Abstract
Objective
To review published evidences about using information technology interventions in diabetes care and determine their effects on managing diabetes.
Design
Systematic review of information technology based interventions.
Research design and methods
MEDLINE®/PubMed were electronically searched for articles published between 2004/07/01 and 2014/07/01. A comprehensive, electronic search strategy was used to identify eligible articles.
Inclusion criteria were defined based on type of study and effect of information technology based intervention in relation to glucose control and other clinical outcomes in diabetic patients. Studies must have used a controlled design to evaluate an information technology based intervention.
A total of 3613 articles were identified based on the searches conducted in MEDLINE from PubMed. After excluding duplicates (n = 6), we screened titles and abstracts of 3607 articles based on inclusion criteria. The remaining articles matched with inclusion criteria (n = 277) were reviewed in full text, and 210 articles were excluded based on exclusion criteria. Finally, 67 articles complied with our eligibility criteria and were included in this study.
Results
In this study, the effect of various information technology based interventions on clinical outcomes in diabetic patients extracted and measured from selected articles is described and compared to each other.
Conclusion
Information technology based interventions combined with the usual care are associated with improved glycemic control with different efficacy on various clinical outcomes in diabetic patients.
Similar content being viewed by others
Introduction
According to International Diabetes Federation (IDF) report, Diabetes Mellitus is a pervasive chronic disease affects 382 million people worldwide and more than 592 million people will be affected within a generation. However most of those cases would be preventable [1].
Diabetic patients with poor blood glucose control have higher mortality and morbidity rate which is related to chronic complications such as neuropathy. Diabetes is a leading cause of death due to increased risk of coronary artery disease and stroke [2].
The estimated total cost of diabetes care in the world was at least USD 548 billion in 2013. This estimation is expected to be more than USD 627 billion for 2035 [1].
A number of information technology based interventions were applied to enhance blood glucose monitoring and diabetes management. Previous evidence demonstrates that information technology can improve diabetes management through better metabolic control and help in the global care of diabetic peoples with chronic illnesses [3–5].
As Marcolino et al. presented in their systematic review and meta-analysis, Telemedicine was associated with a statistically significant and clinically relevant decline in HbA1c level compared to control unlike LDL and blood pressure reduction [6]. Also, according to Siriwardena et al.’s study, Telemedicine appears to be a promising alternative to conventional therapy in diabetic care [7].
Adaji et al. performed a literature review about the use of information technology to enhance diabetes management. They concluded that promoting a productive and informative interaction between the patient and the care team by using information technology based interventions can lead to improve diabetes care [8].
Information technology based interventions have some advantages such as reducing medical errors, generating potential data for research, and increasing the ability for continuous improvement. On the other hand, higher cost of initially and maintenance activities, difficulty of using computer and information systems for healthcare providers and spending more time than interacting with a patient are some disadvantages of using information technology in diabetes care [9, 10].
In this regards, there are some questions: Which intervention is more effective on managing diabetes especially on HbA1C reduction? Is there any relation between type of diabetes and effect of specific intervention? What are the style and variation of interventions in previous studies of using information technology for managing diabetes?
This study was designed in order to perform a comprehensive review of information technology based interventions in diabetes care domain. The purpose of present study was to review published evidences about using information technology in diabetes care and determine the effect of interventions on managing diabetes, includes HbA1C reduction and other clinical outcomes.
Research design and methods
Search methods
A literature search was performed in September 2014 using MEDLINE/PubMed database to identify relevant studies published in last ten years from 2004/07/01 to 2014/07/01.
Combination of the following MESH terms and keywords (all fields) were used:
-
(("Diabetes Mellitus"[Mesh]) or (Diabetic)) and (("Medical Informatics"[Mesh]) or ("information system") or ("mobile health") or ("electronic health") or ("electronic patient record") or ("electronic medical record") or ("information technology") or ("decision support system") or ("diabetes registry") or ("computerized physician order entry") or ("computerized provider order entry") or ("information network") or ("computer aided diagnosis") or ("computer aided therapy") or ("communication technology") or (telemedicine) or (telehealth) or (sms) or ("short message service") or (telenursing) or (telecare) or (teleradiology))
We did not set another search limits based on study design, study outcome, language or peer-reviewed journals. References of identified articles were also searched for potential articles.
Inclusion criteria and study selection
Inclusion criteria were defined based on type of study and beneficial or harmful effect of information technology based intervention in relation to glucose control and other clinical outcomes in diabetic patients. The full text of article must be exists and accessible.
Type of information technology based interventions included in this review were as the follows: (1) Telephone coaching, (2) Clinical Decision Support System, (3) Electronic Medical Record/Electronic Health Record, (4) Distance Learning, (5) Computerized Insulin Dose Adjustment, (6) Personal Health Record, (7) Mobile Health/Short Message Service, (8) Telemedicine/Telehealth.
Interventions must aim to improve or promote diabetic care using any information technology based solutions including: (1) interventions designed to improve treatment, monitoring, and management of diabetes. (2) interventions to deliver treatment, education or other diabetes management programs to patients.
