-
PDF
- Split View
-
Views
-
Cite
Cite
Alexandra Main, Deborah J. Wiebe, Andrea R. Croom, Katie Sardone, Elida Godbey, Christy Tucker, Perrin C. White, Associations of Parent–Adolescent Relationship Quality With Type 1 Diabetes Management and Depressive Symptoms in Latino and Caucasian Youth, Journal of Pediatric Psychology, Volume 39, Issue 10, November/December 2014, Pages 1104–1114, https://doi.org/10.1093/jpepsy/jsu062
Close - Share Icon Share
Abstract
Objective To examine associations of parent–adolescent relationship quality (parental acceptance and parent–adolescent conflict) with adolescent type 1 diabetes management (adherence and metabolic control) and depressive symptoms in Latinos and Caucasians. Methods In all, 118 adolescents and their mothers (56 = Latino, 62 = Caucasian) completed survey measures of parental acceptance, diabetes conflict, adolescent adherence, and adolescent depressive symptoms. Glycemic control was obtained from medical records. Results Across ethnic groups, adolescent-reported mother and father acceptance were associated with better diabetes management, whereas mother-reported conflict was associated with poorer diabetes management and more depressive symptoms. Independent of socioeconomic status, Latinos reported lower parental acceptance and higher diabetes conflict with mothers than Caucasians. Ethnicity moderated some associations between relationship quality and outcomes. Specifically, diabetes conflicts with mothers (mother and adolescent report) and fathers (adolescent report) were associated with poorer mother-reported adherence among Caucasians, but not among Latinos. Conclusions Parent–adolescent relationship quality differs and may have different relations with diabetes management across Latinos and Caucasians.
Type 1 diabetes is among the most common chronic childhood illnesses, and its prevalence is increasing worldwide (Lipman et al., 2013). Adolescence is a developmental period during which adherence, glycemic control, and psychological well-being often deteriorate (Anderson et al., 2002). It is important to investigate factors that contribute to better diabetes management during adolescence because patterns of mismanagement established in adolescence often extend into adulthood (Bryden et al., 2001), and the resulting poor glycemic control has serious and costly complications across the lifespan (Diabetes Control and Complications Trial [DCCT], 1993). Acceptance, warmth, and supportive involvement of parents (Drew et al., 2011; King, Berg, Butner, Butler, & Wiebe, 2014; La Greca, Follansbee, & Skyler, 1990; Palmer et al., 2004) and low levels of family and diabetes conflict (Anderson et al., 2002; Hilliard et al., 2013) have been associated with better diabetes management and psychological well-being. However, this research has been conducted with primarily Caucasian middle-class samples. It is important to examine associations between parent–adolescent relationship quality and diabetes management among ethnic minority youth given ethnic disparities in chronic illness management (Karter et al., 2002) and in the socioeconomic resources that may influence relationship quality and diabetes management (Drew et al., 2011). Little research has examined associations among parent–adolescent relationship variables, diabetes management, and psychological well-being in Latino youth, even though Latinos are the fastest-growing minority group in the USA (US Census Bureau, 2010). The present study explored the role of parental acceptance and diabetes conflicts between parents and adolescents in type 1 diabetes management (adherence and glycemic control) and depressive symptoms for a socioeconomically diverse sample of Latino and Caucasian adolescents.
Parental acceptance is defined as the tendency to communicate warmth and support toward a child such that the child perceives the parent as accepting them for who they are (Palmer et al., 2004). A growing literature demonstrates the importance of parental acceptance for managing diabetes and lessening depressive symptoms among children and adolescents (King et al., 2014; Palmer, et al., 2004). Parental acceptance has been identified as one of three independent dimensions of parental involvement in adolescent diabetes management along with behavioral involvement (e.g., instrumental support, parental diabetes responsibility) and parental monitoring of diabetes (Palmer et al., 2004). Longitudinal declines in parental acceptance predict subsequent declines in adherence to the diabetes regimen across adolescence (King et al., 2014).
A diabetes-specific aspect of relationship quality that is important in this population is diabetes conflict. Parent–adolescent conflict surrounding diabetes is common (Hilliard et al., 2013) and is associated with poor diabetes management (Anderson et al., 2002; Hood, Butler, Anderson, & Laffel, 2007). Diabetes conflicts between parents and adolescents often arise when adolescents perceive parents as lacking understanding and behaving intrusively regarding their diabetes care (Miller & Drotar, 2003). Negative emotions and stress aroused by conflict may adversely affect adolescents’ physiological management of their illness (glycemic control), their ability to engage in proper self-care (Hilliard et al., 2013), and their depressive symptoms (Herzer, Vesco, Ingerski, Dolan, & Hood, 2011).
It remains unclear whether (a) there are ethnic differences in levels of parental acceptance and diabetes conflict and (b) whether acceptance and conflict show similar associations with diabetes management and psychological adjustment across Latinos and Caucasians. Parent–adolescent relationship characteristics might be particularly important for understanding diabetes management in the Latino population because of the centrality of family in Latino culture (Lopez, 2006). However, research in the general developmental and diabetes literatures has been mixed. In the context of diabetes management, research has shown that Latino parents report greater supervision of their children’s diabetes regimen adherence (Gallegos-Macias, Macias, Kaufman, Skipper, & Kalishman, 2003), and parental support for diabetes care is associated with better diabetes outcomes among Latino youth (Hsin, La Greca, Valenzuela, Moine, & Delamater, 2010). In the general developmental literature, however, some studies have suggested that Latino parents often use authoritarian parenting practices (characterized by low warmth and acceptance combined with harsh discipline) to facilitate the internalization of traditional cultural values such as respeto (i.e., respect for authority) in their children (Calzada, Keng-Yeng, Anicama, Fernandez, & Brotman, 2012). Authoritarian parenting is associated with higher parent–adolescent conflict in the general developmental literature (Smetana, 1995). Conversely, other studies have found that Latino parenting is characterized by high warmth and acceptance (Domenech Rodriguez, Donovick, & Crowley, 2009) and family cohesion, which has been identified as a protective factor for Latino adolescents (Rivera et al., 2008). Furthermore, parenting behaviors and relationship quality characteristics may have different meanings in the Latino cultural context compared with Caucasian families (Domenech Rodriguez et al., 2009). Therefore, parental acceptance and parent–adolescent conflict may relate to physical and psychological adjustment differently in Latino compared with Caucasian youth.
