Abstract
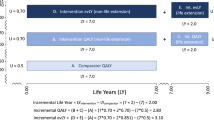
A shortcoming of many economic evaluations is that they do not include all medical costs in life-years gained (also termed indirect medical costs). One of the reasons for this is the practical difficulties in the estimation of these costs. While some methods have been proposed to estimate indirect medical costs in a standardized manner, these methods fail to take into account that not all costs in life-years gained can be estimated in such a way. Costs in lifeyears gained caused by diseases related to the intervention are difficult to estimate in a standardized manner and should always be explicitly modelled. However, costs of all other (unrelated) diseases in life-years gained can be estimated in such a way.
We propose a conceptual model of how to estimate costs of unrelated diseases in life-years gained in a standardized manner. Furthermore, we describe how we estimated the parameters of this conceptual model using various data sources and studies conducted in the Netherlands. Results of the estimates are embedded in a software package called ‘Practical Application to Include future Disease costs’ (PAID 1.0). PAID 1.0 is available as a Microsoft® Excel tool (available as Supplemental Digital Content via a link in this article) and enables researchers to ‘switch off’ those disease categories that were already included in their own analysis and to estimate future healthcare costs of all other diseases for incorporation in their economic evaluations.
We assumed that total healthcare expenditure can be explained by age, sex and time to death, while the relationship between costs and these three variables differs per disease. To estimate values for age- and sex-specific per capita health expenditure per disease and healthcare provider stratified by time to death we used Dutch cost-of-illness (COI) data for the year 2005 as a backbone. The COI data consisted of age- and sex-specific per capita health expenditure uniquely attributed to 107 disease categories and eight healthcare provider categories. Since the Dutch COI figures do not distinguish between costs of those who die at a certain age (decedents) and those who survive that age (survivors), we decomposed average per capita expenditure into parts that are attributable to decedents and survivors, respectively, using other data sources.





Similar content being viewed by others
References
Garber AM, Phelps CE. Economic foundations of cost-effectiveness analysis. J Health Econ 1997 Feb; 16 (1): 1–31
Meltzer D, Egleston B, Stoffel D, et al. Effect of future costs on cost-effectiveness of medical interventions among young adults: the example of intensive therapy for type 1 diabetes mellitus. Med Care 2000 Jun; 38 (6): 679–85
Nyman JA. Should the consumption of survivors be included as a cost in cost-utility analysis? Health Econ 2004 May; 13 (5): 417–27
van Baal PH, Feenstra TL, Hoogenveen RT, et al. Unrelated medical care in life years gained and the cost utility of primary prevention: in search of a ‘perfect’ cost-utility ratio. Health Econ 2007 Apr; 16 (4): 421–33
Lee RH. Future costs in cost effectiveness analysis. J Health Econ 2008 Jul; 27 (4): 809–18
Meltzer D. Response to ‘Future costs and the future of cost-effectiveness analysis’. J Health Econ 2008 Jul; 27 (4): 822–5
Feenstra TL, van Baal PH, Gandjour A, et al. Future costs in economic evaluation: a comment on Lee. J Health Econ 2008 Dec; 27 (6): 1645–9; discussion 1650–1
Rappange DR, van Baal PH, van Exel NJ, et al. Unrelated medical costs in life-years gained: should they be included in economic evaluations of healthcare interventions? Pharmacoeconomics 2008; 26 (10): 815–30
National Institute for Health and Clinical Excellence. Guide to the methods of technology appraisal. London: NICE, 2008 Jun
Rapport Richtlijnen voor farmaco-economisch onderzoek; evaluatie en actualisatie. Diemen: College voor Zorgverzekeringen, 2006
van Baal PHM, Feenstra TL, Polder JJ, et al. Economic evaluation and the postponement of health care costs. Health Econ. Epub 2010 Apr 5
