Abstract
Background: There are few empirical studies on the valuation of health profiles that describe the short-term fluctuations of chronic diseases.
Objective: This study aimed to value chronic obstructive pulmonary disease (COPD) health profiles, which describe the health of these patients over the course of 1 year from a societal perspective.
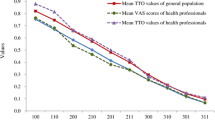
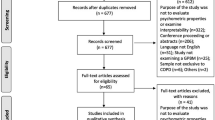
Methods: We developed 16 COPD health profiles. Each profile combined a description of the severity of COPD during the stable phase with a description of the exacerbation profile in terms of severity, frequency and duration. These profiles were valued by a representative sample of 239 Dutch adults using the visual analogue scale (VAS) and time trade-off (TTO) methods. Value functions were estimated using random effects regression analysis.
Results: Both VAS and TTO values consistently decreased as severity of the COPD profiles increased. Estimated TTO values ranged from 0.97 for mild COPD without exacerbations to 0.43 for very severe COPD with one non-serious and one serious exacerbation per year. The estimated decrements in TTO values ranged from 0.010 for having one non-serious exacerbation to 0.088 for having one non-serious plus one serious exacerbation per year.
Conclusions: The value function may be an alternative way to model the joint impact of COPD severity and exacerbations on utility values in health economic modelling studies.





Similar content being viewed by others
References
Bleichrodt H, Pinto J. Conceptual foundations for health utility measurement. In: Jones A, editor. The Elgar Companion to Health Economics. Cheltenham: Edward Elgar Publishing Limited, 2006: 347–58
Johannesson M. The ranking properties of healthy-years equivalents and quality-adjusted life-years under certainty and uncertainty. Int J Technol Assess Health Care 1995; 11 (1): 40–8
Verschuuren M. In search of realistic QALYs for short-term pain: the standard QALY model versus holistic assessment of profiles. Chapter 2. In: Quality adjusted life years and trade off exercises: exploring methodology and validity. Ph.D thesis. Utrecht: Utrecht University, Medical Faculty, 2006 [online]. Available from URL: http://igitur-archive.library.uu.nl/dissertations/2006-0516-200032/title.pdf [Accessed 2007 Apr 15]
Mehrez A, Gafni A. Quality-adjusted life years, utility theory, and healthy-years equivalents. Med Decis Making 1989; 9 (2): 142–9
Johannesson M, Pliskin JS, Weinstein MC. Are healthy-years equivalents an improvement over quality-adjusted life years? Med Decis Making 1993; 13 (4): 281–6
Tsuchiya A, Dolan P. The QALY model and individual preferences for health states and health profiles over time: a systematic review of the literature. Med Decis Making 2005; 25 (4): 460–7
Bonsel G, Janssen M, Birnie E. Mild Diseases & Ailments Study (MIDAS). Ziektelastbepaling van 27 vermoedelijk ‘lichte’ ziekten ten behoeve van rationele beperking van het geneesmiddelenpakket: samenvatting. Amsterdam: Amsterdam Medical Centre, Department of Social Medicine, 2003
Brazier J, Dolan P, Karampela K, et al. Does the whole equal the sum of the parts? Patient-assigned utility scores for IBS-related health states and profiles. Health Econ 2006; 15 (6): 543–51
Celli BR, MacNee W. Standards for the diagnosis and treatment of patients with COPD: a summary of the ATS/ERS position paper. Eur Respir J 2004; 23 (6): 932–46
GOLD. Global Initiative for Chronic Obstructive Lung Disease. Global strategy for diagnosis, management, and prevention of COPD. Bethesda (MD): National Institutes of Health, National Heart, Lung and Blood Institute, 2005 [online]. Available from URL: http://www.goldcopd.com [Accessed 2006 Jul 6]
Pauwels R, Calverley P, Buist AS, et al. COPD exacerbations: the importance of a standard definition. Respir Med 2004; 98 (2): 99–107
Burge S, Wedzicha JA. COPD exacerbations: definitions and classifications. Eur Respir J 2003; 41 Suppl.: 46–53s
Seemungal TA, Donaldson GC, Paul EA, et al. Effect of exacerbation on quality of life in patients with chronic obstructive pulmonary disease. Am J Respir Crit Care Med 1998; 157 (5 Pt 1): 1418–22
Aaron SD, Vandemheen KL, Clinch JJ, et al. Measurement of short-term changes in dyspnea and disease-specific quality of life following an acute COPD exacerbation. Chest 2002; 121 (3): 688–96
Ruchlin HS, Dasbach EJ. An economic overview of chronic obstructive pulmonary disease. Pharmacoeconomics 2001; 19 (6): 623–42
Rutten-van Mölken M, Lee TA. Economic modeling in chronic obstructive pulmonary disease. Proc Am Thorac Soc 2006; 3 (7): 630–4
Dolan P. Modeling valuations for the EuroQol health states. Med Care 1997; 35: 1095–108
Rutten-van Mölken MP, Oostenbrink JB, Tashkin DP, et al. Does quality of life of COPD patients as measured by the generic EuroQol five-dimension questionnaire differentiate between COPD severity stages? Chest 2006; 130 (4): 1117–28
O’Reilly JF, Williams AE, Rice L. Health status impairment and costs associated with COPD exacerbation managed in hospital. Int J Clin Pract 2007; 61 (7): 1112–20
