Abstract
Attention deficit hyperactivity disorder (ADHD) is frequently comorbid with a variety of psychiatric disorders. These include oppositional defiant disorder and conduct disorder (CD), as well as affective, anxiety, and tic disorders. ADHD and ADHD with comorbid CD appear to be distinct subtypes; children with ADHD/CD are at higher risk of antisocial personality and substance abuse as adults. Stimulants are often effective treatments for aggressive or antisocial behavior in patients with ADHD, but mood stabilizers or atypical antipsychotics may be used to treat explosive aggressive outbursts. Response to stimulants is not affected by comorbid anxiety, but children with ADHD/anxiety disorder may show greater benefit from psychosocial interventions than those with ADHD alone. The degree of prevalence of major depressive disorder (MDD) and bipolar disorder among children with ADHD is controversial, but a subgroup of severely emotionally labile ADHD children who present serious management issues for the clinician clearly exists. Antidepressants may be used in conjunction with stimulants to treat MDD, while mood stabilizers and atypical antipsychotics are often required to treat manic symptoms or aggression. After resolution of the manic episode, stimulant treatment of the comorbid ADHD may be safely undertaken. Recent research suggests that stimulants can be safely used in children with comorbid ADHD and tic disorders, but the addition of anti-tic agents to stimulants is often necessary. Clinicians who work with patients with ADHD should be prepared to deal with a wide range of emotional and behavioral problems beyond the core symptoms of inattention and impulsivity/hyperactivity.



Similar content being viewed by others
References
Barkley RA. Attention-deficit hyperactivity disorder: a handbook for diagnosis and treatment. New York: The Guilford Press, 1998
Pliszka SR, Carlson CL, Swanson JM. ADHD with comorbid disorders: clinicial assessment and management. New York: Guilford Press, 1999
Arnold LE, Abikoff HB, Cantwell DP, et al. National Institute of Mental Health Collaborative Multimodal Treatment Study of Children with ADHD (the MTA): design challenges and choices. Arch Gen Psychiatry 1997; 54: 865–70
MTA Cooperative Group. 14 month randomized clinical trial of treatment strategies for children with attention deficit hyperactivity disorder. Arch Gen Psychiatry 1999; 56: 1073–86
Reeves JC, Werry JS, Elkind GS, et al. Attention deficit, conduct, oppositional, and anxiety disorders in children (II): clinical characteristics. J Am Acad Child Adolesc Psychiatry 1987; 26: 144–55
Szatmari P, Boyle M, Offord DR. ADDH and conduct disorder: degree of diagnostic overlap and differences among correlates. J Am Acad Child Adolesc Psychiatry 1989; 28: 865–72
Lahey BB, Piacentini JC, McBurnett K, et al. Psychopathology in the parents of children with conduct disorder and hyperactivity [published erratum appears in J Am Acad Child Adolesc Psychiatry 1988 Jul; 27 (4): 516]. J Am Acad Child Adolesc Psychiatry 1988; 27: 163–70
Biederman J, Faraone SV, Keenan K, et al. Further evidence for family-genetic risk factors in attention deficit hyperactivity disorder: patterns of comorbidity in probands and relatives psychiatrically and pediatrically referred samples. Arch Gen Psychiatry 1992; 49: 728–38
Biederman J, Munir K, Knee D. Conduct and oppositional disorder in clinically referred children with attention deficit disorder: a controlled family study. J Am Acad Child Adolesc Psychiatry 1987; 26: 724–7