We classified the studies according to the hierarchy of study designs developed by the University of California San Francisco Stanford evidence-based practice center and implemented by Kaushal et al. [11] into the following items: Randomized controlled trial (RCT), Non-randomized controlled trial (NRCT), Observational study with control (OS), Observational study without control (OSWC).
Studies must have used a controlled design to evaluate an information technology based intervention. We included all of RCTs, NRCTs and Observational studies with control.
Original articles included in this study. On the other hand, letters (n = 2), opinion papers (n = 10), reviews and studies that reported preliminary data of another included study (n = 46) were not included.
Titles and abstracts of identified articles were screened based on inclusion criteria described above. Full texts of potentially eligible articles were then reviewed. Two of reviewers independently did review, coding and abstracting information from each article. Any discrepancies between the reviewers were resolved through discussion and reference to the original articles.
Exclusion criteria were as follows: (1) case reports or case series with fewer than 10 patients, (2) studies with less than 3 months of follow-up and (3) information technology is not the primary intervention component or information technology based intervention had not implemented (e.g., study protocols).
We did not exclude children with diabetes or pregnant women with gestational diabetes.
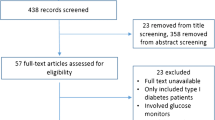
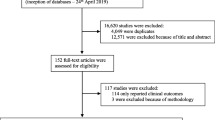
As shown in Fig. 1, a total of 3613 articles were identified based on the searches conducted in MEDLINE from PubMed. After excluding duplicates, we screened titles and abstracts of 3607 articles based on inclusion criteria. (Kappa agreement index = 0.73).
The remaining articles matched with inclusion criteria (n = 277) were reviewed in full text, and 210 articles were excluded based on exclusion criteria. Finally, 67 articles complied with our eligibility criteria and were included in this study. (Kappa agreement index = 0.81).
Quality assessment
As described above, studies had not control group, population with less than 10 patients or with less than 3 months of follow up, were excluded.
Out of the remained studies, 52 items were randomized controlled trials and three of studies were non randomized controlled trials. Another 11 studies were observational study with control.
Data extraction
Titles and abstracts of all selected studies were reviewed independently by two reviewers. Papers identified as relevant or of uncertain relevance based on the abstracts were further independently evaluated by both reviewers. Any discrepancies between the two reviewers were resolved by discussion. Reasons for exclusion were documented according to the exclusion criteria.
The data extraction and quality assessment of the studies were performed by the first author and individually checked by second one for accuracy and to identify missing information.
A data extraction form was developed, piloted, and used to extract data which was a modified version of the template form suggested by the Center for Review and Dissemination guidance for systematic review [12]. This form contains following items:
-
(1)
article properties e.g. title and UID;
-
(2)
study attributes e.g. population, duration of follow, mean age and gender;
-
(3)
research type include RCT, NRCT, Other Observational study with control and Observational study without control;
-
(4)
intervention type according to the description of inclusion criteria;
-
(5)
diabetes type (I, II, GDM, unknown or mixed); and
-
(6)
outcomes according to the American diabetes association recommendations for diabetes management [13].
All of extracted data were organized into a single spreadsheet for easier analysis.
Data-synthesis and analyses
Meta-analysis was not carried out because of the variability of the outcome measures and the heterogeneous nature of the interventions. Therefore, a narrative synthesis carried out based on the interventions, and textual description clustered on the basis of outcome.
The outcomes were effect on the following items:
-
(1)
Glycaemic control (changes in HbA1c as the main indicator of treatment effectiveness in diabetic patients [13], and effect on patient self-monitoring of blood glucose (SMBG) or frequency of blood glucose testing)
-
(2)
pharmacological and overall approaches to treatment
-
(3)
diet and healthy eating
-
(4)
DSMS (Diabetes self-management education and support)
-
(5)
physical activity
-
(6)
blood pressure control (changes in systolic and diastolic blood pressure)
-
(7)
lipid management (effect on blood levels of LDL)
-
(8)
foot care
Results
Description of included studies
Articles were published between 2004/07/01 and 2014/07/01. 12 studies involved a population with type 1 diabetes, and 34 with type 2. A total of 8 studies included a mixed population while type of diabetes was not reported in 13 studies. Table 1 shows the frequency of interventions were applied in studies.
The summation of total diabetic patients were participated in 67 studies that included in final review was 51,155 persons (mean = 786, median = 137) and the mean age of them was 59.5 years. The proportion of male gender in this population was 46 % and the mean duration of follow was 14 months.
Results are described mainly based on outcomes in regard to the recommendations for managing diabetes noted by the American diabetes association [13]. Below, we describe the effects per outcome group for all included studies. Table 2 shows a summary of all reported measured effects of these 67 studies where results are reported separately by outcome group and study design.
