-
PDF
- Split View
-
Views
-
Cite
Cite
John Kyriazis, John Glotsos, Leonidas Bilirakis, Nikos Smirnioudis, The (dP/dt)max derived from arterial pulse waveforms: prospective applications in the haemodialysis setting, Nephrology Dialysis Transplantation, Volume 16, Issue 5, May 2001, Pages 1087–1088, https://doi.org/10.1093/ndt/16.5.1087-a
Close - Share Icon Share
Sir,
A new non‐invasive, pulse‐dynamic technology [1] can provide not only automated systolic and diastolic pressures, but also measurements of the rate of pressure change during the cardiac cycle. Measurements of the maximum rate of BP increase in systole are derived from the brachial pulsation signal, obtained with the use of an inflated cuff, after converting it into its first derivative (dP/dt)max with respect to time. These peripheral (dP/dt)max calculations are in good agreement (r=0.87) with invasive measurements of left ventricular (dP/dt)max [1]. Recently, Germano et al. [2] reported that the (dP/dt)max of normal subjects was significantly greater (P<0.05) than that of cardiac patients with ejection fraction <40%. In the present study, we (i) further investigated the associations between brachial pulse (dP/dt)max and other haemodynamic parameters in a chronic haemodialysis population and (ii) examined the potential role of (dP/dt)max as a tool to track effectively haemodynamic changes during HD.
In the first part of the study, 24 HD patients, 14 men and 10 women, with a mean age of 63±13 y and a mean time on haemodialysis therapy of 55±33 months, underwent conventional echocardiography on a non‐HD day, where the following parameters were determined: cardiac index (CI), stroke index (SI), ejection fraction (EF), fibre fractioning (FS), and velocity of circumferential fibre shortening (VCF). Brachial artery blood pressure (BP) was measured just before the echocardiographic study, using the Dynapulse 5000A automatic oscillometric device (Pulse Metric Inc, San Diego, CA, USA), and the oscillometric cuff signal was used to derive the (dP/dt)max. The mean±1 SD of (dP/dt)max in our HD males and females was 1195±300 and 1280±407 mmHg/s, respectively. The ‘normal’ range of Pulse Metric (dP/dt)max (personal communication), based on data analysed on normotensive subjects between 18 and 80 years old, was 1173±187 mmHg/s for males (n=699) and 1125±195 mmHg/s for females (n=1277). (dP/dt)max correlated positively with EF and FS (r=0.5, P<0.05) and even more substantially with SBP and PP (r=0.6, P<0.01). Multiple regression analysis revealed that brachial pulse's (dP/dt)max could be best predicted, significantly (R2=0.53, P<0.001) and independently, by both PP and VCF. In order to study the reproducibility of the peripheral (dP/dt)max, a second (dP/dt)max was obtained, using the above mentioned protocol, in 18 out of the 24 participants, on the next non‐HD day. The Pearson correlation coefficient between the two measurements was 0.93 (P<0.001) and the variation coefficient of the repeated measures was 7.9±4.4%.
These findings raise the hypothesis that brachial pulse's derivative can be adopted as an additional representative of cardiac function. Given that each arterial pulse waveform obtained during a 24 h BP oscillometric recording can be converted to its first derivative (dP/dt)max, the latter would be extremely useful to monitor cardiac performance during daily activities, or to outline the nycthoemeral rhythm [3]. Furthermore, owing to its satisfactory reproducibility in the HD setting, (dP/dt)max may be adopted in the evaluation of the effects of therapeutic interventions on cardiac function.
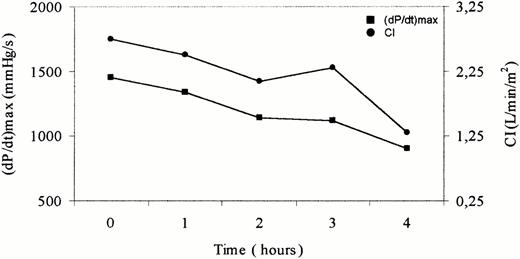
In the second part of the study, the efficiency of the (dP/dt)max to monitor cardiac function, during the course of HD, was assessed in 5 HD patients. In this investigation, the (dP/dt)max was correlated with cardiac indices derived with transthoracic electrical bioimpedance (TEB), which as a method to determine cardiac output has an impressive reproducibility in the HD setting [4]. In each patient, CI, SI and EF were measured non‐invasively before HD and at 1 h intervals during HD, with the NCCOM3‐R7 system (CDIc, Irvine, CA, USA). At the same time points, blood pressure was taken with the same ambulatory BP monitor (Dynapulse 5000A) and from analysis of the pulse signal, the (dP/dt)max was calculated. For each patient (five measurements), the correlation coefficient (r) between (dP/dt)max and the TEB derived indices was calculated. In all patients, high correlations between (dP/dt)max and CI (r⩾0.89), SI (r⩾0.87) and EF (r⩾0.88) were observed. The agreement between TEB‐CI and peripheral (dP/dt)max is depicted graphically in Figure 3. The perspective of calculating routinely (dP/dt)max on each pressure wave, obtained by the use of a sphygmomanometer cuff, would provide HD personnel with a simple means to track non‐invasively cardiac contractility during HD treatment. Such a strategy, by early detection of myocardial dysfunction during HD and, thus, dictating the appropriate therapeutic manoeuvres, may further reduce the morbidity due to HD‐associated haemodynamic instability.
Parallel course of cardiac index (CI) and (dP/dt)max during a 4‐h HD session. Data are taken from a 56‐year‐old female haemodialysis patient.
References
Brinton TJ, Cotter B, Kailasam MT, Brown DL, Chio SS, O'Connor DT, DeMaria AN. Development and validation of a non‐invasive method to determine arterial pressure and vascular compliance.
Germano G, Angotti S, Muscolo M, D'Auria F, Giordano M. The (dP/dt)max derived from arterial pulse waveforms during 24 h blood pressure oscillometric recording.
Germano G, Pecchioli V, Germano U, Muscolo M, Angotti S, D'Auria F, Giordano M. Suprasystolic (dP/dt)max an additional parameter of contractile cardiac function obtained by cuff oscillometric tracings.





Comments