-
PDF
- Split View
-
Views
-
Cite
Cite
Holly Antal, M. Jobayer Hossain, Sandra Hassink, Shannon Henry, Lindsay Fuzzell, Alex Taylor, Tim Wysocki, Audio-Video Recording of Health Care Encounters for Pediatric Chronic Conditions: Observational Reactivity and Its Correlates, Journal of Pediatric Psychology, Volume 40, Issue 1, January/February 2015, Pages 144–153, https://doi.org/10.1093/jpepsy/jsu046
Close - Share Icon Share
Abstract
Objectives Audio-video recording of pediatric clinic visits could generate observational reactivity, affecting measures of communication among patients, parents, and clinicians. Methods We measured observational reactivity in a direct observation study of communication during 155 pediatric visits for any of 5 chronic conditions by coding camcorder awareness behaviors and self-report questionnaires. We analyzed associations between observational reactivity and measures of communication behavior and visit quality. Results Directly observed camcorder awareness behaviors (634 events) comprised 0.59% of all coded events (n = 107,668). Younger children displayed these behaviors more often than did older children (F = 6.47; p < .0001). Clinicians’ camcorder awareness declined significantly over successive study visits (t = −2.096; p = .043). Associations of camcorder awareness with objectively scored communication behaviors or self-reported visit quality were negligible. Conclusions Most recordings included slight evidence of participant camcorder awareness. But there was negligible evidence that camcorder awareness influenced clinic visit communication.
Introduction
Family management of pediatric chronic conditions may be impacted significantly by the quality of communication during health care visits (Cox, Smith, Brown, & Fitzpatrick, 2007; Gavin, Wamboldt, Sorokin, & Levy,1999; Wissow, Brown, & Krupnick, 2010). Effective communication may promote shared understanding of treatment goals and regimen details, facilitate detection of psychosocial barriers to adequate family adaptation to the child’s medical condition, and permit effective anticipatory guidance regarding projected developmental hurdles. Communication during pediatric clinic visits and its associations with care outcomes have been studied extensively in primary care, (e.g. Cox, Smith, Brown, & Fitzpatrick, 2009; Di Matteo, 2004; Drotar, 2009; Nobile & Drotar, 2003; Wissow et al., 2010; Wissow, Wilson, & Roter, 1994) but less so in subspecialty pediatrics (Cohen & Wamboldt, 2000; Gavin et al., 1999). Youth with chronic medical conditions may have more clinic visits than other children and their interactions with health care providers (HCPs) about disease management may differ from those in primary care. It is especially difficult to study these processes in pediatrics because health care visits are assumed to be private and because the child’s role in these interactions tends to change continuously in parallel with the child’s developmental maturation. Further, communication in pediatric visits is inherently triadic (patient–parent–health care provider) (Cahill & Papageorgiu, 2007a, b). Thus, measurement of these interactions is complex, as are the associations among communication behaviors and care outcomes.
One approach to the objective measurement of communication during pediatric health care visits consists of direct observation of those encounters, either through immediate presence of an observer in the visit or by collection of audio-video recording of the visit (Cahill & Papageorgiou 2007b; Cox et al., 2009; Roter & Hall, 1987). While such direct observation methods could potentially be more objective than measurement of visit interactions via participants’ recall of the details of the clinical encounter, the former methods intrude into a sensitive interaction that is typically respected as private and confidential. More intrusive assessment methods, such as direct observation, may be particularly prone to yield observational reactivity, which can be defined as that process by which observation of a phenomenon changes that phenomenon (Heppner, Wampold, & Kivlighan, 2008). Direct observation methods are perhaps more likely than self-report or recall methods of assessment to yield observational reactivity, altering the nature of communication among HCPs, parents, and youth, thus changing the very subject matter of interest. Therefore, a prerequisite to conducting rigorous direct observation research on communication during pediatric care encounters is an assessment of the extent of reactivity generated by direct observation.
