Summary
The observation that drug concentrations in saliva are often proportional to the concentrations in plasma has led to the suggestion that in therapeutic drug monitoring, or in pharmacokinetic studies in general, saliva might be substituted for plasma. Saliva can be collected by non-invasive techniques, generally following the stimulation of salivary flow by chewing on some semi-solid material or by spraying citric acid on the tongue.
There is evidence that many organic compounds enter saliva by a passive diffusion process, where lipid solubility and the degree of ionisation — dependent on plasma and salivary pH —are important factors. In addition, it has been shown for some drugs that their concentration in saliva equals the free or protein-unbound concentration in plasma, which is an advantage because drug plasma concentrations generally represent both bound and unbound drug. Lithium is the most well-known example of a drug that is actively secreted in saliva, but active transport mechanisms have also been proposed for organic drugs since discrepancies and time dependencies in the saliva/plasma concentration ratios have been reported, especially in single dose studies (e.g. theophylline).
If saliva is to be used in therapeutic monitoring then the saliva to plasma concentration ratio should be constant over a wide plasma concentration range. For the anticonvulsant drugs Phenytoin, primidone, ethosuximide and carbamazepine, the existence of a consistent correlation between their concentrations in saliva and plasma has been established under steady state conditions. Saliva concentrations appear to be the same as the protein unbound concentrations in plasma, and the S/P ratio is not influenced by concurrent therapy with other anticonvulsants. For phenobarbitone, a larger variability in the S/P ratio has been observed, probably due to the fact that its salivary concentration is dependent on salivary pH.
For digoxin, a substantial interindividual variation in the S/P ratio has been found in patients on long-term therapy, which makes the use of saliva for digoxin monitoring doubtful. Due to the substantial inter- and intraindividual variation in the S/P ratio of procainamide in patients on long-term therapy it is impossible to predict its plasma concentration on the basis of saliva concentrations. However, clinically, the saliva concentration of procainamide may be relevant, since this concentration and the pharmacological effect are correlated. The value of salivary drug concentration measurements in monitoring quinidine therapy is still unclear, due to the lack of information concerning the salivary excretion of quinidine in patients on long-term therapy.
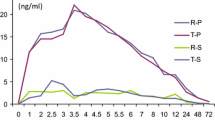
Salivary concentration measurements are of limited value in monitoring theophylline therapy since this drug shows a strong time-dependency in the S/P ratio, resulting in large inter- and intraindividual variations especially during the absorption phase in single oral and rectal dose studies. A substantial interindividual variability also occurs in the S/P ratio with lithium. However, within an individual subject this value remains constant over a long period. Therefore once the S/P ratio has been established, measurement of saliva concentrations provides all information necessary for rational dosage adjustment in lithium therapy. Due to the lack of information concerning the salivary excretion of salicylate under steady state conditions and in the therapeutic concentration range, the value of saliva salicylate concentrations in therapeutic monitoring remains unclear.
For antipyrine, S/P values in the range of about I are usually observed. Therefore, saliva data permit the calculation of pharmacokinetic parameters like plasma half-life, apparent volume of distribution and total body clearance in antipyrine studies. That salivary drug concentration measurements may be a useful approach to acetylation phenotyping has been illustrated with drugs like sulphasalazine and isoniazid. The S/P ratio for a number of other drugs has been summarised but these are probably not of great value for therapeutic drug monitoring purposes.
Similar content being viewed by others
References
Allen, M.A.; Wrenn. J.M.; Putney, J.W. and Borzelleca. J.F.: A study of the mechanism of transport of diphenylhydantoin in the rat submaxillary gland in vitro. Journal of Pharmacology and Experimental Therapeutics 197: 408–413 (1976).
Amberson, W.R. and Hober, R.: The permeability of mammalian salivary glands for organic non-electrolytes. Journal of Cellular and Comparative Physiology 2: 201–221 (1932).
Amdisen. A.: Serum level monitoring and clinical pharmacokinetics of lithium. Clinical Pharmacokinetics 2: 73–92 (1977).
Aucamp, A.K. and Hundt. H.K.L.: Study of carbamazepine and its epoxy and hydroxy metabolites in serum and saliva of male and female epileptic patients. XIIIth Congress of the International League Against Epilepsy. Amsterdam. 9–12 September (1977).
