Abstract
Objectives
The main aims of the study were to explore whether oral anti-coagulation (OAC) for atrial fibrillation (AF) in geriatric outpatients is prescribed in accordance with international (American College of Cardiology/American Heart Association/European Society of Cardiology [ACC/AHA/ESC]) and Dutch national guidelines for the general practitioner (GP) and to identify whether age and selected co-morbid conditions are associated with undertreatment. As a secondary objective, we wanted to establish how many patients discontinue OAC because of major bleeding.
Methods
In 2004, at the first visit of all patients to the geriatric day clinic of the Slotervaart Hospital in Amsterdam, the Netherlands, demographic data, Mini-Mental State Examination score, medical history, Charlson Comorbidity Index score, and data on medication use and changes were documented. The presence of AF was established by assessment of medical history information obtained by the GP, the history taken from patients and their caregivers, and the results of clinical evaluation, including ECG findings. Associations between the use of OAC, demographic data and co-morbid conditions registered in the Dutch NHG (Nederlands Huisartsen Genootschap [Dutch College of General Practitioners]) standard for GPs as risk factors for stroke or contraindications to the use of OAC were analysed. The reasons for discontinuing OAC were assessed after 4 years by requesting the information from the anticoagulation services or the GP.
Results
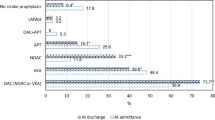
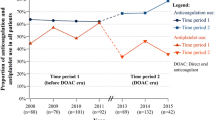
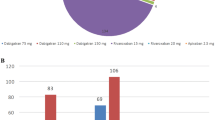
At the time of the initial visit, 17.5% of the 807 outpatients had chronic AF (n= 135) or were known to have paroxysmal AF (n = 6). The mean age of the 141 patients in this cohort was 84.3 years (SD 6.2 years). Co-morbid conditions increasing the risk of stroke were present in 129 patients (91.5%). Contraindications to the use of OAC were observed in 118 patients (83.7%). Of the 116 patients with AF in their history before their visit, 57.8% were being treated with OAC at the time of their visit. After comprehensive geriatric assessment, 73 (51.8%) of the 141 patients with chronic or paroxysmal AF were continued on OAC. Of the 141 patients with chronic or paroxysmal AF, 110 (78.0%) had both extra stroke risk factors and contraindications to the use of OAC. Only increasing age was significantly and independently associated with not being prescribed anticoagulants (p<0.001). At the 4-year follow-up, OAC had been discontinued in 5.5% of patients because of major bleeding; three patients (4.1%) taking OAC had died as a result of major bleeding, and one other patient had discontinued treatment because of a major, non-lethal bleeding episode.
Conclusion
Applying the NHG standard for appropriate prescription, and disregarding age as a risk factor or contraindication, in this population, 14 of 141 patients (9.9%) were inappropriately prescribed OAC, salicylates or no prophylaxis. Since only patient age was associated with not prescribing OAC in this study, higher age still seems to be considered the most important contraindication to anticoagulation therapy. Implementation of better models for stratifying bleeding risk in the frail elderly is needed. After 4 years, the cumulative rate of bleeding causing discontinuation of anticoagulation therapy in this usual-care study of frail older patients was not alarmingly higher than in other usual-care studies.






