Abstracts
The present investigation was a cross-sectional, quantitative research study analyzing incidents associated with nursing care using a root-cause methodological analysis. The study was conducted in a public hospital intensive care unit (ICU) in Santiago de Chile and investigated 18 incidents related to nursing care that occurred from January to March of 2012. The sample was composed of six cases involving medications and the self-removal of therapeutic devices. The contributing factors were related to the tasks and technology, the professional work team, the patients, and the environment. The analysis confirmed that the cases presented with similar contributing factors, thereby indicating that the vulnerable aspects of the system are primarily responsible for the incidence occurrence. We conclude that root-cause analysis facilitates the identification of these vulnerable points. Proactive management in system-error prevention is made possible by recommendations.
Critical care; Intensive Critical Care; Nursing care; Patient safety; Root cause analysis
Investigação quantitativa do tipo transversal que analisou os incidentes relacionados aos cuidados de enfermagem por meio da metodologia de análise da causa raiz. Foi realizado em uma unidade de cuidados intensivos de um hospital público de Santiago do Chile. O universo foi composto por 18 incidentes relacionados aos cuidados de enfermagem ocorridos de janeiro a março de 2012. A amostra foi composta por seis casos relacionados a medicamentos e retirada não planejada de artefatos terapêuticos. Os fatores relacionados foram: tarefa e tecnologia, equipe de trabalho, profissional, paciente e ambiente. Na análise, constatou-se que os casos apresentaram fatores relacionados semelhantes, concluindo que os pontos vulneráveis do sistema são em sua maioria responsáveis pela ocorrência de incidentes. Conclui-se que a análise da causa raiz permite identificar esses pontos vulneráveis e, por meio de recomendações, possibilita a gestão proativa na prevenção de falhas do sistema.
Cuidados críticos; Unidades de Terapia Intensiva; Cuidados de enfermagem; Segurança do paciente; Análise de causa fundamental
Investigación cuantitativa de tipo transversal que analizó los incidentes relacionados a los cuidados de enfermería, por medio de la metodología del análisis causa - raíz. Fue realizado en una unidad de cuidados intensivos de un hospital público de Santiago de Chile. El universo fue compuesto por 18 incidentes relacionados a los cuidados de enfermería ocurridos de enero a marzo del 2012. La muestra fue constituida por seis casos relacionados a medicamentos y retiro no planificado de artefactos terapéuticos. Los factores relacionados fueron: tarea y tecnología, equipo de trabajo, profesional, paciente y ambiente. En el análisis se constató que los casos presentaron factores relacionados semejantes, concluyendo que los puntos vulnerables del sistema son en su mayoría, los responsables por la ocurrencia de incidentes. Se concluye que el análisis de causa - raíz permite la identificación de estos puntos vulnerables y, por medio de recomendaciones, posibilita la gestión proactiva en la prevención de fallas del sistema.
Cuidados críticos; Unidades de Cuidados Intensivos; Atención de enfermería; Seguridad del paciente; Análisis da causa raíz
Introduction
Safe care requires nursing professionals to make decisions and take action when confronting risky situations that threaten patient security and to address possible incident occurrences. These circumstances range from minor occurrences that might even go unnoticed to serious occurrences that may cause injury, disability, or death (adverse events).
Patient safety, defined by the World Alliance for Patient Safety(11. World Health Organization (WHO). Marco Conceptual de la
Clasificación Internacional para la Seguridad del Paciente. Versión 1.1. Informe
Técnico Definitivo [Internet]. Geneva; 2009 [citado 2012 Ju 28]. Disponible en:
http://www.who.int/patientsafety/implementation/icps/icps_full_report_es.pdf
http://www.who.int/patientsafety/impleme...
) as reducing the risk of
unnecessary harm to an acceptable minimum, is a constant component of and is closely
related to patient care. The nursing professional is in charge of the risk process
analysis for the consequent reduction and prevention of incidents.
Patient safety concerns emerged in the 1990s with the important American publication "To Err is Human: building a safer health system(22. Kohn LT,Corrigan JM, Donaldson MC, editors;Institute of Medicine. ToErr Human: building a safer health system. Washington: National Academy Press; 1999.) of the Institute of Medicine (IOM), in which the authors reported the deaths of 44,000 to 98,000 Americans resulting from incidents that were largely preventable. Additionally, the report opens the discussion on the systemic view of event analysis versus the culture of individual blame.
