = 0.10), pre-restriction physical activity level (p = 0.23), or moderate (p = 0.90) and vigorous physical activity (p = 0.22) during restrictions.
Discussion
To the best of our knowledge, this is the first large-scale multinational investigation of physical and mental well-being during the first wave of the COVID-19 pandemic. Although confinement strategies seem effective in curbing the spread of the virus, they may entail a series of adverse health consequences. Most notably, the number of individuals at risk for depression has tripled during lockdowns. With almost half of our sample then falling below the screening cutoff, the reductions in mental well-being, observed across 14 countries, validate and expand available data from other pandemics (3) and early COVID-19 reports [e.g., (6–10)].
Impairments were smaller for physical than for mental well-being. In the first place, this may mean that interventions aiming to mitigate negative health consequences associated with lockdowns should particularly emphasize psychological aspects. However, careful consideration is still needed when aiming to interpret the seemingly low decreases in physical health. The SF-36 BPS combines ratings on musculoskeletal pain and disability. Most theoretical models assume that pain needs to be maintained for a certain period of time until disability manifests (17). Moreover, disability is significantly moderated by psychological distress and fear (17). As the survey referred to a period of a few weeks and as impairments in mental well-being were strong, a more pronounced increase in pain and dysfunction would be plausible at a later point in time.
Our results represent a call to action for health providers and policy makers. Impaired psychological well-being increases not only the odds of depression but also mortality risk (18). This highlights the importance of recognizing the negative mental health consequences during pandemic-related confinements. Newly developed interventions should specifically address the needs of women, who had higher odds for clinically relevant reductions in both the WHO-5 and the SF-36 BPS. Regarding psychological well-being, the present study's findings align with a wealth of evidence demonstrating a gender gap with a higher depression susceptibility of females (19). In summary, health stakeholders need to be aware that restrictions in public life may be associated with substantial decrements in mental and physical well-being. Interestingly, we found only a modest relationship between the restriction level and lower SF-36 values and no relationship between the restriction level and the WHO-5 scores. This may be because the Containment and Health Index contains several elements that are not directly related to individual well-being (e.g., contact tracing and testing paradigm).
Two strategies seem of value to mitigate losses in physical and, particularly, mental well-being. Existing literature suggests working remotely is associated with lower stress levels and decreased risk of depression (20, 21). Also, our survey revealed smaller odds for mental well-being reductions in persons working from home. Besides encouraging and allowing employees to change the workplace, the promotion of regular physical activity could be helpful. Reductions in vigorous activity during restrictions and a high baseline activity prior to restrictions were both related to declines in WHO-5 scores. This means that (a) having been active prepandemic is not protective against well-being decrements and (b) that the development of strategies aiming to maintain the previous movement habits is urgently needed.
Our survey provides strong indications of a subjective well-being decrease in the vast majority of participants. However, it is of interest that a substantial proportion also displayed improvements: One in seven individuals reported increased mental health, and one in five reported improved physical health. Possible reasons for this may include a variety of factors, such as higher amounts of time spent with family, higher task autonomy, reduced work-related travel, or reevaluation of personal health priorities.
Finally, some methodological aspects merit consideration. Our cross-sectional study used retrospective questions. It has been shown that self-reports of health outcomes may be affected by recall bias if relating to the past (22). Although we used relatively short time periods (days to weeks), this phenomenon cannot be ruled out entirely in the examined sample. Another issue relates to the influence and control of background variables: Although we assessed many factors, including age, sex, physical activity levels, work mode, and work volume, it would, inter alia, have been valuable to collect additional sociodemographic data, such as education, profession, and income.
Conclusions
Confinements in countries affected by the novel coronavirus may have caused major reductions in subjective well-being. Strategies promoting telecommuting and maintenance of physical activity may help prevent similar losses in future pandemics or forthcoming waves of COVID-19.
Data Availability Statement
The datasets presented in this article are not readily available because only aggregated data can be shared as per ethics approval. Requests to access the datasets should be directed to Jan Wilke, wilke@sport.uni-frankfurt.de.
Ethics Statement
The study was approved by the Ethics committee of the Faculty of Psychology and Sports Sciences, Goethe University. The participants provided informed consent to participate in this study.
Author Contributions
JW: concept/design, data collection, analysis, interpretation, writing, and critical revision. KH, LM, and AT: concept/design, data collection, analysis, interpretation, and critical revision. PE, CF, MG-G, CS, FL, BT, JP, FP, DJ-P, MS, JJ, MZ, MP, CH, SW, LV, EV, and LH: data collection, interpretation, writing, and critical revision. All authors contributed to the article and approved the submitted version.
