Abstract
Acute bacterial meningitis is still an important cause of morbidity and mortality in children worldwide. Recently, Haemophilus influenzae type b (Hib), once a common cause of meningitis, has virtually disappeared in developed nations, reflecting the overwhelming success of Hib vaccination. Unfortunately, Hib remains a significant pathogen in resource-poor countries. The introduction of the conjugated pneumococcal vaccine in 2000 may lead to similar future trends as witnessed with Hib. As the resistance of Streptococcus pneumoniae to penicillin and cephalosporins continues to evolve, vancomycin has become an important antibacterial in the treatment of bacterial meningitis. The unreliable penetration of this agent into cerebrospinal fluid is of concern, which is compounded by the controversial use of corticosteroids in paediatric meningitis. Some data suggest that in certain situations the addition of rifampicin (rifampin) to ceftriaxone may be a better choice. While dexamethasone is now considered the standard adjunctive therapy in the treatment of pneumococcal meningitis in adult patients, the benefit in children is not so clear and remains controversial; thus, there is no definitive paediatric recommendation. Several anti-inflammatory agents currently under investigation may be used in the future as adjunctive therapy for bacterial meningitis.
It is clear that the current concepts in the treatment of childhood bacterial eningitis are evolving, and other antibacterial options and possible alternatives such as carbapenems and fluoroquinolones should be considered. Fluid restriction because of the Syndrome of Inappropriate Antidiuretic Hormone Secretion is widely advocated and used. Yet, this practice was recently challenged. It seems that most patients with meningitis do not need fluid restriction. The overwhelming success of the conjugated Hib vaccine and the encouraging results of the new conjugated pneumococcal and meningococcal vaccines suggest that the ideal management of bacterial meningitis is prevention and vaccines development against the most common bacterial agents are the best solution.
Similar content being viewed by others
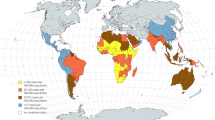
Acute bacterial meningitis remains an important cause of high morbidity and mortality in the paediatric population worldwide. In developed countries over the past 2 decades, two major changes have occurred in the epidemiology of bacterial meningitis; both have significantly altered the management and empirical therapy of this disease (mostly in developed countries). First, Haemophilus influenzae type b (Hib), which once accounted for 70% of bacterial meningitis cases in children <5 years of age,[1] has been virtually eradicated in those countries that introduced immunisation of infants with conjugate Hib vaccines. As a result, Streptococcus pneumoniae has become the most common pathogen beyond the neonatal period[2] and the median age of patients with bacterial meningitis has increased from 15 months to 25 years with a predominance of adults rather than children. Unfortunately, in many resource-poor countries, where the Hib vaccine is not available, invasive Hib diseases (including meningitis) are still common and an estimated 350 000–700 000 children die from this infection every year.[3] In addition, at least 1.2 million cases of meningococcal meningitis worldwide (with 10% mortality) occur each year (apart from epidemics that occur periodically in sub-Saharan Africa, the Middle East, India and China).
A second major epidemiological change is the emergence of penicillin and cephalosporin-resistant S. pneumoniae. In 1967, penicillin-resistant S. pneumoniae strains were first reported,[4] and multi-drug resistance is now a worldwide phenomenon.[5,6] As a result, a third-generation cephalosporin plus vancomycin has become the standard recommendation for empirical therapy for bacterial meningitis.[7] As cephalosporin-resistant strains are reported, the unreliable penetration of vancomycin into the CNS may become a major therapeutic issue.
During the era when Hib was a common cause of meningitis, the adjunctive use of dexamethasone was common practice when initiating therapy. Presently, the use of dexamethasone for meningitis caused by other bacteria is controversial rather than universally accepted. In a recent study of adult patients with meningitis, a significant decrease in mortality was associated with the concomitant use of dexamethasone.[8] Should these results be considered when caring for the paediatric patient with meningitis? As the aetiological agents of bacterial meningitis and antibacterial resistance patterns change, it is certainly important to discuss modifications in the management of paediatric patients with this disease.
1. Aetiological Agents
This review focuses on bacterial meningitis in the otherwise healthy child beyond the neonatal and early infant period (age ≥3 months). In developed countries, the likelihood of Hib meningitis in a child who has received at least two doses of Hib vaccine is exceedingly rare. As a result of routine Hib vaccination, the incidence of invasive Hib disease in the US has declined by at least 97%, from 41 cases per 100 000 (1987) to 1.3 cases per 100 000 (1997).[9] The decline in Hib disease has caused S. pneumoniae to become the most common aetiological agent of bacterial meningitis. In 1995, the US Centers for Disease Control and Prevention (CDC) performed a multistage surveillance study of bacterial meningitis and reported S. pneumoniae as the most commonly identified agent (47%), followed by Neisseria meningitidis (25%) and group B streptococci (12%).[10] Hib remains a common pathogen in resource-poor nations where Hib vaccination is not readily available.
Although S. pneumoniae is currently the most commonly isolated agent, its epidemiology continues to evolve as a result of the introduction of the conjugate pneumococcal vaccine in early 2000. In the US, widespread use of this vaccine has already led to a reduction in the incidence of paediatric invasive pneumococcal disease; the CDC reported a 59% decline in the rate of pneumococcal meningitis from 1998 to end of 2001.[11] The same results (66% reduction) were recently reported by Kaplan et al.[12]
The peak incidence of meningococcal disease occurs in the first year of life, and 35–40% of cases occur in children <5 years of age.[13,14] In The Netherlands, the case fatality rate during a meningococcal meningitis epidemic in 1989–90 was 4.6%.[15] Recently, an increase in clusters of meningococcal disease due to N. meningitidis serogroup C was reported from various developed countries (e.g. Canada, the US, England, Spain). The use of conjugate meningococcal C vaccine has been effective in terminating the spread of this infection. For example, an overall reduction of 86.7% in the incidence of serogroup C infection occurred in the UK from 1999 to 2001, with a concomitant decrease in deaths, from 67 in 1999 to 5 in 2001.[16] In sub-Saharan Africa, N. meningitidis remains the most frequently isolated organism, accounting for up to 61% of cases.[17] Cyclical epidemics of meningococcal meningitis, which occur every 5–10 years during the dry months, may result in >300 000 cases (with 10% mortality).[18] Serogroup A has been the most common cause of epidemic and endemic meningococcal disease; however, a shift to serogroup W135 has occurred recently during the Hajj (pilgrimage) season.
