Abstract
Objectives
The impact of long COVID among persons hospitalized and discharged home is unknown. We aimed to (1) report the prevalence of long COVID in persons hospitalized for COVID-19 and discharged home; (2) estimate the prevalence of physical, sensory, and psychological/mental health impairments; and (3) explore associated factors.
Methods
We conducted a telephone survey of adult residents in Laval, Quebec, who were discharged home ≥ 2 months post-hospitalization for COVID-19. Participants responded to a standard questionnaire regarding persistent symptoms. We calculated the prevalence of long COVID and of persistent types of symptoms and evaluated associated factors using bivariate analysis and multivariable logistic regression.
Results
In our sample (n = 398), 70% reported physical symptoms, 58% psychological problems, and 16% sensory impairments. 31.5% reported being troubled by persistent symptoms (long COVID). Factors associated with long COVID were a greater number of symptoms (odds ratio (OR) = 1.97, 95% confidence interval (CI) = 1.69–2.28) and increased hospital stay (OR = 1.03, 95% CI = 1.01–1.06). Other factors associated with physical and psychological symptoms were female sex (OR = 2.17, 95% CI = 1.27–3.71 and OR = 2.06, 95% CI = 1.25–3.39; respectively), higher education level (OR = 2.10, 95% CI = 1.20–3.68 and OR = 2.43, 95% CI = 1.44–4.14; respectively), and obesity (OR = 1.95, 95% CI = 1.15–3.34 and OR = 1.70, 95% CI = 1.05–2.77; respectively).
Conclusion
In this population-based study of persons hospitalized for COVID-19 and discharged home, nearly one third were troubled by symptoms for 2 months or more post-discharge. There was a high proportion with persistent physical and psychological/mental health symptoms. Further research will assess the specific needs of these patients to inform health policy makers on service requirements for these persons.
Résumé
Objectifs
L’impact de la présence de la COVID longue chez les personnes hospitalisées et lors de leur congé de l’hôpital est inconnu. Dans le cadre de cette étude, nous visions à 1) rapporter la prévalence de la présence de la COVID longue chez les personnes hospitalisées en raison de la COVID-19 et lors de leur congé à la maison; 2) estimer la prévalence des déficiences physiques, sensorielles et psychologiques/cognitives; et 3) explorer les facteurs associés.
Méthodes
Nous avons mené une enquête téléphonique auprès des résidents adultes de Laval, au Québec, qui ont reçu leur congé de l’hôpital plus de deux mois après avoir été hospitalisés en raison de la COVID-19. Les participants ont répondu à un questionnaire standard concernant leurs symptômes résiduels. Nous avons calculé la prévalence de la COVID longue et le type de symptômes résiduels et nous avons évalué les facteurs associés en utilisant une analyse bivariée et une régression logistique multivariable.
Résultats
Dans notre échantillon (n=398), 70 % ont déclaré des symptômes physiques, 58 % des problèmes psychologiques et 16 % des déficiences sensorielles. 31,5 % ont déclaré être perturbés par des symptômes résiduels (COVID longue). Les facteurs associés à la COVID longue étaient un plus grand nombre de symptômes (Rapport de cotes (OR)=1,97, intervalle de confiance à 95% (IC)=1,69-2,28) et une durée d’hospitalisation plus longue (OR=1,03, IC 95%=1,01-1,06). Les autres facteurs associés aux symptômes physiques et psychologiques étaient le sexe féminin (OR=2,17, IC 95%=1,27-3,71 et OR=2,06, IC 95%=1,25-3,39; respectivement), un niveau d’éducation plus élevé (OR=2,10, IC 95%=1,20-3,68 et OR=2,43, IC 95%=1,44-4,14; respectivement) et l’obésité (OR=1,95, IC 95%=1,15-3,34 et OR=1,70, IC 95%=1,05-2,77; respectivement).
Conclusion
Dans cette étude effectuée sur une population de personnes hospitalisées pour la COVID-19 et lors de leur congé de l’hôpital, près d’un tiers ont été perturbées par la présence de symptômes résiduels présents pendant 2 mois ou plus après leur congé. Une forte proportion d’entre elles présentait des symptômes physiques et psychologiques/enjeux de santé mentale persistants. Des recherches futures permettront d’évaluer les besoins spécifiques de ces individus afin d’informer les décideurs politiques en santé de leurs besoins afin d’offrir des services adaptés à leur condition.
