Abstract
Cutaneous allodynia, pain resulting from application of a non-noxious stimulus to normal skin, is a recently described symptom of migraine, with a potential role in directing optimal treatment for migraine attacks. Manifestations of cutaneous allodynia include discomfort when combing the hair, shaving, and wearing glasses, contact lenses, earrings or tight clothing.
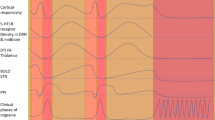
The exact mechanism by which a migraine attack is triggered is not known, but it has been theorised that, in some patients, once the attack has begun, central neurons can propagate information about the pain process without the need for further external stimuli. This process is termed central sensitisation. The trigeminal nerves, which innervate intracranial and extracranial tissues, account for head pain and other symptoms in migraine. The first-order neurons in the trigeminal ganglion receive input from the durai blood vessels, which is transmitted to second-order neurons in the trigeminal brain stem nuclear complex and is finally sent to the third-order neurons in the thalamus. Studies in humans and animals have shown that migraine pain progresses along this neural pathway, with throbbing head pain occurring early in the attack (sensitisation of first-order neurons), followed by central sensitisation and cutaneous allodynia within the referred pain area (second-order) and finally extracephalic allodynia (third-order). The data also indicate that once central sensitisation is established in the second-and third-order neurons, migraine treatment designed to prevent the initiation of central sensitisation can lessen the pain to some extent but cannot reverse it. Thus, treatment affecting the initiation of central sensitisation should be administered immediately after the onset of migraine pain to prevent intracranial hypersensitivity and the establishment of allodynia.
The serotonin 5-HT1B/1D agonist anti-migraine agents (the ‘triptans’) block meningeal nociceptor transmission at presynaptic sites in the dorsal horn. Studies have shown that triptan therapy can abort pain prior to the development of central sensitisation, but not after allodynia has been established. Therefore, in the subset of patients who report symptoms of cutaneous allodynia with migraine attacks, early initiation of triptan therapy is currently the best intervention to achieve rapid, complete and sustained pain relief.
Similar content being viewed by others
References
Lipton RB, Stewart WF, Diamond S, et al. Prevalence and burden of migraine in the United States: data from the American Migraine Study II. Headache 2001; 41: 646–57
Mathew NT. Pathophysiology, epidemiology, and impact of migraine. Clin Cornerstone 2001; 4: 1–17
Graham JR, Wolff HG. Mechanisms of migraine headache and action of ergotamine tartrate. Arch Neurol Psychiatry 1938; 39: 737–63
Martin VT, Behbehani MM. Toward a rational understanding of migraine trigger factors. Med Clin North Am 2001; 85(4): 911–41
Burstein R. Deconstructing migraine headache into peripheral and central sensitization. Pain 2001; 89: 107–10
Burstein R, Yarnitsky D, Goor-Aryeh I, et al. An association between migraine and cutaneous allodynia. Ann Neurol 2000; 47: 614–24
Goadsby PJ, Lipton RB, Ferrari MD. Migraine: current understanding and treatment. N Engl J Med 2002; 346: 257–70
Welch KMA. Contemporary concepts of migraine pathogenesis. Neurology 2003; 6Suppl. 4: S2–8
Weiller C, May A, Limmroth V, et al. Brain stem activation in spontaneous human migraine attacks. Nat Med 1995; 1: 658–60
Leao AAP. Spreading depression of activity in the cerebral cortex. J Neurophysiol 1944; 7: 359–90
Olesen J, Larsen B, Lauritzen M. Focal hyperemia followed by spreading oligemia and impaired activation of rCBF in classic migraine. Ann Neurol 1981; 9: 344–52
Bolay H, Reuter U, Dunn AK, et al. Intrinsic brain activity triggers trigeminal meningeal afferents in a migraine model. Nat Med 2002; 8: 136–47
Strassman AM, Raymond SA, Burstein R. Sensitization of meningeal sensory neurons and the origin of headaches. Nature 1996; 384: 560–4
Burstein R, Yamamura H, Malick A, et al. Chemical stimulation of the intracranial dura induces enhanced responses to facial stimulation in brain stem trigeminal neurons. J Neurophysiol 1998; 79: 964–82
Burstein R, Woolf CJ. The headaches. 2nd ed. Central sensitization and headache. Philadelphia (PA): Lippincott Williams & Wilkins, 2000
Silberstein SD. Neurotoxins in the neurobiology of pain. Headache 2003; 43: S2–8
Burstein R, Cutrer MF, Yarnitsky D. The development of cutaneous allodynia during a migraine attack: clinical evidence for the sequential recruitment of spinal and supraspinal nociceptive neurons in migraine. Brain 2000; 123: 1703–9
Levy D, Jakuabowski M, Burnstein R. Differential effects of sumatriptan on peripheral and central trigeminovascular neurons reveal site of action critical for terminating migraine [abstract]. Cephalalgia 2003; 23: 577
Longmore J, Shaw D, Smith D, et al. Differential distribution of 5HT1D- and 5HT1B-immunoreactivity within the human trigemino-cerebrovascular system: implications for the discovery of new antimigraine drugs. Cephalalgia 1997; 17: 833–42
Pascual J, del Arco C, Romon T, et al. Autoradiographic distribution of [H3]sumatriptan-binding sites in post-mortem human brain. Cephalalgia 1996; 16: 317–22
Burstein R, Jakubowski M. Analgesic triptan action in an animal model of intracranial pain: a race against the development of central sensitization. Ann Neurol 2004; 55(1): 25–36
Burstein R, Collins B, Jakubowski M. Defeating migraine pain with triptans: a race against the development of cutaneous allodynia. Ann Neurol 2004; 55(1): 19–26
Landy SH, McGinnis JE, McDonald SA. Clinical indicators of cutaneous allodynia in patients who treated early with 100mg sumatriptan tablets [abstract S32.006]. 55th Annual Scientific Meeting of the American Academy of Neurology; 2003 Mar 29–Apr 5; Honolulu, Hawaii
Acknowledgements
The authors have provided no information on sources of funding or on conflicts of interest directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Landy, S., Rice, K. & Lobo, B. Central Sensitisation and Cutaneous Allodynia in Migraine. CNS Drugs 18, 337–342 (2004). https://doi.org/10.2165/00023210-200418060-00001
Published:
Issue Date:
DOI: https://doi.org/10.2165/00023210-200418060-00001