We conducted a prospective study that obtains audio-video recordings of clinic visits for chronic medical conditions involving pediatric HCPs, children, and parents. In addition to other study procedures, participating HCPs, patients, and parents consented to audio-video recording of three successive routine clinic visits, but the present report is based solely on data obtained at the first such visit for each family. The study is based on a conceptual framework linking contextual variables (i.e. socioeconomic status [SES], health literacy, child age) to characteristics of health care interactions (i.e. communication ratings, shared decision making, affective expression) that in turn may affect proximal outcomes of the clinic visit (i.e. satisfaction, treatment alliance, recall of treatment responsibilities) and, ultimately, distal outcomes of care (health status, treatment adherence, quality of life). Because these issues have not been studied in the context of subspecialty pediatrics, the sample of participants enrolled in the study was intentionally diverse in terms of child age (5 through 17 years) and medical diagnosis (any of five chronic conditions). The present article focuses on the extent to which observational reactivity could be detected and its associations with directly observed communication during clinic visits and proximal outcomes of those visits.
The study methods include two broad strategies for the measurement of observational reactivity: (1) Along with other observational coding tasks, trained independent raters scored the occurrence of five categories of overt camcorder awareness behaviors among HCPs, parents, and youth; and (2) HCPs and parents reported on the extent to which camcorder awareness affected their own, and the others’, behaviors during the study visits compared with their clinic visits before the study. The purposes of this article were to evaluate the extent of observational reactivity detected by these two distinct methods and to analyze whether the extent of observational reactivity revealed by these methods was associated with differences in directly observed communication behavior of the study participants. These data could permit evaluation of the degree to which observational reactivity supports or negates the merits of direct observation methods in studies of communication during pediatric subspecialty care visits. We expected to find that directly observed camcorder awareness behaviors were uncommon, that participants’ self reports would indicate that camcorder presence had negligible effects on participants’ behavior during visits, and that directly observed communication during the visits was not associated significantly with these indices of camcorder effects. This article evaluates these four hypotheses regarding the magnitude of observational reactivity in this study:
Hypothesis 1: Distributions of HCP ratings of perceived influence of camcorder presence on their own behavior and that of parents/patients will demonstrate negligible evidence of observational reactivity.
Hypothesis 2: Distributions of parental ratings of the extent to which they noticed the camcorder and perceived behavioral effects of the camcorder on themselves, their children or their HCPs will demonstrate negligible evidence of observational reactivity.
Hypothesis 3: The frequency of directly observed camcorder awareness behaviors will be <1% of all coded events, will be significantly more common among children than adults, and will be inversely correlated with child age.
Hypothesis 4: Scores on measures of visit interactions completed by trained raters, HCPs, parents, and children will not be correlated significantly with the frequency of directly observed camcorder awareness behaviors or with parent or HCP reports of behavioral effects of camcorder presence.
We have not attempted to cast our work in a theoretical framework because this study was not designed with a primary aim of understanding observational reactivity. Instead, the article is a methodological analysis that we see as an important contribution to verify that the findings of the overall study, which was designed with a clearly stated conceptual framework, were obtained in a methodologically rigorous, reliable, and valid manner.
Method
Settings
The research was done at five outpatient pediatric medical centers that comprised a pediatric health care system in the Mid-Atlantic and southeastern United States. The study received initial and ongoing approval by an institutional review board (IRB) regarding protection of research volunteers. Each participant signed the appropriate informed consent, parental permission, or children’s assent form before any research procedures.
Participants
Participants were HCPs, child and adolescent patients, and parents or other legal caregivers of each patient. HCPs included physicians (MD), advanced practice nurses (APN), and physician’s assistants (PA) who had primary responsibility for the medical management of youth with either: Acute lymphoblastic leukemia (ALL), asthma (moderately severe or severe persistent), cystic fibrosis, diabetes mellitus (type 1), or obesity. Because there have been no previous direct observation studies in subspecialty pediatrics, a wide variety of medical diagnoses were targeted. The research team sought to enroll up to 15 patients of each enrolled HCP for one of these diagnoses and a parent or other caregiver. Eligibility criteria are specified below.
HCP Enrollment Criteria.Inclusion: MD, APN, or PA responsible for the medical management of patients with one of the targeted diagnoses; agreed to facilitate recruitment of up to 15 established patients with one of these diagnoses; and agreed to participate in the study protocol as described below. Exclusion: Expecting to move during the study.
Youth Enrollment Criteria.Inclusion: Age ≥5 years but <17 years at baseline; diagnosed with a medical condition meeting disease-specific enrollment criteria defined below; considered developmentally normal by the treating HCP; established care at the enrolling site; and sufficient English fluency to converse and to complete study questionnaires (younger children or those with reading problems had items read to them). Exclusion: Disorder of hearing, language, or speech that significantly impeded communication during health care encounters and unlikely to continue to receive medical care for the index condition for the 6 months following study enrollment. The age range was selected based on the intent to capture the full developmental range of meaningful involvement of children and HCPs during health care encounters.