Faraone SV, Biederman J, Keenan K, et al. Separation of DSM-III attention deficit disorder and conduct disorder: evidence from a family-genetic study of American child psychiatric patients. Psychol Med 1991; 21: 109–21
Mannuzza S, Klein RG, Bonagura N, et al. Hyperactive boys almost grown up (V): replication of psychiatric status. Arch Gen Psychiatry 1991; 48: 77–83
Fischer M, Barkley RA, Smallish L, et al. Young adult follow-up of hyperactive children: self-reported psychiatric disorders, comorbidity, and the role of childhood conduct problems and teen CD. J Abnorm Child Psychol 2002; 30: 463–75
Wilens TE, Biederman J, Spencer TJ. Attention deficit/hyperactivity disorder across the lifespan. Annu Rev Med 2002; 53: 113–31
Wilens TE, Biederman J, Mick E. Does ADHD affect the course of substance abuse: findings from a sample of adults with and without ADHD. Am J Addict 1998; 7: 156–63
Barkley RA, McMurray MB, Edelbrock CS, et al. The response of aggressive and nonaggressive ADHD children to two doses of methylphenidate. J Am Acad Child Adolesc Psychiatry 1989; 28: 873–81
Klorman R, Brumaghim JT, Salzman LF, et al. Comparative effects of methylphenidate on attention-deficit hyperactivity disorder with and without aggres-sive/noncompliant features. Psychopharmacol Bull 1989; 25: 109–13
Pliszka SR. Effect of anxiety on cognition, behavior, and stimulant response in ADHD. J Am Acad Child Adolesc Psychiatry 1989; 28: 882–7
Klein RG. Clinical efficacy of methylphenidate in children and adolescents. Encephale 1993; 19: 89–93
Gadow KD, Nolan EE, Sverd J, et al. Methylphenidate in aggressive-hyperactive boys (I): effects on peer aggression in public school settings. J Am Acad Child Adolesc Psychiatry 1990; 29: 710–8
Murphy DA, Pelham WE, Lang AR. Aggression in boys with attention deficit-hyperactivity disorder: methylphenidate effects on naturalistically observed aggression, response to provocation, and social information processing. J Abnorm Child Psychol 1992; 20: 451–66
Hinshaw SP, Heller T, McHale JP. Covert antisocial behavior in boys with attention-deficit hyperactivity disorder: external validation and effects of methylphenidate. J Consult Clin Psychol 1992; 60: 274–81
MTA Cooperative Group. Moderators and mediators of treatment response for children with attention deficit hyperactivity disorder: the MTA study. Arch Gen Psychiatry 1999; 56: 1088–96
Pelham WEJ, Wheeler T, Chronis A. Empirically supported psychosocial treatments for attention deficit hyperactivity disorder. J Clin Child Psychol 1998; 27: 190–205
Klein RG, Abikoff H, Klass E, et al. Clinical efficacy of methylphenidate in conduct disorder with and without attention deficit hyperactivity disorder. Arch Gen Psychiatry 1997; 54: 1073–80
Connor DF, Glatt SJ, Lopez ID, et al. Psychopharmacology and aggression (I): a meta-analysis of stimulant effects on overt/covert aggression-related behaviors in ADHD. J Am Acad Child Adolesc Psychiatry 2002; 41: 253–61
Campbell M, Adams PB, Small AM, et al. Lithium in hospitalized aggressive children with conduct disorder: a double blind and placebo controlled study. J Am Acad Child Adolesc Psychiatry 1995; 34: 445–53
Donovan SJ, Stewart JW, Nunes EV, et al. Divalproex treatment for youth with explosive temper and mood lability: a double-blind, placebo-controlled crossover design. Am J Psychiatry 2000; 157: 818–20
Greenhill LL, Rieder RO, Wender PH, et al. Lithium carbonate in the treatment of hyperactive children. Arch Gen Psychiatry 1973; 28: 636–40
Findling RL, McNamara NK, Branicky LA, et al. A double-blind pilot study of risperidone in the treatment of conduct disorder. J Am Acad Child Adolesc Psychiatry 2000; 39: 509–16
