-
PDF
- Split View
-
Views
-
Cite
Cite
Calvin K. L. Or, Ben-Tzion Karsh, A Systematic Review of Patient Acceptance of Consumer Health Information Technology, Journal of the American Medical Informatics Association, Volume 16, Issue 4, July 2009, Pages 550–560, https://doi.org/10.1197/jamia.M2888
Close - Share Icon Share
Abstract
A systematic literature review was performed to identify variables promoting consumer health information technology (CHIT) acceptance among patients. The electronic bibliographic databases Web of Science, Business Source Elite, CINAHL, Communication and Mass Media Complete, MEDLINE, PsycArticles, and PsycInfo were searched. A cited reference search of articles meeting the inclusion criteria was also conducted to reduce misses. Fifty-two articles met the selection criteria. Among them, 94 different variables were tested for associations with acceptance. Most of those tested (71%) were patient factors, including sociodemographic characteristics, health- and treatment-related variables, and prior experience or exposure to computer/health technology. Only ten variables were related to human-technology interaction; 16 were organizational factors; and one was related to the environment. In total, 62 (66%) were found to predict acceptance in at least one study. Existing literature focused largely on patient-related factors. No studies examined the impact of social and task factors on acceptance, and few tested the effects of organizational or environmental factors on acceptance. Future research guided by technology acceptance theories should fill those gaps to improve our understanding of patient CHIT acceptance, which in turn could lead to better CHIT design and implementation.
Introduction
In the United States, the need to improve the health care system has led to the launch of a national initiative that stresses the use of health information technologies to enhance quality of care, support health care safety, and provide cost-effective health services for consumers, i.e., patients or individuals who receive medical care.1,2 While much of the discussion has focused on how health care organizations such as hospitals need to adopt health information technologies for patient safety, there is a growing recognition that such technologies can be used directly by consumers to acquire new forms of health care, such as telehomecare. When used by patients, these technologies are referred to as consumer health information technologies (CHITs). Several definitions describing CHITs can be found in the literature. In this review article, CHITs are defined as computer-based systems that are designed to facilitate information access and exchange, enhance decision making, provide social and emotional support, and help behavior changes that promote health and well-being.3–5
There is a considerable body of research testing the feasibility, acceptability, and effectiveness of various CHITs for primary health care service delivery, in general, or patient self-care at home, in particular.6–15 For patient self-care, CHITs facilitate the care process by providing patients with prompt access to their medical history, medication and disease specific information, electronic communication, and decision support services at the point of care.3,13,16–18 These readily available resources can lead to a positive impact on patient health outcomes, quality of life, hospital readmission rates, and mortality rates.15,19–22 Moreover, CHITs are becoming more prevalent, and there are reasons to believe that patients will encounter CHITs for treatment and self-management more and more frequently. The first reason that patients may see an increased opportunity to use CHITs is that CHITs empower patients to participate in information sharing and decision making, which enables them to be more in control and contribute to quality health care.23–25 Second, driven by the high cost of conventional health care, patients are discharged from hospitals quickly once their acute conditions are stabilized. The average length of hospital stay for inpatients has been declining, from 7.3 days in 1980 to 4.8 days in 2004.26,27 Because of that, the patient care environment is being shifted from hospitals to other less costly environments, such as the home,28 where CHITs may be largely used by patients for self-care.
While the potential for using CHITs to improve health care has been acknowledged, these technologies are still not always accepted by patients for variety of reasons, including poor device usability, insufficient training on how to use the technology, lack of computer skills, and low self-efficacy.8,29–34 This is a significant concern for patients and health care organizations; patients who reject CHITs will not benefit from them, and rejection means a loss of return on investment for health care organizations. This concern has been realized. Evidence shows that substantial numbers of potential users do not accept CHITs,35 and this has led to technology implementation failure in several projects.30–33 Therefore, studies that examine variables predicting patient CHIT acceptance are needed. Identifying factors that predict acceptance can (1) help create acceptance for the technology, (2) aid in developing and evaluating the ability of CHIT applications to fulfill patients' needs and expectations, and (3) increase the likelihood of technology implementation success.36 Patients' interest and willingness to use (otherwise known as acceptance) CHITs for managing their illnesses has been a scientific research area of much scrutiny. However, to date no attempt has been made to synthesize and interpret the evidence regarding factors quantitatively predict patient CHIT acceptance. To that end, this review study (1) analyzes and synthesizes variables predicting patient CHIT acceptance, (2) examines major gaps in the current CHIT acceptance literature, and (3) gives direction to future research.