Avery, G.S. (Ed): Drug Treatment, p. 888–896 (ADIS Press. Sydney; Lea and Febiger. Philadelphia; Churchill Livingstone. Edinburgh 1976).
Bartels. H.; Oldigs. H.-D. and Gunther. E.: Use of saliva in monitoring carbamazepine medication in epileptic children. European Journal of Pediatrics 126; 37–44 (1977).
Barth. N.; Alvan, G.; Borga. O. and Sjoqvist, F.: Two-fold interindividual variation in plasma protein binding of Phenytoin in patients with epilepsy. Clinical Pharmacokinetics 1: 444–452 (1976).
Bates. T.R.; Blumenthal, H.P. and Pieniaszek, H.J.: Time course of free and N4-acetylated sulfapyridine concentrations in the plasma and saliva of man after sulfasalazine (salicylazosulfapyridine) administration: preliminary findings. Research Communications in Chemical Pathology and Pharmacology 15: 183–189 (1976).
Bender. I.B.; Pressman. R.S. and Tashman. S.G.: Studies on excretion of antibiotics in human saliva. I. Penicillin and streptomycin. The Journal of the American Dental Association 46; 164–170 (1953).
Bochner, F.; Hooper. W.D.; Sutherland, J.M.; Eadie. M.J. and Tyrer, J.H.: Diphenylhydantoin concentrations in saliva. Archives of Neurology 31: 57–59 (1974).
Borga. O.; Odar Cederlof, I.; Ringberger, V.A. and Morlin, A.: Protein-binding of salicylate in uremic and normal plasma. Clinical Pharmacology and Therapeutics 20: 464–475 (1976).
Borzelleca. J.F. and Cherrick. H.M.: The excretion of drugs in saliva. Antibiotics. Journal of Oral Therapeutics and Pharmacology 2: 180–187 (1965).
Borzelleca. J.F. and Putney, J.W.: A model for the movement of salicylate across the parotid epithelium. Journal of Pharmacology and Experimental Therapeutics 174: 527–534 (1970).
Boxenbaum, H.G.; Berkersky. I.; Mattaliano, V. and Kaplan, S.A.: Plasma and salivary concentrations of isoniazid in man: preliminary findings in two slow acetylator subjects. Journal of Pharmacokinetics and Biopharmaceutics 3; 443–456 (1975).
Breimer, D.D.: Pharmacokinetic and biopharmaceutical aspects of hypnotic drug therapy; in Gouveia. Tognoni and Van der Kleijn (Eds) Clinical Pharmacy and Clinical Pharmacology, p. 17–42 (Elsevier/North-Holland, Amsterdam 1976).
Burgen. A.S.V.: The secretion of non-electrolytes in the parotid saliva. Journal of Cellular Physiology 48: 113–138 (1956).
Burgen, A.S.V.: The secretion of lithium in saliva. Canadian Journal of Biochemical Physiology 36: 409–411 (1958).
Chang, K. and Chiou, W.L.: Interactions between drugs and saliva-stimulating parafilm and their implications in measurements of saliva drug levels. Research Communications in Chemical Pathology and Pharmacology 13: 357–360 (1976).
Chang. R.L.; Wood. A.W.; Dixon, W.R.; Conney, A.H.; Anderson. K.E.; Eiseman. J. and Alvares, A.P.: Antipyrine: radioimmunoassay in plasma and saliva following administration of a high dose and a low dose. Clinical Pharmacology and Therapeutics 20: 219–226 (1976).
Cook, C.E.; Amerson. E.; Poole. W.K.; Lesser, P. and O’Tuama. L.: Phenytoin and phenobarbital concentrations in saliva and plasma measured by radioimmunoassay. Clinical Pharmacology and Therapeutics 18: 742–747 (1976).
Conn. H.L. and Luchi, R.J.: Some cellular and metabolic considerations relating to the action of quinidine as a prototype anti-arrhythmic agent. American Journal of Medicine 37: 658–699 (1964).
Das. K.M. and Dubin. R.: Clinical pharmacokinetics of sulphasalazine. Clinical Pharmacokinetics 1: 406–425 (1976).
Das. K.M. and Eastwood, M.A.: Acetylation polymorphism of sulfapyridine in patients with ulcerative colitis and Crohn’s disease. Clinical Pharmacology and Therapeutics 18: 514–520 (1975).