Snyder R, Turgay A, Aman M, et al. Effects of risperidone on conduct and disruptive behavior disorders in children with subaverage IQs. J Am Acad Child Adolesc Psychiatry 2002; 41: 1026–36
Findling RL, McNamara NK, Gracious BL. Antipsychotic agents: traditional and atypical. In: Martin A, Scahill L, Charney DS, et al., editors. Pediatric psychopharmacology: principles and practice. New York: Oxford University Press, 2003: 328–40
Dunbar F, Kusumakar V, Daneman D, et al. Growth and sexual maturation in children are unaffected by long term treatment with risperidone. 49th Meeting of the American Academy of Child and Adolescent Psychiatry; 2002 Oct 22–27; San Franciso
Findling RL, Kusumakar V, Daneman D, et al. Normalization of prolactin levels in children after long-term risperidone treatment. 49th Annual Meeting of the American Academy of Child and Adolescent Psychiatry; 2002 Oct 22–27; San Francisco
Bird HR, Gould MS, Staghezza BM. Patterns of diagnostic comorbidity in a community sample of children aged 9 through 16 years. J Am Acad Child Adolesc Psychiatry 1993; 32: 361–8
Cohen P, Cohen J, Kasen S, et al. An epidemiological study of disorders in late childhood and adolescence (I): age and gender specific pattern. J Child Psychol Psychiatry 1993; 34: 851–67
The MTA Cooperative Group. A 14 month randomized clinical trial of treatment strategies for attention deficit hyperactivity disorder: multimodal treatment study of children with ADHD. Arch Gen Psychiatry 1999; 56(12): 1073–86
Bird HR, Gould MS, Staghezza B. Aggregating data from multiple informants in child psychiatry epidemiological research. J Am Acad Child Adolesc Psychiatry 1992; 31: 78–85
Pliszka SR. Comorbidity of attention deficit hyperactivity disorder and overanxious disorder. J Am Acad Child Adolesc Psychiatry 1992; 31: 197–203
Biederman J, Faraone SV, Keenan K, et al. Familial association between attention deficit disorder and anxiety disorders. Am J Psychiatry 1991; 148: 251–6
Biederman J, Faraone SV, Chen WJ. Social adjustment inventory for children and adolescents: concurrent validity in ADHD children. J Am Acad Child Adolesc Psychiatry 1993; 32: 1059–64
Tannock R. Attention deficit disorders with anxiety disorders. In: Brown TE, editor. Attention-deficit disorders and comorbidities in children, adolescents and adults. New York: American Psychiatric Press, 2000: 125–75
Jensen PS, Shervette RE, Xenakis SN, et al. Anxiety and depressive disorders in attention deficit disorder with hyperactivity: new findings. Am J Psychiatry 1993; 150: 1203–9
Perrin S, Last CG. Relationship between ADHD and anxiety in boys: results from a family study. J Am Acad Child Adolesc Psychiatry 1996; 35: 988–96
Tannock R, Ickowicz A, Schachar R. Effects of comorbid anxiety disorder on stimulant response in children with ADHD. 38th Annual Meeting of the American Academy of Child and Adolescent Psychiatry; 1991 Oct 16–20; San Francisco
DuPaul GJ, Barkley RA, McMurray MB. Response of children with ADHD to methylphenidate: interaction with internalizing symptoms. J Am Acad Child Adolesc Psychiatry 1994; 33: 894–903
Buitelaar JK, Van der Gaag RJ, Swaab-Barneveld H, et al. Prediction of clinical response to methylphenidate in children with attention-deficit hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 1995; 34: 1025–32
Diamond IR, Tannock R, Schachar RJ. Response to methylphenidate in children with ADHD and comorbid anxiety. J Am Acad Child Adolesc Psychiatry 1999; 38: 402–9
March JS, Swanson JM, Arnold LE, et al. Anxiety as a predictor and outcome variable in the multimodal treatment study of children with ADHD (MTA). J Abnorm Child Psychol 2000; 28: 527–41