Methods
Definitions
Consumer Health Information Technologies (CHITs), depending on their purposes, may be used by healthy individuals seeking out health information or by ill/injured individuals for treatment and/or self-management. This latter group is our current population of interest because CHIT acceptance may directly affect their health and well-being. We refer to this group actively receiving (medical) care for an injury or illness as patients. “Acceptance” of technology has been defined in four primary ways: (1) satisfaction with the technology, (2) use or adoption of the technology, (3) efficient or effective use of the technology, and (4) intention or willingness to use the technology.36–40 Therefore, our definition of CHIT acceptance is limited to those four conceptualizations. As described earlier, consumer health information technologies on which this article focuses are patient-oriented computer-based systems used to promote health, well-being, and safety, including telemedicine, e-health, and Web-based health technologies.
Search Strategy
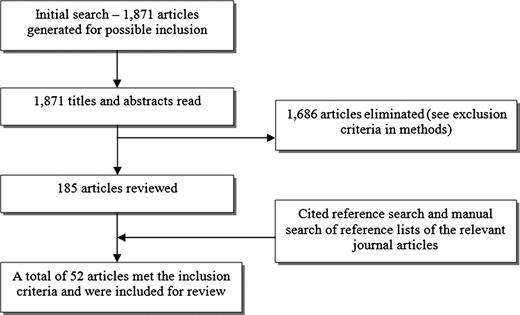
Figure 1. shows the literature search procedure. Online database literature searches were performed in early Dec 2006, and again in Feb 2009 to obtain relevant research articles to review. The electronic bibliographic databases used for searching were Web of Science, Business Source Elite, CINAHL, Communication and Mass Media Complete, MEDLINE, PsycArticles, and PsycInfo. The search terms employed were patient*, senior*, elder*, old*, disabilit*, accept*, abandon*, intent*, intention to use, reject*, satisf*, use*, utiliz*, computer*, eHealth, e-health, e-mail, health* informat*, Internet, technolog*, web*, telemedicine, and combinations of them (e.g., patient e-Health use). In addition to the online database search, we manually searched the following health informatics journals to reduce the likelihood of missing relevant articles: Journal of the American Medical Informatics Association, International Journal of Medical Informatics, Journal of Medical Internet Research, and Telemedicine and e-Health. The literature search strategy used in this review was intentionally broad and covered many types of CHITs. While this is a possible concern, we decided to be broadly inclusive for three reasons. First, it is not known if different variables are important predictors of acceptance for different technologies. A wide net allows us to assess whether the factors that predict acceptance of one CHIT will be the same as others. Second, the extensive research on technology acceptance outside of health care covering many different information technologies has demonstrated consistent predictive factors. Third, a broad search was conducted because the objective of this review was to identify any existing research examining CHIT acceptance by patients. After the initial screen of articles, a cited reference search of all articles initially considered was used to further reduce the likelihood of missing relevant articles. This method used a search algorithm in Web of Science to identify all articles that have cited another article. Additional articles found using the cited reference search were screened.
Flow diagram of the selection process for including articles in review.
Inclusion and Exclusion Criteria
For studies to be eligible for inclusion in this review, they had to meet the following criteria: (1) the study was empirical with a substantive focus on quantitatively determining variables associated with acceptance of CHITs; (2) the objective of the CHIT was to promote health, well-being, or quality of life or facilitate the care delivery process or self-care of individuals; (3) individuals studied in the research were patients; (4) the article was written in the English language; and (5) the article was published in a peer-reviewed journal or one of the following conference proceedings, selected because of their high likelihood of containing relevant research: proceedings of American Medical Informatics Association symposium, the International Congress on Medical Informatics (MEDINFO), and ACM/SIG Computer-Human Interaction.