Davis. R.E.; Hartman. C.W. and Fincher, J.H.: Dialysis of ephedrine and pentobarbital from whole human saliva and stimulated saliva. Journal of Pharmaceutical Sciences 60: 429–432 (1971).
De Blaey. C.J. and De Boer. A.G.: Kwaliteitsbeheersing van aminofylline zetpillen. Pharmaceutisch Weekblad 111: 1216–1221 (1976).
De Boer. A.G.; Pronk, J. and Breimer, D.D.: Unpublished investigations (1977).
Dvorchik. B.H. and Vesell. E.S.: Pharmacokinetic interpretation of data gathered during therapeutic drug monitoring. Clinical Chemistry 22: 868–878 (1976).
Eadie. M.J.: Plasma level monitoring of anticonvulsants. Clinical Pharmacokinetics 1: 52–66 (1976).
Feller. K.; Le Petit. G. and Marx, U.: Zur Verteilung von Pharmaka zwischen Speichel und Blutplasma. Die Pharmazie 31: 745–746 (1976).
Fraser, H.S.; Mucklow, J.C.; Murray, S. and Davies, D.S.: Assessment of antipyrine kinetics by measurement in saliva. British Journal of Clinical Pharmacology 3: 321–325 (1976).
Galeazzi, R.L.; Benet, L.Z. and Sheiner, L.B.: Relationship between the pharmacokinetics and pharmacodynamics of procainamide. Clinical Pharmacology and Therapeutics 20: 278–289 (1976).
Glynn. J.P. and Bastain, W.: Salivary excretion of paracetamol in man. Journal of Pharmacy and Pharmacology 25: 420–421 (1973).
Graham. G. and Rowland. M.: Application of salivary salicylate data to biopharmaceutical studies of salicylates. Journal of Pharmaceutical Sciences 61: 1219–1222 (1972).
Groth. U.; Prellwitz. W. and Jahnchen, E.: Estimation of pharmacokinetic parameters of lithium from saliva and urine. Clinical Pharmacology and Therapeutics 16: 490–498 (1974).
Gruneisen. A. and Witzgall. H.: Abhangigkeit der Speichelkonzentration korperfremder Stoffe von der Blutwasserkonzentration an dem Model von funf Sulfonamiden. European Journal of Clinical Pharmacology 7: 77–79 (1974).
Hepner. G.W. and Vesell, E.S.: Aminopyrine disposition: studies on breath, saliva and urine of normal subjects and patients with liver disease. Clinical Pharmacology and Therapeutics 20: 654–660 (1976).
Hoeprich. P.D. and Warshauer. D.M.: Entry of four tetracyclines in saliva and tears. Antimicrobial Agents and Chemotherapy 5: 330–336 (1974).
Horning. M.G.; Brown. L.; Mowlin, J.; Lertratanangkoon. K.; Kellaway, P. and Zion, T.E.: Use of saliva in therapeutic drug monitoring. Clinical Chemistry 23: 157–164 (1977).
Huffman, D.H.: Relationship between digoxin concentrations in serum and saliva. Clinical Pharmacology and Therapeutics 17: 310–312 (1975).
Hvidberg. E.F. and Dam, M.: Clinical pharmacokinetics of anticonvulsants. Clinical pharmacokinetics 1: 161–188 (1976).
lisalo, E.: Clinical Pharmacokinetics of digoxin. Clinical Pharmacokinetics 2: 1–16 (1977).
Inaba, T. and Kalow, W.: Salivary excretion of amobarbital in man. Clinical Pharmacology and Therapeutics 18: 558–562 (1975).
Jaffe. J.M.; Strum. J.D.; Martineau, P.C. and Collaizzi, J.L.: Relationship between quinidine plasma and saliva levels in humans. Journal of Pharmaceutical Sciences 64: 2028–2029 (1975).
Johnson, G.F.; Dechtiaruk, W.A. and Solomon. H.M.: Gaschromatographic determination of theophylline in human serum and saliva. Clinical Chemistry 21: 144–147 (1975).
Joubert. P.H.: Aucamp. B.N. and Muller, F.O.; Digoxin concentrations in serum and saliva: relationship to E.C.G. changes and dosage in healthy volunteers. British Journal of Clinical Pharmacology 3: 1053–1056 (1976a).
Joubert. PH.; Muller, F.O. and Aucamp. B.N.: Salivary digoxin concentrations. British Journal of Clinical Pharmacology 3: 673–674 (1976b).