2. Principles of Antibacterial Therapy
The cerebrospinal fluid (CSF) has poor ability to respond to bacterial infection. It is a fluid with inadequate immunoglobulin and complement activity, resulting in impaired ability to opsonise and phagocytise infecting organisms. Thus, sterilisation of the CSF, or bacteriological cure, depends on the antibacterial agent(s) used. Several factors are important for the rapid CSF sterilisation which is required for optimal therapy. For β-lactam therapy, there is a significant correlation between increasing drug concentration in the CSF and increasing bactericidal rates. Maximal bactericidal activity occurs when the CSF concentration is 10–30 times higher than the in vitro broth minimal bactericidal concentration (MBC).[19] The aminoglycosides and fluoroquinolones also exhibit an excellent correlation between the CSF concentrations and the bactericidal activity (i.e. the higher the concentration, the better the bacterial killing).[20–22] The maximum bactericidal activity of vancomycin occurred when the CSF concentrations were five to ten times higher than the MBC.[23] In contrast, increasing the CSF concentrations of rifampicin (rifampin) were not associated with increased killing rate.[24]
The CSF penetration of an antibacterial depends on the integrity of the blood-brain barrier (BBB) and the physical and chemical characteristics of the drug. For example, β-lactam antibacterials penetrate poorly in the setting of a normal BBB (approximately 0.5–2.0% of peak serum concentrations). However, in the setting of meningitis, β-lactam penetration across the BBB is significantly enhanced (up to 55% of the peak serum concentration). As demonstrated in the rat meningitis model, the improved penetration results from separation of the intercellular tight junctions and increased vesicular transport.[25] To ensure optimal penetration of the antibacterial into the CNS, maximal parenteral dose administration should be maintained for the entire treatment course; as meningeal inflammation decreases with therapy, antibacterial penetration across the BBB diminishes (e.g. CSF penicillin concentrations were reduced by almost 50% on day 5 of therapy compared with day 1[26]). Certain characteristics of the antibacterial agent itself may also alter its ability to penetrate the BBB. Factors that improve the ability of a drug to cross the BBB include a low molecular weight, simple chemical structure, high lipid solubility, low degree of protein binding and low degree of ionisation.[27] Of note, vancomycin can penetrate the CSF only if the BBB has been damaged significantly, which may explain the wide range of CSF concentrations during meningitis.[28]
In the setting of purulent meningitis, the antibacterials used have varying bactericidal effects. The protein-rich environment of purulent meningitis may decrease the activity of β-lactams. These antibacterials are highly protein-bound, but it is the free (unbound) drug that is needed for a bactericidal effect. The decreased pH in CSF during purulent meningitis may alter the activity of certain classes of antibacterials, such as the aminoglycosides. In addition, the elimination of some drugs from the CSF (e.g. penicillin) is slowed by the inflammatory response, allowing higher concentrations in the CSF.[29]
An understanding of the pharmacodynamic characteristics of a therapeutic agent in the CSF is also important when choosing appropriate dose administration regimens. Antibacterial activity can display two patterns of killing, either concentration- or time-dependent. In concentration-dependent killing, the drug displays bacterial killing over a wide range of antibacterial concentrations that exceed the minimum inhibitory concentration (MIC). There is a direct correlation between the achieved drug concentrations and the rate of bacterial killing. This pattern is seen with the aminoglycosides and fluoroquinolones, where increasing CSF concentrations resulted in higher rates of bacterial killing which allows for less frequent dose administration.[30]
The second pattern of killing is time-dependent killing. For these antibacterials, the most important factor for bactericidal activity is the length of time that the CSF concentration is higher than the MIC and/or the MBC. The time above the MBC correlates better with efficacy. With these agents (e.g. vancomycin and the β-lactams), bactericidal activity is reached by giving the drug at frequent intervals, in order to keep the concentration of the drug above the MIC for the longest time period possible.[30]
It is generally believed that even a short delay in initiation of antibacterial therapy for bacterial meningitis will have a deleterious effect on the outcome. Yet, most studies that examined the impact of the timing of antibacterial administration upon clinical outcome could not find a correlation between the duration of symptoms before antibacterials were initiated and the clinical outcome. Aronin et al.[31] studied a prognostic model for 269 adults with bacterial meningitis and showed that the impact on clinical outcome varied with the initial severity of illness at presentation and not with a specific time delay in the administration of the first dose of antibacterial.[31] Hypotension, altered mental status and seizures at presentation were associated with poorer outcome. Thus, a delay in treatment (even up to 72–96 hours), when a patient has presented with a nonspecific illness, will not alter the risk of sequelae.[32] In patients with overt symptoms of meningitis, a delay in starting therapy may increase the risk of sequelae, depending on the combinations of presenting symptoms mentioned earlier.
3. Antibacterial Agents
Empirical therapy of a child with suspected bacterial meningitis is based on the most likely pathogens for the patient’s age and susceptibility patterns in that geographical location. Once the organism is identified and its antibacterial susceptibilities determined, therapy should be modified as needed.
3.1 Streptococcus pneumoniae
The recommendations for antibacterial therapy for pneumococcal meningitis are based on current in vitro susceptibility patterns (table I). Currently, in some geographical areas of the US >40% of pneumococcal isolates from sterile body sites (not exclusively CSF) are nonsusceptible to benzylpenicillin (penicillin G) and up to 50% of these isolates are highly resistant. Approximately half of these penicillin-nonsusceptible strains are also nonsusceptible to both ceftriaxone and cefotaxime.[33] Although CSF isolates are somewhat less resistant to these antibacterials, the percentage is still high. For example, in a recent multicentre surveillance of only CSF isolates, approximately 20% were penicillin nonsusceptible and 7% were ceftriaxone nonsusceptible.[34] Resistance to penicillin and third-generation cephalosporins has also been reported worldwide. Thus, the American Academy of Pediatrics (AAP) currently recommends empirical combination therapy with vancomycin and cefotaxime or ceftriaxone.[33] It was suggested that this combination is synergistic in experimental pneumococcal meningitis[35] and in children (table II).[36]
National Committee for Clinical Laboratory Standards minimal inhibitory concentration breakpoints for antibacterial agents used to treat Streptococcus pneumoniae infections[37]
At present, pneumococcal resistance to vancomycin has not been reported; however, treatment failure with vancomycin (both as monotherapy and combination therapy) has been reported. Monotherapy with vancomycin is not recommended, as CSF penetration is inconsistent and bactericidal concentrations may not be sustained, especially in the setting of less inflamed meninges. In a study of 11 adults with pneumococcal meningitis, four patients had clinical failure with vancomycin monotherapy.[38] In two of these patients, CSF drug concentrations were undetectable at 48 hours after onset of therapy. Concomitant use of dexamethasone and variability in serum concentrations were thought to be a possible contributors to these failures. Although the combination of vancomycin with a third-generation cephalosporin seems to be effective, careful monitoring of patients receiving this combination is needed. While limited data suggest that CSF vancomycin concentrations exceed the MBC90 for S. pneumoniae (2- to 6-fold),[36] these concentrations are not consistently 5- to 10-fold higher, which is the concentration needed for maximal bactericidal killing. There is evidence that delayed sterilisation of the CSF can contribute to a worse outcome.[39] The wide variation in vancomycin penetration into the CSF may result in lower drug concentrations and slower sterilisation that will affect the clinical outcome. This effect may be exaggerated when vancomycin is given with dexamethasone.[40] It is possible that with the increase in S. pneumoniae resistance to third-generation cephalosporins, the ‘protective effect’ of these agents against vancomycin failures as a result of poor CSF penetration will be diminished and treatment failures with the combination will occur.
While pneumococcal resistance to vancomycin has not been reported, the development of drug tolerance (i.e. the organism is unable to replicate but is not killed) was recently observed. In 1999, a cephalosporin- and vancomycin-tolerant strain of S. pneumoniae was isolated from the CSF of a patient whose symptoms recurred while receiving therapy with vancomycin and a third-generation cephalosporin.[41] The isolate was also tolerant to aminoglycosides and fluoroquinolones. The sensitivity to rifampicin was not reported. Thus, if a patient with bacterial meningitis demonstrates clinical failure, a poor response to therapy or disease recurrence once therapy is discontinued, clinicians should have a high index of suspicion for vancomycin failure due to poor penetration or to a tolerant strain. It should be noted that no additional cephalosporin- and vancomycin-tolerant pneumococcus strain has been isolated to date.
The addition of rifampicin to ceftriaxone has been demonstrated to result in significantly enhanced CSF bactericidal activity compared with that of ceftriaxone alone against cephalosporin-resistant strains.[36] In addition, this combination reduced mortality by almost 50% in the animal meningitis model,[42] probably by decreasing the release of teichoic and lipoteichoic acids from pneumococci, which modulated the magnitude of the inflammatory response.[43] Other data show that the CSF penetration of rifampicin is excellent and is unaffected by the concomitant use of dexamethasone. For these reasons, rifampicin instead of vancomycin as adjunct to a third-generation cephalosporin is recommended by some investigators, especially if dexamethasone is used (table II). Rifampicin should never be used alone for treatment, as resistance will develop rapidly. In addition, although limited data suggest that rifampicin maybe synergistic with ceftriaxone against cephalosporin-resistant S. pneumoniae, caution should be taken in using this combination if the isolated strain is highly resistant to cephalosporins. Additional trials are needed to investigate whether the beneficial effect of rifampicin shown in the animal model of pneumococcal meningitis makes it the preferred drug over vancomycin. Many other features of rifampicin suggest that it may be a better choice.