The systemic analysis of incidents is based on reflective and systemic models, in which errors, ranging from the unsafe actions of nursing staff to managerial-level decisions, are investigated. This approach has replaced the culture of individual blame. Clear and objective event analysis, without the intention to blame, enables the identification of causes, thereby enabling the creation of systemic improvement strategies(22. Kohn LT,Corrigan JM, Donaldson MC, editors;Institute of Medicine. ToErr Human: building a safer health system. Washington: National Academy Press; 1999.-33. Reason J. Human error. New York: Cambridge University Press; 1990.).
Causal analysis models of incidents were primarily developed in the nuclear and aviation industries. Some of these models were adapted for use in healthcare settings. The London Protocol is an incident analysis proposal based on the organizational model of James Reason. The protocol, in which unsafe acts resulting in an incident are viewed more as consequences than as causes, is accepted and recognized worldwide(44. Taylor-Adams S, Vincent CH. System analysis of clinical incidents: the London Protocol. London: Clinical Safety Research Unit, Imperial College; 2004.) .
The London Protocol, which was developed by Taylor-Adams and Vincent, is a healthcare-sector adaptation. The authors stress that this tool may be used to conduct research much more easily and rapidly, i.e., in five to ten minutes. This research tool enables the identification of major problems and contributing factors related to incidence occurrence. The decision to use this tool at a given moment depends on the gravity of the incident, the learning potential, and the available resources. The process can be performed by an individual or by a team and is relatively standardized for the analysis of minor or major incidents(44. Taylor-Adams S, Vincent CH. System analysis of clinical incidents: the London Protocol. London: Clinical Safety Research Unit, Imperial College; 2004.) .
The road to incidence research begins with the decision to conduct research, the selection of a research team, obtaining and organizing the information, establishing the incident chronology, identifying unsafe acts, identifying the contributing factors, and then making recommendations and creating action plans for reducing and preventing new occurrences(44. Taylor-Adams S, Vincent CH. System analysis of clinical incidents: the London Protocol. London: Clinical Safety Research Unit, Imperial College; 2004.) .
Particularly in intensive care units (ICUs), the setting presents a significant number of factors that contribute to incident occurrence, such as patient severity, the use of sophisticated equipment, a diversity in treatment medications, and a range of invasive interventions, among other factors. In this context, the London Protocol, as a causal analysis model, is a thorough and effective tool that promotes reliability in the provision of care.
Studies demonstrate the benefits of the root-cause analysis process in detecting the
true error cause, as well as the consequent development of assertive prevention
strategies. A research study conducted in Taiwan regarding the administration of
chemotherapy drugs identified the lack of protocols and knowledge as main causes of
error and demonstrated a significant decrease in the post-interventional lack of
protocols and knowledge(55. Huang YY, Liao MC, Chen YH, Deng CH. Promotingtheaccuracy of
chemotherapy medication administration for nurses: anapplication of root cause
analysis.Hu Li ZaZhi. 2009;56(3):57-65.) .
Another study of medication errors (conducted in Brazil) identified multiple
factors, including (but not limited to) the dispensing of medications and patient
identification and supervision, and presented a proposal of strategies and
recommendations to avoid these errors(66. Teixeira TCA, Cassiani SHB. Root cause analysis: evaluation of
medication errors at a university hospital.RevEscEnferm USP [Internet]. 2010
[cited 2012 July 28]; 44(1):137-44.Available from:
http://www.scielo.br/pdf/reeusp/v44n1/en_a20v44n1.pdf
http://www.scielo.br/pdf/reeusp/v44n1/en...
) .
Regarding the impact of the methodology of causal incident analysis, in a study done in Texas on medication-related incidents that were considered preventable, a 45% drop in incidence rates was reported in blame-free systemic analysis post-implementation(77. Rex JH, Turnbull JE, Allen SJ, VandeVoorde K, Luther K. Systematic root cause analysis of adverse drugevents in a tertiary referral hospital. JT Comm J QualImprov. 2000;26(10):563-75.). A similar research study done in two Taiwanese hospitals evaluated the effectiveness of the proposed interventions through root cause analysis of post-partum incidents. The study showed that the intervention group presented with a decrease in incidents from 14.24 per 1,000 patients to 6.02 per 1,000 patients post-intervention as well as significant differences (p<0,001) between the incident rate before and after the interventions(88. Chen KH, Chen LR, Su S. Applying root cause analysis to improvepatient safety: decreasing falls in post partum women. QualSafHealthCare. 2010;19(2):138-43.).