Because this review study examined empirical findings about predictors of patient CHIT acceptance, we excluded review papers, theoretical and conceptual articles, editorials, and letters. Example reasons for excluding studies were as follows: (1) the study did not examine factors predicting CHIT acceptance, (2) the study involved healthy individuals (e.g., Internet users or adults in general), (3) the question employed to measure CHIT acceptance did not distinguish if the technology was used by patients or their family members, (4) the purpose/use of the technology was not reflective of health-related usage, or (5) surrogates (most commonly friends or family) used the technology on behalf of the patients. We acknowledge that the acceptance among surrogates of patients is an important category of consumer-driven technology; however the focus of this review is acceptance by patient themselves.
Analysis
The conceptual frameworks developed by Karsh and Holden36,41,42 from reviews of health information technology acceptance literature were used to synthesize the findings. These frameworks demonstrate that health information technology acceptance has been predicted by variables related to (1) the individual user, (2) human-technology interaction, (3) the tasks that the technology is used to perform, (4) characteristics of the organization with which the user interacts, (5) social factors, and (6) environmental factors. Individual factors refer to sociodemographic variables, personality traits, and health status variables. Human-technology interaction factors refer to usability characteristics of a technology or a person's feelings, perceptions, or beliefs about a technology. The task category refers to characteristics of a task such as efficiency or accuracy, and perceptions of those task characteristics. Organizational factors concern organizations' resources (e.g., training, service providers' support), processes (e.g., end user participation), and structures (e.g., organizational hierarchy) and the user's perceptions of them.41,43,44 Finally, environmental factors that may affect acceptance include variables such as layout, space, or lighting of the physical environment where the technology is used. The frameworks further explain how the interaction among the predictor variables impacts the extent to which the technology fits with the needs of the user, and that fit determines acceptance and subsequent use. These six categories of predictors were used to synthesize and organize the results and discussion.
Results
The search returned 1,871 articles and their titles and abstracts were read. Based on the selection criteria, 185 articles were retained for more detailed review. Fifty-two articles met the criteria and were included in this review study.
Of the 52 studies reviewed, the majority examined the use of health-related Internet sites for health issues and information (n=35).29,45–78 Six studies applied telemedicine to different types of medical consultation, including three applications to clinical consultation, one to dermatology, one to home health care, and one to prison inmates with various conditions.79–84 Nine studies examined computer- or Web-based health and decision support systems that offered electronic personal health records, social support, medical advice, decision aids, drug refill features, electronic communication, health assessment resources access, and/or self-management tools.6,9,85–91 Two studies tested Internet-based secure e-mail applications for patient-provider electronic communication.92,93 Table 1 (available as an online data supplement at http://www.jamia.org) illustrates the designs and characteristics of the 52 studies. Among the studies, 41 (79%) used a cross-sectional design. Our review found that the 52 studies measured acceptance in various ways, which could be classified into six groups (see Table 2). Most studies measured acceptance by self-reported use of the system.