As penicillin and cephalosporin resistance continues to emerge, other antibacterials have been evaluated as alternative options, including the carbapenems. Imipenem/cilastatin is associated with a high incidence of drug-related seizure activity; thus, its usefulness is limited in the treatment of CNS infections. However, meropenem is considered to be an alternative therapeutic agent for bacterial meningitis in children ≥3 months of age. In a study comparing the efficacy and safety of meropenem to that of cefotaxime, no significant difference in clinical outcome was found between the two treatment groups. Clinical cure with or without sequelae was reached in 97% and 96% of the meropenem- and cefotaxime-treated patients, respectively.[44] At the 5- to 7-week follow-up, 54% of the meropenem- and 58% of the cefotaxime-treated patients were without neurological sequelae.
Cefuroxime, a second-generation cephalosporin, is not recommended for the treatment of pneumococcal meningitis. It became less favoured for the empirical treatment of bacterial meningitis when clinical trials demonstrated superior results with third-generation cephalosporins in the treatment of meningitis. Ceftriaxone (compared with cefuroxime) was shown to sterilise CSF faster (2% vs 12% CSF cultures positive at 18–36 hours) and resulted in a lower incidence of hearing loss (4% vs 17%).[39] However, it is important to note that all patients with delayed CSF sterilisation had Hib infection. In addition, of the 11 patients who developed hearing impairment, 8 (73%) had Hib meningitis, 2 (18%) had S. pneumoniae and 1 (9%) had N. meningitidis infection.
The new fluoroquinolones are more effective than cephalosporins in vitro against pneumococci and H. influenzae.[45] An in vitro comparison of the activity of moxifloxacin, penicillin, ceftriaxone and ciprofloxacin against S. pneumoniae demonstrated that moxifloxacin was 32-fold more active than ciprofloxacin and was not affected by penicillin and cephalosporin resistance.[46] In a rabbit meningitis model, gemifloxacin reduced bacterial titres in CSF almost as rapidly as ceftriaxone; coadministration of dexamethasone did not affect gemifloxacin serum or CSF concentrations.[47] In another rabbit model, gatifloxacin was found to have excellent CNS penetration and was effective monotherapy against cephalosporin-resistant pneumococci.[48] Successful treatment with ciprofloxacin and pefloxacin of nosocomial meningitis in adults and newborns has been reported.[49] Thus, although not standard therapy, the fluoroquinolones have been investigated for use in CNS infections. Trovafloxacin was found to be as effective as ceftriaxone in a large paediatric study;[50] however, concerns regarding trovafloxacin-related hepatic toxicity prompted withdrawal of this fluoroquinolone from the market.
The excellent activity and substantial CSF penetration of the fluoroquinolones (20–60% of peak serum concentrations, even without meningeal inflammation or dexamethasone coadministration) may make them a promising option in pneumococcal meningitis caused by multi-resistant organisms in children. However, several drawbacks of this group of drugs should be kept in mind. The mutations that cause decreased susceptibility to the fluoroquinolones develop spontaneously at a frequency of 1 in 106 to 109. This rate is comparable with the development of resistance to rifampicin. In paediatric patients with pneumococcal meningitis, there maybe >108/mL infecting organisms in the CSF. Thus, resistance may develop during treatment or as a result of exposure to a person who had been treated previously with a fluoroquinolone. The emergence of fluoroquinolone-resistant S. pneumoniae is rapidly increasing[51,52] and routine susceptibility testing is currently not recommended. Thus, the choice of empirical therapy with a fluoroquinolone will be difficult. In addition, the use of fluoroquinolones in children with meningitis is currently not approved by the US FDA. Their usage should be limited to patients where other antibacterials cannot be used or have failed.
Linezolid, an oxazolinidone, has been shown to be effective in vitro against multi-resistant Gram-positive organisms, including S. pneumoniae. Linezolid is only marginally bactericidal in vitro at concentrations five and ten times above the MIC. The penetration of the drug into ventricular fluid (which may equal lumbar CSF concentrations) was excellent even without inflammation.[53] Little is known about the effectiveness of linezolid in pneumococcal CNS infections. There have been several reports of successful use of linezolid for vancomycin-resistant enterococcal meningitis.[54,55] In the rabbit model, linezolid showed good penetration into the meninges but was less effective than ceftriaxone against penicillin-sensitive strains of S. pneumoniae.[56] Linezolid had inferior killing rates against a penicillin-resistant strain of pneumococcus compared with combination therapy with ceftriaxone and vancomycin. Further investigation is required to determine if the use of linezolid for pneumococcal meningitis will be beneficial.
Chloramphenicol resistance among pneumococci was reported in 1970. Unfortunately, high rates of resistance were reported from many resource-poor countries (e.g. Southeast Asia and Africa) where chloramphenicol is affordable.[57] In addition, unsatisfactory outcomes (due to poor bactericidal activity of this drug against pneumococci) were also reported when chloramphenicol was used to treat meningitis.[58]
The recommended duration of therapy for uncomplicated pneumococcal meningitis, 10–14 days, is not based on scientific data. In the pneumococcal meningitis animal model, adequate CSF sterilisation was demonstrated after only 8 hours of penicillin therapy.[59] A randomised clinical trial of 4 versus 7 days of ceftriaxone for uncomplicated bacterial meningitis resulted in effective treatment of all children with S. pneumoniae meningitis.[60] Patients were followed for 3 months after hospital discharge, and none experienced neurological sequelae or relapse; however, the study was limited by a small sample size. Because shorter lengths of therapy would be beneficial in areas where resources are limited, further studies are needed to evaluate if length of therapy for meningitis due to highly resistant pneumococcal strains can be shortened to ≤1 week.
3.2 Haemophilus influenzae Type B
The recommended initial therapy for Hib meningitis is a third-generation cephalosporin or chloramphenicol (table II).[7] Empirical monotherapy with ampicillin is not recommended, as β-lactamase-producing strains of Hib account for up to 34% of isolates worldwide.[6] In resource-poor countries, chloramphenicol continues to be widely used because of its availability and low cost. However, Hib resistance to chloramphenicol is well described.[61,62] In addition, chloramphenicol was found to be inferior to cefotaxime and ceftriaxone in a prospective study.[63] The third-generation cephalosporins have a significantly better efficacy and safety profile than chloramphenicol, and so ceftriaxone or cefotaxime are the drugs of choice in developed nations. The second-generation cephalosporins are not recommended as they have a slower rate of sterilisation and are associated with higher sequelae rate.[64] Although cefepime[65] and meropenem[44] have shown efficacy and safety comparable with third-generation cephalosporins, they should be rarely used because clinical experience is limited, particularly in cases with S. pneumoniae resistant to penicillin and/or cefotaxine.
The recommended length of therapy for uncomplicated Hib meningitis in the US is 10 days.[66] In a study comparing 7 with 10 days of therapy, 7 days was found to be just as effective treatment.[67] In addition, in a study that compared 4 with 7 days of ceftriaxone for uncomplicated bacterial meningitis, there was no difference in clinical outcome between the two small treatment groups.[60] Thus, the length of therapy can be shortened in most patients and the ultimate length of therapy should be individualised on the basis of the clinical response of each patient.
3.3 Neisseria meningitidis
Penicillin resistance in N. meningitidis has been documented worldwide.[68–70] The majority of resistant isolates are moderately penicillin susceptible, with MIC values for penicillin of 0.12–1.0 μg/mL.[71] High-dose benzylpenicillin (250 000 U/kg/day divided every 4–6 hours) is effective therapy against these moderately susceptible strains.[71] However, it has been suggested that the outcome is poorer.[72] Thus, a third-generation cephalosporin or chloramphenicol should be used for meningococcal meningitis until the penicillin susceptibility of the organism is available (table II). There have been no reports of treatment failure with third-generation cephalosporins. Chloramphenicol remains the first-line therapy in resource-poor countries because of its availability, low cost and ease of administration. Unfortunately, recent reports documented a high level of chloramphenicol resistance among meningococci.[73] As sensitivity patterns continue to evolve, surveillance for resistant patterns must continue globally to document the distribution of resistant strains and, if necessary, to change recommendations for therapy.
