Abstract
Background
A wide variety of oral antiplatelet trials have been carried out, and a large number of cost-effectiveness estimates based on them have been published. Objective: To assess the cost effectiveness of oral antiplatelet treatments in the prevention of cardiovascular events.
Methods
A comprehensive literature search was carried out in PubMed and the Cochrane Library and the data reviewed. Cost-effectiveness or cost-utility studies of oral antiplatelets published since 2000 were selected. Cost-effectiveness analyses from the perspective of the UK NHS were then carried out using a Markov model with a 6-month cycle length and a lifetime horizon. Inputs from the CAPRIE, CHARISMA, (PCI)-CURE, CREDO, COMMIT, CLARITY, ESPS 2 and ESPRIT trials were included. All estimates of cost found (per event avoided, per QALY gained or per life-year gained) were included. Results were analysed in light of the National Institute for Health and Clinical Excellence (NICE) guidelines for the use of antiplatelets for the prevention of cardiovascular events and all estimates were updated to £ (year 2006 values) for easy comparison.
Results
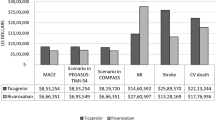
Of the initial 141 studies found, 21 were included in the initial review. The literature and the Markov model subsequently used suggest that aspirin (acetylsalicylic acid) dominates placebo for the secondary prevention of cardiovascular events, as it is effective, is also less costly and is as well tolerated as placebo. Additionally, in periods or patients with elevated risk, more intensive treatment with clopidogrel (alone or together with aspirin) is cost effective compared with aspirin alone for the secondary prevention of ischaemic events. For secondary stroke prevention, combination therapy with aspirin and dipyridamole has a favourable incremental cost-effectiveness ratio (ICER) when compared with aspirin alone and, based on an indirect comparison, also when compared with clopidogrel.
Conclusions
The cost-effectiveness estimates presented in this article support the NICE guidelines for the use of antiplatelets for the prevention of cardiovascular events. Based on these pharmacoeconomic data alone, aspirin should be prescribed for primary or secondary prevention among patients at high risk of cardiovascular events, dipyridamole for the secondary prevention of stroke (for a maximum of 5 years), and clopidogrel for the treatment of symptomatic cardiovascular disease or acute coronary syndrome (for a maximum of 2 years). The cost effectiveness of antiplatelets hinges on the patient’s initial risk, the risk reduction associated with treatment, and the price of the treatment. Evidence suggests that the cost effectiveness of antiplatelets can be optimized by individualising the treatment decision based on patient risk and expected risk reduction.








Similar content being viewed by others
References
National Institute for Health and Clinical Excellence. Clopidogrel and modified release dipyridamole in the prevention of occlusive vascular events [online]. Available from URL: http://guidance.nice.org.uk/ta90/guidance/pdf/english [Accessed 2005 Jan 5]
National Institute for Health and Clinical Excellence. Clopidogrel in the treatment of non-ST-segment-elevation acute coronary syndrome [online]. Available from URL: http://guidance, nice, org.uk/ta8 0/guidance/pdf/english [Accessed 2007 Jan 7]
National Institute for Health and Clinical Excellence. Guidance on the use of glycoprotein IIb/IIa inhibitors in the treatment of acute coronary syndromes [online]. Available from URL http: //guidance.nice.org.uk/ta47/guidance/pdf/english [Accessed 2002 Jan 9]
Antithrombotic Trialists’ Collaboration. Collaborative meta-analysis of randomised trials of antiplatelet therapy for prevention of death, myocardial infarction, and stroke in high risk patients. BMJ 2002; 324: 71–86
Sanmuganathan PS, Ghahramani P, Jackson PR, et al. Aspirin for primary prevention of coronary heart disease: safety and absolute benefit related to coronary risk derived from metaanalysis of randomised trials. Heart 2001 Mar; 85 (3): 265–271
Hayden M, Pignone M, Phillips C, et al. Aspirin for the primary prevention of cardiovascular events: a summary of the evidence for the U.S. Preventive Services Task Force. Ann Intern Med 2002 Jan 15; 136 (2): 161–172
