Abstract
Economic evaluation of health technologies in the form of cost-utility analysis is increasingly advocated. The most common outcome measure in this type of analysis is the QALY. In order to estimate QALYs, appropriate utility values are required.
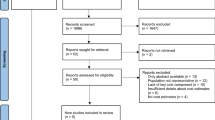
The objective of this review was to identify and critique utility values for schizophrenia-related health states. A critical appraisal was performed on utility values for schizophrenia identified in the systematic literature review that informed the economic analysis of the updated edition of the National Institute for Health and Clinical Excellence (NICE) clinical guideline on schizophrenia for England and Wales.
Seven studies reporting utility values for schizophrenia were identified. The studies employed a variety of methods for generating utility values. None of the reported sets of utility values for schizophrenia were generated using the EQ-5D, which is a measure widely used in cost-utility analysis and preferred by NICE. Nevertheless, the EQ-5D may be less sensitive in capturing aspects of health-related quality of life in patients with schizophrenia.
A condition-specific preference-based instrument may be more appropriate than a generic measure to inform cost-utility analyses of interventions for schizophrenia.


Similar content being viewed by others
References
National Institute for Health and Clinical Excellence. Social value judgements: principles for the development of NICE guidance. 2nd ed. London: NICE, 2008
Pharmaceutical Benefits Advisory Committee. 1995 Guidelines for the pharmaceutical industry on preparation of submission to the Pharmaceutical Benefits Advisory Committee: including major submissions involving economic analyses. Barton (ACT): Australian Government, 1995 [online]. Available from URL: (http://www.health.gov.au/internet/main/publishing.nsf/Content/health-pbsgeneral-pubs-pharmpac-part1.htm) [Accessed 2009 Dec 16]
Russell LB, Gold MR, Siegel JE, et al. The role of costeffectivenessanalysis in health and medicine. JAMA 1996 Oct; 276 (14): 1172–7
Brazier J, Ratcliffe J, Salomon JA, et al. Measuring and valuing health benefits for economic evaluation. New York: Oxford University Press, 2007
Drummond MF, Sculpher MJ, Torrance GW, et al. Methods for the economic evaluation of health care programmes. 3rd ed. New York: Oxford University Press, 2005
Brooks R. EuroQol: the current state of play. Health Policy 1996 Jul; 37 (1): 53–72
Gudex C, Dolan P, Kind P, et al. Health state valuations form the general public using the visual analogue scale. Qual Life Res 1996 Dec; 5 (6): 521–31
Dolan P, Gudex C, Kind P, et al. The time trade-off method: results from a general population study. Health Econ 1996 Mar-Apr; 5 (2): 141–54
Dolan P. Modeling valuations for EuroQol health states. Med Care 1997 Nov; 35 (11): 1095–108
National Institute for Health and Clinical Excellence. Guide to the methods of technology appraisal. London: NICE, 2008
Weinstein MC, Siegel JE, Gold MR, et al. Recommendations of the Panel on Cost-Effectiveness in Health and Medicine. JAMA 1996 Oct; 276 (15): 1253–8
National Institute for Health and Clinical Excellence. Schizophrenia: core interventions in the treatment and management of schizophrenia in adults in primary and secondary care (update). NICE clinical guideline 82. London: NICE, 2009 [online]. Available from URL: (http://www.nice.org.uk/CG82) [Accessed 2010 Aug 20]
National Collaborating Centre for Mental Health. Schizophrenia: the NICE guideline on the core interventions in the treatment and management of schizophrenia in adults in primary and secondary care. Updated ed. Leicester and London: The British Psychological Society and the Royal College of Psychiatrists, 2010
Centre for Reviews and Dissemination. NHS Economic Evaluation Database handbook. York: Centre for Reviews and Dissemination, University of York, 2007 [online]. Available from URL: (http://www.york.ac.uk/inst/crd/pdf/nhseed-handb07.pdf) [Accessed 2009 Oct 20]
Cummins C, Stevens A, Kisely S. The use of olanzapine as a first and second choice treatment in schizophrenia: a West Midlands Development and Evaluation Committee report. Birmingham: University of Birmingham, Department of Public Health and Epidemiology, West Midlands Development and Evaluation Committee, 1998
Oh PI, LanctÔt KL, Mittmann N, et al. Cost-utility of risperidone compared with standard conventional antipsychotics in chronic schizophrenia. JMed Econ 2001; 4 (1-4): 137–56