Cook EH, Wagner KD, March JS, et al. Long-term sertraline treatment of children and adolescents with obsessive-compulsive disorder. J Am Acad Child Adolesc Psychiatry 2001; 40: 1175–81
Geller DA, Hoog SL, Heiligenstein JH, et al. Fluoxetine treatment for obsessive-compulsive disorder in children and adolescents: a placebo-controlled clinical trial. J Am Acad Child Adolesc Psychiatry 2001; 40: 773–9
The Research Unit on Pediatric Psychopharmacology Anxiety Study Group. Fluvoxamine for the treatment of anxiety disorders in children and adolescents. N Engl J Med 2001; 344: 1279–85
Riddle MA, Reeve EA, Yaryura-Tobias JA, et al. Fluvoxamine for children and adolescents with obsessive-compulsive disorder: a randomized, controlled, multicenter trial. J Am Acad Child Adolesc Psychiatry 2001; 40: 222–9
March JS, Biederman J, Wolkow R, et al. Sertaline in children and adolescents with obsessive compulsive disorder: a multicenter, randomized, controlled trial. JAMA 1998; 280: 1752–6
Piacentini J, Shaffer D, Fisher P, et al. The diagnostic interview schedule for children-revised version (DISC-R) [III]: concurrent criterion validity. J Am Acad Child Adolesc Psychiatry 1993; 32: 658–65
Jensen P, Roper M, Fisher P, et al. Test-retest reliability of the diagnostic interview schedule for children (DISC 2.1). Arch Gen Psychiatry 1995; 52: 61–71
Schwab-Stone M, Fisher P, Piacentini J, et al. The diagnostic interview schedule for children-revised version (DISC-R) [II]: test-retest reliability. J Am Acad Child Adolesc Psychiatry 1993; 32: 651–7
Biederman J, Newcorn J, Sprich S. Comorbidity of attention deficit hyperactivity disorder with conduct, depressive, anxiety, and other disorders. Am J Psychiatry 1991; 148: 564–77
The MTA Cooperative Group. Moderators and mediators of treatment response for children with ADHD: The MTA study of children with ADHD. Arch Gen Psychiatry 1999; 56(12): 1088–96
Kovacs M, Akiskal HS, Gatsonis C, et al. Childhood onset dysthymic disorder: clinical features and prospective naturalistic outcome. Arch Gen Psychiatry 1994; 51: 365–74
Biederman J, Faraone S, Mick E, et al. Psychiatric comorbidity among referred juveniles with major depression: fact or artifact? J Am Acad Child Adolesc Psychiatry 1995; 34: 579–90
Kovacs M, Feinberg TL, Crouse-Novack M, et al. Depressive disorders in childhood (I): a longitudinal prospective study of characteristics and recovery. Arch Gen Psychiatry 1984; 41: 229–37
Kovacs M, Paulauskas S, Gatsonis C, et al. Depressive disorders in childhood (III): a longitudinal study of comorbidity with and risk for conduct disorders. J Affect Disord 1988; 15: 205–17
Biederman J, Mick E, Faraone SV. Depression in attention deficit hyperactivity disorder (ADHD) children: “true” depression or demoralization? J Affect Disord 1998; 47: 113–22
Daly JM, Wilens T. The use of tricyclics antidepressants in children and adolescents. Pediatr Clin North Am 1998; 45: 1123–35
Pliszka SR. Antidepressants in the treatment of child and adolescent psychopathology. J Clin Child Psychol 1991; 20: 313–20
Emslie GJ, Heiligenstein JH, Wagner KD, et al. Fluoxetine for acute treatment of depression in children and adolescents: a placebo-controlled, randomized clinical trial. J Am Acad Child Adolesc Psychiatry 2002; 41: 1205–15
Wagner KD, Ambrosini P, Rynn M, et al. Efficacy of sertraline in the treatment of children and adolescents with major depressive disorder: two randomized controlled trials. JAMA 2003; 290(8): 1033–41
Emslie GJ, Mayes TL. Mood disorders in children and adolescents: psychopharmacological treatment. Biol Psychiatry 2001; 49: 1082–90