Jusko, W.J.; Gerbracht. L.; Golden, L.H. and Koup. J.R.: Digoxin concentrations in serum and saliva. Research Communications in Chemical Pathology and Pharmacology 10: 189–192 (1975).
Killmann. S.A. and Thaysen. J.H.: The permeability of the human parotid gland to a series of sulfonamide compounds, para-amino hippurate and inulin. Scandinavian Journal of Clinical Laboratory Investigation 7: 86–91 (1955).
Knoebel. L.K.: Secretion and action of digestive juices, absorption; in Selkurt (Ed) Psysiology p. 571–602 (Little Brown., Boston. 1966).
Knop. H.J.: Kalafusz, R.; Knols. A.J.F. and Van der Kleijn. E.: Preliminary report on the saliva/plasma ratio of theophylline after administration of theophylline derivatives in suppositories. Pharmaceutisch Weekblad 110: 1297–1299 (1975).
Koch-Weser. J.: Serum procainamide levels as therapeutic guides. Clinical Pharmacokinetics 2: 389–402 (1977).
Koch-Weser. J.M. and Klein. S.W.: Procainamide dosage schedules, piasma concentrations and clinical effects. Journal of the American Medical Association 215: 1454–1460 (1971).
Koup. J.R.; Jusko, W.J. and Goldfarb, A.L.: pH-dependent secretion of procainamide into saliva. Journal of Pharmaceutical Sciences 64: 2008–2010 (1975).
Koysooko, R.; Ellis, E.F. and Levy, G.: Relationship between theophylline concentration in plasma and saliva of man. Clinical Pharmacology and Therapeutics 15: 454–460 (1974).
Lange. W.E.; Floriddia. D.G. and Pruyn, F.J.: In vitro binding of salicylates to saliva proteins. Journal of Pharmaceutical Sciences 58: 771–773 (1969).
Levy. G. and Lampman, T.: Relationship between pH of saliva and pH of urine. Journal of Pharmaceutical Sciences 64: 890 (1975).
Levy. G.; Tsuchiya, T. and Amsel, L.P.: Limited capacity for salicylphenolic glucuronide formation and its effects on the kinetics of salicylate elimination in man. Clinical Pharmacology and Therapeutics 13: 258–268 (1972).
Levy. G.; Ellis. E.F. and Koysooko. R.: Indirect plasma-theophylline monitoring in asthmatic children by determination of theophylline concentration in saliva. Pediatrics 53: 873–876 (1974).
Lunde. P.K.M.; Frislid. K. and Hansteen. V.: Disease and acetylation polymorphism. Clinical Pharmacokinetics 2: 182–197 (1977).
Mandel. I.W.: Relation of saliva and plaque to caries. Journal of Dental Research 53: 246–266 (1974).
Martindale: The Extra Pharmacopoeia; Blacow and Wade (Eds) 26th ed. p. XX–XXII (Pharmaceutical Press., London, 1972).
Matin. S.B.: Wan. S.H. and Karam, JH.: Pharmacokinetics of tolbutamide: prediction by concentration in saliva. Clinical Pharmacology and Therapeutics 16: 1052–1058 (1974).
Neu. C.; Dimascio, A. and Williams. D.: Saliva lithium levels: clinical applications. American Journal of Psychiatry 132: 66 (1975).
Odar-Cederlof. I. and Borga. O.: Kinetics of diphenylhydantoin in uraemic patients: Consequences of decreased protein binding. European Journal of Clinical Pharmacology 7: 31–37 (1974).
Paxton. J.W.; Whiting, B. and Stephen, K.W.: Phenytoin concentrations in mixed, parotid and submandibular saliva and serum measured by radioimmunoassay. British Journal of Clinical Pharmacology 4: 185–191 (1977).
Rane, A. and Wilson. J.T.; Plasma level monitoring of diphenylhydantoin and carbamazepine in the pediatric patient; in Gouveia, Tognoni and Van der Kleijn (Eds) Clinical Pharmacy and Clinical Pharmacology p. 295–302 (Elsevier/North-Holland., Amsterdam 1976).
Rasmussen. F.: Salivary excretion of sulphonamides and barbiturates by cows and goats. Acta Pharmacologica et Toxicologica 21: 11–19 (1964).
Reynolds. F.; Ziroyanis. P.N.; Jones, N.F. and Smith. S.E.: Salivary Phenytoin concentrations in epilepsy and in chronic renal failure. Lancet 2: 384–386 (1976).