Parent/Caregiver Enrollment Criteria.Inclusion: Biological parent or legally appointed caregiver of a study patient; at least weekly involvement in the child’s medical care (e.g. administering medications, monitoring symptoms, making/keeping appointments, phone contacts with clinic, etc.); and able to converse in English and to understand and complete study questionnaires. Exclusion: Disorder of hearing, language, or speech that significantly impeded communication during health care encounters; expecting to move or otherwise terminate care at the enrolling clinic within 6 months after study entry; and expecting to relinquish responsibility for the participating child’s health care within 6 months of study entry.
Additional Diagnosis-Specific Eligibility Criteria.Inclusion: (1) ALL patients with standard-risk or high-risk ALL enrolled either at the start of Consolidation Therapy or during the first year of Maintenance Therapy; (2) asthma patients with moderate to severe persistent asthma based on the patient’s/caregiver’s recall of symptoms over the previous 4 weeks, current spirometry, and medications needed to maintain asthma control; (3) children with a primary diagnosis of cystic fibrosis; (4) patients who have been diagnosed with type 1 diabetes mellitus ≥1 year and most recent glycated hemoglobin (HbA1c) of ≤ 11%; and (5) children with age-adjusted body mass index ≥ 95th percentile.
Sample Characteristics
Health Care Providers. Potentially eligible HCPs (n = 61) were first notified about the study by e-mail. Of those 61 HCPs, 53 were later contacted by phone and determined to be eligible. Then, 28 of those HCPs (23 MD, 3 APNs, and 2 PAs) signed informed consent forms and enrolled in the study (53%). Ultimately, patients/parents were recruited for 20 of the enrolled HCPs (16 MD, 2 APNs, and 2 PAs). A variety of issues prevented enrollment of patients for all participating HCPs (uncommon medical diagnoses, limited study budget, clinic logistics, budgetary constraints).
Patients and Parents/Caregivers. Parents or other legal caregivers of potentially eligible children or adolescents with one of the targeted diagnoses were contacted by mail (n = 511). Of those sent a letter about the study, 383 were later reached by telephone about study participation. Of those contacted by telephone and verified as eligible, 170 (45%) agreed to be in the study following an IRB-approved telephone consent conversation. Written parental permission was obtained from 166 parents (89.2% mothers) of 157 youth just before their first study visits. Written assent was obtained from all children ≥7 years of age. Of the 157 youth who enrolled, baseline visits were completed for 155. Two young children dissented from participation as the baseline visit began, and so no data were collected from them. Table I summarizes demographic characteristics of the full sample. The mean (±SD) score on the Hollingshead Four-Factor Index of Social Status was 42.7 ± 14.2, indicative of predominantly middle class families.
Demographic Characteristics of the 155 Patients and 158 Parents/Caregivers Who Participated
| Youths . | Mean . | SD . | . |
|---|---|---|---|
| Age (years) | 10.85 | 3.28 | |
| % Youths | |||
| Race | |||
| Caucasian | 65.2 | ||
| African–American | 21.9 | ||
| Other/multiple | 12.9 | ||
| Ethnicity | |||
| Non-Hispanic | 85.2 | ||
| Hispanic | 14.8 | ||
| Child gender | |||
| Male | 51.6 | ||
| Female | 48.4 | ||
| Medical diagnoses | |||
| Asthma | 27.7 | ||
| Cystic fibrosis | 9.0 | ||
| Diabetes | 28.4 | ||
| Leukemia | 2.6 | ||
| Obesity | 32.3 | ||
| Parents/caregivers | Mean | SD | |
| Age (mother) | 39.72 | 6.58 | |
| Age (father) | 39.69 | 4.77 | |
| Hollings head Four-Factor Index raw score | 42.71 | 14.20 | |