Similar content being viewed by others
Avoid common mistakes on your manuscript.
Introduction
As we enter the third year of the COVID-19 epidemic, it is becoming more frequent to hear of long-term sequelae experienced by many who were infected (Nalbandian et al., 2021). The Centers for Disease Control and Prevention in the United States (CDC) describes long COVID as a condition that has a range of symptoms that can last weeks or months after infection and can worsen with physical or mental activity (Phillips & Williams, 2021). Several definitions for long COVID are suggested in terms of time post-infection with lasting symptoms. The World Health Organization favours 12 weeks (WHO, 2021), the CDC suggests 4 weeks (CDC, 2021), while 2 months has also been proposed (Brodin, 2021).
A systematic review of sequelae at least 4 weeks post-acute COVID-19 infection reported pulmonary, hematologic, cardiovascular, neuropsychiatric, renal, endocrine, gastrointestinal, and dermatologic effects (Nalbandian et al., 2021). Another review described more than 100 long COVID–related symptoms, with the most prevalent being fatigue, pain or discomfort, sleep disturbances, shortness of breath, and anxiety (Domingo et al., 2021). Seven to 9 months post COVID-19 diagnosis, 39% of outpatients reported residual symptoms, with fatigue being the most common, followed by loss of taste or smell, dyspnea, and headache (Nehme et al., 2021). Seeßle et al. (2021) found that after 12 months, only 23% of patients were completely symptom-free (Seeßle et al., 2021).
Patients hospitalized for COVID-19 may be at increased risk for long-term symptoms. Nearly a third of 47,780 individuals discharged from hospital in Britain were readmitted and more than 10% died after discharge (Ayoubkhani et al., 2021). Among those hospitalized and evaluated weeks or months post-discharge, fatigue was the most common symptom; other symptoms included dyspnea, weakness, psychological distress, sleep disturbance, and musculoskeletal symptoms. Patients who were admitted to the intensive care unit (ICU) and women were more likely to have persistent symptoms (Halpin et al., 2021; Huang et al., 2021; Karaarslan et al., 2022).
Most studies on long-term effects following hospitalization for COVID-19 were based in one hospital. We studied residents of an entire city who were hospitalized (at various hospitals) for COVID-19 and discharged home. Participants were interviewed at least 2 months after diagnosis with COVID-19. The rationale was to use a population-based study so that the health authority could plan, prepare, and provide services to persons with long COVID. Specific objectives were to (1) report the prevalence of long COVID in a population-based sample of persons hospitalized with a primary diagnosis of COVID-19 and discharged home; (2) estimate the prevalence of physical, sensory, and psychological/mental health impairments that persist post COVID-19 infection; and (3) determine factors (clinical, sociodemographic, and length of time since diagnosis and discharge) associated with long COVID.
Methods
We used a cross-sectional population survey design. The population included all adult residents of Laval, Quebec, Canada (population approximately 450,000) who were hospitalized for COVID-19 between March 15, 2020 and May 30, 2021 and subsequently discharged home. Those discharged to a facility such as a long-term care home were excluded. Participants were recruited at ≥ 2 months after diagnosis. We received ethics approval from the Comité scientifique et d’éthique de la recherche de CISSS Laval. Contact information for eligible participants was obtained from the Public Health Department of the City of Laval. We sent a recruitment pamphlet by email or by post to explain the objectives and procedures of the study to all potential participants. Research assistants then contacted potential participants by telephone to ask whether they would agree to participate and, if they provided verbal consent, proceeded to conduct the interview.
The interview consisted of the administration of three questionnaires (developed and validated in Europe) as well as several sociodemographic and clinical questions. The questionnaires included the Newcastle Post-COVID Syndrome Follow Up Screening Questionnaire (Burns, 2020), COVID-19 Yorkshire Rehabilitation Scale (O’Connor et al., 2022), and the COVID-19 Rehabilitation Needs Questionnaire (Lemhöfer et al., 2021). In this paper, we describe the results of the Newcastle Post-COVID Syndrome Follow Up Screening Questionnaire. This questionnaire consists of 14 questions that screen for possible long-term symptoms following COVID-19 infection with a goal of identifying patients who may require multi-disciplinary assessment and intervention. Participants are asked to rate how they feel now with respect to how they were prior to COVID-19 infection. The questionnaire was translated into French and was administered in either English or French, according to the participant’s preference. The primary outcome is presence of long COVID, defined by the response to the following question: “Have you made a full recovery or are you still troubled by symptoms?” Other outcomes include categorization of reported symptoms: breathlessness, fatigue, cough, palpitations, weakness, myalgia, anosmia, loss of sense of taste, sleep disturbance, nightmares/flashbacks, low mood, anxious/worry, and weight loss. We created three categories by grouping symptoms as physical health symptoms (at least one of the following: breathlessness, fatigue, cough, palpitations, weakness, myalgia, sleep disturbance, weight loss), sensory problems (at least one of the following: loss of smell and/or taste), and psychological/mental health symptoms (at least one of the following: palpitations, sleep disturbance, nightmares, low mood, anxiety, weight loss). In addition, sociodemographic and COVID-related information were collected.
