Abstract
Background
Although volume displacement (VD) is considered the gold standard for diagnosing breast cancer-related lymphedema, it is inconvenient. We compared bioimpedance (L-Dex) and VD measurements in a prospective cohort of breast cancer patients at risk for lymphedema.
Methods
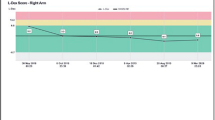
Between 2010 and 2014, a total of 223 breast cancer patients were enrolled. Following exclusions (n = 37), 186 received baseline VD and L-Dex; follow-up measurements were performed at 3–6 months intervals for 3 years. At each visit, patients fitted into one of three categories: normal (normal VD and L-Dex); abnormal L-Dex (L-Dex > 10 or increase in 10 from baseline and normal VD); or lymphedema (relative arm volume difference of >10 % by VD ± abnormal L-Dex). Change in L-Dex was plotted against change in VD; correlation was assessed using the Pearson correlation.
Results
At a median follow-up of 18.2 months, 152 patients were normal, 25 had an abnormal L-Dex, and 9 developed lymphedema without a prior L-Dex abnormality. Of the 25 abnormal L-Dex patients, 4 progressed to lymphedema, for a total of 13 patients with lymphedema. Evaluating all time points, 186 patients had 829 follow-up measurements. Sensitivity and specificity of L-Dex compared with VD were 75 and 93 %, respectively. There was no correlation between change in VD and change in L-Dex at 3 months (r = 0.31) or 6 months (r = 0.21).
Conclusions
VD and bioimpedance demonstrated poor correlation with inconsistent overlap of measurements considered abnormal. Of patients with an abnormal L-Dex, few progressed to lymphedema; most patients with lymphedema did not have a prior L-Dex abnormality. Further studies are needed to understand the clinical significance of bioimpedance.



Similar content being viewed by others
References
Tsai RJ, Dennis LK, Lynch CF, et al. The risk of developing arm lymphedema among breast cancer survivors: a meta-analysis of treatment factors. Ann Surg Oncol. 2009;16(7):1959–72.
Dodds RL, Nielsen KA, Shirley AG, et al. Test-retest reliability of the commercial volumeter. Work. 2004;22(2):107–10.
Karges JR, Mark BE, Stikeleather SJ, et al. Concurrent validity of upper-extremity volume estimates: comparison of calculated volume derived from girth measurements and water displacement volume. Phys Ther. 2003;83(2):134–45.
Fu MR, Cleland CM, Guth AA, et al. L-dex ratio in detecting breast cancer-related lymphedema: reliability, sensitivity, and specificity. Lymphology. 2013;46(2):85–96.
Smoot BJ, Wong JF, Dodd MJ. Comparison of diagnostic accuracy of clinical measures of breast cancer-related lymphedema: area under the curve. Arch Phys Med Rehabil. 2011;92(4):603–10.
Cornish BH, Chapman M, Hirst C, et al. Early diagnosis of lymphedema using multiple frequency bioimpedance. Lymphology. 2001;34(1):2–11.
Blaney JM, McCollum G, Lorimer J, et al. Prospective surveillance of breast cancer-related lymphoedema in the first-year post-surgery: feasibility and comparison of screening measures. Support Care Cancer. 2015;23(6):1549–59.
Armer JM, Stewart BR. A comparison of four diagnostic criteria for lymphedema in a post-breast cancer population. Lymphat Res Biol. 2005;3(4):208–17.
Stout Gergich NL, Pfalzer LA, McGarvey C, et al. Preoperative assessment enables the early diagnosis and successful treatment of lymphedema. Cancer. 2008;112(12):2809–19.
Shih YC, Xu Y, Cormier JN, et al. Incidence, treatment costs, and complications of lymphedema after breast cancer among women of working age: a 2-year follow-up study. J Clin Oncol. 2009;27(12):2007–14.
Hayes SC, Speck RM, Reimet E, et al. Does the effect of weight lifting on lymphedema following breast cancer differ by diagnostic method: results from a randomized controlled trial. Breast Cancer Res Treat. 2011;130(1):227–34.
Specht MC, Miller CL, Russell TA, et al. Defining a threshold for intervention in breast cancer-related lymphedema: what level of arm volume increase predicts progression? Breast Cancer Res Treat. 2013;140(3):485–94.
Dengel LT, Van Zee KJ, King TA, et al. Axillary dissection can be avoided in the majority of clinically node-negative patients undergoing breast-conserving therapy. Ann Surg Oncol. 2014;21(1):22–7.
Giuliano AE, Hunt KK, Ballman KV, et al. Axillary dissection vs no axillary dissection in women with invasive breast cancer and sentinel node metastasis: a randomized clinical trial. JAMA. 2011;305(6):569–75.
Acknowledgments
The authors thank Dr. Kimberly J. Van Zee and Dr. Hiram S. Cody III for their critical review of this manuscript.
Disclosure
This study was a podium presentation at the Society of Surgical Oncology 2015 Annual Cancer Symposium, and was supported by a grant from The Sharpe–Strumia Research Foundation at The Bryn Mawr Hospital, and in part by a National Institutes of Health/National Cancer Institute Cancer Center Support Grant (No. P30 CA008748).
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Barrio, A.V., Eaton, A. & Frazier, T.G. A Prospective Validation Study of Bioimpedance with Volume Displacement in Early-Stage Breast Cancer Patients at Risk for Lymphedema. Ann Surg Oncol 22 (Suppl 3), 370–375 (2015). https://doi.org/10.1245/s10434-015-4683-0
Received:
Published:
Issue Date:
DOI: https://doi.org/10.1245/s10434-015-4683-0