| % Mothers | % Fathers | % Others | |
| Caucasian | 69.2 | 84.6 | 50 |
| African–American | 21.7 | 15.4 | 50 |
| Other | 9.1 | 0 | 0 |
| Hispanic | 15.4 | 15.4 | 0 |
| Highest educational level | |||
| <High school | 2.1 | 0 | 0 |
| High school graduate | 14 | 23.1 | 50 |
| Some college | 42.7 | 46.2 | 50 |
| College graduate | 28 | 7.7 | 0 |
| Advanced degree | 13.3 | 23.1 | 0 |
| Self-reported occupational category | |||
| Executive; professional; owner of large business | 12.6 | 7.7 | 0 |
| Administrator; manager Owner of medium-large business | 11.2 | 23.1 | 0 |
| Lower-level manager; owner of medium-small business; teacher, computer professional; allied health professional | 26.6 | 23.1 | 0 |
| Technician; owner of small business | 2.1 | 15.4 | 0 |
| Clerical; retail sales; public safety | 9.8 | 7.7 | 0 |
| Skilled manufacturing, repair technician; craftsman | 1.4 | 7.7 | 0 |
| Transportation and logistics; service occupation | 1.4 | 7.7 | 0 |
| Manual labor; assistant to craftsman or technician; | 0.7 | 0 | 0 |
| Not currently employed | 32.2 | 7.7 | 100 |
| Youths . | Mean . | SD . | . |
|---|---|---|---|
| Age (years) | 10.85 | 3.28 | |
| % Youths | |||
| Race | |||
| Caucasian | 65.2 | ||
| African–American | 21.9 | ||
| Other/multiple | 12.9 | ||
| Ethnicity | |||
| Non-Hispanic | 85.2 | ||
| Hispanic | 14.8 | ||
| Child gender | |||
| Male | 51.6 | ||
| Female | 48.4 | ||
| Medical diagnoses | |||
| Asthma | 27.7 | ||
| Cystic fibrosis | 9.0 | ||
| Diabetes | 28.4 | ||
| Leukemia | 2.6 | ||
| Obesity | 32.3 | ||
| Parents/caregivers | Mean | SD | |
| Age (mother) | 39.72 | 6.58 | |
| Age (father) | 39.69 | 4.77 | |
| Hollings head Four-Factor Index raw score | 42.71 | 14.20 | |
| % Mothers | % Fathers | % Others | |
| Caucasian | 69.2 | 84.6 | 50 |
| African–American | 21.7 | 15.4 | 50 |
| Other | 9.1 | 0 | 0 |
| Hispanic | 15.4 | 15.4 | 0 |
| Highest educational level | |||
| <High school | 2.1 | 0 | 0 |
| High school graduate | 14 | 23.1 | 50 |
| Some college | 42.7 | 46.2 | 50 |
| College graduate | 28 | 7.7 | 0 |
| Advanced degree | 13.3 | 23.1 | 0 |
| Self-reported occupational category | |||
| Executive; professional; owner of large business | 12.6 | 7.7 | 0 |
| Administrator; manager Owner of medium-large business | 11.2 | 23.1 | 0 |
| Lower-level manager; owner of medium-small business; teacher, computer professional; allied health professional | 26.6 | 23.1 | 0 |
| Technician; owner of small business | 2.1 | 15.4 | 0 |
| Clerical; retail sales; public safety | 9.8 | 7.7 | 0 |
| Skilled manufacturing, repair technician; craftsman | 1.4 | 7.7 | 0 |
| Transportation and logistics; service occupation | 1.4 | 7.7 | 0 |
| Manual labor; assistant to craftsman or technician; | 0.7 | 0 | 0 |
| Not currently employed | 32.2 | 7.7 | 100 |
Demographic Characteristics of the 155 Patients and 158 Parents/Caregivers Who Participated
| Youths . | Mean . | SD . | . |
|---|---|---|---|
| Age (years) | 10.85 | 3.28 | |
| % Youths | |||
| Race | |||
| Caucasian | 65.2 | ||
| African–American | 21.9 | ||
| Other/multiple | 12.9 | ||
| Ethnicity | |||
| Non-Hispanic | 85.2 | ||
| Hispanic | 14.8 | ||
| Child gender | |||
| Male | 51.6 | ||
| Female | 48.4 | ||
| Medical diagnoses | |||
| Asthma | 27.7 | ||
| Cystic fibrosis | 9.0 | ||
| Diabetes | 28.4 | ||
| Leukemia | 2.6 | ||
| Obesity | 32.3 | ||
| Parents/caregivers | Mean | SD | |
| Age (mother) | 39.72 | 6.58 | |
| Age (father) | 39.69 | 4.77 | |
| Hollings head Four-Factor Index raw score | 42.71 | 14.20 | |
| % Mothers | % Fathers | % Others | |
| Caucasian | 69.2 | 84.6 | 50 |
| African–American | 21.7 | 15.4 | 50 |
| Other | 9.1 | 0 | 0 |
| Hispanic | 15.4 | 15.4 | 0 |