It is important to consider ethnic differences in family processes and diabetes management in the context of potential disparities in socioeconomic status (SES). According to resource models, lower income is associated with poorer health outcomes because of increased psychological stress, which may result in lower quality parenting (Conger, Conger, Matthews, & Elder, 1999). Low-income families often experience heightened stress and family conflict (Conger et al., 1999), and poorer parent–adolescent relationship quality has been found to mediate associations between income and metabolic control among adolescents with diabetes (Drew et al., 2011). Because Latino families tend to have fewer socioeconomic resources compared with Caucasian families (Gallegos-Macias et al., 2003), Latino families might be at particular risk for lower parent–adolescent relationship quality, increased conflict, and poor diabetes management.
The goals of the present study were twofold. First, this investigation examined whether there were differences between Caucasians and Latinos in parent–adolescent relationship quality (mother and father acceptance and diabetes conflicts with mothers and fathers) and whether any ethnic differences remained independently of socioeconomic factors. Based on mixed findings of research on differences between Latinos and Caucasians in parenting, we tested ethnic differences in acceptance and conflict but did not have specific hypotheses regarding mean levels. However, we did expect to find lower acceptance and higher diabetes conflict in low SES families (Conger et al., 1999). Second, the present study investigated whether there were differential relations of parental acceptance and diabetes conflict to adolescent diabetes management (metabolic control and adherence) and depressive symptoms across ethnicities. Because youth with type 1 diabetes often have higher rates of depressive symptoms compared with healthy youth (Reynolds & Helgeson, 2011), and because parent–adolescent relationship quality is associated with depressive symptoms, we included depressive symptoms as an outcome. Because of the central role of family in Latino culture (Lopez, 2006), we hypothesized that relationship quality variables would have stronger associations with diabetes management and depressive symptoms among Latinos compared with Caucasians independently of SES.
Method
Participants
Participants included 118 adolescents (56 = Latino, 62 = Caucasian) with type 1 diabetes mellitus and their mothers recruited from an interdisciplinary outpatient pediatric endocrinology clinic. Early to middle adolescents between 10 and 15 years of age (Smetana, Campione-Barr, & Metzgar, 2006) (M = 12.74, SD = 1.64) were recruited if they had been diagnosed with diabetes for at least 1 year (M = 4.12, SD = 2.78), self-identified as either Caucasian or Latino, and could read and speak English or Spanish. It is in this age range when diabetes management and glycemic control typically begin to decline (Anderson et al., 2002) and parent–adolescent conflict typically increases (Collins & Laursen, 1992). Adolescents were fairly evenly divided by gender (54% female). Mothers were recruited because they are most often the primary caregivers in families with chronically ill children (Quittner et al., 1998). For each adolescent, one mother figure was allowed to participate. Adolescents were required to be living with their participating mother >50% of the time. Stepmothers or adopted mothers were eligible if they had lived with the adolescent for at least 1 year. Adolescents also identified and reported on the father figure who was most involved in their diabetes care. Mothers were primarily biological (92%) and married (75%), and 73% reported living in two-parent households with the participating child’s father; there were no ethnic differences in these family composition variables. Most adolescents followed a regimen of multiple daily injections; consistent with general treatment procedures at participating clinics, 25% were on an insulin pump.
Of the 246 qualifying individuals approached, 118 (48%) agreed to participate in the study and were enrolled, while 63 (25.6%) refused. An additional 65 (26.4%) individuals expressed a desire to participate but could not be reached to confirm interest or schedule a research appointment. Reasons for refusal included distance of commute or transportation problems (27%), too busy (33%), and scheduling conflicts that could not be resolved (40%). Comparisons of eligible adolescents who participated versus those who did not revealed no differences in adolescent sex, age, pump status, or glycated hemoglobin (HbA1c). A chi-square test revealed that Caucasian adolescents were marginally less likely to agree to participate compared with Latino adolescents, χ2 (1, N = 246) = 3.84, p = .053.
Procedure
Participants were recruited for the study at a large pediatric endocrinology clinic in an urban area in the southwestern USA and received consent and assent forms to review before a later appointment at the campus research laboratory. During the study session, mothers and adolescents independently completed questionnaire measures on a computer. All participants received a brief tutorial on how to complete surveys on the computer; participants who indicated discomfort in completing electronic surveys were provided with paper versions of the questionnaires. When Spanish versions of measures were not available, the measure was translated and back translated from English to Spanish by bilingual staff. Each mother and adolescent participant received a $40 gift card at the completion of the one-time assessment.
Measures
Demographics
Most Latino adolescents were second- or third-generation Mexican-American: 12% were classified as first generation with both mother and adolescent born outside the USA, 57% were second generation with the adolescent born in the USA and mother born outside the USA, and 31% were third generation with both adolescent and mother born inside the USA. Of the mothers born outside the USA, 84% reported Mexico as their country of origin, with the remaining from Puerto Rico, Argentina, Bolivia, El Salvador, and Guatemala. Less than half of Latina mothers reported English as the primary language spoken at home (43%), but only one adolescent chose to complete measures in Spanish. Neighborhood income (i.e., median family income) was collected from census tract data based on the participants’ zip codes. Neighborhood income was used as a proxy for SES because it was the income variable most strongly correlated with HbA1c and has been linked to HbA1c levels in prior research (Wang, Wiebe, & White, 2011).
Parental Acceptance
The acceptance subscale of the Mother-Father-Peer Scale (Epstein, 1983) consists of five items in which adolescents and mothers rated on a 1 (strongly disagree) to 5 (strongly agree) scale how much the parent communicated love and acceptance. An average score across items was obtained (adolescent report of mother acceptance: Caucasian: α = .83, Latino: α = .87; mother report of her own acceptance: Caucasian: α = .45, Latina: α =.38; adolescent report of father acceptance: Caucasian: α = .87, Latino: α = .90). Given the low reliability of mothers’ report, mother-reported acceptance was not analyzed further in the present study. This low reliability was likely because of a ceiling effect (M = 4.82 and 4.64 for Caucasians and Latinas, respectively).
Diabetes Conflict
The Diabetes Family Conflict Scale (Rubin, Young-Human, & Peyrot, 1989) consists of 15 items in which adolescents and mothers rated on a 1 (almost never) to 3 (almost always) scale how frequently they argue about specific diabetes-related tasks (e.g., “remembering to check blood sugars”, “remembering to give insulin shots or boluses”). An average score across items was obtained (adolescent report of conflict with mothers: Caucasian: α = .96, Latino: α = .95; mother report conflict: Caucasian: α = .90, Latina: α = .92; adolescent report of conflict with fathers: Caucasian: α = .98, Latino: α = .97).