Approaches Used to Measure Acceptance in the 52 Studies
| Measurement Approach | Number of Study |
| Self-reported use | 30 |
| Self-reported interest in using or intention/willingness to use | 8 |
| Self-reported acceptability/satisfaction level | 6 |
| Objective measure of use | 5 |
| Both self-reported use and intention to use | 2 |
| Both objective measure of use and self-reported intention to use | 1 |
| Measurement Approach | Number of Study |
| Self-reported use | 30 |
| Self-reported interest in using or intention/willingness to use | 8 |
| Self-reported acceptability/satisfaction level | 6 |
| Objective measure of use | 5 |
| Both self-reported use and intention to use | 2 |
| Both objective measure of use and self-reported intention to use | 1 |
Approaches Used to Measure Acceptance in the 52 Studies
| Measurement Approach | Number of Study |
| Self-reported use | 30 |
| Self-reported interest in using or intention/willingness to use | 8 |
| Self-reported acceptability/satisfaction level | 6 |
| Objective measure of use | 5 |
| Both self-reported use and intention to use | 2 |
| Both objective measure of use and self-reported intention to use | 1 |
| Measurement Approach | Number of Study |
| Self-reported use | 30 |
| Self-reported interest in using or intention/willingness to use | 8 |
| Self-reported acceptability/satisfaction level | 6 |
| Objective measure of use | 5 |
| Both self-reported use and intention to use | 2 |
| Both objective measure of use and self-reported intention to use | 1 |
The effects of 94 different factors on patient CHIT acceptance were tested in the 52 studies reviewed. Those factors were related to patients (such as sociodemographic characteristics, health- and treatment-related variables, and prior experience or exposure to computer/health technology), human-technology interaction, the organization, or the environment. This review showed that 67 (71%) of the 94 factors tested were patient factors. Of those 67 patient factors, 37 were related to patients' health or their treatment in some way; and 30 were sociodemographic or related to the individual's prior experience or exposure to computer/health technology. Ten (11%) and 16 (17%) of the 94 factors examined were human-technology interaction and organizational factors, respectively. Human-technology interaction factors included perceived usefulness, perceived ease of use, Internet dependence, self-efficacy toward computer/CHITs, computer anxiety or fear of technology, intrinsic motivation, perceived reliability/exactitude of the health information, belief that the use of CHITs can lead to positive outcomes, technology quality and set-up time, and technology as support. Organizational factors included satisfaction with medical care services or health plan, satisfaction with the amount of disease treatment-related information given by the physician, difficulty obtaining necessary health care access, and Internet skill training. One type of environmental variable was tested–patient location when using the CHIT. No variables were tested that fit into the categories of task or social factors. Overall, of the 94 variables tested for their associations with acceptance, 62 (66%) were found to predict acceptance in at least one study. Table 3 (available as an online data supplement at http://www.jamia.org) shows which patient, human-technology interaction, organizational, and environmental factors predicted acceptance of CHIT.
Discussion
The purpose of this study was to systematically review empirical studies of patient CHIT acceptance to examine factors that predict acceptance and determine directions for future research. Ninety-four different variables were tested for associations with acceptance. The current literature largely focuses on patient factors such as sociodemographic, health, and treatment-related variables. This focus may be insufficient to really understand and explain patient CHIT acceptance or to guide CHIT implementation.41,94 Few organizational variables were tested, fewer human-technology interaction or environmental variables were examined, and no task or social variables were studied. Successful technology implementation requires an understanding of how different system factors—individual, human-technology interaction, organizational, social, task, and environmental—affect acceptance.41 Furthermore, most studies failed to employ any theory or framework to guide the selection of acceptance factors to explore, perhaps explaining why 94 different predictors of acceptance were tested. The exceptions were Boberg et al,6 Lu and Gustafson,9 Wilson and Lankton,87 Lai et al,91 and Klein.92
Patient Factors
Age was examined in 39 studies and did not show a consistent effect. Among those 39 studies, 26 (67%) found significant relationships and 13 did not. Among the 26 studies with significant relationships, only one showed that higher age was associated with increased acceptance, 19 found that age was negatively associated with acceptance, and six found a nonlinear relationship. Gender, the second most studied variable, demonstrated no effect in 84% of the studies that tested the variable. Education, examined in 28 studies, fared better; 68% of those studies found that acceptance increased with higher education. Prior experience or exposure to computer/health technology appears to be associated with increased acceptance. Twenty studies examined the effects of different dimensions of prior experience or exposure to computer/health technology (i.e., computer ownership, computer use in the past, use of the Internet, previous awareness of health Web site or health technology, and having Internet access at home), 15 found that prior experience was associated with increased acceptance. The rest of the sociodemographic variables were either examined in too few studies to draw conclusions or the results were mixed. Similarly, the 28 health status variables listed in Table 3 were typically examined in only one study. The same can be said for the nine treatment-related variables. Any conclusions made based on these findings should be drawn with caution.