| Highest educational level | |||
| <High school | 2.1 | 0 | 0 |
| High school graduate | 14 | 23.1 | 50 |
| Some college | 42.7 | 46.2 | 50 |
| College graduate | 28 | 7.7 | 0 |
| Advanced degree | 13.3 | 23.1 | 0 |
| Self-reported occupational category | |||
| Executive; professional; owner of large business | 12.6 | 7.7 | 0 |
| Administrator; manager Owner of medium-large business | 11.2 | 23.1 | 0 |
| Lower-level manager; owner of medium-small business; teacher, computer professional; allied health professional | 26.6 | 23.1 | 0 |
| Technician; owner of small business | 2.1 | 15.4 | 0 |
| Clerical; retail sales; public safety | 9.8 | 7.7 | 0 |
| Skilled manufacturing, repair technician; craftsman | 1.4 | 7.7 | 0 |
| Transportation and logistics; service occupation | 1.4 | 7.7 | 0 |
| Manual labor; assistant to craftsman or technician; | 0.7 | 0 | 0 |
| Not currently employed | 32.2 | 7.7 | 100 |
| Youths . | Mean . | SD . | . |
|---|---|---|---|
| Age (years) | 10.85 | 3.28 | |
| % Youths | |||
| Race | |||
| Caucasian | 65.2 | ||
| African–American | 21.9 | ||
| Other/multiple | 12.9 | ||
| Ethnicity | |||
| Non-Hispanic | 85.2 | ||
| Hispanic | 14.8 | ||
| Child gender | |||
| Male | 51.6 | ||
| Female | 48.4 | ||
| Medical diagnoses | |||
| Asthma | 27.7 | ||
| Cystic fibrosis | 9.0 | ||
| Diabetes | 28.4 | ||
| Leukemia | 2.6 | ||
| Obesity | 32.3 | ||
| Parents/caregivers | Mean | SD | |
| Age (mother) | 39.72 | 6.58 | |
| Age (father) | 39.69 | 4.77 | |
| Hollings head Four-Factor Index raw score | 42.71 | 14.20 | |
| % Mothers | % Fathers | % Others | |
| Caucasian | 69.2 | 84.6 | 50 |
| African–American | 21.7 | 15.4 | 50 |
| Other | 9.1 | 0 | 0 |
| Hispanic | 15.4 | 15.4 | 0 |
| Highest educational level | |||
| <High school | 2.1 | 0 | 0 |
| High school graduate | 14 | 23.1 | 50 |
| Some college | 42.7 | 46.2 | 50 |
| College graduate | 28 | 7.7 | 0 |
| Advanced degree | 13.3 | 23.1 | 0 |
| Self-reported occupational category | |||
| Executive; professional; owner of large business | 12.6 | 7.7 | 0 |
| Administrator; manager Owner of medium-large business | 11.2 | 23.1 | 0 |
| Lower-level manager; owner of medium-small business; teacher, computer professional; allied health professional | 26.6 | 23.1 | 0 |
| Technician; owner of small business | 2.1 | 15.4 | 0 |
| Clerical; retail sales; public safety | 9.8 | 7.7 | 0 |
| Skilled manufacturing, repair technician; craftsman | 1.4 | 7.7 | 0 |
| Transportation and logistics; service occupation | 1.4 | 7.7 | 0 |
| Manual labor; assistant to craftsman or technician; | 0.7 | 0 | 0 |
| Not currently employed | 32.2 | 7.7 | 100 |
Study Design
This prospective observational study involved collection of digital audio-video recordings of routine clinic visits, administration of various questionnaires regarding those visits obtained from patients, their parents, and HCPs who agreed to participate and collection of certain medical record information. Although collection of research data would occur at three successive clinic visits for each participating patient/parent, the present report is limited to data obtained at the first such visit for each patient/parent. Each patient/parent participated in both a core protocol, consisting of collection of generic measures and a substudy that consisted of collection of certain measures that were specific to the child’s medical condition. Some measures were indices of proximal outcomes of study visits (e.g. visit satisfaction), whereas others assessed more stable characteristics (e.g. quality of life, treatment adherence). The present report concerns only the core protocol measures that assessed proximal outcomes of the study visit. The measures and procedures are described below.