Based on previous accounts on factors associated with both mortality and morbidity related to COVID-19 (Halpin et al., 2021; Huang et al., 2021; Jaspard et al., 2021; Karaarslan et al., 2022; Nielsen et al., 2021; Taylor et al., 2021), that included sex, older age, obesity, comorbid conditions, disease severity (being admitted to ICU and length of hospital stay), and length of time since diagnosis, we hypothesized that similar factors may be associated with long COVID. In addition, civil status, education level, and employment status were considered as they are often associated with chronic disease (Oates et al., 2017). Thus, we investigated the following factors: sex, age, time since diagnosis, employment status pre-infection, civil status, education, body mass index (BMI), intensive care unit admission, level of respiratory support, length of hospital stay, and time since diagnosis. We also explored whether being unvaccinated was associated with long COVID.
All analyses were performed using SAS, version 9.4 (SAS Institute Inc.). Statistical analysis consisted of a description of the sample, prevalence of long COVID, and prevalence of various symptoms. We describe the prevalence of each of the symptoms as well as symptom categories: physical symptoms, sensory symptoms, and psychological/mental health–related symptoms. Finally, we evaluated factors associated with long COVID and symptom categories using bivariate analysis and multivariable logistic regression models. We constructed multivariable models to explore independent factors associated with having long COVID as well as factors associated with the category of symptoms: physical, psychological/mental health, and sensory. We included all factors described above in the model except for level of respiratory support since this was highly correlated with intensive care unit admission (the latter being included in the model). We also performed stratified analyses to explore effect modification based on sex. It is important to note that the intent was to explore associated factors and not to develop a prediction model for long COVID. We did not have access to important variables for such a prediction model, such as immunologic profiles and other comorbidities and certain lifestyle factors (e.g., smoking).
Results
There were 1124 persons who were eligible to participate; of these, 314 could not be reached (e.g., wrong phone number, no answer) and among the 810 who were contacted, 398 consented to participate in the study, for a response rate of 35.4% (398/1124) (Figure 1).
We compared participants to both groups who did not participate (those who refused, and those who could not be reached). There were no differences in sex distribution; however, participants were on average younger (61.1 ± 16.5) than both the group who refused (64.8 ± 19.0) (p = 0.003) and those who could not be reached (66.6 ± 18.1) (p = 0.001). Participants also had a shorter mean length of stay in hospital (12.0 ± 18.4 days) compared to both the group who refused (17.5 ± 30.2) (p = 0.002) and the group not reached (18.2 ± 23.0) (p = 0.001). The time between discharge and the phone call also differed, with those who participated responding to the call an average of 262 (sd = 138) days after hospital discharge, compared to those who could not be reached (283 days; sd = 131; p = 0.042).
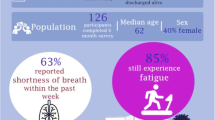
The sample was 45% female, with a mean age of 61.1 years (sd = 16.5) and mean BMI of 29.9 (sd = 7.8). The mean length of stay in hospital was 12.0 days (sd = 18.4) and the median length of stay was 6 days. Mean time between COVID-19 diagnosis and the telephone interview was 281.4 days (sd = 140.4; range: 69–587); median time was 232 days. At the time of interview, 72.6% were more than six months and 27.9% were more than a year post-diagnosis. Ninety-three participants (23.4%) had been admitted to the ICU. There were a total of 27 (6.8%) who were intubated. A description of the sample is presented in Table 1.