Hughes CL, Emslie GJ, Crismon ML, et al. The Texas children’s medication algorithm project: report of the Texas consensus conference panel on medication treatment of childhood major depressive disorder. J Am Acad Child Adolesc Psychiatry 1999; 38(11): 1442–54
Gammon GD, Brown TE. Fluoxetine and methylphenidate in combination for treatment of attention deficit and comorbid depressive disorder. J Child Adolesc Psychopharmacol 1993; 3: 1–10
Keller MB, Ryan ND, Strober M, et al. Efficacy of paroxetine in the treatment of adolescent major depression: a randomized, controlled trial. J Am Acad Child Adolesc Psychiatry 2001; 40: 762–72
Daviss WB, Bentivoglio P, Racusin R, et al. Bupropion sustained release in adolescents with comorbid attention-deficit/hyperactivity disorder and depression. J Am Acad Child Adolesc Psychiatry 2001; 40: 307–14
Michelson D, Allen AJ, Busner J, et al. Once-daily atomoxetine treatment for children and adolescents with attention deficit hyperactivity disorder: a randomized, placebo-controlled study. Am J Psychiatry 2002; 159: 1896–901
Michelson D, Faries D, Wernicke J, et al. Atomoxetine in the treatment of children and adolescents with attention-deficit/hyperactivity disorder: a randomized, placebo-controlled, dose-response study. Pediatrics 2001; 108: 1–9
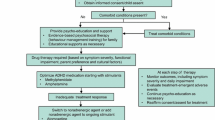
Pliszka SR, Greenhill LL, Crismon ML, et al. The Texas children’s medication algorithm project: report of the Texas consensus conference panel on medication treatment of childhood attention deficit/hyperactivity disorder (part I). J Am Acad Child Adolesc Psychiatry 2000; 39: 908–19
Anderson JC, Williams S, McGee R, et al. DSM-III disorders in preadolescent children: prevalence in a large community sample. Arch Gen Psychiatry 1987; 44: 69–76
August GJ, Realmuto GM, MacDonald AW, et al. Prevalence of ADHD and comorbid disorders among elementary school children screened for disruptive behavior. J Abnorm Child Psychol 1996; 24: 571–95
Costello EJ, Angold A, Burns BJ, et al. The Great Smokey Mountain Study of youth: goals, designs, methods, and the prevalence of DSM-III-R disorders. Arch Gen Psychiatry 1996; 53: 1129–36
Carlson GA. Classification of bipolar disorders in childhood. Psychiatr Dev 1984; 2: 273–85
Thompson LL, Riggs PD, Mikulich SK, et al. Contribution of ADHD symptoms to substance problems and delinquency in conduct-disordered adolescents. J Abnorm Child Psychol 1996; 24: 325–47
Wozniak J, Biederman J, Kiely K, et al. Mania-like symptoms suggestive of childhood onset bipolar disorder in clinically referred children. J Am Acad Child Adolesc Psychiatry 1995; 34: 867–76
Biederman J, Faraone SV, Mick E, et al. Attention deficit hyperactivity disorder and juvenile mania: an overlooked comorbidity? J Am Acad Child Adolesc Psychiatry 1996; 35: 997–1008
Wozniak J, Biederman J, Mundy E, et al. A pilot family study of childhood-onset mania. J Am Acad Child Adolesc Psychiatry 1995; 34: 1577–83
Geller B, Warner K, Williams M, et al. Prepubertal and young adolescent bipolarity versus ADHD: assessment and validity using the WASH-U-KSADS, CBCL and TRF. J Affect Disord 1998; 51: 93–100
Geller B, Williams M, Zimerman B, et al. Prepubertal and early adolescent bipolarity differentiate from ADHD by manic symptoms, grandiose delusion, ultra-rapid or ultradian cycling. J Affect Disord 1998; 51: 81–91
Klein RG, Pine DS, Klein DF. Resolved: mania is mistaken for ADHD in prepubertal children, negative. J Am Acad Child Adolesc Psychiatry 1998; 37: 1093–6
Gittelman R, Mannuzza S, Shenker R, et al. Hyperactive boys almost grown up (I): psychiatric status. Arch Gen Psychiatry 1985; 42: 937–47