Hankey GJ, Sudlow CL, Dunbabin DW. Thienopyridines or aspirin to prevent stroke and other serious vascular events in patients at high risk of vascular disease? A systematic review of the evidence from randomized trials. Stroke 2000 Jul; 31 (7): 1779–1784
CAPRIE Steering Committee. A randomised, blinded, trial of clopidogrel versus aspirin in patients at risk of ischaemic events (CAPRIE). Lancet 1996; 348: 1329–1339
The Clopidogrel in Unstable angina to prevent Recurrent Events trial investigators. Effects of clopidogrel in addition to aspirin in patients with acute coronary syndromes without st-segment elevation. N Engl J Med 2001; 345: 494–502
Mehta SR, Yusuf S, Peters R J, et al. Effects of pretreatment with clopidogrel and aspirin followed by long-term therapy in patients undergoing percutaneous coronary intervention: the PCI-CURE study. Lancet 2001 Aug 18; 358 (9281): 527–533
Steinhubl S, Berger P, Mann III J, et al. Early sustained dual oral antiplatelet therapy following percutaneous coronary intervention. JAMA 2002; 288: 2411–2420
Bhatt DL, Fox KA, Hacke W, et al. A global view of atherothrombosis: baseline characteristics in the Clopidogrel for High Atherothrombotic Risk and Ischemic Stabilization, Management, and Avoidance (CHARISMA) trial. Am Heart J 2005 Sep; 150 (3): 401
Sabatine MS, Cannon CP, Gibson CM, et al. Addition of clopidogrel to aspirin and fibrinolytic therapy for myocardial infarction with ST-segment elevation. N Engl J Med 2005 Mar 24; 352 (12): 1179–1189
Chen ZM, Jiang LX, Chen YP, et al. Addition of clopidogrel to aspirin in 45 852 patients with acute myocardial infarction: randomised placebo-controlled trial. Lancet 2005 Nov 5; 366 (9497): 1607–1621
Diener HC, Cunha L, Forbes C, et al. European Stroke Prevention Study: 2. Dipyridamole and acetylsalicylic acid in the secondary prevention of stroke. J Neurol Sci 1996 Nov; 143 (1–2): 1–13
Halkes PH, van Gijn J, Kappelle LJ, et al. Aspirin plus dipyridamole versus aspirin alone after cerebral ischaemia of arterial origin (ESPRIT): randomised controlled trial. Lancet 2006 May 20; 367 (9523): 1665–1673
Doggrell SA. CLARITY about the use of clopidogrel in patients with acute coronary syndromes and myocardial infarction. Expert Opin Pharmacother 2005 Aug; 6 (10): 1761–1764
Ho WK, Hankey GJ, Eikelboom JW. Prevention of coronary heart disease with aspirin and clopidogrel: efficacy, safety, costs and cost-effectiveness. Expert Opin Pharmacother 2004 Mar; 5 (3): 493–503
Beard SM, Gaffney L, Bamber L, et al. Economic modelling of antiplatelet therapy in the secondary prevention of stroke. J Med Econ 2004; 7: 117–134
Chambers M, Hutton J, Gladman J. Cost-effectiveness analysis of antiplatelet therapy in the prevention of recurrent stroke in the UK: aspirin, dipyridamole and aspirin-dipyridamole. Pharmacoeconomics 1999; 16 (5 pt 2): 577–593
Shah H, Gondek K. Aspirin plus extended-release dipyridamole or clopidogrel compared with aspirin monotherapy for the prevention of recurrent ischemic stroke: a cost-effectiveness analysis. Clin Ther 2000 Mar; 22 (3): 362–370
Sarasin FP, Gaspoz JM, Bounameaux H. Cost-effectiveness of new antiplatelet regimens used as secondary prevention of stroke or transient ischemic attack. Arch Intern Med 2000 Oct 9; 160 (18): 2773–2778
Lindgren P, Jonsson B, Yusuf S. Cost-effectiveness of clopidogrel in acute coronary syndromes in Sweden: a long-term model based on the CURE trial. J Intern Med 2004 May; 255 (5): 562–570
Schleinitz MD, Weiss JP, Owens DK. Clopidogrel versus aspirin for secondary prophylaxis of vascular events: a cost-effectiveness analysis. Am J Med 2004 Jun 15; 116 (12): 797–806
Main C, Palmer S, Griffin S, et al. Clopidogrel used in combination with aspirin compared with aspirin alone in the treatment of non-ST-segment-elevation acute coronary syndromes: a systematic review and economic evaluation. Health Technol Assess 2004 Oct; 8 (40): iii–xvi, 1
Cowper PA, Udayakumar K, Sketch JR MH, et al. Economic effects of prolonged clopidogrel therapy after percutaneous coronary intervention. J Am Coll Cardiol 2005 Feb 1; 45 (3): 369–376
Lindgren P, Stenestrand U, Malmberg K, et al. The long-term cost-effectiveness of clopidogrel plus aspirin in patients undergoing percutaneous coronary intervention in Sweden. Clin Ther 2005 Jan; 27 (1): 100–110
Weintraub WS, Mahoney EM, Lamy A, et al. Long-term cost-effectiveness of clopidogrel given for up to one year in patients with acute coronary syndromes without ST-segment elevation. J Am Coll Cardiol 2005 Mar 15; 45 (6): 838–845