Among our sample, 70.5% revealed that they still had physical symptoms, 58.1% still had psychological/mental health–related symptoms, and 16.4% still had sensory symptoms. Physical symptoms were predominant: 53% reported fatigue, 42% breathlessness, and 38% weakness that limited activities. Other symptoms cited were hair loss (n = 22; 5.5%), problems with memory (n = 14; 3.5%) and concentration (n = 14; 3.5%), headache (n = 14; 3.5%), numbness (n = 12; 3%), and dizziness (n = 11; 2.8%). The frequency of each of the symptoms listed in the Newcastle questionnaire is presented in Table 2. Among those with long COVID, more than 50% reported breathlessness, fatigue, weakness, myalgia, low mood, weight loss, and anxiety whereas among those who reported a full recovery, 35% reported fatigue and less than 25% reported each of the other symptoms. A greater percentage of participants in the long COVID group reported each symptom.
Although only 104 (26.3%) claimed to have no symptoms whatsoever, over two thirds of participants (n = 270; 68.5%) said that they had recovered and were no longer troubled by symptoms and on average, recovery occurred within 2 months. On the other hand, 124 (31.5%) reported that they were “troubled by persisting symptoms” (long COVID cases); they were more likely to have more than a high school education level, be obese (BMI ≥ 30), have been in ICU, have required a higher level of respiratory support, and have had a longer stay in hospital (Table 3). The time since COVID diagnosis for the long COVID group was on average 281.6 days: 74.8% were ≥ 6 months and 28.5% ≥ 12 months.
In order to compare our definition of long COVID to that of the WHO, we calculated the proportion at 12 weeks for those troubled by persisting symptoms which was 31.8%. We also calculated the proportion complaining of any symptom which was 73.7% at both 8 weeks and 12 weeks.
Bivariate analysis for each of the three symptom categories (physical, psychological/mental health, and sensory) indicated the following. Females were more likely than males to have physical (p = 0.02) and sensory (p = 0.03) symptoms. Those with higher education were more likely to have physical (p = 0.02) and psychological/mental health (p = 0.01) symptoms. Individuals who were obese had a greater number of physical symptoms (p = 0.01) and those who were admitted to ICU were more likely to have at least one physical symptom (p = 0.03) and psychological/mental health symptom (p = 0.03).
Multivariable logistic regression models for five outcomes (long COVID; physical symptoms; psychological/mental health–related symptoms; sensory symptoms; any symptom) are presented in Table 4. Having long COVID was associated with longer stay in hospital and having a greater number of symptoms as well as having been working pre-COVID diagnosis. Females, those having higher levels of education, and those who were obese were more likely to have physical, psychological/mental health symptoms, or any symptom; and longer hospital stay was associated with both physical and psychological/mental health–related symptoms. Stratified analyses based on sex showed no evidence of effect modification. For example, not working pre-diagnosis was associated with not having long COVID in both females (OR = 0.2, 95% CI = 0.1, 0.8) and males (OR = 0.2, 95% CI = 0.1, 0.7). Having more symptoms was associated with having long COVID in both females (OR = 2.1, 95% CI = 1.6, 2.7) and males (OR = 1.9, 95% CI = 1.6, 2.3).
Discussion
In this population-based study on hospitalized patients who were discharged home following COVID-19 infection, we found that 31.5% were troubled by persisting symptoms (long COVID), with physical symptoms such as fatigue and weakness being the most prevalent ones. Factors associated with persistent symptoms were having a greater number of symptoms, an increased length of stay in hospital, female sex, and higher educational level.
The 31.5% prevalence of long COVID among patients who were hospitalized for COVID and discharged home indicates that a substantial proportion of them reported symptoms that persist past 2 months. For almost three quarters of those with long COVID, symptoms persisted beyond 6 months. It must be noted that this represents the response to those who said that they were still troubled by symptoms, although there were more who reported fatigue (53%), breathlessness (42%), and weakness that limited their function (38%) more than before they had COVID. Our percentages are actually higher than those in a French COMEBAC study (The Writing Committee for the COMEBAC Study Group, 2021), and are similar to those in a report from China (Huang et al., 2021). It is interesting that even though persons claimed having a full recovery, they still reported having symptoms, although the percentages were significantly lower than among those with long COVID. There were nearly three quarters of respondents who still reported any symptom. Over a third of persons who reported full recovery claimed to still have fatigue. This is a substantial number; however, based on their response, we did not consider them in our primary outcome of long COVID, and considered them as having made a full recovery and no longer being troubled by symptoms. Although we cannot be certain, they may correspond to a subset of persons with lower perceived need for services who believe that the symptoms will go away (Taber et al., 2015).