Funding
DJ-P is supported by a grant from the Spanish Ministry of Science and Innovation—MINECO (RYC-2014-16938). The research fellowship of KH was funded by the German Research Foundation (Grant no. HO 6214/2-1).
Conflict of Interest
The authors declare that the research was conducted in the absence of any commercial or financial relationships that could be construed as a potential conflict of interest.
References
1. Tobías A. Evaluation of the lockdowns for the SARS-CoV-2 epidemic in Italy and Spain after one month follow up. Sci Total Environ. (2020) 725:138539. doi: 10.1016/j.scitotenv.2020.138539
2. Holt-Lunstad J, Smith TB, Baker M, Harris T, Stephenson D. Loneliness and social isolation as risk factors for mortality: a meta-analytic review. Perspect Psychol Sci. (2015) 10:227–37. doi: 10.1177/1745691614568352
3. Brooks SK, Webster RK, Smith LE, Woodland L, Wessely S, Greenberg N, et al. The psychological impact of quarantine and how to reduce it: rapid review of the evidence. Lancet. (2020) 395:912–20. doi: 10.1016/S0140-6736(20)30460-8
4. Wiese CW, Kuykendall L, Tay L. Get active? A meta-analysis of leisure-time physical activity and subjective well-being. J Pos Psychol. (2016) 13:57–66. doi: 10.1080/17439760.2017.1374436
5. Sulutvedt Holth H, Buchardt Werpen HK, Hagen K. Physical inactivity is associated with chronic musculoskeletal complaints 11 years later: results from the Nord-Trøndelag Health Study. BMC Muskuloskel. Disord. (2008) 9:159. doi: 10.1186/1471-2474-9-159
6. Huang Y, Zhao N. Generalized anxiety disorder, depressive symptoms and sleep quality during COVID-19 outbreak in China: a web-based cross-sectional survey. Psychiatr Res. (2020) 288:112954. doi: 10.1016/j.psychres.2020.112954
7. Wang C, Pan R, Wan X, Tan Y, Xu L, Ho CS, et al. Immediate psychological responses and associated factors during the initial stage of the 2019 coronavirus disease (COVID-19) epidemic among the general population in China. Int J Environment Res Pub Health. (2020) 15:1729. doi: 10.3390/ijerph17051729
8. Fiorenzato E, Zabberoni S, Costa A, Cona G. Cognitive and mental health changes and their vulnerability factors related to COVID-19 lockdown in Italy. PLoS One. (2021) 16:e0246204. doi: 10.1371/journal.pone.0246204
9. Fountoulakis KN, Apostolidou MK, Atsiova MB, Filippidou AK, Florou AK, Gousiou DS, et al. Self-reported changes in anxiety, depression and suicidality during the COVID-19 lockdown in Greece. J Affect Disord. (2021) 279:624–9. doi: 10.1016/j.jad.2020.10.061
10. Simpson RJ, Katsanis E. The immunological case for staying active during the COVID-19 pandemic. Brain Behav Immun. (2020) 87:6–7. doi: 10.1016/j.bbi.2020.04.041
11. Wilke J, Mohr L, Tenforde AS, Vogel O, Hespanhol L, Vogt L, et al. Activity and health during the SARS-CoV2 pandemic (ASAP): study protocol for a multi-national network trial. Front Med. (2020) 7:302. doi: 10.3389/fmed.2020.00302
12. Winther Topp C, Ostergaard SD, Sondergaard S, Bech P. The WHO-5 well-being index: a systematic review of the literature. Psychother Psychosom. (2015) 84:167–76. doi: 10.1159/000376585
13. Hawker GA, Mian S, Kendzerska T, French M. Measures of adult pain: visual analog scale for pain (VAS Pain), numeric rating scale for pain (NRS Pain), McGill pain questionnaire (MPQ), short-form McGill pain questionnaire (SF-MPQ), chronic pain grade scale (CPGS), short form-36 bodily pain scale (SF-36 BPS), and measure of intermittent and constant osteoarthritis pain (ICOAP). Arthritis Care Res. (2011) 63:S240–52. doi: 10.1002/acr.20543
14. Bahr R, Clarsen B, Derman W, et al. International Olympic Committee consensus statement: methods for recording and reporting of epidemiological data on injury and illness in sport 2020 (including STROBE Extension for Sport Injury and Illness Surveillance (STROBE-SIIS)). Br J Sports Med. (2020) 54:372–89. doi: 10.1136/bjsports-2019-101969
15. Thomas H, Angrist N, Cameron-Blake E, Hallas L, Kira B, Majumdar S, Petherick A, Phillips T, Tatlow H, Webster S (2020). Oxford COVID-19 Government Response Tracker. Blavatnik School of Government.