Karnon J, Brennan A, Pandor A, et al. Modelling the long term cost effectiveness of clopidogrel for the secondary prevention of occlusive vascular events in the UK. Curr Med Res Opin 2005 Jan; 21 (1): 101–112
Karnon J, Bakhai A, Brennan A, et al. A cost-utility analysis of clopidogrel in patients with non-ST-segment-elevation acute coronary syndromes in the UK. Int J Cardiol 2006 May 24; 109 (3): 307–316
Matchar DB, Samsa GP, Liu S. Cost-effectiveness of anti-platelet agents in secondary stroke prevention: the limits of certainty. Value Health 2005 Sep; 8 (5): 572–580
Ringborg A, Lindgren P, Jonsson B. The cost-effectiveness of dual oral antiplatelet therapy following percutaneous coronary intervention: a Swedish analysis of the CREDO trial. Eur J Health Econ 2005 Dec; 6 (4): 354–362
Mahoney EM, Mehta S, Yuan Y, et al. Long-term cost-effectiveness of early and sustained clopidogrel therapy for up to 1 year in patients undergoing percutaneous coronary intervention after presenting with acute coronary syndromes without ST-segment elevation. Am Heart J 2006 Jan; 151 (1): 219–227
Lamotte M, Anne mans L, Evers T, et al. A multi-country economic evaluation of low-dose aspirin in the primary prevention of cardiovascular disease. Pharmacoeconomics 2006; 24 (2): 155–169
Pignone M, Earnshaw S, Tice J A, et al. Aspirin, statins, or both drugs for the primary prevention of coronary heart disease events in men: a cost-utility analysis. Ann Intern Med 2006 Mar 7; 14 (5): 326–336
Lamy A, Jonsson B, Weintraub WS, et al. The cost-effectiveness of the use of clopidogrel in acute coronary syndromes in five countries based upon the CURE study. Eur J Cardiovasc Prev Rehabil 2004 Dec; 11 (6): 460–465
Schleinitz MD, Heidenreich PA. A cost-effectiveness analysis of combination antiplatelet therapy for high-risk acute coronary syndromes: clopidogrel plus aspirin versus aspirin alone. Ann Intern Med 2005 Feb 15; 142 (4): 251–259
Durand-Zaleski I, Bertrand M. The value of clopidogrel versus aspirin in reducing atherothrorribotic events: the CAPRIE study. Pharmacoeconomics 2004; 22 Suppl. 4: 19–27
Beinart SC, KolmP, Veledar E, et al. Long-term cost effectiveness of early and sustained dual oral antiplatelet therapy with clopidogrel given for up to one year after percutaneous coronary intervention results: from the Clopidogrel for the Reduction of Events During Observation (CREDO) trial. J Am Coll Cardiol 2005 Sep 6; 46 (5): 761–769
Eidelman RS, Hebert PR, Weisman SM, et al. An update on aspirin in the primary prevention of cardiovascular disease. Arch Intern Med 2003 Sep 22; 163 (17): 2006–2010
ICATT. Koersconverter [online]. Available from URL: www.koersconverter.nl [Accessed 2006 Nov]
Heeg BMS, van Gestel A, van Hout BA, et al. Costs and effects of clopidogrel versus aspirin in high-risk acute coronary syndrome patients in Denmark [in Danish]. Ugeskrift for Lager 2006; 168: 2911–2915
Heeg B, Peters R, Botteman M, et al. Long-term clopidogrel therapy in PCI patients. Pharmacoeconomics 2007; 25 (9): 769–782
van Luijn JCF. Pharmacoeconomic report clopidogrel (Plavix). Amstelveen: Dutch Healthcare Insurance board (CVZ), 2004
The Dutch Institute for Healthcare Improvement (CBO). Multi disciplinary guideline cardiovascular risk management. Utrecht: The Dutch Institute for Healthcare Improvement (CBO), 2006
The Dutch Institute for Healthcare Improvement (CBO). Treatment and prevention of coronary heart disease by lowering plasma cholesterol levels. Utrecht: The Dutch Institute for Healthcare Improvement (CBO), 1998
Task Force Revised Guidelines Hypertension. Revised guidelines hypertension [in Dutch]. Utrecht: The Dutch Institute for Healthcare Improvement (CBO), 2000
Zeymer U, Gitt AK, Junger C, et al. Effect of clopidogrel on 1-year mortality in hospital survivors of acute ST-segment elevation myocardial infarction in clinical practice. Eur Heart J 2006 Nov; 27 (22): 2661–2666
Taneja AK, Collinson J, Flather MD, et al. Mortality following non-ST elevation acute coronary syndrome: 4 years follow-up of the PRAIS UK Registry (Prospective Registry of Acute Ischaemic Syndromes in the UK). Eur Heart J 2004 Nov; 25 (22): 2013–2018
Armstrong PW, Fu Y, Chang WC, et al. Acute coronary syndromes in the GUSTO-IIb trial: prognostic insights and impact of recurrent ischemia. The GUSTO-IIb Investigators. Circulation 1998 Nov 3; 98 (18): 1860–1868