Decramer M, Rutten-van Molken M, Dekhuijzen PN, et al. Effects of N-acetylcysteine on outcomes in chronic obstructive pulmonary disease (Bronchitis Randomized on NAC Cost-Utility Study, BRONCUS): a randomised placebo-controlled trial. Lancet 2005; 365 (9470): 1552–60
Vincken W, van Noord JA, Greefhorst AP, et al. Improved health outcomes in patients with COPD during 1 year’s treatment with tiotropium. Eur Respir J 2002; 19 (2): 209–16
Casaburi R, Mahler DA, Jones PW, et al. A long-term evaluation of once-daily inhaled tiotropium in chronic obstructive pulmonary disease. Eur Respir J 2002; 19 (2): 217–24
Streiner D, Norman G. Health measurement scales: a practical guide to their development and use. Oxford: Oxford University Press, 1989
Lamers LM, Stalmeier PF, Krabbe PF, et al. Inconsistencies in TTO and VAS values for EQ-5D health states. Med Decis Making 2006; 26 (2): 173–81
Efron B, Tibshirani R. Cross-validation and other estimates of prediction error. Chapter 17. An introduction to the bootstrap. New York: Chapman & Hall, 1993
Richardson J, Hall J, Salkeld G. The measurement of utility in multiphase health states. Int J Technol Assess Health Care 1996; 12 (1): 151–62
Kuppermann M, Shiboski S, Feeny D, et al. Can preference scores for discrete states be used to derive preference scores for an entire path of events? An application to prenatal diagnosis. Med Decis Making 1997; 17 (1): 42–55
Lipscomb J. Time preference for health in cost-effectiveness analysis. Med Care 1989; 27 (3 Suppl.): S233–53
MacKeigan LD, O’Brien BJ, Oh PI. Holistic versus composite preferences for lifetime treatment sequences for type 2 diabetes. Med Decis Making 1999; 19 (2): 113–21
Chapman GB. Preferences for improving and declining sequences of health outcomes. J Behav Dec Making 2000; 13: 203–18
Lamers LM, McDonnell J, Stalmeier PF, et al. The Dutch tariff: results and arguments for an effective design for national EQ-5D valuation studies. Health Econ 2006; 15 (10): 1121–32
Borg S, Ericsson A, Wedzicha JA, et al. A computer simulation model of the natural history and economic impact of chronic obstructive pulmonary disease. Value Health 2004; 7 (2): 153–67
Oostenbrink JB, Rutten-van Molken MP, Monz BU, et al. Probabilistic Markov model to assess the cost-effectiveness of bronchodilator therapy in COPD patients in different countries. Value Health 2005; 8 (1): 32–46
Hoogendoorn M, Feenstra T, Hoogenveen R, et al. A health policy model for COPD: effects of smoking cessation. Rotterdam: iMTA, Erasmus MC, 2003 Nov
Spencer M, Briggs AH, Grossman RF, et al. Development of an economic model to assess the cost effectiveness of treatment interventions for chronic obstructive pulmonary disease. Pharmacoeconomics 2005; 23 (6): 619–37
Sin DD, Golmohammadi K, Jacobs P. Cost-effectiveness of inhaled corticosteroids for chronic obstructive pulmonary disease according to disease severity. Am J Med 2004; 116 (5): 325–31
Pickard AS, Kohlmann T, Janssen MF, et al. Evaluating equivalency between response systems: application of the Rasch model to a 3-level and 5-level EQ-5D. Med Care 2007; 45 (9): 812–9
Miller G. The magic number seven, plus or minus two: some limits in our capacity for processing information. Psychol Rev 1956; 63 (2): 81–97
Greiner W, Weijnen T, Nieuwenhuizen M, et al. A European EQ-5D VAS valuation set. In: Brooks R, Rabin R, De Charro F, editors. The measurement and valuation of health status using EQ-5D: a European perspective. Dordrecht: Kluwer Academic, 2003: 143–65
Revicki DA, Leidy NK, Brennan-Diemer F, et al. Development and preliminary validation of the multiattribute Rhinitis Symptom Utility Index. Qual Life Res 1998; 7 (8): 693–702
Revicki DA, Leidy NK, Brennan-Diemer F, et al. Integrating patient preferences into health outcomes assessment: the multiattribute Asthma Symptom Utility Index. Chest 1998; 114 (4): 998–1007
Acknowledgements
Financial support for this study was provided by Boehringer Ingelheim International and Pfizer Global Pharmaceuticals. The funding agreement ensured the authors’ independence in designing the study, interpreting the data and writing and publishing the report. The authors would particularly like to thank Prof. Dr Gouke Bonsel for his advice in constructing the profiles and designing the study, and Mr Joost van der Burgh, Prof. Dr Miel Wouters and Dr Niels Chavannes for advice on the chronic obstructive pulmonary disease profile descriptions. We would also like to thank all the respondents who participated in this study. The authors have no conflicts of interest that are directly relevant to the content of this study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Rutten-van Mölken, M.P.M.H., Hoogendoorn, M. & Lamers, L.M. Holistic Preferences for 1-Year Health Profiles Describing Fluctuations in Health. Pharmacoeconomics 27, 465–477 (2009). https://doi.org/10.2165/00019053-200927060-00003
Published:
Issue Date:
DOI: https://doi.org/10.2165/00019053-200927060-00003