Glycaemic control
Fifty seven studies assessed the effect of information technology strategies on HbA1c. Forty studies (70.2 %) Included 29 RCTs, 1 NRCTs and 8 observational studies with control demonstrated a significant reduction in HbA1c. Other seventeen studies (29.8 %) included 14 RCTs, 2 NRCTs and 1 observational study with control did not find a statistically significant difference between the control and the intervention group with regard to HbA1c reduction. But HbA1c decrease was seen in intervention groups in most studies. It seems most information technology based interventions had a great positive effect on glycaemic control [14–68].
In type I diabetic population, computerized insulin dose adjustment (n = 1, 100 % positive effect), and also distance Learning (n = 5, 83.3 % positive effect) and Telemedicine/Telehealth (n = 14, 82.4 % positive effect) in both type I and type II diabetic population were effective interventions in reducing HbA1c compared with other information technology strategies. On the other hand, telephone coaching and EHR had less effect on HbA1c reduction.
Pharmacological and overall approaches to treatment
Six articles were classified in this group. Five studies contained 3 RCTs, 1 NRCT and 1 observational study with control indicated a significant positive changes on medication status for all interventions included CDSS (n = 1, 100 % positive effect), PHR (n = 1, 100 % positive effect), mHealth (n = 1, 100 % positive effect) and Telemedicine/Telehealth (n = 3, 66.7 % positive effect). Five of those studies were done in diabetic type II population and 1 was done in both of type I and type II population [14, 17–19, 69].
Diet and healthy eating
Three articles include 2 RCTs and 1 observational study with control was classified in this group. Two studies indicated significant positive changes on diet status and healthy eating. Both of them applied a Tele-care intervention. According to those studies, Telephone coaching (n = 1) and Telemedicine/Telehealth (n = 1) had a positive effect on diabetic patient’s diet [15, 16, 69].
Another study had used a CDSS for patients and providers. This study demonstrated no changes in diet status and healthy eating in type I and type II diabetic population. As noted by authors, delivering the decision support outside of the point of care and being the intervention untimely may be led to obtain negative findings [16].
Diabetes self-management education and support (DSMS)
Ten studies assessed the effect of information technology strategies on patient empowerment, knowledge and promoting DSMS. Eight studies (80 %) Included 6 RCTs and 2 observational studies with control demonstrated a significant positive effect on DSMS. Other 2 RCT studies (20 %) did not find a statistically significant difference between the control and the intervention group with regard to effect on DSMS. But increasing patient knowledge was seen in intervention groups in both studies. It seems most information technology based interventions had a great positive effect on DSMS [15, 18, 20, 25, 35, 50, 52, 60, 68].
In both type I and type II diabetic population, Telemedicin/Telehealth (n = 4, 100 % positive effect), and mHealth (n = 2, 100 % positive effect) and also CDSS (n = 1, 100 % positive effect) in type II and EHR (n = 1, 100 % positive effect) in type I diabetic population were effective in promoting DSMS and patient knowledge. But telephone coaching has no positive effect on patient empowerment [25, 60].
Physical activity
Nine articles were classified in this group. Six studies contained 5 RCTs and 1 observational study with control indicated significant positive changes on patient’s physical activity status and other 3 RCT studies demonstrated no changes [15, 16, 18, 25, 32, 45, 52, 69].
As noted in these studies, telephone coaching (n = 2, 50 % positive effect) had a positive effect on physical activity changes only in type II diabetic population. In both type I and type II diabetic population, Telemedicin/Telehealth (n = 3, 66.6 % positive effect), CDSS (n = 2, 100 % positive effect) and mHealth (n = 1, 100 % positive effect) were effective in patient’s physical activity status [25, 69].
Blood pressure control (changes in systolic and diastolic blood pressure)
Seventeen studies assessed the effect of information technology strategies on blood pressure control. Ten studies (58.8 %) Included 9 RCTs and 1 observational study with control demonstrated a significant reduction in systolic and diastolic blood pressure. Other 7 RCT studies (41.2 %) did not find a statistically significant difference between the control and the intervention group with regard to blood pressure reduction. Although more marked effects were seen among patients with worse baseline levels [30].
Telephone coaching (n = 1, 100 % positive effect), and CDSS (n = 3, 66.7 % positive effect) and PHR (n = 2, 50 % positive effect) and Telemedicine/Telehealth (n = 9, 66.7 % positive effect) were effective interventions in reducing blood pressure compared with other information technology strategies. On the other hand, EHR and mHealth had no effect on blood pressure reduction. It is notable most studies were applied on type II diabetic population [16, 17, 19, 20, 28–30, 32, 35, 41, 44, 47, 50, 55, 59, 67, 70].
Lipid management (effect on blood levels of LDL)
Twenty articles include 17 RCTs and 3 observational study with control were classified in this group. Ten studies (52.6 %) include 9 RCTs and 1 observational study with control indicated a significant reduction in LDL levels. Other 10 studies include 8 RCTs and 2 observational study with control did not find a statistically significant difference between the control and the intervention group with regard to blood LDL reduction.