Due to the viability and benefits of the proposed methodology in the London Protocol for analyzing nursing care-related incidents, this methodology was applied in a public health institution to empirically demonstrate how and why such incidents occur. In addition, the viability of utilizing this method has served to create prevention strategies and recommendations.
Consequently, the objectives of the present study were to analyze incidents related to nursing care by using the London Protocol methodology and to publicize the benefits of utilizing root cause as a tool for improving patient security.
Method
This cross-sectional quantitative study utilizing a root-cause analysis methodology involved researching phenomena through observation and a description of the facts and contextual aspects to determine how and why the phenomenon occurred(99. Heuvel LNV, Lorenzo KD, Montgomery RL, Hanson WE, Rooney JR. Root cause analysis handbook: a guide to effective incident investigation. Brookfield: ABS Consulting; 2005.), thereby facilitating cause determination.
The present investigation was conducted in the general ICU of a public hospital in Santiago de Chile, which is the main emergency medicine healthcare center for adults in the metropolitan region of Santiago de Chile. The facility is considered a highly specialized hospital that primarily treats emergency cardiovascular conditions and trauma from accidents or violence. The ICU includes 31 hospital beds and is set up for clinical and surgical care.
In total, there were 18 incidents reported and related to nursing care that occurred from January to March of 2012. These incidents were recorded in the incident notification registry, which is housed in the institution’s Quality Department. The 18 reported incidents are associated with medication errors and the non-programmed withdrawal of therapeutic devices. Given the homogeneity of the cases, the sample for root-cause analysis was composed of six cases: three related to medications and three involving the self-withdrawal of therapeutic devices. The six cases were selected through the accessibility of patient files and the available resources for data collection and to reach the study goal of publicizing the benefits of utilizing root-cause analysis as a tool for improving patient safety.
The present investigation was approved by the Scientific Ethics Committee of the Nursing Department at the Andres Bello University. The study was registered in a numbered book on page 42, which corresponds to the broadcasted approval certification registry, and was granted prior institutional authorization. The study goals and procedures were explained in a detailed manner to the healthcare team, who handled the appointments and requested a signature of informed consent prior to the interviews.
Identification and decision to research
This first phase consists of decision-making regarding incidents for investigation based on the incident severity, the available resources, and the institutional learning potential(44. Taylor-Adams S, Vincent CH. System analysis of clinical incidents: the London Protocol. London: Clinical Safety Research Unit, Imperial College; 2004.). In the current study, the analyzed incidents were selected by the researchers according to the greatest frequency of occurrence, the possibility of accessing the clinic patient registries, and the scientific evidence, thereby guaranteeing a greater potential for organizational learning.
Group researcher selection
The research-group selection process must evaluate research experience and the members’ knowledge of the incidents. The group should include no more than three or four lead researchers(44. Taylor-Adams S, Vincent CH. System analysis of clinical incidents: the London Protocol. London: Clinical Safety Research Unit, Imperial College; 2004.). Thus, the present research group was composed of three investigators and two nurses from the institution's Quality and Risk Management Department. This group complemented each other in research knowledge and incidence experience as well as in specific clinical knowledge and experience.
Obtaining and organizing the information
This step consists of compiling and organizing all possible information, including a minimal complete clinical history, the protocols and procedures related to the incident, statements and immediate observations, interviews with those involved, and physical evidence (e.g., floor plans, shift lists, and documents regarding the lives of the involved team members, amongst others)(44. Taylor-Adams S, Vincent CH. System analysis of clinical incidents: the London Protocol. London: Clinical Safety Research Unit, Imperial College; 2004.). The data for performing the analysis was obtained through the patient clinical history; the requested clinical forms were gathered from the Medical Archives Service. The data related to the protocols and procedures, as well as to other relevant aspects, such as the shift-rotation rate and the availability of personnel, were obtained through interviews with the nursing team and through field observations.
Establishment of the chronological incidence
In this phase, using all of the information, it is possible to design the entire sequence of the facts and to compare them to events that actually occurred according to the policies, protocols, and procedures present in the service(44. Taylor-Adams S, Vincent CH. System analysis of clinical incidents: the London Protocol. London: Clinical Safety Research Unit, Imperial College; 2004.). In the present study, the research investigator led discussions of how the events actually occurred versus how the events should have occurred.