From a health services and policy perspective, the fact that nearly one third of patients were troubled by their symptoms many months after infection indicates the need for follow-up and management of these symptoms after hospital discharge, particularly for those with physical or psychological/mental health–related symptoms. Another implication of our results is the importance of controlling the spread of COVID-19 in order to prevent long COVID and reduce its long-term burden on the health care system. In our bivariate analyses, severity of disease (ICU admission and level of respiratory support) was associated with long COVID. However, in the multivariable models, only duration of hospitalization was independently associated with long COVID and with persistent physical and psychological/mental health symptoms. Although length of stay is not necessarily indicative of disease severity for many types of hospital admissions (Iezzoni et al., 1996; Hicks & Kammerling, 1993), it may be more correlated with severity in those who survived COVID and were discharged home (i.e., not to a convalescent home, rehabilitation centre, or seniors residence). Thus, survivors of COVID who were discharged home but had a lengthier course in hospital appear to be at higher risk for developing long COVID.
Female sex was associated with having persistent physical and psychological/mental health symptoms. This is in line with some of the recent reports on long COVID that also found female predominance (Ganesh et al., 2021; Karaarslan et al., 2022; Sudre et al., 2021; Thompson et al., 2021). We found that obesity was associated with long COVID which is consistent with findings by others (Sudre et al., 2021; Thompson et al., 2021). We did not find that older age was associated with long COVID, unlike some reports (Sudre et al., 2021; Thompson et al., 2021); however, our study was done exclusively among those who had been hospitalized and was restricted to persons who were discharged home and not to a seniors residence or other facility. Having higher level of education was associated with a higher probability of physical and psychological symptoms. This is in line with the findings from Thompson et al. (2021) where not having a higher education degree was associated with a lower risk of long COVID. Although higher socioeconomic status is usually associated with better access to health care (McMaughan et al., 2020), in the context of the current pandemic, there was likely reduced access to care for non-life-threatening symptoms which affected everybody regardless of socioeconomic status.
It is noteworthy that time since COVID infection was not associated with the likelihood of long COVID; in fact, nearly three quarters of our sample were diagnosed more than 6 months prior to the interview. The fact that these symptoms did not resolve quickly indicates the need for additional health services.
A strength of our study is that it is a population-based survey of persons who had a confirmed diagnosis of COVID-19. We used a standard questionnaire and the time span is from the beginning of the pandemic until 18 months later, which includes the time since introduction of the vaccines in February/March of 2021 in the province of Quebec.
Limitations
A main limitation of this study was the response rate of 35%. Nonetheless, our sample was similar to the Canadian population hospitalized for COVID-19 whose average hospital length of stay was 11.9 days (current study: 12 days). The Canadian statistics for ICU admission among those hospitalized for COVID-19 is 27% but that includes those who died; if we consider only those who survived, the Canadian percentage is 23.1% which is similar to our percentage of 23.4% admitted to ICU among those who survived (CIHI, 2022). Furthermore, even if we were able to have included the entire eligible sample, including those who refused and those who could not be reached, and assume that they did not have any persistent symptoms, the percentage of those with long COVID would be 11%, a substantial number among hospitalized patients.
Seeking health care is associated with several factors (Andersen, 1995). These include predisposing factors (mainly sociocultural and health beliefs), enabling factors (availability of services and ability to access these), and need (perceived or evaluated need). Our main outcome was reflected by the question “Have you made a full recovery or are you still troubled by symptoms?” which focuses on the need aspect. Although many persons may still have symptoms (as reflected by our results), they may not be troubled by these and still consider that they had made a full recovery (i.e., low perceived need) (Taber et al., 2015). Nevertheless, we cannot be certain that those who responded that they made a full recovery and were no longer troubled by symptoms but still had lingering symptoms, may require services. Further, since the definition of long COVID does not include a minimum of symptoms or severity of symptoms nor is there a universally agreed-upon diagnosis for post COVID-19 condition (Government of Canada, 2022), our definition of long COVID may actually be an underestimation.
Another limitation is that we did not have information on comorbidities except for obesity. However, the questions in the Newcastle questionnaire refer to how you feel now with respect to how you were pre-COVID-19 infection. This provides a comparison to the health status pre-COVID, which is likely associated with comorbidity. We also had no information on some lifestyle factors, notably smoking which may be associated with worse outcomes (Patanavanich & Glantz, 2021).