According to those studies, Telephone coaching (n = 1, 100 % positive effect), CDSS (n = 4, 75 % positive effect), Distance Learning (n = 1, 100 % positive effect) and Telemedicine/Telehealth (n = 6, 83.3 % positive effect) were effective in reducing LDL levels. On the other hand, EHR, PHR and mHealth had no effect on LDL reduction [16, 17, 19, 28, 29, 32, 39, 41, 43, 46, 47, 49, 55, 57, 59, 63, 64, 67, 71].
Foot care
Four studies assessed the effect of information technology strategies on foot care. Two studies Included 1 RCT and 1 observational study with control demonstrated a significant positive effect on foot care status. Other RCT study did not find a statistically significant difference between the control and the intervention group with regard to foot care status.
In type II diabetic population, EHR (n = 1, 100 % positive effect) and mHealth (n = 1, 100 % positive effect) were effective interventions in foot care compared with other information technology strategies. On the other hand, CDSS had no effect on foot care status in both type I and type II diabetic patients [16, 18, 72].
Discussion
This systematic review (67 studies, 51,155 patients) indicates that in diabetes patients, information technology based interventions are associated with HbA1c decrease when compared to the usual care alone. HbA1c is a valuable indicator of treatment effectiveness in patients with diabetes, because it is correlated with diabetes complications and reflects average glycaemia over several months [13].
Heterogeneity between studies was not formally assessed and the results of studies (in terms of whether there was a benefit associated with the intervention) were grouped together despite differences in study design, participant characteristics, intervention characteristics and outcomes assessed.
This study has a clearly defined search strategy and study selection method. Therefore, the existence of publication bias cannot be ruled out. We were also not able to carry out a meta-analysis on the impact information technology based interventions have on patient’s clinical status because of heterogeneity and different metrics of reported outcomes.
Our findings demonstrate that distance Learning and Telemedicine/Telehealth in both type I and type II diabetic population were more effective interventions in reducing HbA1c compared with other information technology strategies. Also using new technologies such as Telemedicin/Telehealth and mHealth can improve patient’s knowledge and promote DSMS.
Although previous researches described that elderly peoples have poor technical skills may cause problems in using information technology based interventions and some patients are too busy to use the diabetes self management systems [15], but there is an increase in using of mobile health technologies by patients [73].
Additionally, our review shows that interventions such as Telephone coaching, CDSS, and Telemedicine/Telehealth had a positive impact on LDL and blood pressure.
As noted by Holbrook et al. many primary care providers believed that the technical difficulties with the clinical decision support systems had negative effect on the perceived usefulness of the intervention [44]. Also McMahon et al. expressed a direct relationship between the number of PHR data uploads and larger declines in HbA1c levels [67].
Kim and Song noted that diabetic type II patients benefited from an individualized approach in which the care plan was formulated according to each person’s characteristics [57].
As demonstrated by Sáenz et al. matching information technology with treatment decisions can help providers to obtain better diabetic patients’ health results. On the other hand, computer applications such as decision support systems are useful as an aid for physicians when setting the type and dose of insulin during care period [14].
Also Lowe et al. noted that a template with predefined elements of good wound care in EHR helps providers for measuring and documenting components of good wound care and tracking wound care outcomes [72].
Our findings suggest that information technology based interventions can improve glycaemic control in patients with diabetes and lead to better management of diabetes with different effect of intervention on various clinical findings. Combining multiple information technology based interventions and proposing a comprehensive solution for obtaining better results in various clinical findings lead to better diabetes management may be the suggested future research.
However it seems there is a need to apply some interventions for studying the effect of information technology based interventions on HbA1c and other clinical outcomes in diabetic population.
Limitations
The articles for this systematic review were selected exclusively from MEDLINE/PubMed based on the search query described. Inaccessibility to the full text of some articles were another limitation in this study.
Conclusion
A number of health information technology strategies are currently being used to manage diabetes. This systematic review has shown that information technology based interventions combined with the usual care are associated with improved glycemic control with different efficacy on various clinical outcomes in diabetic patients.
The authors stated that there was a distinct need for more comprehensive interventions, in which several technologies were integrated to be able to manage diabetes. Also other randomized studies need to be conducted to evaluate information technologies and their impact on managing diabetes.
References
Cho NH, Whiting D, Guariguata L, Montoya PA, Forouhi N, Hambleton I, et al. IDF Diabetes Atlas. 6th edn. International Diabetes Federation; 2013.
Baghbanian A, Tol A. The introduction of self-management in Type 2 Diabetes care: a narrative review. J Educ Health Promot. 2012;1:35 [PMCID: PMC3577389] [PubMed: 23555138].
Holtz B, Lauckner C. Diabetes management via mobile phones: a systematic review. Telemed e-Health. 2012;18(3):175–84.
Polisena J, Tran K, Climon K, Hutton B, McGill S, Palmer K. Home telehealth for diabetes management: a systematic review and meta-analysis. Diabetes Obesity Metab. 2009;11:913–30.