Adherence
An adapted version of the Self-Care Inventory (La Greca et al., 1990; Lewin et al., 2009) measured adolescent adherence. In consultation with a certified diabetes educator, items were rephrased to be relevant to those using an insulin pump or injections, and two items were added to reflect current treatment standards (i.e., “How well have you (has your adolescent) followed recommendations for counting carbohydrates?” and “How well have you (has your adolescent) followed recommendations for calculating insulin doses based on carbohydrates in meals and snacks?”). Participants were given a not applicable option for items not relevant to their regimen. Adolescents reported adherence to their regimen over the past month, while mothers reported on whether their adolescent adhered to the regimen (1 = never did it to 5 = always did this as recommended without fail); average scores were analyzed (adolescent report: α = .87 for both Latinos and Caucasians; mother report: Caucasian: α = .93, Latina: α = .92). Findings for analyses conducted with and without the two additional items were the same.
Metabolic Control
Metabolic control was indexed by HbA1c recorded in medical records. Point-of-care HbA1c was measured by clinic staff using the Bayer DCA Vantage. HbA1c represents the average blood glucose over the prior ∼3 months, with higher levels indicating poorer metabolic control. We used the HbA1c measure obtained during the clinic visit when participants were recruited to capture metabolic control nearest to the study assessment. The average length of time between HbA1c assessment and the study visit was 3 weeks (range = 0–6 weeks). Time since HbA1c assessment was covaried in the analyses.
Adolescent Depressive Symptoms
Adolescents completed the Children’s Depression Inventory (Kovacs, 1985) to indicate depressive symptoms in the past 2 weeks (e.g., 1 = I am sad once in a while, 2 = I am sad many times, 3 = I am sad all the time). This 27-item scale has strong reliability and is related to diabetes management (e.g., Grey, Davidson, Boland, & Tamborlane, 2001). Summed scores were analyzed (Caucasian: α = .81; Latino: α = .87).
Analysis Plan
SPSS version 22 was used to conduct the analyses. First, correlations of relationship quality with diabetes management and depressive symptoms were conducted. Second, t-tests or chi-square tests were conducted to examine ethnic differences in sociodemographic, relationship quality, and illness variables. Univariate analyses of covariance tested whether ethnic differences in relationship quality held after controlling for SES. Third, hierarchical multiple regressions were conducted to examine whether (1) relationship quality variables were associated with outcomes independently of sociodemographic characteristics, and (2) ethnicity moderated relations of parental acceptance or conflict with diabetes management and depressive symptoms.
Variables were first screened for normality. Using the cutoffs of two and seven for skew and kurtosis, respectively (West, Finch, & Curran, 1995), all variables were normally distributed. To reduce the number of predictors in the regression models and the possibility of multicollinearity, an SES variable consisting of a composite of mother education and median neighborhood household income (r = .47, p < .001) was created by standardizing both variables and calculating the mean. This SES variable was included as a covariate in all regression analyses. Adolescent sex, age, time since diagnosis, and diabetes regimen (pump vs. multiple daily injections) were also included as covariates in all regression analyses because each was correlated with at least one outcome variable. Interactions between sex and the relationship quality variables in predicting outcomes were explored; these interaction terms were not significant and thus were dropped from the final regression analyses.
Results
Associations Between Relationship Quality and Outcomes in the Full Sample
Means, standard deviations, and zero-order correlations among study variables in the full sample are presented in Table I. Adolescent-reported mother and father acceptance were correlated with better adherence (adolescent report) and fewer depressive symptoms. Mother-reported conflict was correlated with higher HbA1c, lower adherence, and more depressive symptoms. Adolescent-reported conflicts with mothers and fathers were not correlated with diabetes management or depressive symptoms.
Means, Standard Deviations (SD), and Correlations Among Primary Study Variables Across the Full Sample
| Study variables . | M (SD) . | 1 . | 2 . | 3 . | 4 . | 5 . | 6 . | 7 . | 8 . | 9 . | 10 . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Mother acceptance (A) | 4.28 (.83) | – | .34*** | −.21* | −.37*** | −.15 | −.24** | −.16 | .21* | .02 | −.37*** |
| 2. Father acceptance (A) | 4.00 (1.01) | – | −.13 | −.31** | .16 | −.21* | −.16 | .21* | .15 | −.31** | |
| 3. Diabetes conflicts with mother (A) | 1.79 (.62) | – | .33** | .72*** | .22* | .12 | .01 | −.02 | .15 | ||
| 4. Diabetes conflicts with mother (M) | 1.66 (.51) | – | .19 | .35*** | .37*** | −.18 | −.26** | .27** | |||
| 5. Diabetes conflicts with father (A) | 1.54 (.65) | – | .11 | .04 | .16 | .10 | −.01 | ||||
| 6. Ethnicity (−1 = Caucasian, 1 = Latino) | −.05 (1.00) | – | .14 | −.09 | .13 | .12 | |||||
| 7. Glycated hemoglobin | 8.55 (1.55) | – | −.22* | −.27** | .20* | ||||||
| 8. Adherence (A) | 4.04 (.68) | – | .30** | −.50*** | |||||||
| 9. Adherence (M) | 3.91 (.73) | – | −.14 | ||||||||
| 10. Depressive symptoms (A) | 8.36 (6.09) | – |
| Study variables . | M (SD) . | 1 . | 2 . | 3 . | 4 . | 5 . | 6 . | 7 . | 8 . | 9 . | 10 . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Mother acceptance (A) | 4.28 (.83) | – | .34*** | −.21* | −.37*** | −.15 | −.24** | −.16 | .21* | .02 | −.37*** |
| 2. Father acceptance (A) | 4.00 (1.01) | – | −.13 | −.31** | .16 | −.21* | −.16 | .21* | .15 | −.31** | |
| 3. Diabetes conflicts with mother (A) | 1.79 (.62) | – | .33** | .72*** | .22* | .12 | .01 | −.02 | .15 | ||
| 4. Diabetes conflicts with mother (M) | 1.66 (.51) | – | .19 | .35*** | .37*** | −.18 | −.26** | .27** | |||
| 5. Diabetes conflicts with father (A) | 1.54 (.65) | – | .11 | .04 | .16 | .10 | −.01 | ||||
| 6. Ethnicity (−1 = Caucasian, 1 = Latino) | −.05 (1.00) | – | .14 | −.09 | .13 | .12 | |||||
| 7. Glycated hemoglobin | 8.55 (1.55) | – | −.22* | −.27** | .20* | ||||||
| 8. Adherence (A) | 4.04 (.68) | – | .30** | −.50*** | |||||||
| 9. Adherence (M) | 3.91 (.73) | – | −.14 | ||||||||
| 10. Depressive symptoms (A) | 8.36 (6.09) | – |
Notes. (M) = mother report; (A) = adolescent report.