Manns B, Meltzer D, Taub K, et al. Illustrating the impact of including future costs in economic evaluations: an application to end-stage renal disease care. Health Econ 2003 Nov; 12 (11): 949–58
de Kok I, Polder J, Habbema J, et al. The impact of healthcare costs in the last year of life and in all life years gained on the cost-effectiveness of cancer screening. Br J Cancer 2009; 100 (8): 1240–4
van den Berg M, van Baal PH, Tariq L, et al. The cost-effectiveness of increasing alcohol taxes: a modelling study. BMC Med 2008 Nov 28; 6: 36
van Baal PH, van den Berg M, Hoogenveen RT, et al. Cost-effectiveness of a low-calorie diet and orlistat for obese persons: modeling long-term health gains through prevention of obesity-related chronic diseases. Value Health 2008 Dec; 11 (7): 1033–40
Zweifel P, Felder S, Meiers M. Ageing of population and health care expenditure: a red herring? Health Econ 1999 Sep; 8 (6): 485–96
Polder JJ, Barendregt JJ, van Oers H. Health care costs in the last year of life: the Dutch experience. Soc Sci Med 2006 Oct; 63 (7): 1720–31
Seshamani M, Gray A. Ageing and health-care expenditure: the red herring argument revisited. Health Econ 2004 Apr; 13 (4): 303–14
Hakkinen U, Martikainen P, Noro A, et al. Aging, health expenditure, proximity to death, and income in Finland. Health Econ Policy Law 2008 Apr; 3 (Pt 2): 165–95
O’Neill C, Groom L, Avery AJ, et al. Age and proximity to death as predictors of GP care costs: results from a study of nursing home patients. Health Econ 2000 Dec; 9 (8): 733–8
Werblow A, Felder S, Zweifel P. Population ageing and health care expenditure: a school of ‘red herrings’? Health Econ 2007 Oct; 16 (10): 1109–26
Wong A, van Baal PH, Boshuizen HC, et al. Exploring the influence of proximity to death on disease-specific hospital expenditures: a carpaccio of red herrings. Health Econ. Epub 2010 Mar 15
Gandjour A, Lauterbach KW. Does prevention save costs? Considering deferral of the expensive last year of life. J Health Econ 2005 Jul; 24 (4): 715–24
Poos M, Smit J, Groen J, et al. Kosten van ziekten in Nederland 2005. Bilthoven: RIVM, 2008. RIVM rapport no. 270751019
Polder JJ, Meerding WJ, Koopmanschap MA, et al. The cost of sickness in the Netherlands in 1994: the main determinants were advanced age and disabling conditions. Ned Tijdschr Geneeskd 1998 Jul 11; 142 (28): 1607–11
Meerding WJ, Bonneux L, Polder JJ, et al. Demographic and epidemiological determinants of healthcare costs in Netherlands: cost of illness study. BMJ 1998 Jul 11; 317 (7151): 111–5
Slobbe L, Kommer G, Smit J, et al. Kosten van ziekten in Nederland 2003. Zorg voor euro’s-1. Bilthoven: RIVM, 2006
Orosz E, Morgan D. SHA-based national health accounts in thirteen OECD countries: a comparative analysis. OECD health working papers no. 16. Paris: OECD, 2004 [online]. Available from URL: http://www.oecd.org/dataoecd/10/53/33661480.pdf [Accessed 2010 Jan 1]
Voorburg/Heerlen, Netherlands Central Bureau of Statistics 1999 [online]. Available from URL: http://www.statline.nl [Accessed 2010 Jan 1]
Heijink R, Noethen M, Renaud T, et al. Cost of illness: an international comparison. Australia, Canada, France, Germany and the Netherlands. Health Policy 2008 Oct; 88 (1): 49–61
Payne G, Laporte A, Deber R, et al. Counting backward to health care’s future: using time-to-death modeling to identify changes in end-of-life morbidity and the impact of aging on health care expenditures. Milbank Q 2007; 85 (2): 213–57
Acknowledgements
The study was supported by a grant from the Dutch National Institute for Public Health and the Environment Strategic Research Fund (SOR S/260186/01/FU) and the Dutch Ministry of Health, Welfare and Sports, with full freedom of research and publication. The authors have no conflicts of interest that are directly relevant to the content of this article.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
van Baal, P.H., Wong, A., Slobbe, L.C. et al. Standardizing the Inclusion of Indirect Medical Costs in Economic Evaluations. Pharmacoeconomics 29, 175–187 (2011). https://doi.org/10.2165/11586130-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11586130-000000000-00000