Jackson CL, Bolen S, Brancati FL, Batts-Turner ML, Gary TL. A systematic review of interactive computer-assisted technology in diabetes care: interactive information technology in diabetes care. J Gen Intern Med. 2006;21:105–10.
Marcolino MS, Maia JX, Alkmim MBM, Boersma E, Ribeiro AL. Telemedicine application in the care of diabetes patients: systematic review and meta-analysis. Plos One. 2013;8(11):e79246.
Siriwardena LSAN, Sudarshana Wickramasinghe WA, Dussantha Perera KL, Marasinghe RB, Katulanda P, Hewapathirana R. A review of telemedicine interventions in diabetes care. J Telemed Telecare. 2012;18:164–8. doi:https://doi.org/10.1258/jtt.2012.SFT110.
Adaji A, Schattner P, Jones K. The use of information technology to enhance diabetes management in primary care: a literature review. Inform Primary Care. 2008;16:229–37.
Pradeepa R, Prabu AV, Jebarani S, Subhashini S, Mohan V. Use of a large diabetes electronic medical record system in India: clinical and research applications. J Diabetes Sci Technol. 2011;5(3):543–52.
Riazi H, Jafarpour M, Bitaraf E. Towards National eHealth Implementation - A Comparative Study on WHO/ITU National eHealth Strategy Toolkit In Iran. Stud Health Technol Inform. 2014;205:246–50.
Kaushal R, Shojania KG, Bates DW. Effects of computerized physician order entry and clinical decision support systems on medication safety. Arch Intern Med. 2003;163:1409–16.
CRD. Systematic reviews: CRD's guidance for undertaking reviews in health care. York: Centre for Reviews and Dissemination; 2009.
Standards of Medical Care in Diabetes-2013. Diabetes Care. 2013; 36(Supplement 1): S11-66. doi: 10.2337/dc13-S011.
Sáenz A, Brito M, Morón I, Torralba A, García-Sanz E, Redondo J. Development and validation of a computer application to aid the physician’s decision-making process at the start of and during treatment with insulin in type 2 diabetes: a randomized and controlled trial. J Diabetes Sci Technol. 2012;6(3):581–8.
Chen L, Chuang LM, Chang CH, Wang CS, Wang IC, Chung Y, et al. Evaluating self-management behaviors of diabetic patients in a Telehealthcare program: longitudinal study over 18 months. J Med Internet Res. 2013;15(12), e266.
MacLean CD, Gagnon M, Callas P, Littenberg B. The Vermont diabetes information system: a cluster randomized trial of a population based decision support system. J Gen Intern Med. 2009;24(12):1303–10. doi:https://doi.org/10.1007/s11606-009-1147-x.
Grant RW, Wald JS, Schnipper JL, Gandhi TK, Poon EG, Orav EJ, et al. Practice-linked online personal health records for type 2 diabetes mellitus: a randomized controlled trial. Arch Intern Med. 2008;8:168(16). doi:https://doi.org/10.1001/archinte.168.16.1776.
Arora S, Peters AL, Burner E, Lam CN, Menchine M. Trial to examine text message-based mhealth in emergency department patients with diabetes (TExT-MED): a randomized controlled trial. Ann Emerg Med. 2014;63(6):745–54.
Ralston JD. Web-based collaborative care for type 2 diabetes. Diabetes Care. 2009;32(2):234–9. doi:https://doi.org/10.2337/dc08-1220.
Carter EL, Nunlee-Bland G, Callender C. A patient-centric, provider-assisted diabetes telehealth self-management intervention for urban minorities. Perspectives in Health Information Management. 2011.
Pinsker JE, Nguyen C, Young S, Fredericks GJ, Chan D. A pilot project for improving paediatric diabetes outcomes using a website: the Pediatric Diabetes Education Portal. J Telemed Telecare. 2011;17:226–30. doi:https://doi.org/10.1258/jtt.2010.100812.
Mulvaney SA, Anders S, Smith AK, Pittel E, Johnson KB. A pilot test of a tailored mobile and web-based diabetes messaging system for adolescents. J Telemed Telecare. 2012;18:115–8. doi:https://doi.org/10.1258/jtt.2011.111006.
Kim H-S. A randomized controlled trial of a nurse short-message service by cellular phone for people with diabetes. Int J Nursing Stud. 2007;44:687–92. doi:https://doi.org/10.1016/j.ijnurstu.2006.01.011.
Graziano JA, Gross CR. A randomized controlled trial of an automated telephone intervention to improve glycemic control in type 2 diabetes. Adv Nursing Sci. 2009;32(3):E42–57.
Nunn E, King B, Smart C, Anderson D. A randomized controlled trial of telephone calls to young patients with poorly controlled type 1 diabetes. Pediatr Diabetes. 2006;7:254–9.
Farmer AJ, Gibson OJ, Dudley C, Bryden K, Hayton PM, Tarassenko L, et al. A randomized controlled trial of the effect of real-time telemedicine support on glycemic control in young adults with type 1 diabetes (ISRCTN 46889446). Diabetes Care. 2005;28(11):2697–702.