The current recommended length of therapy for meningococcal meningitis is 7 days.[71] However, significantly shorter courses of therapy have proven effective. A single dose of long-acting penicillin or chloramphenicol has each been used successfully.[74,75] Additional studies found 3 or 4 days of antibacterial therapy to be effective.[76,77]
4. Adjunctive Dexamethasone Therapy
The inflammatory process associated with bacterial meningitis is due to bacterial products that stimulate massive cytokine release into the subarachnoid space.[3] This inflammatory response is important in the pathophysiology of bacterial meningitis and can lead to permanent neurological sequelae, including (most commonly) hearing loss. Various anti-inflammatory agents have been successful in reducing the harmful effect of the inflammatory response in animal models of bacterial meningitis.[3] Currently, corticosteroids (given before or concomitantly with antibacterials) are the only anti-inflammatory agent that have shown efficacy in humans.
The benefit of dexamethasone in the treatment of bacterial meningitis in children was evaluated in a meta-analysis of clinical trials published between 1988 and 1996.[78] It was concluded that, for Hib meningitis, there was significant benefit of adjunctive dexamethasone (0.15 mg/kg every 6 hours for 2 days). This benefit was most significant regarding prevention of hearing loss. However, the benefit of dexamethasone for pneumococcal meningitis was not definitive. As Hib meningitis has now been virtually eradicated in the developed world, the empirical use of adjunctive corticosteroids in areas where pneumococci are the most common pathogen has been controversial. There are several reasons to question the suggested benefit of dexamethasone in pneumococcal meningitis. Several studies that were included in the meta-analysis by McIntyre et al.[78] are questionable. For example, the Egyptian study had an unusually high mortality rate (28%) and children <5 years of age were not assessed for hearing loss.[79] This study included 429 patients ranging in age from 3 months to 60 years (mean 12.5 years) but only 106 of these patients had pneumococcal meningitis. The authors observed a significant reduction in mortality and hearing impairment in patients with pneumococcal meningitis, but they did not specify if the observed effects of dexamethasone were in adults or children, or both. In addition, the Turkish study included only children >2 years of age, and the differences in moderate or severe hearing loss were statistically insignificant at 6 weeks’ follow-up.[80] This study enrolled 53 patients with pneumococcal meningitis (27 received dexamethasone and 26 received placebo). There were no differences between the two groups in mortality or neurological outcome. One patient with profound hearing loss (at 6 weeks’ follow-up) who received dexamethasone was found to have a normal hearing at 3 months after discharge in the Turkish study. With this ‘improvement’, hearing impairment became significantly less in the dexamethasone group. The authors of the meta-analysis admitted that “the Egyptian study differed from others”, and that “the statistical significance of protection from early dexamethasone was vulnerable to exclusion of this study. Without the Egyptian study, the odds ratio for early dexamethasone became 0.3 (95% CI, 0.03–1.84; p = 0.26)”;[78] the statistical significance of a beneficial effect of dexamethasone is lost. In a retrospective study of 97 children with pneumococcal meningitis (41 of whom received dexamethasone and 56 who did not), no significant differences between the treatment groups were found in regard to presence of seizures, subdural effusions, hydrocephalus or death. In addition, no differences in neurological or audiological outcome were found at 6 weeks’ and 4 months’ follow-up. The number of survivors with any adverse outcome was smaller in patients who received corticosteroids within 24 hours of initiating antibacterials compared with those who never received corticosteroid therapy (4 of 35 vs 14 of 43, p = 0.033).[81]
With the current recommended therapy of vancomycin and a third-generation cephalosporin, the benefit of dexamethasone in the treatment of pneumococcal meningitis is even more in doubt. As dexamethasone is an anti-inflammatory agent, it significantly reduces the ability of some antibacterials to cross the BBB, leading to diminished CSF antibacterial concentrations. In animal models, vancomycin concentrations in the CSF were reduced by 44–77% when administered with dexamethasone.[40,82] As a result, a delay in CSF sterilisation was observed in the animals treated with dexamethasone. The concern about the diminished CNS penetration of vancomycin in patients receiving adjunctive corticosteroids led to the recommendation in adults that rifampicin be preferred over vancomycin if dexamethasone is used.[83]
Recently, De Gans and Van de Beek[8] concluded that early treatment with dexamethasone improved the overall clinical outcome of adults with bacterial meningitis. Extrapolation of this study’s results to paediatric patients is difficult. First, all of the pneumococcal isolates available for susceptibility testing (72%) in this trial were penicillin-sensitive; no patient was treated with vancomycin. In addition, there was no significant beneficial effect on neurological sequelae, including hearing loss, which is a major concern in the paediatric population. Secondly, pneumococcal meningitis in adults is different from that in paediatric patients both by the predisposing or associated conditions and by the spectrum of complications and outcome.[84] In general, fatalities are less frequent in children than in adults, and any attempt to extrapolate from the De Gans and Van de Beek study to paediatric patients must take these differences into account.
Several other observations suggest that any decision to add dexamethasone to the current recommended therapy for pneumococcal meningitis should be made with caution. A 3-year multicentre retrospective study of pneumococcal meningitis (from 1993 to 1996), which included 40 children who had received dexamethasone (initiated before or within 1 hour after the initiation of antibacterials), showed that the incidence of moderate-to-severe hearing loss was significantly higher in the dexamethasone group (46%) compared with the group who did not receive any corticosteroids (23%).[34] However, the children who received dexamethasone were more critically ill, with more abnormal CSF parameters on presentation. When such factors were controlled for, the incidence of neurological sequelae between the two groups was no longer statistically significant.
The largest placebo-controlled, double-blind, randomised trial of adjunctive dexamethasone therapy for bacterial meningitis was performed in Malawi by Molyneux et al.[85] This study included 598 children (aged 2 months to 13 years old); 51% received dexamethasone, while 49% received placebo. Five to ten minutes after adjunctive therapy was given, patients were treated with benzylpenicillin and chloramphenicol. The aetiological agents included S. pneumoniae (40%), Hib (28%), N. meningitidis (11%) and Salmonella species (5%). Thirteen percent of patients had negative CSF cultures. Of the 229 pneumococcal isolates, 39 (17%) were resistant to chloramphenicol and 47 (20%) were resistant to penicillin. Comorbidities in this population included HIV infection, malnutrition and anaemia. In comparing the outcome of both groups, there was no difference in survival or neurological sequelae. It was concluded that corticosteroids are not an effective adjuvant in the treatment of acute bacterial meningitis in resource-poor countries. The relevance of the outcome of this study in a resource-poor country is not clear regarding paediatric care in developed countries or in developing countries with better health systems than Malawi.
Recently, two studies using different animal models showed increased hippocampal neuronal apoptosis when dexamethasone was added to treatment of pneumococcal meningitis.[86,87] Furthermore, dexamethasone therapy was associated with reduced learning capacity and spatial memory.[87] If a large prospective, randomised, placebo-controlled trial to evaluate the use of dexamethasone in pneumococcal meningitis is performed, it should assess all the possible effects of the drug on the CNS and not only hearing loss. Taking into account this information, recommendations regarding dexamethasone treatment should be made with maximum caution. With the current pneumococcal vaccination recommendations to prevent invasive infections and the resultant decreased incidence of pneumococcal meningitis, the need to make this difficult decision may become a rare event.
5. Other Adjunctive Anti-inflammatory Agents
Currently, dexamethasone is the only anti-inflammatory agent extensively studied and used, both in experimental models and in clinical paediatric trials. There are several other anti-inflammatory agents that have been reported as possible adjunctive therapy for bacterial meningitis, all with the common goal of reducing brain injury. Such experimental therapies, studied in animal meningitis models, include: NSAIDs such as ketorolac, which, with ampicillin, reduced sensorineural hearing loss compared with placebo;[88] monoclonal antibody against tumour necrosis factor-α, which lowered intracranial pressure and reduced CSF pleocytosis;[89] and the bradykinin receptor antagonist labradimil (RMP-7), which increases BBB permeability at the endothelial tight junctions and improves the CNS penetration of both antimicrobials and chemotherapeutics.[90] Induced hypothermia has also been evaluated as adjunctive treatment to decrease intracranial pressure and cerebral oedema;[91] similar hypothermic treatment has been proposed for patients with traumatic brain injury. As all of these adjunctive treatments are considered experimental, none is currently recommended for the treatment of patients with bacterial meningitis.