This raises another interpretive issue, though; what might be the mechanism by which many of the patient factors affect acceptance? Technology acceptance studies in the field of information systems have suggested that age, gender, education level, computing experience, and voluntariness of use moderate the effects of performance expectancy, effort expectancy, subjective norm, and computer anxiety on acceptance.38,95–97 However, no studies reviewed tested the interactions among those variables, and no studies measured voluntariness of use. Although age did not reveal a consistent effect, among the studies finding age as a significant factor, it appears that, in general, older adults are less likely to accept CHITs. This could possibly be due to less computer familiarity or literacy among older patients,34 which can result in negative attitudes toward computing technology. Previous studies of information technologies have showed that, relative to younger adults, older adults perceived less comfort, efficacy, and control over computing technologies.98–100 Those negative perceptions in turn can decrease acceptance.29,101
Most of the studies that tested the effect of gender demonstrated that gender had no direct impact on acceptance. However, studies of other types of technologies have found that gender was a significant moderator of computer anxiety and perceived behavioral control. Perceived behavioral control refers to individuals' perceptions of internal and external constraints on using a technology: (a) internal constraints such as being able to use the technology or perceiving that use of the technology is within the individual's control, and (b) external constraints such as the availability of resources needed to engage in the behavior.102,103 Previous studies demonstrated that women were more likely to report higher computer anxiety than men,104,105 and perceived behavioral control was more salient for women in the early stages of experiencing technology.106,107 Such results suggest the need for more complex modeling to better understand the role of gender in CHIT acceptance, where gender might moderate the relationships between certain predictors and acceptance.
The role of patient health status in CHIT acceptance also needs more study. Chae et al82 showed that better health (less severely ill patients) was associated with increased acceptance; however, Jennot et al67 and Millard and Fintak49 found that poorer health (more severely ill patients) was associated with increased acceptance. Perhaps health status is actually acting as a proxy for other more salient variables, such as physical, visual, or cognitive functional abilities. Studies showing that physical, visual, and cognitive limitations are associated with decreased acceptance provide possible evidence for that hypothesis.86,90 Future studies need to incorporate those more complex mediated pathways to determine if health status is a proxy for those functional abilities.
Our review found religious preference, having school age children at home, marital status, and bariatric patients compared to colorectal patients, for example, predicted CHIT acceptance. But it is unclear what the mechanisms for the relationships are. Having school age children at home might lead to more computer experience and less computer anxiety among parents who are patients, but the mechanisms for the others are not clear. It is possible that these measured variables were acting as proxies for other more direct mechanisms such as subjective norm, perceived usefulness, or support, but in the absence of clear theoretical guidance or testable models, this remains speculation.
Human–Technology Interaction Factors
Davis' Technology Acceptance Model37 has been one of the most influential theories for studying acceptance with diverse types of information technologies and population (including CHITs and patient population).6,9,87,108 The model posits perceived usefulness and perceived ease of use as the main predictors of technology acceptance. Interestingly, even though those two variables are the most reliable predictors of technology acceptance,36–38,40,41 only 7 of the 52 patient CHIT studies explored their effects. Computer/technology self-efficacy, another reliable predictor of technology acceptance,101,109–111 was only examined in two studies. With two exceptions, all studies that tested the influences of usefulness, ease of use, and computer/technology self-efficacy demonstrated that those variables were significant predictors of acceptance. Furthermore, most other human-technology interaction variables also predicted acceptance. Computer anxiety was tested in 3 of the 52 studies, and all three studies indicated that computer anxiety was negatively associated with acceptance. Computer anxiety refers to a negative affective reaction toward computers such as apprehension or fear of using computers.112,113 Feelings of anxiety surrounding computers can be negatively associated with perceived ease of use, and in turn influence acceptance.110,112,114,115 Future CHIT acceptance research should, at minimum, measure perceived ease of use and usefulness and incorporate them into models to avoid misspecification and to help explain CHIT acceptance.