Identification of the unsafe acts and identification of the contributing factors
According to the methodology utilized in the London Protocol, once the sequence of facts that led to the incident is determined, the unsafe acts and contributing factors are separately identified.
An unsafe act is defined as conduct that occurs during the healthcare process by an action or omission of team members. Each unsafe act can be involved with one or more contributing factors, which may be related to the tasks and technology, the work environment, team factors, patients, individual factors, and the institutional context(44. Taylor-Adams S, Vincent CH. System analysis of clinical incidents: the London Protocol. London: Clinical Safety Research Unit, Imperial College; 2004.).
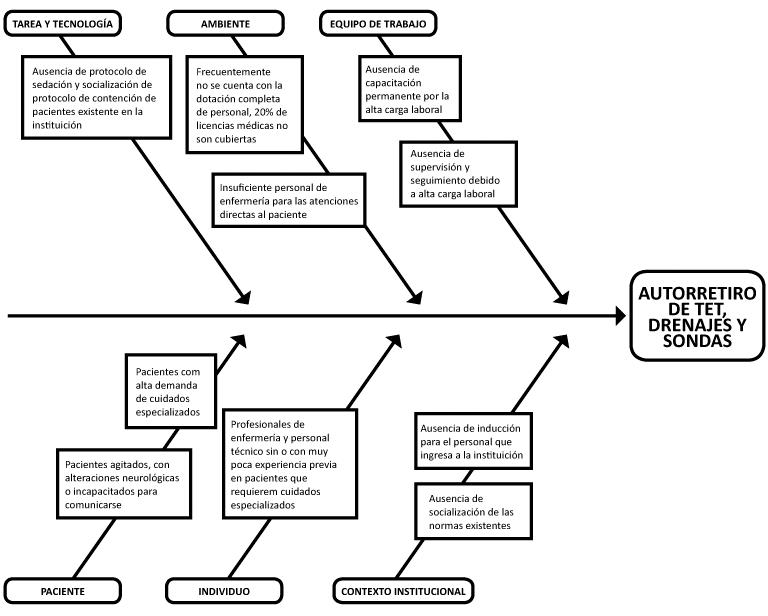
Once researchers have identified the unsafe acts that have led to incidents, they design the contributing factors related to each unsafe act using a fishbone diagram(44. Taylor-Adams S, Vincent CH. System analysis of clinical incidents: the London Protocol. London: Clinical Safety Research Unit, Imperial College; 2004.). The fishbone diagram, also known as the Ishikawa diagram or the cause-and-effect diagram, is one of the most utilized tools in action improvement and quality control in organizations as it enables grouping the causes of the phenomena that are expected to be improved. The fishbone diagram also enables graphically establishing a relationship between the detected problem and its possible causes, thereby enabling its visualization in an easier and more understandable manner(1010. González FJM, Mera AC, Lacoba SR. Introducción a la gestión de lacalidad. Madri: Delta; 2007.).
Recommendations and action plan
After recognizing the contributing factors, a series of recommendations and improvement plans were made based on the weaknesses found; these recommendations and plans were translated into demonstrable improvements in line with the organization’s situation(44. Taylor-Adams S, Vincent CH. System analysis of clinical incidents: the London Protocol. London: Clinical Safety Research Unit, Imperial College; 2004.). From the contributing factors identified in this study, a series of recommendations was proposed to improve the identified weaknesses.
Results
Each incidence was separately analyzed according to the London Protocol phases described in the method. However, due to the nature of this method, the events are presented in two categories: medication-related incidences and incidences related to the self-withdrawal of therapeutic devices.
The medication-related incidences involved dosage omissions, medication errors, and dosage errors, and the incidences related to the self-withdrawal of therapeutic devices were associated with drainages, nasogastric catheters, and endotracheal tubes.
Root-cause analysis of the medication-related incidences
The first case involved dosage omission and medication error. In this case, a dose of antibiotics was not administered to a patient with a severe infectious condition due to the unavailability of venous access.
The registries, interviews, and observations revealed that the patient had a single, peripheral venous access through which vasoactive drugs were administered, making it impossible to utilize this site for administering other medications. This patient did not always have an adequate central venous route, even when receiving vasoactive drugs.
In light of all of this information and case discussion, unsafe acts were identified as premature non-installation of a central venous route to a patient in serious condition utilizing vasoactive drugs with single, peripheral venous access.