6. Other Considerations
6.1 Syndrome of Inappropriate Antidiuretic Hormone Secretion
Hyponatraemia, which commonly occurs in bacterial meningitis, can worsen the course of the disease and its outcome.[92] Because the secretion of antidiuretic hormone in most of these children was found to be increased (Syndrome of Inappropriate Antidiuretic Hormone Secretions; SIADH), it was assumed that retention of body water due to this hormone is the cause of the hyponatraemia. As a result, fluid restriction (two-thirds of usual maintenance) has been widely advocated and used. For example, Duke and Molyneux[93] suggested that administration of 0.9% saline (with 5% dextrose) at less than maintenance volume will result in lower frequency of hyponatraemia and neurological events. In recent years this practice was challenged because it was shown that many of these children were dehydrated[94] and/or hypovolaemic[95] for other reasons (e.g. vomiting, diminished intake, diarrhoea). In addition, Singhi et al.[96] showed that routine fluid restriction did not improve the outcome and may be associated with a higher mortality rate in those children who had reduction in extracellular water of >10 mL/kg because of fluid restriction during the initial 48 hours of medical therapy. Therefore, only a selected group of patients (those with hyponatraemia clearly due to SIADH) may benefit from fluid restriction. The diagnosis of SIADH should be based on the following strict criteria (as described by Bartter and Schwartz[97]): (i) hyponatraemia with corresponding hypo-osmolality of the serum and extracellular fluid; (ii) continued renal excretion of sodium; (iii) absence of chemical evidence of volume depletion; (iv) osmolality of urine greater than that appropriate for the concomitant tonicity of the plasma; (v) normal renal function; and (vi) normal adrenal function. Empirical fluid restriction in all patients with bacterial meningitis should be avoided. Only patients with a diagnosis of ‘true’ SIADH (based on these criteria) or developing increased intracranial pressure should be treated with fluid restriction.
6.2 Prophylaxis
The secondary attack rate of N. meningitidis in households of an index case is about 3 per 1000, a rate 1000 times the attack rate in the general population.[98] Because of this significantly increased risk, chemoprophylaxis is recommended for household contacts of an index case and for others with close contact. For healthcare workers, prophylaxis is indicated only when intimate exposure with nasopharyngeal secretions occurred, such as mouth-to-mouth resuscitation or endotracheal intubation. Individuals in close contact with the index case up to 7 days before onset of illness should be considered for prophylaxis.[71]
There are three recommended agents for chemoprophylaxis against N. meningitidis (table III). A fourth drug, sulfadiazine, which was the original drug used for meningococcal chemoprophylaxis, is no longer recommended because of the emergence of sulfa-resistant strains. Oral rifampicin is currently the drug of choice for chemoprophylaxis in the paediatric population. Alternatives include a single intramuscular dose of ceftriaxone or a single dose of oral ciprofloxacin. The use of fluoroquinolones is not approved for pregnant women and children.
Unfortunately, rifampicin resistance among N. meningitidis was reported in Israel in the mid-1990s[99] and has been recently reported in the US;[100] increasing rifampicin resistance may have significant public health impact, as it is the sole oral agent recommended in the paediatric population.
The benefit of chemoprophylaxis to prevent the spread of Hib is controversial.[101,102] Yet, the AAP[66] recommends chemoprophylaxis for households in the following circumstances: (i) if there is at least one contact <4 years of age who is not immunised or incompletely immunised; (ii) if there is a child <12 months of age that has not received the primary series; or (iii) if there is an immunocompromised child in the household (regardless of immunisation status). Chemoprophylaxis is also indicated for nursery school and child care contacts, regardless of age, when two or more cases of Hib invasive disease have occurred within 60 days, and for the index case, if <2 years of age or a member of a household with a susceptible contact and treated with a regimen other than cefotaxime or ceftriaxone. In the latter instance, chemoprophylaxis should be given at the time of hospital discharge. Rifampicin, which eradicated 95% of nasopharyngeal carriage,[103] is recommended (20 mg/kg/day twice daily for 2 days; maximum dose 600mg).
6.3 Vaccination
The overwhelming success of Hib vaccination in the developed world is an example of the impact that immunisation can have on the disease. For S. pneumoniae, a 23-valent polysaccharide vaccine has been available for many years and is useful in preventing invasive disease in the elderly population. However, this vaccine is poorly immunogenic in children younger than 2 years of age, in whom the highest proportion of invasive pneumococcal disease occurs. In 2000, a pneumococcal vaccine was introduced which contains seven capsular polysaccharide antigens, each of which is conjugated to a diphtheria protein (cross-reactive material CRM197). This protein-conjugated vaccine elicits an adequate T cell-dependent response in young children, thus protecting this vulnerable population against the seven strains of pneumococci most associated with invasive disease. As noted in section 1, a significant reduction in paediatric invasive pneumococcal disease has already been demonstrated, especially in children <2 years of age.[12,104] Both 9- and 11-valent conjugated pneumococcal vaccines are currently under investigation.[11]
Primary prevention of meningococcal disease is essential; the disease may be so fulminant on presentation that medical therapy (including antibacterials) makes no impact on the course of the disease. Thus, purified capsular polysaccharide vaccines against N. meningitidis serogroups A, C, Y and W135 have been developed. They are available as monovalent A and C, bivalent A/C and quadrivalent A/C/Y/W135 vaccines; the quadrivalent polysaccharide is the only vaccine that is licensed and available in the US. Group A vaccine is effectively immunogenic in all age groups. This vaccine has been effective in terminating epidemics of group A disease.[105] The recent introduction of conjugate group C vaccine in the UK resulted in an approximately 80% reduction in the incidence of group C disease.[106] In addition, a herd immunity (i.e. reduction in attack rate of unvaccinated people) was documented.[107] Unfortunately, no vaccine exists against serogroup B, as the capsular polysaccharide of this serogroup is not immunogenic in humans. Development of a vaccine against serogroup B remains a priority, and investigational trials continue. Intranasal administration of a meningococcal outer membrane vesicle vaccine was shown to induce persistent local and serum antibodies.[108] Two outer membrane meningococcal B vaccines, developed in Cuba and Norway, were found to be useful during epidemics with a single circulating serotype B.[109,110] Such a vaccine is also being evaluated in New Zealand, where a meningococcal B epidemic is ongoing since 1991.[111] Unfortunately, this vaccine will not be useful for routine immunisation because many endemic areas have multiple B serosubtypes (i.e. heterogeneous) and the protection provided by the vaccine will be limited to the substrain from which it was developed. Others are attempting to develop an immunogenic vaccine by chemically modifying the polysaccharide and conjugating it to an immunogenic protein carrier.[112] This vaccine is currently undergoing clinical trials.
Since 1987, Saudi Arabia health authorities require compulsory vaccination with the bivalent A and C vaccine for all Hajj pilgrims and annual vaccination campaigns for all local populations living in pilgrimage sites. However, in the past several years serogroup W135 has emerged, including an outbreak of >300 cases in Saudi Arabia and nine other countries among the Hajj pilgrims or their close contacts.[113] As a result, vaccination policies since 2002 include the quadrivalent vaccine for both local residents and Hajj pilgrims.
Routine childhood vaccination with the quadrivalent vaccine is not recommended because of its low immunogenicity in young children.[114] The AAP recommends vaccination of those who have functional or anatomic asplenia, terminal complement component or properdin deficiencies, and college students who live in dormitories.[71]
7. Conclusions
Despite advances in antibacterial therapy and vaccine development, bacterial meningitis remains a significant cause of morbidity and mortality in paediatric patients. Resource-poor countries continue to face the hardship of economic constraints, unable to offer the benefits of vaccine technology. Hib remains a significant cause of disease in these countries, while its incidence has dramatically decreased in the developed world as a result of widespread vaccination. In developed countries, advances in pneumococcal and meningococcal vaccination are likely to lead to similar trends.