***p < .001, **p < .01,*p < .05.
Means, Standard Deviations (SD), and Correlations Among Primary Study Variables Across the Full Sample
| Study variables . | M (SD) . | 1 . | 2 . | 3 . | 4 . | 5 . | 6 . | 7 . | 8 . | 9 . | 10 . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Mother acceptance (A) | 4.28 (.83) | – | .34*** | −.21* | −.37*** | −.15 | −.24** | −.16 | .21* | .02 | −.37*** |
| 2. Father acceptance (A) | 4.00 (1.01) | – | −.13 | −.31** | .16 | −.21* | −.16 | .21* | .15 | −.31** | |
| 3. Diabetes conflicts with mother (A) | 1.79 (.62) | – | .33** | .72*** | .22* | .12 | .01 | −.02 | .15 | ||
| 4. Diabetes conflicts with mother (M) | 1.66 (.51) | – | .19 | .35*** | .37*** | −.18 | −.26** | .27** | |||
| 5. Diabetes conflicts with father (A) | 1.54 (.65) | – | .11 | .04 | .16 | .10 | −.01 | ||||
| 6. Ethnicity (−1 = Caucasian, 1 = Latino) | −.05 (1.00) | – | .14 | −.09 | .13 | .12 | |||||
| 7. Glycated hemoglobin | 8.55 (1.55) | – | −.22* | −.27** | .20* | ||||||
| 8. Adherence (A) | 4.04 (.68) | – | .30** | −.50*** | |||||||
| 9. Adherence (M) | 3.91 (.73) | – | −.14 | ||||||||
| 10. Depressive symptoms (A) | 8.36 (6.09) | – |
| Study variables . | M (SD) . | 1 . | 2 . | 3 . | 4 . | 5 . | 6 . | 7 . | 8 . | 9 . | 10 . |
|---|---|---|---|---|---|---|---|---|---|---|---|
| 1. Mother acceptance (A) | 4.28 (.83) | – | .34*** | −.21* | −.37*** | −.15 | −.24** | −.16 | .21* | .02 | −.37*** |
| 2. Father acceptance (A) | 4.00 (1.01) | – | −.13 | −.31** | .16 | −.21* | −.16 | .21* | .15 | −.31** | |
| 3. Diabetes conflicts with mother (A) | 1.79 (.62) | – | .33** | .72*** | .22* | .12 | .01 | −.02 | .15 | ||
| 4. Diabetes conflicts with mother (M) | 1.66 (.51) | – | .19 | .35*** | .37*** | −.18 | −.26** | .27** | |||
| 5. Diabetes conflicts with father (A) | 1.54 (.65) | – | .11 | .04 | .16 | .10 | −.01 | ||||
| 6. Ethnicity (−1 = Caucasian, 1 = Latino) | −.05 (1.00) | – | .14 | −.09 | .13 | .12 | |||||
| 7. Glycated hemoglobin | 8.55 (1.55) | – | −.22* | −.27** | .20* | ||||||
| 8. Adherence (A) | 4.04 (.68) | – | .30** | −.50*** | |||||||
| 9. Adherence (M) | 3.91 (.73) | – | −.14 | ||||||||
| 10. Depressive symptoms (A) | 8.36 (6.09) | – |
Notes. (M) = mother report; (A) = adolescent report.
***p < .001, **p < .01,*p < .05.
Ethnic Differences in Demographic, Illness, and Study Variables
As displayed in Table II, there were no significant differences between ethnic groups on age, sex, time since diagnosis, and insulin pump usage, p > .05. Latina mothers reported lower education levels than Caucasians, completing an average of 13 years (range = < 7th grade to graduate degree) versus 15.5 years (range = high school graduate to graduate degree). Twenty-eight percent of Latina mothers did not graduate high school, and only one had a graduate degree, whereas 48% of Caucasian mothers held a bachelor’s degree or above. Latino families also had lower neighborhood median family income than Caucasians ($51,000 vs. $72,000, p < .001). Latino adolescents reported lower mother and father acceptance than Caucasian adolescents. Latino adolescents and mothers also reported more diabetes conflicts than Caucasian adolescents and mothers. There were no ethnic differences in adolescents’ reports of conflict with fathers or in the outcome variables (HbA1c, adherence, and depressive symptoms).
Descriptive Data by Ethnicity
| Variable . | Caucasian (M/SD) . | Latino (M/SD) . | t, X2 (df) . |
|---|---|---|---|
| N | 62 | 56 | |
| Female sex, % | 46.8 | 62.5 | 2.65 (115) |
| Adolescent age | 13.19 (1.63) | 13.30 (1.70) | −.56 (115) |
| Mother education (years) | 15.5 (2.9) | 13.0 (8.9) | 7.16 (113)*** |
| Median neighborhood family income | $72,000 ($28,000) | $51,000 ($18,000) | 4.68 (106)*** |
| Pump status, % Yes | 31 | 20 | 1.73 (115) |
| Illness duration (years) | 4.90 (3.14) | 4.31 (2.45) | 1.05 (115) |
| Mother acceptance (A) | 4.47 (.66) | 4.07 (.95) | 4.92 (115)** |
| Father acceptance (A) | 4.20 (.95) | 3.79 (1.04) | 1.48 (112)* |
| Diabetes conflicts with mother (A) | 1.66 (.62) | 1.92 (.60) | 2.63 (115)* |
| Diabetes conflicts with mother (M) | 1.51 (.42) | 1.87 (.54) | 3.68 (106)*** |
| Diabetes conflicts with father (A) | 1.48 (.60) | 1.61 (.70) | −1.12 (111) |
| Glycated hemoglobin | 8.35 (1.43) | 8.77 (1.67) | −1.54 (115) |
| Adherence (A) | 4.09 (.57) | 3.97 (.78) | .93 (114) |
| Adherence (M) | 3.82 (.74) | 4.01 (.73) | −1.21 (108) |
| Depressive symptoms (A) | 7.69 (5.32) | 9.11 (6.83) | −1.27 (115) |
| Variable . | Caucasian (M/SD) . | Latino (M/SD) . | t, X2 (df) . |
|---|---|---|---|
| N | 62 | 56 | |
| Female sex, % | 46.8 | 62.5 | 2.65 (115) |
| Adolescent age | 13.19 (1.63) | 13.30 (1.70) | −.56 (115) |
| Mother education (years) | 15.5 (2.9) | 13.0 (8.9) | 7.16 (113)*** |
| Median neighborhood family income | $72,000 ($28,000) | $51,000 ($18,000) | 4.68 (106)*** |
| Pump status, % Yes | 31 | 20 | 1.73 (115) |
| Illness duration (years) | 4.90 (3.14) | 4.31 (2.45) | 1.05 (115) |
| Mother acceptance (A) | 4.47 (.66) | 4.07 (.95) | 4.92 (115)** |
| Father acceptance (A) | 4.20 (.95) | 3.79 (1.04) | 1.48 (112)* |
| Diabetes conflicts with mother (A) | 1.66 (.62) | 1.92 (.60) | 2.63 (115)* |
| Diabetes conflicts with mother (M) | 1.51 (.42) | 1.87 (.54) | 3.68 (106)*** |
| Diabetes conflicts with father (A) | 1.48 (.60) | 1.61 (.70) | −1.12 (111) |
| Glycated hemoglobin | 8.35 (1.43) | 8.77 (1.67) | −1.54 (115) |
| Adherence (A) | 4.09 (.57) | 3.97 (.78) | .93 (114) |
| Adherence (M) | 3.82 (.74) | 4.01 (.73) | −1.21 (108) |
| Depressive symptoms (A) | 7.69 (5.32) | 9.11 (6.83) | −1.27 (115) |
Notes. SD = standard deviation, df = degrees of freedom, (A) = adolescent report, (M) = mother report.