16. Lewis E, Hardy M, Snaith B. Estimating the risk of nonresponse bias in a survey of hospital organizations. Eval Health Prof. (2013) 36:330–51. doi: 10.1177/0163278713496565
17. Lee H, Hübscher M, Moseley L, Kramper SJ, Traeger AC, Mansell G, et al. How does pain lead to disability? A systematic review and meta-analysis of mediation studies in people with back and neck pain. Pain. (2015) 156:988–97. doi: 10.1097/j.pain.0000000000000146
18. Martín-María N, Miret M, Caballero FF, Rico-Uribe LA, Steptoe A, Chatterij S, et al. The impact of subjective well-being on mortality: a meta-analysis of longitudinal studies in the general population. Psychosom Med. (2017) 79:565–75. doi: 10.1097/PSY.0000000000000444
19. Van de Velde S, Bracke P, Levecque K. Gender differences in depression in 23 European countries. Cross-national variation in the gender gap in depression. Soc Sci Med. (2020) 71:305–13. doi: 10.1016/j.socscimed.2010.03.035
20. Henke RM, Benevent R, Schulte P, Rinehart, Crighton KA, Corcoran M. The effect of telecommuting intensity on employee health. Am J Health Promot. (2016) 30:604–12. doi: 10.4278/ajhp.141027-QUAN-544
21. Allen TD, Golden TD, Shockley KM. How effective is telecommuting? Assessing the status of our scientific findings. Psychol Sci Pub Interrest. (2015) 16:40–68. doi: 10.1177/1529100615593273
Keywords: coronavirus, WHO-5, SF-36, psychological health, pain, lockdowns
Citation: Wilke J, Hollander K, Mohr L, Edouard P, Fossati C, González-Gross M, Sánchez Ramírez C, Laiño F, Tan B, Pillay JD, Pigozzi F, Jimenez-Pavon D, Sattler MC, Jaunig J, Zhang M, van Poppel M, Heidt C, Willwacher S, Vogt L, Verhagen E, Hespanhol L and Tenforde AS (2021) Drastic Reductions in Mental Well-Being Observed Globally During the COVID-19 Pandemic: Results From the ASAP Survey. Front. Med. 8:578959. doi: 10.3389/fmed.2021.578959
Received: 01 July 2020; Accepted: 17 February 2021;
Published: 26 March 2021.
Edited by:
Marion C. Aichberger, Humboldt-Universität zu Berlin, GermanyReviewed by:
Luiz Ricardo Berbert, Federal University of Rio de Janeiro, BrazilTam Thi Minh Ta, Charité University Medicine Berlin, Berlin, Germany
Copyright © 2021 Wilke, Hollander, Mohr, Edouard, Fossati, González-Gross, Sánchez Ramírez, Laiño, Tan, Pillay, Pigozzi, Jimenez-Pavon, Sattler, Jaunig, Zhang, van Poppel, Heidt, Willwacher, Vogt, Verhagen, Hespanhol and Tenforde. This is an open-access article distributed under the terms of the Creative Commons Attribution License (CC BY). The use, distribution or reproduction in other forums is permitted, provided the original author(s) and the copyright owner(s) are credited and that the original publication in this journal is cited, in accordance with accepted academic practice. No use, distribution or reproduction is permitted which does not comply with these terms.
*Correspondence: Jan Wilke, wilke@sport.uni-frankfurt.de
 Jan Wilke
Jan Wilke Karsten Hollander
Karsten Hollander Lisa Mohr
Lisa Mohr Pascal Edouard
Pascal Edouard Chiara Fossati6
Chiara Fossati6  Marcela González-Gross
Marcela González-Gross Julian David Pillay
Julian David Pillay David Jimenez-Pavon
David Jimenez-Pavon Matteo C. Sattler
Matteo C. Sattler Johannes Jaunig
Johannes Jaunig Christoph Heidt
Christoph Heidt Steffen Willwacher
Steffen Willwacher Evert Verhagen
Evert Verhagen Luiz Hespanhol
Luiz Hespanhol