Similar content being viewed by others
References
Chatap G, Giraud K, Vincent J. Atrial fibrillation in the elderly: facts and management. Drugs Aging 2002; 19: 819–46
Fuster V, Rydén LE, Asinger RW, et al. ACC/AHA/ESC guidelines for the management of patients with atrial fibrillation: executive summary. A report of the American College of Cardiology/American Heart Association Task Force on practice guidelines and the European Society of Cardiology Committee for practice guidelines and policy conferences (Committee to Develop Guidelines for the Management of Patients with Atrial Fibrillation) developed in collaboration with the North American Society of Pacing and Electrophysiology. Circulation 2001; 104: 2118–50
Fuster V, Ryden LE, Cannom DS, et al. ACC/AHA/ESC 2006 guidelines for the management of patients with atrial fibrillation: executive summary. Circulation 2006; 114: 700–52
Laupacis A, Albers G, Dalen J, et al. Antithrombotic therapy in atrial fibrillation. Chest 1998; 114: 579–89
Boode BSP, Frijling BD, Heeringa J, et al. NHG standard atrial fibrillation [in Dutch]. Huisarts Wet 2003; 46: 819–30
Bradley BC, Perdue KS, Tisdel KA, et al. Frequency of anticoagulation for atrial fibrillation and reasons for its non-use at a Veterans Affairs medical center. Am J Cardiol 2000; 85: 568–72
Weisbord SD, Whittle J, Brooks RC. Is warfarin really underused in patients with atrial fibrillation? J Gen Intern Med 2001; 16:743–9
Laguna P, Martín A, del Arco C, et al., on behalf of the Investigators in the Spanish Atrial Fibrillation in Emergency Medicine Study Group (GEFAUR). Risk factors for stroke and thromboprophylaxis in atrial fibrillation: what happens in daily clinical practice? The GEFAUR-1 study. Ann Emerg Med 2004; 44: 3–11
Själander A, Engström G, Berntorp E, et al. Risk of haemorrhagic stroke in patients with oral anticoagulation compared with the general population. J Intern Med 2003; 254: 434–8
Gorter JW. Major bleeding during anticoagulation after cerebral ischemia: patterns and risk factors. Neurology 1999; 53: 1319
Vasishta S, Toor F, Johansen A, et al. Stroke prevention in atrial fibrillation: physicians’ attitudes to anticoagulation in older people. Arch Gerontol Geriatr 2001; 33(3): 219–26
Baker DW, Hayes RP, Massie BM, et al. Variations in family physicians’ and cardiologists’ care for patients with heart failure. Am Heart J 1999; 138: 826–34
Villa A, Bacchetta A, Omboni E, et al. Underuse of antithrombotic therapy in stroke patients with chronic atrial fibrillation response. Stroke 2000; 21: 2266–78
Ceresne L, Upshur RE. Atrial fibrillation in a primary care practice: prevalence and management. BMC Fam Prac 2002; 3: 11
Lipton HL, Bero LA, Bird JA, et al. Undermedication among geriatric outpatients: results of a randomized controlled trial. Ann Rev Gerontol Ger 1992; 12: 95–108
Man-Son-Hing M, Nichol G, Lau A, et al. Choosing antithrombotic therapy for elderly patients with atrial fibrillation who are at risk for falls. Arch Intern Med 1999; 159: 677–85
Man-Son-Hing M, Laupacis A. Anticoagulant-related bleeding in older persons with atrial fibrillation: physicians’ fears often unfounded. Arch Intern Med 2003; 163: 1580–6
Folstein MF, Folstein SE, McHugh PR. “Mini-Mental State”: a practical method for grading the cognitive state of patients for the clinician. J Psychiatr Res 1975; 12: 189–98
Charlson ME, Pompei P, Ales KL, et al. A new method of classifying prognostic comorbidity in longitudinal studies: development and validation. J Chronic Dis 1987; 40(5): 373–83
Samsa GP, Hanlon JT, Schmader KE, et al. A summated score for the Medication Appropriateness Index: development and assessment of clinimetric properties including content validity. J Clin Epidemiol 1994; 47: 891–6
Fick DM, Cooper JW, Wade WE, et al. Updating the Beers criteria for potentially inappropriate medication use in older adults: results of a US consensus panel of experts. Arch Intern Med 2003; 163: 2716–24
Gage BF, Waterman AD, Shannon W, et al. Validation of clinical classification schemes for predicting strokes: results from the National Registry of Atrial Fibrillation. JAMA 2001; 285: 2864–70
Wittkowsky AK. Effective anticoagulation therapy: defining the gap between clinical studies and clinical practice. Am J Manag Care 2004; 10(10 Suppl.): S297–306
Heeringa J, Van der Kuip DAM, Hofman A, et al. Prevalence, incidence and lifetime risk of atrial fibrillation: the Rotterdam Study. Eur Heart J 2006; 27: 949–53
Nieuwlaat R, Capucci A, Camm AJ, et al. Atrial fibrillation management: a prospective survey in ESC Member Countries. The Euro Heart Survey on Atrial Fibrillation. Eur Heart J 2005; 26: 2422–34