Differences between Caucasian and Latino samples are significant at ***p < .001, **p < .01, and *p < .05.
Descriptive Data by Ethnicity
| Variable . | Caucasian (M/SD) . | Latino (M/SD) . | t, X2 (df) . |
|---|---|---|---|
| N | 62 | 56 | |
| Female sex, % | 46.8 | 62.5 | 2.65 (115) |
| Adolescent age | 13.19 (1.63) | 13.30 (1.70) | −.56 (115) |
| Mother education (years) | 15.5 (2.9) | 13.0 (8.9) | 7.16 (113)*** |
| Median neighborhood family income | $72,000 ($28,000) | $51,000 ($18,000) | 4.68 (106)*** |
| Pump status, % Yes | 31 | 20 | 1.73 (115) |
| Illness duration (years) | 4.90 (3.14) | 4.31 (2.45) | 1.05 (115) |
| Mother acceptance (A) | 4.47 (.66) | 4.07 (.95) | 4.92 (115)** |
| Father acceptance (A) | 4.20 (.95) | 3.79 (1.04) | 1.48 (112)* |
| Diabetes conflicts with mother (A) | 1.66 (.62) | 1.92 (.60) | 2.63 (115)* |
| Diabetes conflicts with mother (M) | 1.51 (.42) | 1.87 (.54) | 3.68 (106)*** |
| Diabetes conflicts with father (A) | 1.48 (.60) | 1.61 (.70) | −1.12 (111) |
| Glycated hemoglobin | 8.35 (1.43) | 8.77 (1.67) | −1.54 (115) |
| Adherence (A) | 4.09 (.57) | 3.97 (.78) | .93 (114) |
| Adherence (M) | 3.82 (.74) | 4.01 (.73) | −1.21 (108) |
| Depressive symptoms (A) | 7.69 (5.32) | 9.11 (6.83) | −1.27 (115) |
| Variable . | Caucasian (M/SD) . | Latino (M/SD) . | t, X2 (df) . |
|---|---|---|---|
| N | 62 | 56 | |
| Female sex, % | 46.8 | 62.5 | 2.65 (115) |
| Adolescent age | 13.19 (1.63) | 13.30 (1.70) | −.56 (115) |
| Mother education (years) | 15.5 (2.9) | 13.0 (8.9) | 7.16 (113)*** |
| Median neighborhood family income | $72,000 ($28,000) | $51,000 ($18,000) | 4.68 (106)*** |
| Pump status, % Yes | 31 | 20 | 1.73 (115) |
| Illness duration (years) | 4.90 (3.14) | 4.31 (2.45) | 1.05 (115) |
| Mother acceptance (A) | 4.47 (.66) | 4.07 (.95) | 4.92 (115)** |
| Father acceptance (A) | 4.20 (.95) | 3.79 (1.04) | 1.48 (112)* |
| Diabetes conflicts with mother (A) | 1.66 (.62) | 1.92 (.60) | 2.63 (115)* |
| Diabetes conflicts with mother (M) | 1.51 (.42) | 1.87 (.54) | 3.68 (106)*** |
| Diabetes conflicts with father (A) | 1.48 (.60) | 1.61 (.70) | −1.12 (111) |
| Glycated hemoglobin | 8.35 (1.43) | 8.77 (1.67) | −1.54 (115) |
| Adherence (A) | 4.09 (.57) | 3.97 (.78) | .93 (114) |
| Adherence (M) | 3.82 (.74) | 4.01 (.73) | −1.21 (108) |
| Depressive symptoms (A) | 7.69 (5.32) | 9.11 (6.83) | −1.27 (115) |
Notes. SD = standard deviation, df = degrees of freedom, (A) = adolescent report, (M) = mother report.
Differences between Caucasian and Latino samples are significant at ***p < .001, **p < .01, and *p < .05.
To examine whether ethnic differences in relationship quality remained after controlling SES, we conducted univariate analyses of covariance on (a) mother and father acceptance (adolescent report) and (b) diabetes conflicts with mothers (adolescent and mother report) and fathers (adolescent report), with SES as the covariate. The effect of ethnicity was significant for adolescent-reported mother acceptance, F(1, 102) = 4.09, p = .046, η = .039, and mother-reported conflict, F(1, 102) = 7.34, p = .008, η = .067. Ethnic differences in adolescent-reported father acceptance and adolescent-reported conflicts with mothers were no longer significant after controlling for SES.