Schmidt-Nielsen. B. The pH in parotid and mandibular saliva. Acta Phsyiologica Scandinavica 11: 104–110 (1946).
Schmidt. D. and Kupferberg. H.J.: Diphenylhydantoin, phenobarbital, and primidone in saliva, plasma and cerebrospinal fluid. Epilepsia 16: 735–741 (1975).
Schneyer, L.H.; Young, J.A. and Schneyer. C.A.: Salivary secretion of electrolytes. Physiological Reviews 52: 720–777 (1972).
Shah. V.P. and Riegelman, S.: G.L.C. determination of theophylline in biological fluids. Journal of Pharmaceutical Sciences 63: 1283–1285 (1974).
Shimizu. M. and Smith. D.F.; Salivary and urinary lithium clearance while recumbent and upright. Clinical Pharmacology and Therapeutics 21: 212–215 (1977).
Shopsin. B.; Gershon, S. and Pinckney, L.: The secretion of lithium in human mixed saliva: effects of ingested lithium on electrolyte distribution in saliva and serum. International Pharmacopsychiatry 2: 148–169 (1969).
Smith. T.W.; Butler. V.P. and Haber. E.: Determination of therapeutic and toxic serum digoxin concentrations by radioimmunoassay. New England Journal of Medicine 281: 1212–1216 (1969).
Smith. T.W. and Haber. E.: Clinical value of the radioimmunoassay of the digitalis glycosides. Pharmacological Reviews 25: 219–228 (1973).
Spring. K.R. and Spirtes. M.A.: Salivary excretion of lithium. I. Human parotid and submaxillary secretions. Journal of Dental Research 48: 546–549 (1969a).
Spring. K.R. and Spirtes. M.A.: Salivary excretion of lithium. II. Functional anaylsis. Journal of Dental Research 48: 550–554 (1969b).
Stephen, K.W. and Speirs, C.F.: Methods for collecting individual components of mixed saliva. The relevance to clinical pharmacology. British Journal of Clinical Pharmacology 3: 315–319 (1976).
Troupin. A.S. and Friel. P.: Anticonvulsant level in saliva, serum and cerebrospinal fluid. Epilepsia 16: 223–227 (1975).
Tuberculosis Chemotherapy Centre, Madras: A controlled comparison of two fully supervised once-weekly regimens in the treatment of newly diagnosed pulmonary tuberculosis. Tubercle 54: 23–45 (1973).
Van Boxtel. C.J.: Wilson. J.F.; Lindgren. S. and Sjoqvist. F.: Comparison of the half-life of antipyrine in plasma, whole blood, and saliva of man. European Journal of Clinical Pharmacology 9: 327–332 (1976).
Van der Vijgh. W.J.F.: Comparison of salivary digoxin concentrations with plasma levels in man. Netherlands Journal of Medicine 18: 269–272 (1975).
Vesell. E.S.; Passananti. G.T.; Glenwright. A. and Dvorchik, B.H.: Studies on the disposition of antipyrine, aminopyrine and phenacetin using plasma, saliva and urine. Clinical Pharmacology and Therapeutics 18: 259–272 (1975).
Wallace. S.M.: Shah. V.P. and Riegelman. S.: GLC analysis of acelazolamide in blood plasma and saliva following oral administration to normal subjects. Journal of Pharmaceutical Sciences 66: 527–530 (1977).
Weintraub, M.: Interpretation of the serum digoxin concentration. Clinical Pharmacokinetics 2: 205–219 (1977).
Welch. R.M.; De Angelis. R.L.; Wingfield, M. and Farmer. T.W.: Elimination of antipyrine from saliva as a measure of metabolism in man. Clinical Pharmacology and Therapeutics 18: 249–258 (1975).
Westenberg. H.G.M.; De Zeeuw. R.A.; Van der Kleijn. E. and Oei. T.T.: Relationship between carbamazepine concentrations in plasma and saliva in man as determined by liquid chromatography. Clinica Chimica Acta 79: 155–161 (1977).
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Danhof, M., Breimer, D.D. Therapeutic Drug Monitoring in Saliva. Clin Pharmacokinet 3, 39–57 (1978). https://doi.org/10.2165/00003088-197803010-00003
Published:
Issue Date:
DOI: https://doi.org/10.2165/00003088-197803010-00003