The data on symptoms and function were based on self-report as opposed to doing a clinical examination and using objective functional measures. However, data related to dates of diagnosis, hospital admission, and discharge were obtained from the Public Health Department database. Although some of our findings are consistent with studies done elsewhere (e.g., in Europe), it is possible that our data may not be generalizable to other jurisdictions.
Conclusion
In this population-based study of patients hospitalized for COVID-19 and discharged home, we found nearly one third had long COVID, reinforcing the importance of controlling the spread of COVID-19 in order to prevent long COVID and reduce its long-term burden on the health care system. There were a high proportion with both persistent physical and psychological/mental health symptoms. There is a need to provide services to help people with long COVID manage their ongoing symptoms/problems. Models of care for persons with post-COVID-19 conditions should have professionals with various areas of expertise and ability to intervene in areas of physical health, mental health, functional disabilities, and social support (INESSS, 2022). Further research will assess the specific needs of these patients to inform health policy makers as we hope to emerge from the pandemic situation to an endemic one, albeit with many who will still require additional services or attention for their ongoing symptoms.
Contributions to knowledge
What does this study add to existing knowledge?
-
The prevalence of long COVID in a population-based sample of people who had been hospitalized for COVID-19 and discharged home (and not to a nursing home or other facility) is 31.5%.
-
Time since COVID-19 infection was not associated with the likelihood of long COVID; in fact, nearly three quarters of our sample were diagnosed more than 6 months prior to the interview, indicating that these symptoms do not resolve quickly.
-
Factors associated with persistent symptoms were: having a greater number of symptoms, an increased length of stay in hospital, female sex, and higher educational level.
What are the key implications for public health interventions, practice, or policy?
-
The fact that nearly one third of patients were troubled by their symptoms many months after COVID-19 infection indicates the need for follow-up and management of these symptoms after hospital discharge, particularly for those with physical or psychological/mental health–related symptoms.
-
There is a need to provide services to help manage persons with long COVID who are dealing with ongoing problems, perhaps by instituting more long COVID clinics that are staffed with various health care professionals who can address these problems.
Data availability
All authors have access to the data and the data are available on the CRIR platform.
References
Andersen, R. M. (1995). Revisiting the behavioral model and access to medical care: Does it matter? Journal of Health and Social Behavior, 36(1), 1–10.
Ayoubkhani, D., Khunti, K., Nafilyan, V., Maddox, T., Humberstone, B., Diamond, I., et al. (2021). Post-covid syndrome in individuals admitted to hospital with covid-19: Retrospective cohort study. British Medical Journal, 372, n693. https://doi.org/10.1136/bmj.n693
Brodin, P. (2021). Immune determinants of COVID-19 disease presentation and severity. Nature Medicine, 27(1), 28–33. https://doi.org/10.1038/s41591-020-01202-8
Burns, G. (2020). Newcastle post-COVID syndrome follow up screening questionnaire. https://postcovidsyndromebsol.nhs.uk/images/Content/Newcastle_post_Covid_Screening_Tool.pdf. Accessed 1 Feb 2022.
CDC. (2021). COVID-19. Post-COVID conditions. https://www.cdc.gov/coronavirus/2019-ncov/long-term-effects/index.html. Accessed 1 Feb 2022.
CIHI. (2022). COVID-19 hospitalization and emergency department statistics, 2021–2022. CIHI; October 2021. https://www.cihi.ca/en/covid-19-hospitalization-and-emergency-department-statistics. Accessed 1 Feb 2022.
Domingo, F. R., Waddell, L. A., Cheung, A. M., Cooper, C. L., Belcourt, V. J., Zuckermann, A. M. E., et al. (2021). Prevalence of long-term effects in individuals diagnosed with COVID-19: An updated living systematic review. medRxiv, 2021.2006.2003.21258317. https://doi.org/10.1101/2021.06.03.21258317.
Ganesh, R., Grach, S. L., Bierle, D. M., Salonen, B. R., Collins, N. M., Joshi, A. Y., et al. (2021). The female predominant persistent immune dysregulation of the post COVID syndrome: A cohort study. medRxiv, 2021.2005.2025.21257820. https://doi.org/10.1101/2021.05.25.21257820.
Government of Canada. (2022). Post COVID-19 condition (long COVID). https://www.canada.ca/en/public-health/services/diseases/2019-novel-coronavirus-infection/symptoms/post-covid-19-condition.html. Accessed 17 Jul 2022.