Moderation of Associations Between Relationship Quality and Outcomes by Ethnicity
We next examined whether relationship quality variables were associated with outcomes independent of SES, and whether these associations differed across ethnic groups. For all regressions, in Step 1, the covariates (SES, adolescent sex, adolescent age, illness duration, pump status, and time since HbA1c assessment) were entered. In Step 2, the main effects were entered (acceptance and ethnicity or conflict and ethnicity), allowing us to test associations of relationship quality with outcomes independent of SES and illness-related variables. In Step 3, the interaction of relationship quality (acceptance or conflict) with ethnicity was entered to test whether these associations differed across ethnicity. All continuous predictors were mean centered, as suggested by Aiken and West (1991). Separate models for each relationship quality variable (adolescent-reported mother and father acceptance, adolescent- and mother-reported diabetes conflicts with mothers, and adolescent-reported diabetes conflicts with fathers) predicting each outcome (HbA1c, mother- and adolescent-reported adherence, depressive symptoms) resulted in 20 total regressions.
As shown in Step 2 of Table III, relationship quality associations with outcomes generally remained after covarying SES and other variables. Adolescent-reported mother and father acceptance correlated with higher adolescent-reported adherence and fewer depressive symptoms. Mother-reported diabetes conflicts correlated with higher HbA1c and lower mother-reported adherence. Adolescent-reported diabetes conflicts were not associated with any outcomes.
Multiple Regressions Predicting Glycemic Control, Adherence, and Depressive Symptoms From Parental Acceptance, Diabetes Conflict With Parents, and Ethnicity
| Variable . | DV: glycated hemoglobin (HbA1c) . | DV: adherence (A) . | DV: adherence (M) . | DV: depressive symptoms (A) . | ||||
|---|---|---|---|---|---|---|---|---|
| β . | ΔR2 . | β . | ΔR2 . | β . | ΔR2 . | β . | ΔR2 . | |
| Regressions using adolescent-reported mother acceptance as a predictor | ||||||||
| Step 1 | .23*** | .11* | .10* | .06 | ||||
| Socioeconomic status (SES) | −.22* | .04 | .04 | −.05 | ||||
| Adolescent sex | −.22* | −.18 | .02 | .08 | ||||
| Adolescent age | .14 | −.24** | −.27** | .13 | ||||
| Illness duration | .31*** | .03 | −.14 | .15 | ||||
| Pump status | .26** | −.07 | .00 | .11 | ||||
| Step 2 | .00 | .03 | .02 | .11*** | ||||
| Ethnicity | .06 | .01 | .16 | .04 | ||||
| Mother acceptance (A) | −.03 | .18* | .00 | −.35*** | ||||
| Step 3 | .02 | .00 | .03† | .00 | ||||
| Acceptance X ethnicity | −.22 | −.07 | −.26 | .01 | ||||
| Regressions using adolescent-reported father acceptance as a predictor | ||||||||
| Ethnicity | .06 | .00 | .03 | .04 | .17 | .03 | .07 | .08** |
| Father acceptance (A) | −.03 | .20* | .14 | −.28** | ||||
| Acceptance X ethnicity | .24 | .03 | .10 | .00 | −.08 | .00 | .10 | .00 |
| Regressions using adolescent-reported diabetes conflicts with mothers as a predictor | ||||||||
| Ethnicity | .06 | .00 | −.02 | .00 | .17 | .02 | .08 | .03 |
| Mother conflict (A) | .03 | .01 | −.07 | .15 | ||||
| Conflict X ethnicity | −.09 | .00 | .17 | .01 | .26* | .04* | −.16 | .01 |
| Regressions using mother-reported diabetes conflicts with mothers as a predictor | ||||||||
| Ethnicity | −.01 | .05* | .03 | .02 | .26* | .08** | .06 | .04† |
| Mother conflict (M) | .24* | −.16 | −.54*** | .19 | ||||
| Conflict X ethnicity | −.14 | .01 | .12 | .01 | .33* | .04* | −.12 | .01 |
| Regressions using adolescent-reported diabetes conflicts with fathers as a predictor | ||||||||
| Ethnicity | .06 | .00 | .00 | .01 | .14 | .02 | .10 | .01 |
| Father conflict (A) | .02 | .11 | .03 | .02 | ||||
| Conflict X ethnicity | −.14 | .01 | .26 | .03 | .30* | .04* | −.18 | .01 |
| Variable . | DV: glycated hemoglobin (HbA1c) . | DV: adherence (A) . | DV: adherence (M) . | DV: depressive symptoms (A) . | ||||
|---|---|---|---|---|---|---|---|---|
| β . | ΔR2 . | β . | ΔR2 . | β . | ΔR2 . | β . | ΔR2 . | |
| Regressions using adolescent-reported mother acceptance as a predictor | ||||||||
| Step 1 | .23*** | .11* | .10* | .06 | ||||
| Socioeconomic status (SES) | −.22* | .04 | .04 | −.05 | ||||
| Adolescent sex | −.22* | −.18 | .02 | .08 | ||||
| Adolescent age | .14 | −.24** | −.27** | .13 | ||||
| Illness duration | .31*** | .03 | −.14 | .15 | ||||
| Pump status | .26** | −.07 | .00 | .11 | ||||
| Step 2 | .00 | .03 | .02 | .11*** | ||||
| Ethnicity | .06 | .01 | .16 | .04 | ||||
| Mother acceptance (A) | −.03 | .18* | .00 | −.35*** | ||||
| Step 3 | .02 | .00 | .03† | .00 | ||||
| Acceptance X ethnicity | −.22 | −.07 | −.26 | .01 | ||||
| Regressions using adolescent-reported father acceptance as a predictor | ||||||||
| Ethnicity | .06 | .00 | .03 | .04 | .17 | .03 | .07 | .08** |
| Father acceptance (A) | −.03 | .20* | .14 | −.28** | ||||
| Acceptance X ethnicity | .24 | .03 | .10 | .00 | −.08 | .00 | .10 | .00 |
| Regressions using adolescent-reported diabetes conflicts with mothers as a predictor | ||||||||
| Ethnicity | .06 | .00 | −.02 | .00 | .17 | .02 | .08 | .03 |
| Mother conflict (A) | .03 | .01 | −.07 | .15 | ||||
| Conflict X ethnicity | −.09 | .00 | .17 | .01 | .26* | .04* | −.16 | .01 |
| Regressions using mother-reported diabetes conflicts with mothers as a predictor | ||||||||
| Ethnicity | −.01 | .05* | .03 | .02 | .26* | .08** | .06 | .04† |
| Mother conflict (M) | .24* | −.16 | −.54*** | .19 | ||||
| Conflict X ethnicity | −.14 | .01 | .12 | .01 | .33* | .04* | −.12 | .01 |
| Regressions using adolescent-reported diabetes conflicts with fathers as a predictor | ||||||||
| Ethnicity | .06 | .00 | .00 | .01 | .14 | .02 | .10 | .01 |
| Father conflict (A) | .02 | .11 | .03 | .02 | ||||
| Conflict X ethnicity | −.14 | .01 | .26 | .03 | .30* | .04* | −.18 | .01 |
Notes. (M) = mother report; (A) = adolescent report, β = standardized regression coefficient, DV = dependent variable. ***p < .001, **p < .01, *p < .05. In all regression equations, the covariates (age, sex, SES, time since HbA1c assessment, illness duration, and pump status) were controlled. Step 2 represents main effects before the interaction term is entered into the model.