Resistance patterns to currently available antibacterials continue to evolve. As a result, clinicians must remain vigilant in detecting the emergence of new resistant strains. The continued development of new and effective antibacterials for bacterial meningitis is greatly needed. In addition, we must continue to evaluate the possible usefulness of adjunctive anti-inflammatory agents as dexamethasone use remains controversial in pneumococcal meningitis.
The widespread availability of preventive vaccines against the common pathogens of bacterial meningitis is the ultimate goal; until this goal is reached, timely diagnosis and treatment is paramount to minimise morbidity and mortality.
References
Wenger JD, Hightower AW, Facklam RR, et al. Bacterial meningitis in the United States, 1986: report of a multistate surveillance study. J Infect Dis 1990; 162: 1316–23
Short WR, Tunkel AR. Changing epidemiology of bacterial meningitis in the United States. Curr Infect Dis Rep 2000; 2: 327–31
Koedel U, Scheid WM, Pfister HW. Pathogenesis and pathophysiology of pneumococcal meningitis. Lancet Infect Dis 2002; 2: 721–36
Hansman D, Bullen MM. A resistant pneumococcus. Lancet 1967; 1: 264–5
Whitney CG, Farley MM, Hadler M, et al. Increasing prevalence of multidrug-resistant Streptococcus pneumoniae in the United States. N Engl J Med 2000; 343: 1917–24
Hoban DJ, Doern GV, Fluit AC, et al. Worldwide prevalence of antimicrobial resistance in Streptococcus pneumoniae, Haemophilus influenzae, and Moraxella catarrhalis in the SENTRY Antimicrobial Surveillance Program, 1997–1999. Clin Infect Dis 2001; 32 Suppl. 2: S81–93
Feigin, RD, Pearlman E. Bacterial meningitis beyond the neonatal period. In: Feigin RD, Cherry JO, Demmber GJ, et al., editors. Textbook of pediatric infectious diseases. 5th ed. Philadelphia (PA): Saunders, 2003: 443–74
De Gans J, Van de Beek D. Dexamethasone in adults with bacterial meningitis. N Engl J Med 2002; 347: 1549–56
Centers for Disease Control and Prevention. Progress towards eliminating Haemophilus influenzae type b disease among infants and children: United States, 1987–1997. MMWR Morb Mortal Wkly Rep 1998; 47(46): 993–8
Schuchat A, Robinson K, Wenger JD, et al. Bacterial meningitis in the United States in1995. N Engl J Med 1997; 337: 970–6
Whitney CG, Farley MM, Hadler JH, et al. Decline in invasive pneumococcal disease after the introduction of protein-polysaccharide conjugate vaccine. N Engl J Med 2003; 348: 1737–46
Kaplan SL, Mason EO, Wald ER, et al. Decrease of invasive pneumococcal infections in children among 8 children’s hospitals in the United States after the introduction of the 7-valent pneumococcal conjugate vaccine. Pediatrics 2004; 113: 443–9
Pastor P, Medley KB, Murphy TV. Meningococcal disease in Dallas County, Texas: results of a six-year population-based study. Pediatr Infect Dis J 2000; 19: 324–48
Rosenstein N, Perkins B, Stephens D, et al. The changing epidemiology of meningococcal disease in the United States, 1992–1996. J Infect Dis 1999; 180: 1894–901
Scholten R, Bijlmer H, Valkenburg H, et al. Patient and strain characteristics in relation to the outcome of meningococcal disease: a multivariate analysis. Epidemiol Infect 1994; 112: 115–9
Balmer P, Borrow R, Miller E. Impact of meningococcal C conjugate vaccine in the UK. J Med Microbiol 2002; 51: 717–22
Emele FE. Etiologic spectrum and pattern of antimicrobial drug susceptibility in bacterial meningitis in Sokoto, Nigeria. Acta Paediatr 2000; 89: 942–6
World Health Organization. Epidemic meningococcal disease. WHO Fact Sheet105. Geneva: WHO, 1998
Tauber MG, Doroshow CA, Hackbarth CJ, et al. Antibacterial activity of β-lactam antibiotics in experimental meningitis due to Streptococcus pneumoniae. J Infect Dis 1984; 149: 568–74
Scheid WM, Brown RS, Sande MA. Comparison of netilmicin and gentamicin in the therapy of experimental Escherichia coli meningitis. Antimicrob Agents Chemother 1978; 13: 899–904
Kim YS, Liou Q, Chow LL, et al. Trovafloxacin in treatment of rabbits with experimental meningitis caused by high-level penicillin-resistant Streptococcus pneumoniae. Antimicrob Agents Chemother 1997; 41: 1186–9
Nau R, Schmidt T, Kaye K, et al. Quinolone antibiotics in therapy of experimental pneumococcal meningitis in rabbits. Antimicrob Agents Chemother 1995; 39: 593–7
Lutsar I, McCracken GH, Friedland IR, et al. Antibiotic pharmacodynamics in cerebrospinal fluid. Clin Infect Dis 1998; 27: 1117–29
Nau R, Kaye K, Sachdeva M, et al. Rifampin for therapy of experimental pneumococcal meningitis in rabbits. Antimicrob Agents Chemother 1994; 38: 1186–9
Quagliarello VJ, Long WJ, Scheid WM. Morphologic alterations of the blood-brain barrier with experimental meningitis in the rat. J Clin Invest 1986; 77: 1084–95
Hieber JP, Nelson JD. A pharmacologic evaluation of penicillin in children with purulent meningitis. N Engl J Med 1977; 297: 410–3
Chowdhury MH, Tunkel AR. Antibacterial agents in infections of the central nervous system. Infect Dis Clin N Am 2000; 14: 391–408
Krontz DP, Strausbaugh LJ. Effect of meningitis and probenecid on the penetration of vancomycin into cerebrospinal fluid in rabbits. Antimicrob Agents Chemother 1980; 18: 882–6
Spector R, Lorenzo AV. Inhibition of penicillin transport from the CSF following intracisternal inoculation of bacteria. J Clin Invest 1974; 54: 316–25
Craig WA. Pharmacokinetic/pharmacodynamic parameters: rationale for antibacterial dosing of mice and men. Clin Infect Dis 1998; 26: 1–12
Aronin SI, Peduzzi P, Quagliarello VJ. Community-acquired bacterial meningitis: risk stratification for adverse clinical outcome and effect of antibiotic timing. Ann Intern Med 1998; 129: 862–9
Radetsky M. Duration of symptoms and outcome in bacterial meningitis: an analysis of causation and the implications of a delay in diagnosis. Pediatr Infect Dis J 1992; 11: 694–8
American Academy of Pediatrics. Pneumococcal infections. In: Pickering LK, editor. Red book: 2003 report of the Committee on Infectious Diseases. 26th ed. Elk Grove Village (IL): American Academy of Pediatrics, 2003: 490–500
Arditi M, Mason EO, Bradley JS, et al. Three-year multicenter surveillance of pneumococcal meningitis in children: clinical characteristics, and outcome related to penicillin susceptibility and dexamethasone use. Pediatrics 1998; 102: 1087–97
Friedland IR, Paris M, Ehrett S, et al. Evaluation of antimicrobial regimens for treatment of experimental penicillin- and cephalosporin-resistant pneumococcal meningitis. Antimicrob Agents Chemother 1993; 37: 1630–6
Klugman KP, Friedland IR, Bradley JS. Bactericidal activity against cephalosporin-resistant Streptococcus pneumoniae in cerebrospinal fluid of children with acute bacterial meningitis. Antimicrob Agents Chemother 1995; 39: 1988–92
National Committee for Clinical Laboratory Standards. Performance standards for antimicrobial susceptibility testing. 13th Informational Supplement (Aerobic Dilution). Wayne (PA): National Committee for Clinical Laboratory Standards, 2003: 44–6