Saager L, Collins GL, Burnside B, Tymkew H, Zhang L, Jacobsohn E, et al. A randomized study in diabetic patients undergoing cardiac surgery comparing computer-guided glucose management with a standard sliding scale protocol. J Cardiothoracic Vasc Anesthesia. 2008;22(3):377–82. doi:https://doi.org/10.1053/j.jvca.2007.09.013.
Shea S, Weinstock RS, Teresi JA, Palmas W, Starren J, Cimino JJ, et al. A randomized trial comparing telemedicine case management with usual care in older, ethnically diverse, medically underserved patients with diabetes mellitus: 5 year results of the IDEATel study. J Am Med Inform Assoc. 2009;16:446–56. doi:https://doi.org/10.1197/jamia.M3157.
Stone RA, Rao RH, Sevick MA, Cheng C, Hough LJ, Macpherson DS, et al. Active care management supported by home telemonitoring in veterans with type 2 diabetes. Diabetes Care. 2010;33(3):478–84.
Jordan RE, Lancashire RJ, Adab P. An evaluation of Birmingham Own Health® telephone care management service among patients with poorly controlled diabetes. a retrospective comparison with the General Practice Research Database. BMC Public Health. 2011;11:707. http://www.jdmdonline.com/content/14/1/49/abstract.
O’Reilly D, Holbrook A, Blackhouse G, Troyan S, Goeree R. Cost-effectiveness of a shared computerized decision support system for diabetes linked to electronic medical records. J Am Med Inform Assoc. 2012;19:341e345. doi:https://doi.org/10.1136/amiajnl-2011-000371.
Rossi MCE, Nicolucci A, Di Bartolo P, Bruttomesso D, Girelli A, Ampudia FJ, et al. Diabetes interactive diary: a new telemedicine system enabling flexible diet and insulin therapy while improving quality of life. Diabetes Care. 2010;33(1):109–15. doi:https://doi.org/10.2337/dc09-1327.
Kim S-I, Kim H-S. Effectiveness of mobile and internet intervention in patients with obese type 2 diabetes. Int J Med Informatics. 2008;77:399–404. doi:https://doi.org/10.1016/j.ijmedinf.2007.07.006.
Hussein WI, Hasan K, Jaradat AA. Effectiveness of mobile phone short message service on diabetes mellitus management; the SMS-DM study. Diabetes Res Clin Pract. 2011;94:e24–6. doi:https://doi.org/10.1016/j.diabres.2011.07.025.
Faridi Z, Liberti L, Shuval K, Northrup V, Ali A, Katz DL. Evaluating the impact of mobile telephone technology on type 2 diabetic patients’ self-management: the NICHE pilot study. J Eval Clin Practice. 2008;14:465–9. doi:https://doi.org/10.1111/j.1365-2753.2007.00881.x.
Istepanian RSH, Zitouni K, Harry D, Moutosammy N, Sungoor A, Tang B, et al. Evaluation of a mobile phone telemonitoring system for glycaemic control in patients with diabetes. J Telemed Telecare. 2009;15:125–8. doi:https://doi.org/10.1258/jtt.2009.003006.
Timmerberg BD, Wurst J, Patterson J, Spaulding RJ, Belz NE. Feasibility of using videoconferencing to provide diabetes education: a pilot study. J Telemed Telecare. 2009;15:95–7. doi:https://doi.org/10.1258/jtt.2008.080813.
Weinstock RS, Teresi JA, Goland R, Izquierdo R, Palmas W, Eimicke JP, et al. Glycemic control and health disparities in older ethnically diverse underserved adults with diabetes. Diabetes Care. 2011;34:274–9. doi:https://doi.org/10.2337/dc10-1346.
Kearns JW, Bowerman D, Kemmis K, Izquierdo RE, Weinstock RS. Group diabetes education administered through telemedicine: tools used and lessons learned. Telemed e-Health. 2012;18(5):347–53. doi:https://doi.org/10.1089/tmj.2011.0165.
O’Connor PJ, Crain AL, Rush WA, Sperl-Hillen JM, Gutenkauf JJ, Duncan JE. Impact of an electronic medical record on diabetes quality of care. Ann Fam Med. 2005;3:300–6. doi:https://doi.org/10.1370/afm.327.
O’Connor PJ, Sperl-Hillen JM, Rush WA, Johnson PE, Amundson GH, Asche SE, et al. Impact of electronic health record clinical decision support on diabetes care: a randomized trial. Ann Fam Med. 2011;9:12–21. doi:https://doi.org/10.1370/afm.1196.
Kim H-S. Impact of web-based nurse’s education on glycosylated haemoglobin in type 2 diabetic patients. J Clin Nurs. 2007;16:1361–6. doi:https://doi.org/10.1111/j.1365-2702.2005.01506.