Multiple Regressions Predicting Glycemic Control, Adherence, and Depressive Symptoms From Parental Acceptance, Diabetes Conflict With Parents, and Ethnicity
| Variable . | DV: glycated hemoglobin (HbA1c) . | DV: adherence (A) . | DV: adherence (M) . | DV: depressive symptoms (A) . | ||||
|---|---|---|---|---|---|---|---|---|
| β . | ΔR2 . | β . | ΔR2 . | β . | ΔR2 . | β . | ΔR2 . | |
| Regressions using adolescent-reported mother acceptance as a predictor | ||||||||
| Step 1 | .23*** | .11* | .10* | .06 | ||||
| Socioeconomic status (SES) | −.22* | .04 | .04 | −.05 | ||||
| Adolescent sex | −.22* | −.18 | .02 | .08 | ||||
| Adolescent age | .14 | −.24** | −.27** | .13 | ||||
| Illness duration | .31*** | .03 | −.14 | .15 | ||||
| Pump status | .26** | −.07 | .00 | .11 | ||||
| Step 2 | .00 | .03 | .02 | .11*** | ||||
| Ethnicity | .06 | .01 | .16 | .04 | ||||
| Mother acceptance (A) | −.03 | .18* | .00 | −.35*** | ||||
| Step 3 | .02 | .00 | .03† | .00 | ||||
| Acceptance X ethnicity | −.22 | −.07 | −.26 | .01 | ||||
| Regressions using adolescent-reported father acceptance as a predictor | ||||||||
| Ethnicity | .06 | .00 | .03 | .04 | .17 | .03 | .07 | .08** |
| Father acceptance (A) | −.03 | .20* | .14 | −.28** | ||||
| Acceptance X ethnicity | .24 | .03 | .10 | .00 | −.08 | .00 | .10 | .00 |
| Regressions using adolescent-reported diabetes conflicts with mothers as a predictor | ||||||||
| Ethnicity | .06 | .00 | −.02 | .00 | .17 | .02 | .08 | .03 |
| Mother conflict (A) | .03 | .01 | −.07 | .15 | ||||
| Conflict X ethnicity | −.09 | .00 | .17 | .01 | .26* | .04* | −.16 | .01 |
| Regressions using mother-reported diabetes conflicts with mothers as a predictor | ||||||||
| Ethnicity | −.01 | .05* | .03 | .02 | .26* | .08** | .06 | .04† |
| Mother conflict (M) | .24* | −.16 | −.54*** | .19 | ||||
| Conflict X ethnicity | −.14 | .01 | .12 | .01 | .33* | .04* | −.12 | .01 |
| Regressions using adolescent-reported diabetes conflicts with fathers as a predictor | ||||||||
| Ethnicity | .06 | .00 | .00 | .01 | .14 | .02 | .10 | .01 |
| Father conflict (A) | .02 | .11 | .03 | .02 | ||||
| Conflict X ethnicity | −.14 | .01 | .26 | .03 | .30* | .04* | −.18 | .01 |
| Variable . | DV: glycated hemoglobin (HbA1c) . | DV: adherence (A) . | DV: adherence (M) . | DV: depressive symptoms (A) . | ||||
|---|---|---|---|---|---|---|---|---|
| β . | ΔR2 . | β . | ΔR2 . | β . | ΔR2 . | β . | ΔR2 . | |
| Regressions using adolescent-reported mother acceptance as a predictor | ||||||||
| Step 1 | .23*** | .11* | .10* | .06 | ||||
| Socioeconomic status (SES) | −.22* | .04 | .04 | −.05 | ||||
| Adolescent sex | −.22* | −.18 | .02 | .08 | ||||
| Adolescent age | .14 | −.24** | −.27** | .13 | ||||
| Illness duration | .31*** | .03 | −.14 | .15 | ||||
| Pump status | .26** | −.07 | .00 | .11 | ||||
| Step 2 | .00 | .03 | .02 | .11*** | ||||
| Ethnicity | .06 | .01 | .16 | .04 | ||||
| Mother acceptance (A) | −.03 | .18* | .00 | −.35*** | ||||
| Step 3 | .02 | .00 | .03† | .00 | ||||
| Acceptance X ethnicity | −.22 | −.07 | −.26 | .01 | ||||
| Regressions using adolescent-reported father acceptance as a predictor | ||||||||
| Ethnicity | .06 | .00 | .03 | .04 | .17 | .03 | .07 | .08** |
| Father acceptance (A) | −.03 | .20* | .14 | −.28** | ||||
| Acceptance X ethnicity | .24 | .03 | .10 | .00 | −.08 | .00 | .10 | .00 |
| Regressions using adolescent-reported diabetes conflicts with mothers as a predictor | ||||||||
| Ethnicity | .06 | .00 | −.02 | .00 | .17 | .02 | .08 | .03 |
| Mother conflict (A) | .03 | .01 | −.07 | .15 | ||||
| Conflict X ethnicity | −.09 | .00 | .17 | .01 | .26* | .04* | −.16 | .01 |
| Regressions using mother-reported diabetes conflicts with mothers as a predictor | ||||||||
| Ethnicity | −.01 | .05* | .03 | .02 | .26* | .08** | .06 | .04† |
| Mother conflict (M) | .24* | −.16 | −.54*** | .19 | ||||
| Conflict X ethnicity | −.14 | .01 | .12 | .01 | .33* | .04* | −.12 | .01 |
| Regressions using adolescent-reported diabetes conflicts with fathers as a predictor | ||||||||
| Ethnicity | .06 | .00 | .00 | .01 | .14 | .02 | .10 | .01 |
| Father conflict (A) | .02 | .11 | .03 | .02 | ||||
| Conflict X ethnicity | −.14 | .01 | .26 | .03 | .30* | .04* | −.18 | .01 |
Notes. (M) = mother report; (A) = adolescent report, β = standardized regression coefficient, DV = dependent variable. ***p < .001, **p < .01, *p < .05. In all regression equations, the covariates (age, sex, SES, time since HbA1c assessment, illness duration, and pump status) were controlled. Step 2 represents main effects before the interaction term is entered into the model.