Measures and Procedures
The following measures were completed by trained independent raters.
Observational Ratings of Visit Recordings. A digital audio-video camcorder (Sony Handycam HDR-XR150) equipped with a wide angle lens (Raynox HD Wide Angle Conversion Lens HD-5050PRO-LE) was placed in the examination room just before each study visit in a position that maximized capture of the interactions that occurred during the visits. Participants were instructed via the informed consent and assent documents that they could ask that the camcorder be turned off during discussion of sensitive issues or when it was necessary for the child to undress for the physical examination. They were also informed that they could ask to have the recording erased immediately after the visit. No participant requested either such action during the study. HCPs either covered the camcorder lens or diverted the camcorder if the child needed to undress. Research staff retrieved the camcorder immediately after the parent, patient, and HCP left the room at the end of the visit. The camcorder hard drive was then promptly downloaded to a secure password-protected server, and then the camcorder memory was erased. A senior member of the research team randomly assigned visit recordings to each of nine trained raters who then scored each recording using the Roter Interaction Analysis System (RIAS; Roter & Hall, 1987) as it had been adapted for pediatric visits by Cox et al. (2007). Ratings were assigned randomly among raters, resulting in ∼80% of raters’ assigned visits involving HCPs at a different clinic site than the rater’s employment site. Each codeable event was coded according to the person initiating the behavior, a behavioral code selected from among 58 categories, and the person(s) to whom the utterance or other behavior was directed. This system yields summary scores for these 11 dimensions of communication during the visit: Medical Questions; Lifestyle-Psychosocial Questions; Giving Medical Information; Giving Lifestyle-Psychosocial Information; Procedural Talk; Negative Rapport; Positive Rapport; Emotion Focus; Social Focus; Patient Activation; and a Patient-Centeredness Index. Thorough details about the RIAS can be found at this Web site: http://www.riasworks.com/index.html. In addition to the RIAS communication codes, behavioral “states” were also coded as supplements to the RIAS such as physician posture (standing or sitting); physician computer use (using or not using); and certain categories of camcorder awareness behaviors (reactivity) that are described below. The physician posture and computer use codes were not analyzed for the purposes of this article.
Nine raters (the first author and eight masters-level behavioral science research coordinators) completed training in RIAS coding consisting of participation in a 2-day workshop taught by a representative of the RIAS developers followed by group coding of the first six visit recordings made for this study. Each of these recordings was reviewed utterance by utterance on video conference calls to achieve consensus on the coding of specific events, to resolve disagreements, and to refine coding decision rules. By the time all six recordings had been reviewed by the team, disagreements among raters were uncommon and agreement on the more commonly used coding categories was excellent. Subsequent ratings were each completed by one rater because of high reliability and labor intensity of coding process.
To assess interrater agreement throughout the study, on five occasions distributed about 2 months apart, a visit recording was selected at random for independent coding by all nine raters. Once all had completed that coding, two raters were randomly selected to collaborate in producing a “consensus coding” of that recording. The two raters were charged with working utterance by utterance through the visit recording and choosing the most appropriate code for each utterance. Coding issues that could not be resolved were brought to the principal investigator, who resolved it after considering the source of the disagreement in relation to the coding rules. Thereafter, the project statistician calculated several indices of interrater agreement using two general methods: (1) calculation of each rater’s agreement with the “consensus coding” and (2) calculation of each rater’s agreement with the mean scores derived from all other raters. Both methods yielded mean interrater agreement of ≥0.80 on every communication dimension derived from this method, and no evidence was found to suggest significant “observer drift” over time. Average interrater agreement with the “consensus coding” results was Pearson r = 0.906 (range 0.836–0.940) for the individual raters. Average interrater agreement on RIAS scores obtained from each rater compared with those obtained from all other raters was r = 0.873 (range = 0.797–0.940). The team was prepared to increase the frequency of conducting these reliability checks, but the results over time proved this to be unnecessary.
The same rater who coded a given visit recording also completed two rating scales regarding the entire visit. These included the OPTION Scale, a 12-item measure (alpha = .81 for this sample) of the extent to which shared medical decision making occurred during the visit (Elwyn et al., 2003) and the Global Affect Rating Scale (alpha = .81 for this sample) that is part of the RIAS (Roter & Hall, 1987).