Organizational Factors
Fifteen studies examined organizational factors. Organizational factors that were found to lead to increased acceptance included being less satisfied with medical care services, being less satisfied with one's health plan, being less reliant on others for transportation, having Internet skill training, being less satisfied with the amount of disease treatment-related information given by physician, having a regular primary care provider, attending one of the two study hospitals, being in an academic medical center (vs. veterans affairs hospital), having difficulty accessing necessary health care, having more trust in one's health care provider, having more trust in the technology vendor, and having a higher external control belief. Each of those variables was tested in only one study, except the effects of being in an academic medical center and satisfaction with medical care services, which were examined in two and three studies, respectively. For satisfaction with medical care services, while a study demonstrated that the factor was negatively associated with acceptance, two other studies found no association. Future patient CHIT acceptance research should further explore the role of trust in acceptance; while there is not much research in CHIT trust to date, the little research that does exist suggests it is an important variable,35,116 and this is supported by a considerable amount of research on trust and technology outside of health care.117–122
In addition, literature suggests there may be other important organizational variables to examine, such as organizational support, organizational justice, satisfaction with training, technical support, and end user participation.36,123–127 These have all received empirical support in literatures outside of consumer health informatics, and there are reasons to hypothesize they would be important here too. Igbaria et al126 described that higher levels of organizational support, which in the case of patients could be support from their clinic or hospital, are believed to promote more favorable beliefs about the technology, which could then improve acceptance. Nurse training of patients or technical help lines for patients may influence acceptance through perceived ease of use, perceived usefulness, and self-efficacy. Organizational justice123,127 could influence acceptance to the extent that patients believe that they are (un)fairly required to use CHITs, or that the methods used to install the CHIT and train them to use the technology were (un)fair. The CHITs might also change the organization of patient's daily lives or daily routines. If those changes are large, and the large changes are perceived as introducing extra workload with low utility, acceptance could be impacted.
Environmental Factors
Only one type of environmental variable (i.e., patient location when using the technology) was examined in two of the studies reviewed. Chae et al81 examined patient satisfaction with telemedicine for home health care patients; their study demonstrated that patients at home were more satisfied with the technology than patients in nursing homes. Similarly, Mekhjian et al84 also found that patient location was a significant factor. However, several environmental factors that were not explored in the literature may also be important for patient CHIT acceptance. Environmental factors refer to the physical aspects of the environment; for example, when CHITs are designed to be used at home, the environment can be the residential living space where the patient interacts with the technology. Environmental factors are important because they will impede or facilitate individuals' abilities to use technology effectively and efficiently,128,129 which in turn can influence technology acceptance of the individual. Lighting, noise, temperature, housekeeping, and air flow might all affect CHIT acceptance.128,129 Poor lighting could cause readability problems and physical discomfort when using a computer-based (health) information system.129 Other factors such as noise and thermal discomfort, which can cause sensory disruption, also hold relevance in CHIT acceptance. For instance, having a medical consultation with a health care provider at a remote site using an interactive telemedicine can be challenging when the device is used in a noisy household area. As a result, noise may influence acceptance directly or through the individual's perceptions or attitudes toward the technology, such as perceived ease of use, perceived usefulness, or affect. These additional environmental factors should be taken into account in future CHIT acceptance research.