Halpin, S., O’Connor, R., & Sivan, M. (2021). Long COVID and chronic COVID syndromes. Journal of Medical Virology, 93(3), 1242–1243. https://doi.org/10.1002/jmv.26587
Hicks, N., & Kammerling, R. (1993). The relationship between a severity of illness indicator and mortality and length-of-stay. Health Trends, 25(2), 65–68.
Huang, C., Huang, L., Wang, Y., Li, X., Ren, L., Gu, X., et al. (2021). 6-month consequences of COVID-19 in patients discharged from hospital: A cohort study. Lancet, 397(10270), 220–232. https://doi.org/10.1016/s0140-6736(20)32656-8
Iezzoni, L. I., Shwartz, M., Ash, A. S., & Mackiernan, Y. D. (1996). Does severity explain differences in hospital length of stay for pneumonia patients? Journal of Health Services Research & Policy, 1(2), 65–76. https://doi.org/10.1177/135581969600100204
INESSS. (2022). Organization of care and services for the prevention and management of post COVID-19 (English Summary) in Organisation des soins et des services pour la prévention et la prise en charge des affections post Covid-19. https://www.inesss.qc.ca/fileadmin/doc/INESSS/COVID-19/INESSS_Post_COVID_conditions_Summary.pdf. Accessed 1 May 2022.
Jaspard, M., Sow, M. S., Juchet, S., Dienderé, E., Serra, B., Kojan, R., et al. (2021). Clinical presentation, outcomes and factors associated with mortality: A prospective study from three COVID-19 referral care centres in West Africa. International Journal of Infectious Diseases, 108, 45–52. https://doi.org/10.1016/j.ijid.2021.05.024
Karaarslan, F., Güneri, F. D., & Kardeş, S. (2022). Long COVID: Rheumatologic/musculoskeletal symptoms in hospitalized COVID-19 survivors at 3 and 6 months. Clinical Rheumatology, 41(1), 289–296. https://doi.org/10.1007/s10067-021-05942-x
Lemhöfer, C., Gutenbrunner, C., Schiller, J., Loudovici-Krug, D., Best, N., Bökel, A., et al. (2021). Assessment of rehabilitation needs in patients after COVID-19: Development of the COVID-19-rehabilitation needs survey. Journal of Rehabilitation Medicine, 53(4), jrm00183. https://doi.org/10.2340/16501977-2818
McMaughan, D. J., Oloruntoba, O., & Smith, M. L. (2020). Socioeconomic status and access to healthcare: Interrelated drivers for healthy aging. [Mini Review]. Frontiers in Public Health, 8, 231. https://doi.org/10.3389/fpubh.2020.00231
Nalbandian, A., Sehgal, K., Gupta, A., Madhavan, M. V., McGroder, C., Stevens, J. S., et al. (2021). Post-acute COVID-19 syndrome. Nature Medicine, 27(4), 601–615. https://doi.org/10.1038/s41591-021-01283-z
Nehme, M., Braillard, O., Alcoba, G., Aebischer Perone, S., Courvoisier, D., Chappuis, F., et al. (2021). COVID-19 symptoms: Longitudinal evolution and persistence in outpatient settings. Annals of Internal Medicine, 174(5), 723–725. https://doi.org/10.7326/m20-5926
Nielsen, J., Nørgaard, S. K., Lanzieri, G., Vestergaard, L. S., & Moelbak, K. (2021). Sex-differences in COVID-19 associated excess mortality is not exceptional for the COVID-19 pandemic. Scientific Reports, 11(1), 20815. https://doi.org/10.1038/s41598-021-00213-w
O’Connor, R. J., Preston, N., Parkin, A., Makower, S., Ross, D., Gee, J., et al. (2022). The COVID-19 Yorkshire Rehabilitation Scale (C19-YRS): Application and psychometric analysis in a post-COVID-19 syndrome cohort. Journal of Medical Virology, 94(3), 1027–1034. https://doi.org/10.1002/jmv.27415
Oates, G. R., Jackson, B. E., Partridge, E. E., Singh, K. P., Fouad, M. N., & Bae, S. (2017). Sociodemographic patterns of chronic disease: How the Mid-South region compares to the rest of the country. American Journal of Preventive Medicine, 52(1S1), S31–S39. https://doi.org/10.1016/j.amepre.2016.09.004
Patanavanich, R., & Glantz, S. A. (2021). Smoking is associated with worse outcomes of COVID-19 particularly among younger adults: A systematic review and meta-analysis. BMC Public Health, 21(1), 1554. https://doi.org/10.1186/s12889-021-11579-x
Phillips, S., & Williams, M. A. (2021). Confronting our next national health disaster — long-haul Covid. New England Journal of Medicine, 385(7), 577–579. https://doi.org/10.1056/NEJMp2109285