In light of the case analysis, the identified contributing factors were related to the tasks and technology (i.e., lack of socialization of the norms for managing and administering medications through central and peripheral venous routes), the work team (i.e., lack of supervision), the professional staff (i.e., lack of experience), and the patients (i.e., specialized care) (Figure 1).
The second case analyzed was due to medication error. In this situation, the patient was given a medication that was not prescribed for the medical indication. The notification registries stated that the medication was suspended and not communicated. The interview and observations revealed that the medical indication is transcribed on individual cards for each patient and is utilized for personnel as a guide for medication administration. The cards are not always updated throughout the shift because of time constraints. Following the case analysis and discussion, the unsafe act was identified as the nursing staff’s failure to update the patient’s card, which is a situation that could have been avoided if the nursing professional had communicated the change. Therefore, insufficient communication among the nursing team and an excessive workload were identified as contributing factors (Figure 1).
- Contributing factors identified by the root-cause analysis of medication-related incidences – Santiago de Chile, 2012.
Regarding the last medication-related case, a lower dose of antibiotics than what was prescribed was given to the patient for his/her medical indication. This case was viewed as a dosage error. In the patient clinic form, it was stated that the medication dosage was modified for the same indication. The interviews and observations revealed that this change was not communicated and that the transcription card was not updated due to time constraints. In the case analysis, the same contributing factors as in the previous case were identified (Figure 1).
Root-cause analysis of incidences related to the self-withdrawal of therapeutic devices
In the first and second cases, the same patient was treated, and these situations involved the self-withdrawal of a thoracic drainage tube and a nasogastric catheter during a patient episode of psychomotor agitation. From the clinic registry forms, information was obtained documenting the medical indication to reduce sedation until the medication was suspended. The interviews and observations revealed that the doctors ordered sedation according to their own criteria, without following the drug reduction and suspension phase. In addition, it was impossible to constantly monitor the patient due to lack of time and staff.
In the analysis carried out, unsafe acts such as patient agitation due to inadequate sedation, monitoring, follow-up and utilization of physical control led to the identification of contributing factors related to the lack of sedation protocols, lack of socialization of containment protocols, and the lack of patient monitoring and follow-up due to high work load (Figure 2).
- Contributing factors identified by the root-cause analysis of incidences related to the self-withdrawal of therapeutic devices- Santiago de Chile, 2012.
The third case of incidences related to the self-withdrawal of therapeutic devices was related to the self-withdrawal of an endotracheal tube, whereby the patient (without signs of psychomotor agitation, without sedation, and with mechanical control) removed the endotracheal tube. The tube was re-inserted with no complications.
Discussion
Root-cause analysis of medication-related incidences
According to the National Coordinating Council for Medication Error Reporting and
Prevention (NCC MERP)(1111. National Coordinating Council for Medications Errors Reporting
and Prevention.The NCC MERP Taxonomy of MedicationErrors [Internet]. [cited 2012
July 28]. Availablefrom:
http://www.nccmerp.org/pdf/taxo2001-07-31.pdf
http://www.nccmerp.org/pdf/taxo2001-07-3...
), dosage
omission-type medication error refers to the non-administration of an indicated
dosage before administering the next dose.
In the first case related to dosage omission, the identified contributing factors were related to the tasks and technology (i.e., lack of socialization of the norms for managing and administering medications through central and peripheral venous routes), the work environment (i.e., lack of supervision), the professional staff (i.e., lack of experience), and the patients (i.e., specialized care).
The studies of medication errors reveal that dosage omission is the most prevalent type of error, and these investigations reveal various factors related not only to the nursing team but also to processes that begin with medication distribution by the pharmaceutical industry to treat patient conditions(1212. Silva AEBC, Reis AMM, Miasso AI, Santos JO, Cassiani SHB. Adverse drugevents in a sentinel hospital in theState of Goiás, Brazil.Rev Latino Am Enferm.2011;19(2): 378-86.-1313. Toffoletto MC, Padilha KG. Consequences of medical errors in intensive and semi-intensivecareunits.RevEscEnferm USP. 2006;40(2):247-52. ).
Care related to the management and maintenance of adequate venous access is the responsibility of the nursing professional and is directly related to the safe administration of medications. A patient who is in serious condition with inadequate venous access, in addition to receiving a vasoactive drug, indicates the absence of nursing staff supervision and a lack of internal policies for maintaining adequate venous access for patients in serious condition.
In addition to the absence of supervision, the lack of experience in critical patient care among nursing professionals is a key factor, both in the administration of medications and in all aspects of patient safety.