Weiss G, Hechtman L, Trokenberg L. Hyperactive children grown up: empirical findings and theoretical considerations. New York: Guildford Press, 1986
Biederman J. Resolved: mania is mistaken for ADHD in prepubertal children, affirmative. J Am Acad Child Adolesc Psychiatry 1998; 37: 1091–3
Akiskal HS. Mood disorders: introduction and overview. In: Sadock BJ, Sadock VA, editors. Comprehensive textbook of psychiatry. 7th ed. Philadelphia (PA): Lippincott Williams & Wilkins, 2000: 1284–97
Geller B, Cooper TB, Sun K, et al. Double-blind and placebo-controlled study of lithium for adolescent bipolar disorders with secondary substance dependency. J Am Acad Child Adolesc Psychiatry 1998; 37: 171–8
Bowden CL, Brugger AM, Swann AC, et al. Efficacy of divalproex vs lithium and placebo in the treatment of mania. JAMA 1994; 271: 918–24
Wagner KD, Weller EB, Carlson GA, et al. An open-label trial of divalproex in children and adolescents with bipolar disorder. J Am Acad Child Adolesc Psychiatry 2002; 41: 1224–30
Del Bello MP. Olanzapine treatment for adolescent bipolar disorder. 49th Meeting of the American Academy of Child and Adolescent Psychiatry; 2002 Oct 22–27; San Francisco
Scheffer RE. Combination pharmacotherapy in pediatric bipolars-treating comorbid ADHD. 49th Annual Meeting of the American Academy of Child and Adolescent Psychiatry; 2002 Oct 22–27; San Francisco
Gadow KD, Sverd J, Sprafkin J, et al. Long-term methylphenidate therapy in children with comorbid attention-deficit hyperactivity disorder and chronic multiple tic disorder. Arch Gen Psychiatry 1999; 56: 330–6
Gadow KD, Sverd J, Sprafkin J, et al. Efficacy of methylphenidate for attention-deficit hyperactivity disorder in children with tic disorder. Arch Gen Psychiatry 1995; 52: 444–55
Gadow KD, Nolan E, Sprafkin J, et al. School observations of children with attention-deficit hyperactivity disorder and comorbid tic disorder: effects of methylphenidate treatment. J Dev Behav Pediatr 1995; 16: 167–76
Nolan EE, Gadow KD, Sprafkin J. Stimulant medication withdrawal during longterm therapy in children with comorbid attention-deficit hyperactivity disorder and chronic multiple tic disorder. Pediatrics 1999; 103: 730–7
Law SF, Schachar RJ. Do typical clinical doses of methylphenidate cause tics in children treated for attention-deficit hyperactivity disorder? J Am Acad Child Adolesc Psychiatry 1999; 38: 944–51
Spencer T, Biederman J, Coffey B, et al. A double-blind comparison of desipramine and placebo in children and adolescents with chronic tic disorder and comorbid attention-deficit/hyperactivity disorder. Arch Gen Psychiatry 2002; 59: 649–56
Connor DF, Fletcher KE, Swanson JM. A meta-analysis of clonidine for symptoms of attention-deficit hyperactivity disorder. J Am Acad Child Adolesc Psychiatry 1999; 38: 1551–9
Scahill L, Chappell PB, Kim YS, et al. A placebo-controlled study of guanfacine in the treatment of children with tic disorders and attention deficit hyperactivity disorder. Am J Psychiatry 2001; 158: 1067–74
Tourette’s Syndrome Study Group. Treatment of ADHD in children with tics: a randomized controlled trial. Neurology 2002; 58: 527–36
Acknowledgements
The authors have provided no information on sources of funding or on conflicts of interest directly relevant to the content of this review.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Pliszka, S.R. Psychiatric Comorbidities in Children with Attention Deficit Hyperactivity Disorder. Pediatr-Drugs 5, 741–750 (2003). https://doi.org/10.2165/00148581-200305110-00003
Published:
Issue Date:
DOI: https://doi.org/10.2165/00148581-200305110-00003