Kleinbaum D, Klein M. Parametric survival models: survival analyses. 2nd ed. New York: Springer, 2005
Hollander D, Koudstraal P, Bots M, et al. Incidence, risk, and case fatality of first ever stroke in the elderly population: the Rotterdam study. J Neurol Neurosurg Psychiatry 2003; 74: 317–321
Anderson KM, Odell PM, Wilson P, et al. Cardiovascular disease risk profiles. Am Heart J 1991; 121: 293–298
Koek HL, de BA, Gast F, et al. Short- and long-term prognosis after acute myocardial infarction in men versus women. Am J Cardiol 2006 Oct 15; 98 (8): 993–999
WHO. Life table for WHO member states (UK) [online]. Available from URL: http://www.who.int/nha/country/gbr/en/ [Accessed 2007 Mar]
Caro J, Migliaccio-Walle K, for the CAPRA Study Group. Generalizing the results of clinical trials to actual practice: the example of clopidogrel therapy for the prevention of vascular events. Am J Med 1999; 107: 568–572
Clarke P, Gray A, Legood R, et al. The impact of diabetes-related complications on healthcare costs: results from the United Kingdom Prospective Diabetes Study (UKPDS study no. 65). Diabetic Med 2003; 20: 442–450
Palmer S, Sculpher M, Philips Z, et al. A cost-effectiveness model comparing alternative management strategies for the use of glycoprotein IIB/IIIA antagonists in non-ST-elevation acute coronary syndrome. NICE Appraisal report [online]. Available from URL: http://guidance.nice.org.uk/page.aspx?o=32030 [Accessed 2007 Mar]
Department of Health. NHS reference costs 2005-06. London: Department of Health, 2006 [online]. Available from URL: http://www.dh.gov.uk/en/publicationsandstatistics/publications/publicationspolicyandguidance/dh_062884 [Accessed 2006 Dec]
Robinson M, Palmer S, Sculpher M, et al. Cost-effectiveness of alternative strategies for the initial medical management of non-ST elevation acute coronary syndrome: systematic review and decision-analytical modelling. Health Technol Assess 2005 Jul; 9 (27): iii–xi, 1
British Medical Association and Royal Pharmaceutical Society of Great Britain. British national formulary. London: British Medical Association and Royal Pharmaceutical Society of Great Britain, 2006 [online]. Available from URL: http://www.bnf.org/bnf/bnf/current [Accessed 2006 Nov]
Eichler HG, Kong SX, Gerth WC, et al. Use of cost-effectiveness analysis in health-care resource allocation decision-making: how are cost effectiveness thresholds expected to emerge? Value Health 2004; 7: 518–528
Wiviott SD, de Lemos JA, Cannon CP, et al. A tale of two trials: a comparison of the post-acute coronary syndrome lipid-lowering trials A to Z and PROVE IT-TIMI 22. Circulation 2006 Mar 21; 113 (11): 1406–1414
Liebson PR. CARDS and A to Z. Prev Cardiol 2005; 8 (1): 59–62
de Lemos JA, Blazing MA, Wiviott SD, et al. Early intensive vs a delayed conservative simvastatin strategy in patients with acute coronary syndromes: phase Z of the A to Z trial. JAMA 2004 Sep 15; 292 (11): 1307–1316
Heart Protection Study Collaborative Group. MRC/BHF Heart Protection Study of cholesterol lowering with simvastatin in 20 536 high-risk individuals: a randomised placebo-controlled trial. Lancet 2002 Jul 6; 360 (9326): 7–22
Collins R, Armitage J, Parish S, et al. MRC/BHF Heart Protection Study of cholesterol-lowering with simvastatin in 5963 people with diabetes: a randomised placebo-controlled trial. Lancet 2003 Jun 14; 361 (9374): 2005–2016
Eriksson P. Long term clopidogrel therapy after percutaneous coronary intervention in PCI-CURE and CREDO: the “Emperor’s New Clothes” revisited. Eur Heart J 2004; 25: 720–722
Acknowledgements
The first two authors acknowledge each other as equal first co-authors.
No funding was received to assist in the preparation of this study. Pharmerit International has in the past provided health economic services concerning the reimbursement trajectory of clopidogrel in The Netherlands. The authors have no other conflicts of interest that are directly relevant to the contents of this study.
Author information
Authors and Affiliations
Corresponding author
Electronic supplementary material
Rights and permissions
About this article
Cite this article
Heeg, B., Damen, J. & Van Hout, B. Oral Antiplatelet Therapy in Secondary Prevention of Cardiovascular Events. Pharmacoeconomics 25, 1063–1082 (2007). https://doi.org/10.2165/00019053-200725120-00007
Published:
Issue Date:
DOI: https://doi.org/10.2165/00019053-200725120-00007