Oh PI, Iskedjian M, Addis A, et al. Pharmacoeconomic evaluation of clozapine in treatment-resistant schizophrenia: a cost-utility analysis. Can J Clin Pharmacol 2001 Winter; 8 (4): 199–206
Chouinard G, Albright PS. Economic and health state utility determinations for schizophrenic patients treated with risperidone or haloperidol. J Clin Psychopharmacol 1997 Aug; 17 (4): 298–307
Lenert LA, Sturley AP, Rapaport MH, et al. Public preferences for health states with schizophrenia and a mapping function to estimate utilities from positive and negative symptom scale scores [published erratum appears in Schizophr Res 2005 Dec 1; 80 (1): 135-6]. Schizophr Res 2004 Nov 1; 71 (1): 155–65
Revicki DA, Shakespeare A, Kind P. Preferences for schizophrenia-related health states: a comparison of patients, caregivers and psychiatrists. Int Clin Psychopharmacol 1996 Jun; 11 (2): 101–8
Briggs A, Wild D, Lees M, et al. Impact of schizophrenia and schizophrenia treatment-related adverse events on quality of life: direct utility elicitation. Health Qual Life Outcomes 2008 Nov; 6: 105
Rosser R, Cottee M, Rabin R, et al. Index of health-related quality of life. In: Hopkins A, editor. Measures of the quality of life and the uses to which such measures may be put. London: Royal College of Physicians, 1992: 81–90
Barton GR, Hodgekins J, Mugford M, et al. Cognitive behaviour therapy for improving social recovery in psychosis: cost-effectiveness analysis. Schizophr Res 2009 Jul; 112 (1-3): 158–63
De Ridder A, De Graeve D. Comparing the cost effectiveness of risperidone and olanzapine in the treatment of schizophrenia using the net-benefit regression approach. Pharmacoeconomics 2009; 27 (1): 69–80
Knapp M, Windmeijer F, Brown J, et al. Cost-utility analysis of treatment with olanzapine compared with other antipsychotic treatments in patients with schizophrenia in the pan-European SOHO study. Pharmacoeconomics 2008; 26 (4): 341–58
Lewis SW, Davies L, Jones PB, et al. Randomised controlled trials of conventional antipsychotic versus new atypical drugs, and new atypical drugs versus clozapine, in people with schizophrenia responding poorly to, or intolerant of, current drug treatment. Health Technol Assess 2006 May; 10 (17): iii-iv, ix-xi, 1–165
Lenert LA, Rupnow MFT, Elnitsky C. Application of a disease-specific mapping function to estimate utility gains with effective treatment of schizophrenia. Health Qual Life Outcomes 2005 Sep 11; 3: 57
Rosenheck RA, Leslie DL, Sindelar J, et al. Cost-effectiveness of second-generation antipsychotics and perphenazine in a randomized trial of treatment for chronic schizophrenia. Am J Psychiatry 2006 Dec; 163 (12): 2080–9
Gilbody SM, House AO, Sheldon TA. Outcome measurement in psychiatry: a critical review of outcomes measurement in psychiatric research and practice [NHS CRD report no. 23]. York: University of York, 2003 [online]. Available from URL: (http://www.york.ac.uk/inst/crd/CRD_Reports/crdreport24.pdf) [Accessed 2010 Mar 5]
Jacobs R. Investigating patient outcome measures in mental health [CHE research paper no. 48]. York: University of York, 2009 [online]. Available from URL: (http://www.york.ac.uk/inst/che/pdf/rp48.pdf) [Accessed 2010Mar 5]
Prieto L, Sacristán JA, Hormaechea JA, et al. Psychometric validation of a generic health-related quality of life measure (EQ-5D) in a sample of schizophrenic patients. Curr Med Res Opin 2004 Jun; 20 (6): 827–35
König HH, Roick C, Angermeyer MC. Validity of the EQ-5D in assessing and valuing health status in patients with schizophrenic, schizotypal or delusional disorders. Eur Psychiatry 2007 Apr; 22 (3): 177–87
Barton GR, Hodgekins J, Mugford M, et al. Measuring the benefits of treatment for psychosis: validity and responsiveness of the EQ-5D. Br J Psychiatry 2009 Aug; 195 (2): 170–7
van de Willige G, Wiersma D, Nienhuis FJ, et al. Changes in quality of life in chronic psychiatric patients: a comparison between EuroQol (EQ-5D) and WHOQoL. Qual Life Res 2005 Mar; 14 (2): 441–51
Meijer CJ, Schene AH, Koeter MWJ. Quality of life in schizophrenia measured by the MOS SF-36 and the Lancashire Quality of Life Profile. Acta Psychiatr Scand 2002 Apr; 105 (4): 293–300
Leese M, Schene A, Koeter M, et al. SF-36 scales, and simple sums of scales, were reliable quality-of-life summaries for patients with schizophrenia. J Clin Epidemiol 2008 Jun; 61 (6): 588–96