Viladrich PF, Gudiol F, Linares J, et al. Evaluation of vancomycin for therapy of adult pneumococcal meningitis. Antimicrob Agents Chemother 1991; 35: 2467–72
Schaad UB, Suter S, Gianella-Borradori A, et al. A comparison of ceftriaxone and cefuroxime for the treatment of bacterial meningitis in children. N Engl J Med 1990; 322: 141–7
Paris MM, Hickey SM, Uscher MI, et al. Effect of dexamethasone on therapy of experimental penicillin- and cephalosporin-resistant pneumococcal meningitis. Antimicrob Agents Chemother 1994; 38: 1320–4
Novak R, Henriques B, Charpentier E, et al. Emergence of vancomycin tolerance in Streptococcus pneumoniae. Nature 1999; 399: 590–3
Nau R, Wellmer A, Soto A, et al. Rifampin reduces early mortality in experimental Streptococcus pneumoniae meningitis. J Infect Dis 1999; 179: 1557–60
Gerber J, Yamini P, Nau R. After pretreatment by rifampin, ceftriaxone releases smaller quantities of lipoteichoic and teichoic acids (LTA/TA) from Streptococcus pneumoniae than ceftriaxone alone [abstract no. 1788]. 39th Interscience Conference on Antimicrobial Agents and Chemotherapy; 1992 Sep 26–29; San Francisco
Odio CM, Puig JR, Feris JM, et al. Prospective, randomized, investigator-blinded study of the efficacy and safety of meropenem vs cefotaxime therapy in bacterial meningitis in children. Pediatr Infect Dis J 1999; 18: 581–90
Thornsberry C, Ogilvie P, Holley HP, et al. The activity of fluoroquinolones and other antimicrobial agents against Streptococcus pneumoniae, Haemophilius influenzae, and Moraxella catarrhalis. Drugs 1999; 58 Suppl. 2: 346–8
Tarasi A, Capone A, Tarasi D, et al. Comparative in-vitro activity of maxifloxacin, penicillin, ceftriaxone, and ciprofloxacin against pneumococci isolated from meningitis. J Antimicrob Chemother 1999; 43: 833–5
Smirnov A, Welmer A, Gerber J, et al. Gemifloxacin is effective in experimental pneumonococcal meningitis. Antimicrob Agents Chemother 2000; 44: 767–70
Lutsar I, Friedland IR, Wubbel L, et al. Pharmacodynamics of gatifloxacin in cerebrospinal fluid in experimental cephalosporin-resistant pneumococcal meningitis. Antimicrob Agents Chemother 1998; 42: 2650–5
Filka J, Uher J, Kurak H, et al. Ciprofloxacin in the treatment of nosocomial meningitis in neonates and infants. Drugs 1999; 58 Suppl. 2: 263–5
Saez-Llorens X, McCoig C, Feris JM, et al. Quinolone treatment for pediatric bacterial meningitis: a comparative study of trovafloxacin and ceftriaxone with or without vancomycin. Pediatr Infect Dis J 2002; 21: 14–22
Ho PL, Que TL, Tsang DN, et al. Emergence of fluoroquinolone resistance among multiple resistant strains of Streptococcus pneumoniae in Hong Kong. Antimicrob Agents Chemother 1999; 43: 1310–3
Chen DK, McGeer A, de Azavedo JC, et al. Decreased susceptibility of Streptococcus pneumoniae to fluoroquinolones in Canada. N Engl J Med 1999; 341: 233–9
Yogev R, Edge-Padbury B, Naberhuis-Stehouwer S, et al. Linezolid vs vancomycin in children with complicated skin/ skin structure infections: the Linezolid Pediatric Study Group [poster no. 1839]. Pediatric Academic Societies’ Meeting (PAS); 2003 May 3–6; Seattle
Zeana C, Kublin CJ, Della-Latta P, et al. Vancomycin-resistant Enterococcus faecium meningitis successfully managed with linezolid: case report and review of the literature. Clin Infect Dis 2001; 33: 477–82
Shaikh ZH, Peloquin CA, Ericcson CD. Successful treatment of vancomycin-resistant Enterococcus faecium meningitis with linezolid: case report and review of the literature. Scand J Infect Dis 2001; 33: 375–9
Cottagnoud P, Gerber CM, Acosta F, et al. Linezolid against penicillin-sensitive and -resistant pneumococci in the rabbit model. J Antimicrob Chemother 2000; 46: 981–5
Lee H, Park J, Jang SE. High incidence of resistance to multiply antimicrobials in clinical isolates of Streptococcus pneumoniae from a university hospital in Korea. Clin Infect Dis 1995; 20: 826–35
Friedland IR, Klugman KP. Failure of chloramphenicol therapy in penicillin-resistant pneumococcal meningitis. Lancet 1992; 339: 405–8
Sande MA, Korzeniowski OM, Allegro GM. Intermittent or continuous therapy of experimental meningitis due to Streptococcus pneumoniae in rabbits: preliminary observations on the postantibiotic effect in vivo. Rev Infect Dis 1981; 3: 98–109
Roine I, Ledermann W, Foncea LM. Randomized trial of four vs seven days of ceftriaxone treatment for bacterial meningitis in children with rapid initial recovery. Pediatr Infect Dis J 2000; 19: 219–22
Campos J, Garcia-Tornel S, Gairi JM, et al. Multiply resistant Haemophilus influenzae type b causing meningitis: comparative clinical and laboratory study. J Pediatr 1986; 108: 897–902
Givner LB, Abramson JS, Wasilauskas B. Meningitis due to Haemophilus influenzae type b resistant to ampicillin and chloramphenicol. Rev Infect Dis 1989; 11: 329–34
Peltola J, Anttila M, Renkonen OV, et al. Randomized comparison of chloramphenicol, ampicillin, cefotaxime, and ceftriaxone for childhood bacterial meningitis. Lancet 1989; I: 1281–7
Lebel MH, McCracken Jr GH. Delayed cerebrospinal fluid sterilization and adverse outcome of bacterial meningitis in infants and children. Pediatrics 1989; 83: 161–7
Saez-Llorens X, Castano E, Garcia R, et al. Prospective randomized comparison of cefepime and cefotaxime for treatment of bacterial meningitis in infants and children. Antimicrob Agents Chemother 1995; 39: 937–40
American Academy of Pediatrics. Haemophilus influenzae infections. In: Pickering LK, editor. Red Book: 2003 report of the Committee on Infectious Diseases. 26th ed. Elk Grove Village (IL): American Academy of Pediatrics, 2003: 293–301
Lin TY, Chrane DF, Nelson JD, et al. Seven days of ceftriaxone therapy is as effective as ten days’ treatment for bacterial meningitis. JAMA 1985; 253: 3559–63
Saez-Nieto JA, Lujan R, Berron S, et al. Epidemiology and molecular basis of penicillin-resistant Neisseria meningitidis in Spain: a 5-year history (1985–89). Clin Infect Dis 1992; 14: 394–402
Klugman KP, Madhi SA. Emergence of drug resistance: impact on bacterial meningitis. Infect Dis Clin North Am 1999; 13: 637–46
Woods CR, Smith AL, Wasilauskas BL, et al. Invasive disease caused by Neisseria meningitidis relatively resistant to penicillin in North Carolina. J Infect Dis 1994; 170: 453–6
American Academy of Pediatrics. Meningococcal infections. In: Pickering LK, editor. Red book: 2003 report of the Committee on Infectious Diseases. 26th ed. Elk Grove Village (IL): American Academy of Pediatrics, 2003: 430–6
Luaces Cubells C, Garcia Garcia JJ, Roca Martinez J, et al. Clinical data in children with meningococcal meningitis in a Spanish hospital. Acta Paediatr 1997; 86: 26–9
Galimand M, Gerbaud G, Guibourdenche M, et al. High-level chloramphenicol resistance in Neisseria meningitidis. N Engl J Med 1998; 339: 868–74
Macfarlane JT, Anjorin FI, Cleland PG, et al. Single injection treatment of meningococcal meningitis. 1: long-acting penicillin. Trans R Soc Trop Med Hyg 1979; 73: 693–7