Studies have demonstrated the presence of an excessive number of nurses with less than five years of experience in specialized care, despite the requirements of solid techno-scientific knowledge and the fundamental prerequisites for managing the drugs utilized in intensive care(1414. Padilha KG, Kitahara PH, Gonçalves C CS, Sanches AC. Iatrogenic occurrence swith medication in I. C. U: nurse'sprocedures and feelings.RevEscEnferm USP. 2006; 36(1):50-57. ).
Regarding the second and third cases, following the analysis and discussion, the unsafe act was identified as the nursing staff’s failure to update the patient care, which is a situation that could have been avoided if the change had been communicated to the nursing professionals. In addition, the contributing factors were identified as insufficient communication among the nursing team and an excessive workload.
A study conducted in four Brazilian hospitals with 152 nursing professionals demonstrated that the most frequently cited medication errors involved the prescription and transcription of the medications(1515. Miasso AI, Grou CR, Cassiani SHB, Silva AEBC, Fakih FT. Medicationerrors: types, causes and measures taken in four brazilian hospitals. RevEscEnferm USP. 2006; 40(4):524-32.). Medication transcription is one of the phases in the process of administering medications and is primarily performed by nursing professionals. A mistake in this phase initiates a chain of errors that alter the process, leading to patient safety risks.
The process of communicating specific information from a patient to a healthcare
provider is conducted in a manner that assures continuity and safety in patient
care(1616. Joint Commission. Improving America's Hospitals: a Reporton
Quality and Safety, 2006 [Internet].Washington;2007 [cited 2012 July 28].
Available from:
http://www.jointcommission.org/assets/1/6/2006_Annual_Report.pdf
http://www.nccmerp.org/pdf/taxo2001-07-3...
). Studies have
revealed that the main problem with ineffective communication stems from a lack of
"face-to-face" interactions and from transmitted information that is imprecise,
ambiguous, and disorganized(1717. Arora V, Johnson J, Lovinger D, Humphrey H, Meltzer D.
Communication failures in patient sign-out and suggestions for improvement: a
critical incident analyisis. QualSafHealthCare.
2005;14(6):401-7.).
Various studies have demonstrated the implications of the workload on patient safety, whereby the impact of new technologies and patient severities increasingly require more specialized professionals, resulting in excess costs at hospital institutions(1818. Lima MKF, Tsukamoto R, Fugulin FMT. Aplicação do Nursing Activities Score em pacientes de alta dependência de enfermagem. Texto Contexto Enferm. 2008;17(4):638-46. ).
Root-cause analysis of incidences related to the self-withdrawal of therapeutic devices
Regarding the self-withdrawal of therapeutic devices, a study conducted in seven Brazilian ICUs revealed that, of 113 incidences, 57.5% occurred in patients with psychomotor agitation and clinical instability. Of these cases, 40.7% were related to the non-programmed removal of catheters and drainage tubes(1919. Padilha KG. Iatrogenic occurences in the intensive care units: analysis of there lated factors. Rev Paul Enferm. 2006;25(1):18-23.).
The literature has not been clear and consistent regarding the use of a physical-containment strategy to guarantee the prevention of events that are primarily related to falls or to the self-withdrawal of devices. In Chile, the Health Department does not provide any protocols or patient-containment norms. The majority of Chilean hospitals have their own physical-control norms, which involve techniques and materials that cause no harm to patients. However, pharmacological control is the first choice to ensure patient safety and comfort.
Evidence suggests that the use of sedation guided by protocols, combined with the active participation of the nursing staff to ensure compliance, reduces complications that arise from the inadequate and heterogeneous utilization of drugs(2020. Kress JP, Pohlman AS, O'Connor MF, Hall JB. Daily interruption of sedative infusions in critically ill patients under going mechanical ventilation. N Engl J Med.2000;342(20):1471-7. ).
The third case is related to the self-withdrawal of an endotracheal tube, whereby the patient (without signs of psychomotor agitation, without sedation, and with mechanical control) removed the endotracheal tube; the device was re-inserted without complications.
Self-withdrawal of an endotracheal tube is a worrisome event due to the severity of the possible consequences because many patients may require the insertion of a new tube. This situation can cause worsening of the clinical condition.
A Brazilian study conducted in five ICUs demonstrated that patients who suffer a self-withdrawal event or the accidental removal of an endotracheal tube have a four-fold greater chance of dying of complications related to tube re-insertion(2121. Toffoletto MC. Fatores associados aos eventos adversos em Unidade de Terapia Intensiva [tese doutorado]. São Paulo: Escola de Enfermagem, Universidade de São Paulo; 2008.).
