Abstract
Background: As Parkinson’s disease (PD) progresses, patients and their families experience substantial health and economic burdens. Because motor fluctuations (also called ‘off-time’) are linked to poor quality of life and higher healthcare costs, minimizing off-time is an effective strategy for reducing costs associated with PD.
Objective: To assess the cost utility of rasagiline or entacapone as adjunctive therapies to levodopa versus levodopa/carbidopa/entacapone (LCE) versus standard levodopa monotherapy in patients with advanced PD and motor fluctuations in the US.
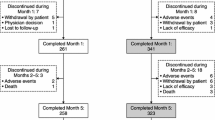
Methods: A 2-year stochastic Markov model was utilized to examine the cost effectiveness of treatments of advanced PD. The model assumed that patients transition health status every 4 months. Transition probabilities, including uncertainties, were estimated from clinical trial data. Medical costs, daily drug costs and utility weights were obtained from published literature.
Results: Over 2 years, all therapy options showed greater effectiveness than levodopa alone. Rasagiline + levodopa and LCE were cost saving from a payor perspective, while entacapone + levodopa was cost saving from a societal perspective. Mean benefits over 2 years were 0.12 (90% credibility interval [CI] 0.07, 0.18) additional quality-adjusted life-years (QALYs) for rasagiline + levodopa, entacapone + levodopa and LCE, 5.08 (90% CI 3.87, 6.28) additional months with ≤25% off-time for rasagiline + levodopa and 4.85 (90% CI 3.63, 6.06) additional months with ≤25% off-time for entacapone + levodopa and LCE versus levodopa alone.
Conclusion: From a payor perspective, rasagiline + levodopa and LCE were dominant therapies over levodopa monotherapy, while entacapone+ levodopa was effective at a higher cost. With no additional cost over a 2-year period, rasagiline + levodopa presents a valuable alternative to entacapone + levodopa, LCE and levodopa monotherapy in the treatment of advanced PD patients. Results from this cost-utility model and prior adjunctive clinical data provide ongoing support for the adjunctive use of rasagiline in advanced PD patients with motor fluctuations.







Similar content being viewed by others
References
Tanner CM, Goldman SM. Epidemiology of Parkinson’s disease. Neurol Clin 1996; 14: 317–35
Oertel WH, Quinn NP. Parkinsonism. In: Brandt T, Caplan LR, Dichgans J, et al., editors. Neurological disorders: course and treatment. San Diego (CA): Academic Press, 1996: 715–72
Hudry J, Rinne JO, Keränen T, et al. Cost-utility model of rasagiline in the treatment of advanced Parkinson’s disease in Finland. Annals Pharmacother 2006; 40: 651–7
Dodel RC, Singer M, Kohne-Volland R, et al. The economic impact of Parkinson’s disease: an estimation based on a 3-months prospective analysis. Pharmacoeconomics 1998; 14: 299–312
Vose D. Risk analysis, a quantitative guide. 3rd ed. Hoboken (NJ): John Wiley & Sons, 2008
Gold MR, Siegel JE, Russell LB, et al. Cost-effectiveness in health and medicine. New York: Oxford University Press, 1996
Rascol O, Brooks DJ, Melamed E, et al. Rasagiline as an adjunct to levodopa in patients with Parkinson’s disease and motor fluctuations (LARGO, Lasting effect in Adjunct therapy with Rasagiline Given Once daily, study): a randomized, double-blind, parallel-group trial. Lancet 2005; 365: 947–54
Beck JR, Kassirer JP, Pauker SG. A convenient approximation of life expectancy (the “DEALE”): I. Validation of the method. Am J Med 1982; 73: 833–8
Herlofson L, Lie SA, Arsland D, et al. Mortality and Parkinson disease: a community based study. Neurology 2004; 62: 937–42
Palmer CS, Schmier JK, Snyder E, et al. Patient preferences and utilities for ‘off-time’ outcomes in the treatment of Parkinson’s disease. Qual Life Res 2000; 9: 819–27
Orsini L, Castelli-Haley J, Kennedy S, et al. Healthcare utilization and expenditures among privately insured patients with Parkinson’s disease in the US. Poster presented at the 8th Annual Meeting of the Movement Disorder Society’s International Congress; Jun 2004; Italy
US Department of Labor: Bureau of Labor Statistics. Consumer price index — all urban consumers (current series). 2006 [online]. Available from URL: http://data.bls.gov/PDQ/ outside.jsp?survey=cu [Accessed 2009 Apr 1]
Dodel RC, Berger K, Oertel WH. Health-related quality of life and healthcare utilization in patients with Parkinson’s disease: impact of motor fluctuations and dyskinesias. Pharmacoeconomics 2001; 19: 1013–38
LePen C, Wait S, Moutard-Martin F, et al. Cost of illness and disease severity in a cohort of French patients with Parkinson’s disease. Pharmacoeconomics 1999; 16: 59–69
Whetten-Goldstein K, Sloan F, Kulas E, et al. The burden of Parkinson’s disease on society, family, and the individual. J Am Geriatr Soc 1997; 45: 844–9
Keränen T, Kaakkola S, Sotaniemi K, et al. Economic burden and quality of life impairment increase with severity of PD. Parkinsonism Relat Disord 2003; 9: 163–8
Huse DM, Schulman K, Orsini L, et al. Burden of illness in Parkinson’s disease. Mov Disord 2005; 20: 1449–54
Scheife RT, Schumock GT, Burstein A, et al. Impact of Parkinson’s disease and its pharmacologic treatment on quality of life and economic outcomes. Am J Health-Syst Pharm 2000; 57: 953–62
Red Book for Windows. Version 61127, vol. 50. Montvale (NJ): Thomson PDR, 2009 Jan
World HealthOrganization Collaborating Centre for Drug Statistics Methodology [online]. Available from URL: http://www.whocc.no/atcddd/ [Accessed 2009 Jul 31]
Hoerger TJ, Bala MV, Rowland C, et al. Cost effectiveness of pramipexole in Parkinson’s disease in the US. Pharmacoeconomics 1998; 14: 541–57
Müller T, Voß B, Hellwig K, et al. Treatment benefit and daily drug costs in Parkinson’s disease clinics. CNS Drugs 2004; 18(2): 105–11
Siebert U, Bornschein B, Walbert T, et al. Systematic assessment of decision models in PD. Value Health 2004; 7: 610–26
Grosset KA, Reid JL, Grosset DG. Medicine-taking behavior: implications of suboptimal compliance in Parkinson’s disease. Mov Disord 2005; 20(11): 1397–404
Acknowledgements
The funding source for this manuscript was Teva Neuroscience, Kansas City, MO, USA. Dr Groenendaal is a partner at Vose Consulting US LLC, an independent risk analysis and modeling consulting firm that received research funding for this study from Teva Neuroscience. Dr Tarrants is an employee of Teva Neuroscience, a pharmaceutical company. Dr Armand is an employee of H. Lundbeck A/S and a paid consultant to Teva Neuroscience.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Groenendaal, H., Tarrants, M.L. & Armand, C. Treatment of Advanced Parkinson’s Disease in the United States. Clin. Drug Investig. 30, 789–798 (2010). https://doi.org/10.2165/11538520-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11538520-000000000-00000