Social Factors
Social factors, which have played a prominent predictive role in technology acceptance studies outside of health care, were not examined in any study reviewed. Thompson et al130 (p. 126) defined social factors as “the individual's internalization of the reference groups' subjective culture, and specific interpersonal agreements that the individual has made with others, in specific social situations.” That is, social factors concern the influences of others/groups to which one belongs.41 Although a study reviewed claimed to test the effect of subjective norm, it was actually operationalized by patients' gender and race.91 In the Unified Theory of Acceptance and Use of Technology (UTAUT),38 developed from the Technology Acceptance Model,37 there are four categories of variables that influence information technology acceptance: performance expectancy, effort expectancy, facilitating conditions, and social influence. The first two involve perceived usefulness and perceived ease of use, respectively, both of which were examined in the reviewed literature, albeit in few studies. However, the variable category of social influence, which was also represented as social factors or reference group culture in Thompson et al,130 subjective norm in Ajzen131 and Taylor and Todd,102 and image in Moore and Benbasat,132 was not explored. In other health care delivery contexts social factors have been found to predict acceptance of information technology. For example, Yi et al133 found that physicians' acceptance of a personal digital assistant, a handheld computer that was used to support clinical practice, was significantly affected by subjective norm (e.g., their supervisors or colleagues who are important to them). Others have also found social factors to be important predictors of health information technologies,134 but the results are not always consistent.135,136 Among the reviewed studies, Boberg et al6 did not test the impact of subjective norm, but in their conclusion, they emphasized the need for testing the relationship between subjective norm and patient acceptance in future research. Based on the theories and empirical studies that suggest the impact of social factors on acceptance, we believe that social factors are also particularly important in the context of patient CHIT acceptance. Patients might be more or less likely to accept CHIT depending on, for example, the extent to which their physician, home care nurse, children, or grandchildren urge them to use it.
Task Factors
Just as the introduction of a new technology in a work organization will lead to changes in the nature of the tasks supported by the technology (e.g., demand on the users and time spent on the new technology),36,137 the implementation of CHITs will also alter the way patients perform disease management and self-care. For example, in the absence of computers, tools used by homebound patients for health management are mainly paper based, such as calendars, phone books, and papers, and those tools are often kept in kitchens, bathrooms, and bedrooms for future use.138 With CHITs, the same types of tools become electronic. This can change the nature of disease management and self-care in many ways, which in turn can influence perceptions and attitudes toward the technology.36,137 The literature outside of health care revealed that individuals were more likely to demonstrate negative perceptions about a new technology when the technology caused a greater change in the nature of the task.36,137 In this review, we did not find any study that examined the effect of task factors on patient CHIT acceptance; however, future research is needed to understand the impact.
Implications for Design
That so many variables empirically demonstrated to impact acceptance were not included in studies of patient CHIT acceptance leads to a concern about model misspecification139 and therefore result interpretation. In the previous paragraphs, many directions for future research were proposed to help address this problem. In particular, it is worth repeating here the need that future patient CHIT acceptance studies should, at least, incorporate possible moderators, such as age, gender, education level, computing experience, and voluntariness of use,38 to better understand the interactions between various predictors and acceptance. There is also a need to study the influence of task and social variables, as well as other organizational, environmental, and human-technology interaction variables.
There are also implications for CHIT design and implementation that apply to diverse patient populations. For instance, in all cases, system developers should pay attention to task-technology fit140 as well as system user-friendliness, which can help create the perception of system usefulness and ease of use. However, our findings are perhaps especially important for elderly patient users because of their unique characteristics. Also, since the current effort in CHIT development largely focuses on patient populations that are mostly older adults (e.g., chronically ill patients),33,35,141–143 in the paragraphs that follow we discuss implications related to aging and elderly patients.
The articles in this review showed mixed results regarding the association between age and acceptance; however, more studies showed negative associations. Plausible mechanisms exist to explain why older age may represent a barrier to acceptance.98,144–147 Understanding these mechanisms is particularly important for those who want to design a system for an elderly population or a patient population such as heart failure patients who are mostly elderly. Czaja et al148 found that adults over 65 years of age have fewer computer skills and have less computer self-efficacy than younger adults. Evidence has demonstrated that lack of computer skills and computer self-efficacy could lead to less use or less intention to use computer technology. Skill-based training may be one way to improve skills and self-efficacy. Although older individuals may perceive the learning of new skills as an obstacle, in the current review, we found that the provision of computer and Internet skills resulted in greater acceptance of the technology.46 Evangelista et al149 also demonstrated that elderly patients with limited computer skills can and will use CHITs when sufficient instructions on how to use the technology were provided.