A US study of 1,976 healthcare professionals (including doctors, nurses, and kinesiologists) demonstrated that those who were surveyed considered the following to be high-risk factors for unplanned tube removal: lack of physical control (72%), high workload (60%), patient transport (59%), and inadequate sedation (43%)(2222. Tanios MA, Epstein SK, Livelo J, Teres D. Can we identify patients at high risk for unplanne dextubation? A large-scale multi disciplinarysurvey. RespirCare. 2010; 55(5):561-8.). Previous data corroborate the contributing factors found in the analysis of the present case, namely, the lack of a sedation protocol, the failure to socialize the control protocols, and the absence of patient monitoring and follow-up due to heavy workloads.
Strategies and recommendations for the proposed reduction and prevention, drawn from the contributing factors
The present study identified some of the active flaws that occur during daily practice, including unsafe actions and omissions in patient care. It is noteworthy that the proposed recommendations in the present study are the beginning of a series of interventions that should be consolidated to assure safe care for each patient who enters this or any other hospital institution.
√ The strategies and recommendations based on the contributing factors revealed by root-cause analysis of the incidences are presented as follows:
√ Socializing the existing institutional norms related to:
o Installing and managing central venous routes
o Administering medications via the central and peripheral venous routes.
√ Training the members of the healthcare team regarding communication, with priority given to topics related to efficient communication during the entire period of patient care.
√ Designing and implementing a program for the induction of professional and technical personnel and incorporating this program into the institution.
√ Designing and implementing an ongoing training program for managing patients who require specialized care.
√ Implementing sedation protocols for patients with psychomotor agitation.
√ Socialization and training regarding the existing physical-control protocols for patients with psychomotor agitation.
Conclusions
The current study employed a root-cause methodological analysis to identify and analyze six cases of incidences related to nursing care for critical patients, with the goal of empirically demonstrating how and why these incidences occur and of publicizing the benefits of utilizing root-cause analysis to guarantee patient safety.
The incidences with the highest frequencies and greatest access to information were selected from the notification registries. It was confirmed that all of the analyzed incidences caused no harm to the patients and were avoidable.
The literature reveals that a significant proportion of the incidences that occur during patient care do not cause harm and many times are unnoticed. These incidences must be assessed independently from the degree of harm because they enable the identification of vulnerable elements in the system that may lead to a serious incidence.
The contributing factors identified in the analysis of incidences were related to the tasks and technology (i.e., failure to socialize the norms and protocols), the work environment (i.e., lack of supervision and communication; a high workload), the professional staff (i.e., lack of experience and knowledge), and the patients (i.e., specialized care).
The incidence analysis, despite identifying various unsafe actions, confirmed that the six cases presented similar contributing factors and represented vulnerable points in the system that are primarily responsible for incidence occurrence.
We conclude that a root-cause analysis enables the identification of these vulnerable points and, through strategies and recommendations, facilitates proactive management for preventing system errors.
Regarding the relevance of the results, the current study presented limitations related to the difficulty of accessing the patient registries and the probable under-notification of the incidences.
The results and recommendation proposals were socialized with the institution’s Quality and Risk Management Department, the field of study, and the knowledge of the benefits of utilizing root-cause analysis as a tool for improving patient safety.
References
-
1World Health Organization (WHO). Marco Conceptual de la Clasificación Internacional para la Seguridad del Paciente. Versión 1.1. Informe Técnico Definitivo [Internet]. Geneva; 2009 [citado 2012 Ju 28]. Disponible en: http://www.who.int/patientsafety/implementation/icps/icps_full_report_es.pdf
» http://www.who.int/patientsafety/implementation/icps/icps_full_report_es.pdf -
2Kohn LT,Corrigan JM, Donaldson MC, editors;Institute of Medicine. ToErr Human: building a safer health system. Washington: National Academy Press; 1999.
-
3Reason J. Human error. New York: Cambridge University Press; 1990.
-
4Taylor-Adams S, Vincent CH. System analysis of clinical incidents: the London Protocol. London: Clinical Safety Research Unit, Imperial College; 2004.
-
5Huang YY, Liao MC, Chen YH, Deng CH. Promotingtheaccuracy of chemotherapy medication administration for nurses: anapplication of root cause analysis.Hu Li ZaZhi. 2009;56(3):57-65.