Lim S, Kang SM, Shin H, Lee HJ, Won Yoon J, Yu SH, et al. Improved glycemic control without hypoglycemia in elderly diabetic patients using the biquitous healthcare service, a new medical information system. Diabetes Care. 2011;34:308–13. doi:https://doi.org/10.2337/dc10-1447.
Holbrook A, Thabane L, Keshavjee K, Dolovich L, Bernstein B, Chan D, et al. Individualized electronic decision support and reminders to improve diabetes care in the community: COMPETE II randomized trial. CMAJ. 2009;181(1–2):37–44. doi:https://doi.org/10.1503/cmaj.081272.
Weinstoch RS, Brooks G, Palmas W, Morin PC, Teresi JA, Eimicke JP, et al. Lessened decline in physical activity and impairment of older adults with diabetes with telemedicine and pedometer use: results from the IDEATel study. Age Ageing. 2011;40:98–105. doi:https://doi.org/10.1093/ageing/afq147.
Harno K, Kauppinen-Makelinw R, Syrjalainen J. Managing diabetes care using an integrated regional e-health approach. J Telemed Telecare. 2006;12 Suppl 1:S1:13–5.
Cho J-H, Lee H-C, Lim D-J, Kwon H-S, Yoon K-H. Mobile communication using a mobile phone with a glucometer for glucose control in Type 2 patients with diabetes: as effective as an Internet-based glucose monitoring system. J Telemed Telecare. 2009;15:77–82. doi:https://doi.org/10.1258/jtt.2008.080412.
Ellis DA, Naar-King S, Chen X, Moltz K, Cunningham PB, Idalski-Carcone A. Multisystemic therapy compared to telephone support for youth with poorly controlled diabetes: findings from a randomized controlled trial. Ann Behav Med. 2012;44(2):207–15. doi:https://doi.org/10.1007/s12160-012-9378-1.
Fischer HH, Eisert SL, Everhart RM, Durfee MJ, Moore SL, Soria S, et al. Nurse-run, telephone-based outreach to improve lipids in people with diabetes. Am J Manag Care. 2012;18(2):77–84.
Wakefield BJ, Ray A, Scherubel M, Adams MR, Hills SL. Outcomes of a home telehealth intervention for patients with diabetes and hypertension. Telemed e-Health. 2012;18(8):575–9. doi:https://doi.org/10.1089/tmj.2011.0237.
Williams ED, Bird D, Forbes AW, Russell A, Ash S, Friedman R, et al. Randomised controlled trial of an automated, interactive telephone intervention (TLC Diabetes) to improve type 2 diabetes management: baseline findings and six-month outcomes. BMC Public Health. 2012;12:602.
Glasgow RE, Nutting PA, King DK, Nelson CC, Cutter G, Gaglio B, et al. Randomized effectiveness trial of a computer-assisted intervention to improve diabetes care. Diabetes Care. 2005;28(1):33–9.
Gay CL, Chapuis F, Bendelac N, Tixier F, Treppoz S, Nicolino M. Reinforced follow-up for children and adolescents with type 1 diabetes and inadequate glycaemic control: a randomized controlled trial intervention via the local pharmacist and telecare. Diabetes Metab. 2006;32:159–65.
Izquierdo R, Morin PC, Bratt K, Moreau Z, Meyer S, Ploutz-Snyder R, et al. School-centered telemedicine for children with type 1 diabetes mellitus. J Pediatrics. 2009;155(3):374–82.
Shea S, Kothari D, Teresi JA, Kong J, Eimicke JP, Lantigua RA, et al. Social impact analysis of the effects of a telemedicine intervention to improve diabetes outcomes in an ethnically diverse, medically underserved population: findings from the IDEATel study. Am J Public Health. 2013;103(10):1888–94. doi:https://doi.org/10.2105/AJPH.2012.300909.
Nagrebetsky A, Larsen M, Craven A, Turner J, McRobert N, Murray E, et al. Stepwise self-titration of oral glucose-lowering medication using a mobile telephone-based telehealth platform in type 2 diabetes: a feasibility trial in primary care. J Diabetes Sci Technol. 2013;7(1):123–34.
Kim H-S, Song M-S. Technological intervention for obese patients with type 2 diabetes. Appl Nurs Res. 2008;21:84–9. doi:https://doi.org/10.1016/j.apnr.2007.01.007.
Jansa M, Vidal M, Viaplana J, Levy I, Conget I, Gomis R, et al. Telecare in a structured therapeutic education programme addressed to patients with type 1 diabetes and poor metabolic control. Diabetes Res Clin Practice. 2006;74:26–32. doi:https://doi.org/10.1016/j.diabres.2006.03.005.
Davis RM, Hitch AD, Salaam MM, Herman WH, Zimmer-Galler IE, Mayer-Davis EJ. TeleHealth improves diabetes self-management in an underserved community. Diabetes Care. 2010;33(8):1712–7. doi:https://doi.org/10.2337/dc09-1919.