Seeßle, J., Waterboer, T., Hippchen, T., Simon, J., Kirchner, M., Lim, A., et al. (2021). Persistent symptoms in adult patients one year after COVID-19: A prospective cohort study. Clinical Infectious Diseases, 74(7), 1191–1198. https://doi.org/10.1093/cid/ciab611
Sudre, C. H., Murray, B., Varsavsky, T., Graham, M. S., Penfold, R. S., Bowyer, R. C., et al. (2021). Attributes and predictors of long COVID. Nature Medicine, 27(4), 626–631. https://doi.org/10.1038/s41591-021-01292-y
Taber, J. M., Leyva, B., & Persoskie, A. (2015). Why do people avoid medical care? A qualitative study using national data. Journal of General Internal Medicine, 30(3), 290–297. https://doi.org/10.1007/s11606-014-3089-1
Taylor, E. H., Marson, E. J., Elhadi, M., Macleod, K. D. M., Yu, Y. C., Davids, R., et al. (2021). Factors associated with mortality in patients with COVID-19 admitted to intensive care: A systematic review and meta-analysis. Anaesthesia, 76(9), 1224–1232. https://doi.org/10.1111/anae.15532
The Writing Committee for the COMEBAC Study Group. (2021). Four-month clinical status of a cohort of patients after hospitalization for COVID-19. Journal of the American Medical Association, 325(15), 1525–1534. https://doi.org/10.1001/jama.2021.3331
Thompson, E. J., Williams, D. M., Walker, A. J., Mitchell, R. E., Niedzwiedz, C. L., Yang, T. C., et al. (2021). Risk factors for long COVID: Analyses of 10 longitudinal studies and electronic health records in the UK. medRxiv, 2021.2006.2024.21259277. https://doi.org/10.1101/2021.06.24.21259277.
WHO. (2021). A clinical case definition of post COVID-19 condition by a Delphi consensus, 6 October 2021. https://www.who.int/publications/i/item/WHO-2019-nCoV-Post_COVID-19_condition-Clinical_case_definition-2021.1. Accessed 1 Feb 2022.
Acknowledgements
Many thanks to the Fondation Cité de la Santé and the Jewish Rehabilitation Hospital Foundation for funding this research and to the Direction de santé publique de Laval for their collaboration in accessing the participants. Thank you to Aliki Thomas, Alex Battaglini, Claudia Tremblay, Samir Sangani, and Vira Rose from the Centre intégré de santé et de services sociaux de Laval. We express appreciation for the dedication of the project coordinators and research assistants: LingXin He, Charlotte Davan, Melanie Halevy, Marie-An Hoang, Farah Jaber, Alicia Nguy, Dan Vu, and An Kateri Vu. Many thanks to Garbis Meshefedjian for assistance with the data management and analysis.
Code availability
Not applicable.
Funding
This study was funded by the Fondation Cité de la Santé & the Jewish Rehabilitation Hospital Foundation.
Author information
Authors and Affiliations
Contributions
All authors conceived of the study, acquired funding, were involved in the writing of the manuscript, and approved the final version for publication. DEF and BM were responsible for data acquisition.
Corresponding author
Ethics declarations
Ethics approval
We received ethics approval from the Comité scientifique et d’éthique de la recherche de CISSS Laval. Contact information for eligible participants was obtained from the Public Health Department of the City of Laval. Participants gave oral consent.
Consent for publication
Not applicable.
Conflict of interest
The authors declare no competing interests.
Additional information
Publisher’s note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Rights and permissions
Springer Nature or its licensor holds exclusive rights to this article under a publishing agreement with the author(s) or other rightsholder(s); author self-archiving of the accepted manuscript version of this article is solely governed by the terms of such publishing agreement and applicable law.
About this article
Cite this article
Feldman, D.E., Boudrias, MH. & Mazer, B. Long COVID symptoms in a population-based sample of persons discharged home from hospital. Can J Public Health 113, 930–939 (2022). https://doi.org/10.17269/s41997-022-00695-9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.17269/s41997-022-00695-9