-
6Teixeira TCA, Cassiani SHB. Root cause analysis: evaluation of medication errors at a university hospital.RevEscEnferm USP [Internet]. 2010 [cited 2012 July 28]; 44(1):137-44.Available from: http://www.scielo.br/pdf/reeusp/v44n1/en_a20v44n1.pdf
» http://www.scielo.br/pdf/reeusp/v44n1/en_a20v44n1.pdf -
7Rex JH, Turnbull JE, Allen SJ, VandeVoorde K, Luther K. Systematic root cause analysis of adverse drugevents in a tertiary referral hospital. JT Comm J QualImprov. 2000;26(10):563-75.
-
8Chen KH, Chen LR, Su S. Applying root cause analysis to improvepatient safety: decreasing falls in post partum women. QualSafHealthCare. 2010;19(2):138-43.
-
9Heuvel LNV, Lorenzo KD, Montgomery RL, Hanson WE, Rooney JR. Root cause analysis handbook: a guide to effective incident investigation. Brookfield: ABS Consulting; 2005.
-
10González FJM, Mera AC, Lacoba SR. Introducción a la gestión de lacalidad. Madri: Delta; 2007.
-
11National Coordinating Council for Medications Errors Reporting and Prevention.The NCC MERP Taxonomy of MedicationErrors [Internet]. [cited 2012 July 28]. Availablefrom: http://www.nccmerp.org/pdf/taxo2001-07-31.pdf
» http://www.nccmerp.org/pdf/taxo2001-07-31.pdf -
12Silva AEBC, Reis AMM, Miasso AI, Santos JO, Cassiani SHB. Adverse drugevents in a sentinel hospital in theState of Goiás, Brazil.Rev Latino Am Enferm.2011;19(2): 378-86.
-
13Toffoletto MC, Padilha KG. Consequences of medical errors in intensive and semi-intensivecareunits.RevEscEnferm USP. 2006;40(2):247-52.
-
14Padilha KG, Kitahara PH, Gonçalves C CS, Sanches AC. Iatrogenic occurrence swith medication in I. C. U: nurse'sprocedures and feelings.RevEscEnferm USP. 2006; 36(1):50-57.
-
15Miasso AI, Grou CR, Cassiani SHB, Silva AEBC, Fakih FT. Medicationerrors: types, causes and measures taken in four brazilian hospitals. RevEscEnferm USP. 2006; 40(4):524-32.
-
16Joint Commission. Improving America's Hospitals: a Reporton Quality and Safety, 2006 [Internet].Washington;2007 [cited 2012 July 28]. Available from: http://www.jointcommission.org/assets/1/6/2006_Annual_Report.pdf
» http://www.nccmerp.org/pdf/taxo2001-07-31.pdf -
17Arora V, Johnson J, Lovinger D, Humphrey H, Meltzer D. Communication failures in patient sign-out and suggestions for improvement: a critical incident analyisis. QualSafHealthCare. 2005;14(6):401-7.
-
18Lima MKF, Tsukamoto R, Fugulin FMT. Aplicação do Nursing Activities Score em pacientes de alta dependência de enfermagem. Texto Contexto Enferm. 2008;17(4):638-46.
-
19Padilha KG. Iatrogenic occurences in the intensive care units: analysis of there lated factors. Rev Paul Enferm. 2006;25(1):18-23.
-
20Kress JP, Pohlman AS, O'Connor MF, Hall JB. Daily interruption of sedative infusions in critically ill patients under going mechanical ventilation. N Engl J Med.2000;342(20):1471-7.
-
21Toffoletto MC. Fatores associados aos eventos adversos em Unidade de Terapia Intensiva [tese doutorado]. São Paulo: Escola de Enfermagem, Universidade de São Paulo; 2008.
-
22Tanios MA, Epstein SK, Livelo J, Teres D. Can we identify patients at high risk for unplanne dextubation? A large-scale multi disciplinarysurvey. RespirCare. 2010; 55(5):561-8.
-
*
Taken from the study “Análisis causa raíz: efectividad de las intervenciones en la seguridad del paciente: un estudio piloto en el Hospital de Urgencia Asistencia Publica de Santiago de Chile” (in process), Nursing Department of Andrès Bello University, 2011.
Publication Dates
-
Publication in this collection
Oct 2013
History
-
Received
24 Sept 2012 -
Accepted
05 June 2013