Moreover, older adults may have very different characteristics than younger adults in terms of functional abilities as well as attitudes and beliefs. Relative to younger adults, older adults are likely to perceive more anxiety, less comfort, lower efficacy, and less control over computers.148,150,151 Furthermore, the use of CHITs by older adults could be restricted by several constraints such as motor limitations, perceptual limitations, cognitive limitations, external limitations, and general health limitations.150,151 Older adults or elderly patients who feel anxiety, apprehension, or less control over computers or who are physically, cognitively, or perceptually limited would have more difficulty using the technology. Therefore, when designing generic technologies or health technologies for patients, in general, or elderly patients, in particular, it is important to understand and address their characteristics, needs, abilities, and preferences in the design of the technology to improve the fit between the technology and the users.
Study Limitations
This review study has several limitations. First, studies focusing on healthy individuals using CHIT were excluded. As such, the conclusions may not be generalizable to CHIT acceptance in general, just to CHIT used by patients. Second, studies focusing on surrogates using CHITs on behalf of patients were also excluded. Acceptance among this population is very important as many patients have family, friends, or caregivers who might access technologies relevant to the patient's care. However, what drives acceptance among those groups might reasonably differ from what drives patients' acceptance, and so the exclusion was necessary to maintain a more homogenous set of studies. Third, this review included studies of many different kinds of CHITs used by patients. We could have limited the review, for example, to only telemedicine or only computer-based health support applications. However, theoretically there was no reason to exclude one type of CHITs or the other. Fourth, in the review, a single reviewer identified articles meeting the inclusion and exclusion criteria. Multiple reviewers may have reduced bias. Fifth, while the manual searching of specific journals and conference proceedings could reduce the likelihood of missing relevant articles, it could also introduce bias. Finally, no formal meta-analysis was conducted; therefore, the ability to make clear conclusions about the relative importance of each variable is limited.
Conclusions
The purpose of this review was to examine factors that determine patient CHIT acceptance based on the empirical findings in the literature. The review examined 52 studies, and 94 different predictors of acceptance were tested in the studies reviewed. Variables that were associated with CHIT acceptance were related to patient, human-technology interaction, the organization, and the environment. None of the studies examined whether social or task variables might predict acceptance. Most of the studies were atheoretical, left out reliable predictors of acceptance, and did not test possible mediators and moderators that could help explain findings. This is a problem that needs to be solved; CHITs will increasingly be used to support treatment, disease management, and patient self-care, so the stakes are high.
Evidence does show that CHITs can improve patients' quality of life and well-being, and increase medication adherence.15,152–154 However, technologies cannot help facilitate self-monitoring and self-management or improve patients' health outcomes when patients do not accept the technology. Further, current CHIT users may abandon CHITs when they perceive the technology as disadvantageous or functionally incompatible with their needs, existing values, or past experiences.31,32 Therefore, in order for any patient health information technologies to be successfully implemented, the needs of patient end-users (physical, psychological, and social) must be adequately met and addressed.155,156 Consumer Health Information Technologies system developers and those who implement the systems should also pay attention to the underlying reasons and motives for patient acceptance of the technology. By understanding a priori what factors are important in predicting patients' willingness to use health technology, system developers can focus their efforts on those factors when designing the system or developing strategies to promote acceptance and adoption of CHITs. That will require future research on CHIT acceptance to consider a variety of theoretically relevant individual, human-technology interaction, organizational, social, task, and environmental variables.
References
Footnotes
This study was funded in part by a grant from the National Library of Medicine (NLM-LM 6249) to Patricia Flatley Brennan, PI. The authors thank Samuel Alper, Richard Holden, and A. Joy Rivera for their helpful comments on the earlier versions of the manuscript and thank the anonymous reviewers for their helpful comments.