Wali SS, Macfarlane JT, Weir WRC, et al. Single injection treatment of meningococcal meningitis. 2: long-acting chloramphenicol. Trans R Soc Trop Med Hyg 1979; 73: 698–702
Viladrich PF, Pallares R, Ariza J, et al. Four days of penicillin therapy for meningococcal meningitis. Arch Intern Med 1986; 146: 2380–2
O’Neill P. How long to treat bacterial meningitis. Lancet 1993; 341: 530–2
McIntyre PB, Berkey CS, King SM, et al. Dexamethasone as adjunctive therapy in bacterial meningitis: a meta-analysis of randomized clinical trials since1988. JAMA 1997; 278: 925–31
Girgis NI, Farid Z, Mikhail IA, et al. Dexamethasone treatment for bacterial meningitis in children and adults. Pediatr Infect Dis 1989; 8: 848–51
Kanra GY, Ozen H, Secmeer G, et al. Beneficial effects of dexamethasone in children with pneumococcal meningitis. Pediatr Infect Dis J 1995; 14: 490–4
Kennedy WA, Hoyt MJ, McCracken GH. The role of corticosteroid therapy in children with pneumococcal meningitis. Am J Dis Child 1991; 145: 1374–8
Cabellos C, Martinez-Lacasa J, Martos A, et al. Influence of dexamethasone on efficacy of ceftriaxone and vancomycin therapy in experimental pneumococcal meningitis. Antimicrob Agents Chemother 1995; 39: 2158–60
Quagliarello VJ, Scheld WM. Treatment of bacterial meningitis. N Engl J Med 1997; 336: 708–16
Kastenbauer S, Pfister HW. Pneumococcal meningitis in adults: spectrum of complications and prognostic factors in a series of 87 cases. Brain 2003; 126: 1015–25
Molyneux EM, Walsh AL, Forsyth H, et al. Dexamethasone treatment in childhood bacterial meningitis in Malawi: a randomized controlled trial. Lancet 2002; 360: 211–8
Zysk G, Bruck W, Gerber J, et al. Anti-inflammatory treatment influences neuronal apoptotic cell death in the dentate gyrus in experimental pneumococcal meningitis. J Neuropathol Exp Neurol 1996; 55: 722–8
Leib SL, Heimgartner C, Bifrafe YD, et al. Dexamethasone aggravates hippocampal apoptosis and learning deficiency in pneumococcal meningitis in infant rats. Pediatr Res 2003; 54: 353–7
Rappaport JM, Bhatt SM, Burkard RF, et al. Prevention of hearing loss in experimental pneumococcal meningitis by the administration of dexamethasone and ketorolac. J Infect Dis 1999; 179: 264–8
Park WS, Chang YS, Ko SY, et al. Efficacy of anti-tumor necrosis factor-alpha antibody as an adjunctive therapy in experimental Escherichia coli meningitis in the newborn piglet. Biol Neonate 1999; 75: 377–87
Alavi A, Shoa L, Lattanand C, et al. Brain tumor permeability enhanced by RMP-7, a novel bradykinin agonist. Can J Infect Dis 1995; 6 Suppl. C: 4153–7
Irazuzta JE, Pretzlaff R, Rowin M, et al. Hypothermia as an adjunctive treatment for severe bacterial meningitis. Brain Res 2000; 881: 88–97
Kaplan SL, Feigin RD. The syndrome of inappropriate secretion of antidiuretic hormone in children with bacterial meningitis. J Pediatr 1978; 92: 758–61
Duke T, Molyneux EL. Intravenous fluids for seriously ill children: time to reconsider. Lancet 2003; 362: 1320–3
Kanakriyeh M, Carvajal HF, Vallone AM. Initial fluid therapy for children with meningitis with consideration of syndrome of inappropriate antidiuretic hormone. Clin Pediatr 1987; 26: 126–30
Powell KR, Sugarman LI, Eskenazi AE, et al. Normalization of plasma arginine vasopressin concentrations when children with meningitis are given maintenance plus replacement fluid therapy. J Pediatr 1990; 117: 515–22
Singhi SC, Singhi PD, Srinivas B, et al. Fluid restriction does not improve the outcome of acute meningitis. Pediatr Infect Dis J 1995; 14: 495–503
Bartter FC, Schwartz WB. The syndrome of inappropriate secretion of antidiuretic hormone. Am J Med 1967; 42: 790–806
Stanwell-Smith RE, Stuart JM, Hughes AO, et al. Smoking, the environment, and meningococcal disease: a case control study. Epidemiol Infect 1994; 112: 315–28
Almog R, Block C, Gdalevitch M, et al. First recorded outbreak of meningococcal disease in the Israel Defence Force: three clusters due to serotype C and the emergence of resistance to rifampicin. Infection 1994; 22: 67–71
Abadi FJ, Carter PE, Cash P, et al. Rifampicin resistance in Neisseria meningitidis due to alterations in membrane permeability. Antimicrob Agents Chemother 1996; 40: 646–51
Osterholm MT, Murphy TD. Does rifampin prophylaxis prevent disease caused by Haemophilus influenzae type b? JAMA 1984; 251: 2408–9
Mann M, Hull HF. New Haemophilus influenzae type b control strategy: premature commitment to prophylaxis? Pediatrics 1983; 72: 118–21
Shapiro ED, Wald ER. Efficacy of rifampin in eliminating pharyngeal carriage of Haemophilus influenzae type b. Pediatrics 1980; 66: 5–8
Foster C, Nadel S. New therapies and vaccines for bacterial meningitis. Expert Opin Investig Drugs 2002; 11: 1051–60
Lennon D, Gellin B, Hood D, et al. Successful intervention in group A meningococcal outbreak in Auckland, New Zealand. Pediatr Infect Dis J 1992; 11: 617–23
Ramsey ME, Andrews N, Kaczmarski EB, et al. Efficacy of meningococcal serogroup C conjugate vaccine in teenagers and toddlers in England. Lancet 2001; 357: 195–6
Ramsay ME, Andrews NJ, Trotter CL, et al. Herd immunity from meningococcal serogroup C conjugate vaccination in England: database analysis. BMJ 2003; 326: 365–6
Haneberg B, Dalseg R, Wedege E, et al. Intranasal administration of a meningococcal outer membrane vesicle vaccine induces persistent local mucosal antibodies and serum antibodies with strong bactericidal activity in humans. Infect Immun 1998; 66: 1334–41
Sierra GV, Campa HC, Varcacel NM, et al. Vaccine against group B Neisseria meningitidis: protection trial and mass vaccination results in Cuba. NIPH Ann 1991; 14: 195–210
Bjune G, Høiby EA, Grønnesby JK, et al. Effect of outer membrane vesicle vaccine against group B meningococcal disease in Norway. Lancet 1991; 338: 1093–6
O’Hallahan J, Lennon D, Oster P. The strategy to control New Zealand’s epidemic of group B meningococcal disease. Ped Infect Dis J 2004; 23 Suppl. 12: S293–8
Fucso PC, Michon F, Tai JY, et al. Preclinical evaluation of a novel group B meningococcal conjugate vaccine that elicits bactericidal activity in both mice and nonhuman primates. J Infect Dis 1997; 175: 364–72
Memish A. Meingococcal disease and travel. Clin Infect Dis 2002; 34: 84–90
Control and prevention of serogroup C meningococcal disease: evaluation and management of suspected outbreaks. Recommendations of the Advisory Committee on Immunization Practices (ACIP). MMWR Recomm Rep 1997; 46(RR-5): 13–21
Acknowledgements
The authors would like to thank Dr Stanford T. Shulman for his helpful comments and Sara Calvert for her secretarial assistance.
No sources of funding were used to assist in the preparation of this review. The authors have no conflicts of interest directly relevant to the content of this review.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Yogev, R., Guzman-Cottrill, J. Bacterial Meningitis in Children. Drugs 65, 1097–1112 (2005). https://doi.org/10.2165/00003495-200565080-00005
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003495-200565080-00005