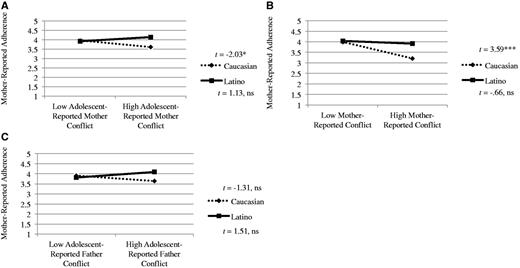
As displayed in Step 3 of Table III, ethnicity interacted with some aspects of relationship quality to predict outcomes. In contrast to expectations, however, diabetes conflicts were associated with poorer outcomes in Caucasian compared with Latino adolescents. Specifically, diabetes conflicts with mothers (adolescent and mother reports) and with fathers (adolescent report) interacted with ethnicity to predict mother-reported adherence. As shown in Figure 1, simple slopes tests of the plotted regression lines revealed diabetes conflict with mothers was associated with poorer adherence for Caucasians, but the slope was not significantly different from zero for the Latinos. For diabetes conflicts with fathers, there was a similar pattern, though the slope of the regression line for each group was not significantly different from zero.
(A) Adolescent-reported diabetes conflict with mothers and ethnicity predicting mother-reported adherence. (B) Mother-reported diabetes conflict with adolescents and ethnicity predicting mother-reported adherence. (C) Adolescent-reported diabetes conflict with fathers and ethnicity predicting mother-reported adherence.
Discussion
The present study is among the first to examine the role of family processes in adolescent type 1 diabetes management in a diverse sample of Caucasian and Latino youth. Consistent with research on primarily Caucasian samples, adolescent-reported mother and father acceptance were associated with better adjustment, whereas diabetes conflict with mothers (across reporter) was associated with poorer adjustment. However, ethnic differences emerged in both the level of relationship quality variables and in their associations with outcomes even after controlling for SES. Such findings suggest a need to more fully examine whether and how family factors that have been consistently associated with diabetes management among Caucasians may generalize to Latinos or other ethnic minorities.
The findings that acceptance was lower and diabetes conflict was higher among Latinos compared with Caucasians are consistent with the general literature indicating that Latino parents may engage in more authoritarian parenting practices compared with Caucasians (Calzada et al., 2012), which has implications for amount of parent–adolescent conflict and parental acceptance (Smetana, 1995). Because differences in relationship quality were found independently of SES, acculturation might influence these family processes (Hsin et al., 2010). Specifically, as immigrant Latino families become acculturated to U.S. culture, parental control and parent–adolescent conflict might decrease.1 Future research examining dimensions of parenting simultaneously (e.g., levels of acceptance considered combined with levels of control and conflict) and the effect of acculturation on these associations would contribute to our understanding of cultural aspects of parenting in the context of diabetes management.
Despite these group differences, Latino adolescents did not have significantly different diabetes outcomes than Caucasians, and there was some evidence that diabetes conflict was more strongly associated with outcomes for Caucasians than for Latinos. These findings ran counter to our hypothesis that relationship quality variables would be more strongly associated with diabetes management among Latinos because of the central role of family in Latino culture. However, there is some evidence that parenting is associated less strongly with adjustment for Latinos compared with Caucasians (Halgunseth, Ispa, & Rudy, 2006). Therefore, lower diabetes conflict may not have had the same level of protective effects on health outcomes among Latinos compared with Caucasians. Future research exploring possible protective mechanisms for Latino families in the context of diabetes management is needed. Interestingly, these findings were only present for mother-reported adherence as an outcome. Although measures in the present study were forward and back translated, using measures that are specifically designed for use with Latino samples is an important future direction.
There are several limitations in the present study. First, the cross-sectional design prevents causal interpretations or exploration of how shifts in parent–adolescent relationship characteristics affect diabetes management over time. Second, Latinos are a heterogeneous group, and this sample consisted primarily of Mexican-American families. Future research including Latino families from multiple ethnic backgrounds (e.g., Dominican Americans, Cuban Americans) would ensure more representative research on Latinos (Calzada et al., 2012). Third, although the present study included both mother and adolescent report, fathers’ reports of their own relationship quality were not obtained. Fourth, self-report measures may not accurately assess adherence or relationship variables. Although there were some cross-reporter effects, associations were stronger within reporter than across reporter. Future research using observational and interview methodologies may better capture such constructs across ethnicity. Fifth, we did not correct for type 1 error given the paucity of data available in Latino youth with type 1 diabetes. Finally, SES is a complex construct, and the combination of neighborhood income and parental education may not capture the nuances of SES in the context of diabetes management. There is a need to replicate these findings in a larger sample.
The present investigation contributes to our understanding of the associations of relationship quality with diabetes management in a socioeconomically and ethnically diverse sample of Latino and Caucasian youth. There has been little work examining both positive (e.g., acceptance) and negative (e.g., conflict) aspects of parent–adolescent relationship quality in a single study, so this study contributes to our understanding of how these processes affect adolescent diabetes management and depressive symptoms across different domains of the relationship with both mothers and fathers. The present study also contributes to a growing body of literature that parental acceptance and less conflict (at least with mothers) is related to better glycemic control, better adherence, and fewer depressive symptoms. More research needs to be done to elucidate the protective factors that may buffer Latino adolescents from poor illness management despite lower reported parent–adolescent relationship quality. The present study holds implications that clinicians should make parents aware of the important role of family support in helping adolescents manage their diabetes across adolescence. Identifying features of parent–adolescent relationships that make the transition to more autonomous self-care for adolescents smooth and how these characteristics may vary by culture is crucial for promoting positive health outcomes across adolescence.
Acknowledgments
The authors wish to thank Ryan Garcia, Alyssa Parker, and Vincent Tran for assisting in participant recruitment, data collection, and data management. We are also grateful to the staff at the Pediatric Endocrinology Clinics at Children’s Medical Center Dallas and to all families who participated in the study.
Funding
This research was supported by a grant from the Timberlawn Psychiatric Research Foundation awarded to Deborah Wiebe while at the University of Texas Southwestern Medical Center, Dallas.
Conflicts of interest: None declared.
1 The present study included measures of acculturation for the Latino subsample. We conducted partial correlations to examine associations between Latino and Caucasian cultural orientations and relationship quality variables controlling for SES. Results indicated that mothers’ Mexican cultural orientation was associated with lower adolescent-reported mother acceptance.