Gage BF, Boechler M, Doggette AL, et al. Adverse outcomes and predictors of underuse of antithrombotic therapy in Medicare beneficiaries with chronic atrial fibrillation. Stroke 2000; 31: 822–7
Pengo V, Legnani C, Noventa F, et al., on behalf of the ISCOAT study. Oral anticoagulant therapy in patients with nonrheumatic atrial fibrillation and risk of bleeding: a multicenter inception cohort study. Thromb Haemost 2001; 85: 418–22
DiMarco JP, Flaker G, Waldo AL, et al. Factors affecting bleeding risk during anticoagulant therapy in patients with atrial fibrillation: observations from the Atrial Fibrillation Follow-up Investigation of Rhythm Management (AFFIRM) Study. Am Heart J 2005; 149: 650–6
Fang MC, Chang Y, Hylek EM, et al. Advanced age, anticoagulation intensity, and risk for intracranial hemorrhage among patients taking warfarin for atrial fibrillation. Ann Intern Med 2004; 141: 745–52
Douketis JD, Arneklev K, Goldhaber SZ, et al. Comparison of bleeding in patients with nonvalvular atrial fibrillation treated with ximelagatran or warfarin. Arch Intern Med 2006; 166: 853–9
Hylek EM, Evans-Molina C, Shea C, et al. Major hemorrhage and tolerability of warfarin in the first year of therapy among elderly patients with atrial fibrillation. Circulation 2007; 115: 2689–96
Sudlow M, Thomson R, Thwaites B, et al. Prevalence of atrial fibrillation and eligibility for anticoagulants in the community. Lancet 1998; 352: 167–71
Johnson CE, Lim WK, Workman BS. People aged over 75 in atrial fibrillation on warfarin: the rate of major hemorrhage and stroke in more than 500 patient-years of follow-up. J Am Geriatr Soc 2005; 53: 655–9
Brophy MT, Snyder KR, Gaehde S, et al. Anticoagulant use for atrial fibrillation in the elderly. J Am Geriatr Soc 2004; 52: 1151–6
Nair A, Hazell W, Sutton T, et al. Antithrombotic therapy in atrial fibrillation: an assessment of compliance with guidelines. N Z Med J 2005; 118(1208): U1258
Hylek EM, D’Antonio J, Evans-Molina C, et al. Translating the results of randomized trials into clinical practice: the challenge of warfarin candidacy among hospitalized elderly patients with atrial fibrillation. Stroke 2006; 37: 1075–80
Partington SL, Abid S, Teo K, et al. Pre-admission stroke and atrial fibrillation: the appropriate use and barriers to oral anticoagulant therapy. Thromb Res 2007; 120: 663–9
Doucet J, Gréboval-Furstenfeld E, Tavildari A, et al. Which parameters differ in very old patients with chronic atrial fibrillation treated by anticoagulant or aspirin? Fundam Clin Pharmacol 2008; 22(5): 569–74
Currie CJ, Goodfellow J, McEwan P, et al. Evaluation of survival and ischaemic and thromboembolic event rates in patients with nonvalvular atrial fibrillation in the general population when treated and untreated with warfarin. Heart 2006; 92: 196–200
Mant J, Hobbs R, Fletcher K, et al. Warfarin versus aspirin for stroke prevention in an elderly community population with atrial fibrillation (the Birmingham Atrial Fibrillation Treatment of the Aged Study, BAFTA): a randomised controlled trial. Lancet 2007; 370: 493–503
Rash A, Downes T, Portner R, et al. Thromboprophylaxis in octogenarians with atrial fibrillation: a randomised controlled trial of warfarin versus aspirin in octogenarians with atrial fibrillation (WASPO). Age Ageing 2007; 36: 151–6
Van Deelen BAJ, van den Bemt PMLA, Egberts TCG, et al. Cognitive impairment as determinant for sub-optimal control of oral anticoagulation treatment in elderly patients with atrial fibrillation. Drugs Aging 2005; 22(4): 353–60
Reicke B, Masuhr F, Weih M. Reasons for underuse of oral anticoagulation in atrial fibrillation-associated stroke: prospective study of German stroke patients [in German]. Fortschr Neurol Psych 2008; 76(7): 391–5
Friberg L, Hammar N, Ringh M, et al. Stroke prophylaxis in atrial fibrillation: who gets it and who does not? Report from the Stockholm Cohort Study on Atrial Fibrillation. Eur Heart J 2006; 27: 1954–64
Go AS, Hylek EM, Chang Y, et al. Anticoagulation therapy for stroke prevention in atrial fibrillation: how well do randomized trial translate into clinical practice? JAMA 2003; 290: 2685–92
Acknowledgements
No sources of funding were used to assist in the preparation of this study. The authors have no conflicts of interest that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Tulner, L.R., Van Campen, J.P.C.M., Kuper, I.M.J.A. et al. Reasons for Undertreatment with Oral Anticoagulants in Frail Geriatric Outpatients with Atrial Fibrillation. Drugs Aging 27, 39–50 (2010). https://doi.org/10.2165/11319540-000000000-00000
Published:
Issue Date:
DOI: https://doi.org/10.2165/11319540-000000000-00000