Dale J, Caramlau I, Sturt J, Friede T, Walker R. Telephone peer-delivered intervention for diabetes motivation and support: the telecare exploratory RCT. Patient Educ Couns. 2009;75:91–8. doi:https://doi.org/10.1016/j.pec.2008.09.014.
Charpentier G, Benhamou PY, Dardari D, Clergeot A, Franc S, Schaepelynck-Belicar P, et al. The diabeo software enabling individualized insulin dose adjustments combined with telemedicine support improves hba1c in poorly controlled type 1 diabetic patients. Diabetes Care. 2011;34:533–9. doi:https://doi.org/10.2337/dc10-1259.
Stone RA, Sevick MA, Rao RH, Macpherson DS, Cheng C, Kim S, et al. The Diabetes Telemonitoring Study Extension: an exploratory randomized comparison of alternative interventions to maintain glycemic control after withdrawal of diabetes home telemonitoring. J Am Med Inform Assoc. 2012;19:973–9. doi:https://doi.org/10.1136/amiajnl-2012-000815.
Moattari M, Hashemi M, Dabbaghmanesh MH. The impact of electronic education on metabolic control indicators in patients with diabetes who need insulin: a randomised clinical control trial. J Clin Nurs. 2012;22:32–8. doi:https://doi.org/10.1111/j.1365-2702.2012.04200.x.
Salzsieder E, Augstein P. The Karlsburg Diabetes Management System: translation from research to eHealth application. J Diabetes Sci Technol. 2011;5(1):13–22.
Whittemore R, Jaser SS, Faulkner MS, Murphy K, Delamater A, Grey M. Type 1 diabetes ehealth psychoeducation: youth recruitment, participation, and satisfaction. J Med Internet Res. 2013;15(1):e15.
McFarland M, Davis K, Wallace J, Wan J, Cassidy R, Morgan T, et al. Use of home telehealth monitoring with active medication therapy management by clinical pharmacists in veterans with poorly controlled type 2 diabetes mellitus. Pharmacotherapy. 2012;32(5):420–6.
McMahon GT, Gomes HE, Hickson Hohne S, Hu TM, Levine BA, Conlin PR. Web-based care management in patients with poorly controlled diabetes mellitus. Diabetes Care. 2005;28(7):1624–9.
McCarrier KP, Ralston JD, Hirsch IB, Lewis G, Martin DP, Zimmerman FJ, et al. Web-based collaborative care for type 1 diabetes: a pilot randomized trial. Diabetes Technol Therapeut. 2009;11(4):211–7. doi:https://doi.org/10.1089/dia.2008.0063.
Graves N, Barnett AG, Halton KA, Veerman JL, Winkler E, Owen N, et al. Cost-effectiveness of a telephone-delivered intervention for physical activity and diet. PLoS One. 2009;4(9):e7135. doi:https://doi.org/10.1371/journal.pone.0007135.
Logan AG, Irvine MJ, McIsaac WJ, Tisler A, Rossos PG, Easty A, et al. Effect of home blood pressure telemonitoring with self-care support on uncontrolled systolic hypertension in diabetics. J Am Heart Assoc. 2012;60:51–7. doi:https://doi.org/10.1161/HYPERTENSIONAHA.111.188409.
Love TE, Cebul RD, Einstadter D, Jain AK, Miller H, Harris CM, et al. Electronic medical record-assisted design of a cluster-randomized trial to improve diabetes care and outcomes. J Gen Intern Med. 2007;23(4):383–91. doi:https://doi.org/10.1007/s11606-007-0454-3.
Lowe JR, Raugi GJ, Reiber GE, Whitney JD. Does incorporation of a clinical support template in the electronic medical record improve capture of wound care data in a cohort of veterans with diabetic foot ulcers? J Wound Ostomy Continence Nurs. 2013;40(2):157–62. doi:https://doi.org/10.1097/WON.0b013e318283bcd8.
Boulos MN, Wheeler S, Tavares C, Jones R. How smartphones are changing the face of mobile and participatory healthcare: an overview, with example from eCAALYX. Biomed Eng Online. 2011;10:24.
Author information
Authors and Affiliations
Corresponding author
Additional information
Competing interests
The authors declare that they have no competing interests.
Authors’ contributions
HR carried out the papers and drafted the manuscript. BL was participated in designing search frame and controlling final results. ML contributed in the review phase and study managing and finalized the manuscript. LS was consultant of the study and contributed in classification of papers and manuscript organization. All authors read and approved the final manuscript.
Rights and permissions
This is an Open Access article distributed under the terms of the Creative Commons Attribution License (http://creativecommons.org/licenses/by/4.0), which permits unrestricted use, distribution, and reproduction in any medium, provided the original work is properly credited. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.
About this article
Cite this article
Riazi, H., Larijani, B., Langarizadeh, M. et al. Managing diabetes mellitus using information technology: a systematic review. J Diabetes Metab Disord 14, 49 (2015). https://doi.org/10.1186/s40200-015-0174-x
Received:
Accepted:
Published:
DOI: https://doi.org/10.1186/s40200-015-0174-x