Brazier JE, Roberts J, Deverill M. The estimation of a preference based measure of health from the SF-36. J Health Econ 2002 Mar; 21 (2): 271–92
Brazier J. Measuring and valuing mental health for use in economic evaluation. J Health Serv Res Policy 2008 Oct; 13 Suppl. 3: 70–5
McCrone P, Patel A, Knapp M, et al. A comparison of SF-6D and EQ-5D utility scores in a study of patients with schizophrenia. J Ment Health Policy Econ 2009 Mar; 12 (1): 27–31
Chisholm D, Healey A, Knapp M. QALYs and mental health care. Soc Psychiatry Psychiatr Epidemiol 1997 Feb; 32 (2): 68–75
Knapp M, Mangalore R. The trouble with QALYs.... Epidemiol Psichiatr Soc 2007 Oct-Dec; 16 (4): 289–93
Brazier J, Czoski—Murray C, Roberts J, et al. Estimation of a preference—based index from a condition—specific measure: the King’s Health Questionnaire. Med Decis Making 2008 Feb; 28 (1): 113–26
Sundaram M, Smith MJ, Revicki DA, et al. Rasch analysis informed the development of a classification system for a diabetes-specific preference-based measure of health. J Clin Epidemiol 2009 Aug; 62 (8): 845–56
Yang Y, Brazier J, Tsuchiya A, et al. Estimating a preference-based single index from the Overactive Bladder Questionnaire. Value Health 2009 Jan; 12 (1): 159–66
Yang Y, Tsuchiya A, Brazier JE, et al. Estimating a preference-based single index from the Asthma Quality of Life Questionnaire (AQLQ) [Health Economics and Decision Science discussion paper no. 07/02]. Sheffield: School of Health and Related Research, 2007 [online]. Available from URL: (http://www.shef.ac.uk/content/1/c6/01/87/47/HEDS%20DP%200702v2.pdf) [Accessed 2009 Nov 15]
Brazier J, Deverill M, Green C, et al. A review of the use of health status measures in economic evaluation. Health Technol Assess 1999; 3 (9): i-iv, 1–164
Bebbington PE, Angermeyer M, Azorin JM, et al. Sideeffects of antipsychotic medication and health-related quality of life in schizophrenia. Acta Psychiatr Scand Sup 2009; 119 (438): 22–8
Lee TT, Ziegler JK, Sommi R, et al. Comparison of preferences for health outcomes in schizophrenia among stakeholder groups. J Psychiatr Res 2000 May-Jun; 34 (3): 201–10
Lenert LA, Ziegler J, Lee T, et al. Differences in health values among patients, family members, and providers for outcomes in schizophrenia. Med Care 2000 Oct; 38 (10): 1011–21
Ubel PA, Loewenstein G, Jepson C. Whose quality of life? A commentary exploring discrepancies between health state evaluations of patients and the general public. Qual Life Res 2003 Sep; 12 (6): 599–607
Shumway M. Preference weights for cost-outcome analyses of schizophrenia treatments: comparison of four stakeholder groups. Schizophr Bull 2003; 29 (2): 257–66
Brazier J, Akehurst R, Brennan A, et al. Should patients have a greater role in valuing health states? Appl Health Econ Health Policy 2005; 4 (4): 201–8
Voruganti L-NP, Awad AG, Oyewumi LK, et al. Assessing health utilities in schizophrenia: a feasibility study. Pharmacoeconomics 2000 Mar; 17 (3): 273–86
Acknowledgements
The author would like to thank the Guideline Development Group of the updated edition of the NICE guideline on schizophrenia and especially Ms Sarah Stockton for developing the search strategies and conducting the database searches of economic evidence in the area of schizophrenia. Special acknowledgement is given to Dr Ilias Kazanis (University of Cambridge) for useful comments in the development of the manuscript.
The systematic literature review of utility values for schizophrenia was undertaken to inform the updated edition of the NICE clinical guideline on schizophrenia, developed by the National Collaborating Centre for Mental Health (NCCMH), commissioned and funded by NICE in the UK. The author is an employee of the NCCMH and participated in the development of the updated edition of the NICE clinical guideline on schizophrenia. The views expressed in this paper are those of the author and do not necessarily reflect those of NICE.
No sources of funding were used to assist in the preparation of this review. The author has no conflicts of interest that are directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Mavranezouli, I. A Review and Critique of Studies Reporting Utility Values for Schizophrenia-Related Health States. Pharmacoeconomics 28, 1109–1121 (2010). https://doi.org/10.2165/11537300-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11537300-000000000-00000