Postvisit Recall of Treatment Recommendations. This measure was constructed for this study and consisted of three steps. First, the one rater who scored the visit recording also noted each specific action with respect to the child’s health care discussed during that visit that the parent was expected to complete after the visit. Second, parents and older patients together completed the same form to indicate what they recalled as treatment actions they had agreed to during the visit. Finally, that same rater’s entries were compared with the patient/parent entries to measure accuracy of their recall. Each parent and patient ≥11 years of age completed this measure together just after each clinic visit for the study, reporting actions that they recalled as having been discussed in the areas of medications, diet, exercise, laboratory, or radiologic tests, etc. Their responses were then compared with those obtained separately from the independent raters who recorded the same information as they coded each study visit recording. Because the specific number of treatment actions reported by a given parent/child was free to vary, scoring was calculated as the mean score obtained for all rater-recorded actions, each of which were scored as either 0 (false recall), 1 (unable to recall), 2 (partial recall), and 3 (accurate and detailed recall). Postvisit Recall of Treatment Recommendations (PVR) scores are derived by calculating the quotient of the number of items for which the participant earned a score of “3” (accurate and detailed recall) divided by the number of all items for which the rater entered any category of item score.
Assessment of Observational Reactivity. Participants’ self-reports and raters’ objective behavioral observations were used to assess observational reactivity resulting from the presence of a camcorder at each study visit: Subjective Report: At the completion of each recorded visit, parents were asked (1) “To what extent did you notice the camera during today’s appointment?” (2) “To what extent did the camera affect your behavior during today’s appointment?” (3) “To what extent did the camera affect your child’s behavior during today’s appointment?”, and (4) “To what extent did the behavior of your doctor differ from his/her behavior during previous visits?” Parents responded on a scale of 0 to 3 (0 = not at all, 1 = very little, 2 = somewhat, and 3 = to a great extent). HCPs rated the following statements on a 5-point scale: (1) The behavior of the parent and/or patient was affected by the camera, and (2) My behavior was affected by the camera. Scale responses were as follows: 1 = strongly disagree, 2 = mildly disagree, 3 = neither agree nor disagree, 4 = mildly agree, 5 = strongly agree. Behavioral Observation: During the team’s group coding of the first six visits recordings made for this study, the team decided to begin measuring camcorder awareness behaviors that could be directly observed. A series of potential coding categories and associated decision rules were evaluated until the team decided on a system to use for the remainder of the study. Raters recorded instances of these five behaviors that reflected awareness of, or reaction to, the camcorder for all participants: (1) a passing glance at the camera (≤1s), (2) staring into the camera (≥2s), (3) talking about the camera, (4) self-focused behavior such as primping due to awareness of camera, and (5) hiding from the camera. Interrater agreement, calculated as above for the RIAS communication coding, averaged 0.89 (range 0.76–1.00 across the five categories) in comparison with consensus coding results and 0.86 (range 0.78–1.00) in comparison with the mean of all raters’ scores. The category “hiding from the camera” was not coded by any rater in any of the visits used for these calculations.
The following measures were completed by HCPs.
Clinician/Physician Satisfaction Questionnaire. This 20-item scale completed by the HCP just after a clinic visit (Suchman, Roter, Green & Lipkin, 1993) measures the quality of the patient–provider relationship, adequacy of collection of clinical information, efficient use of clinician time, and absence of excessive patient demands. The items are rated on a 5-point Likert scale ranging from 1 “strongly disagree” to 5 “strongly agree.” Higher scores convey more favorable visit satisfaction by the HCP. The total score, with an alpha coefficient of .82 based on this sample’s data, was used for the present analyses. As mentioned above, two items were added to assess the physicians’ perspective of the extent to which the presence of the camcorder affected their own behavior or that of the parent/child compared with their previous visits.
The following measures were completed by parents and youth. Internal consistency (coefficient alpha) was calculated where appropriate for the questionnaires listed below based on data collected in the present study. Only scales with alpha >.70 were used in data analyses.
General Information Form. This form used in our prior studies records the child's age, sex, date of birth, race, ethnicity, country of origin, language spoken at home, parental age and gender, family composition, and each parent’s occupation and highest level of educational attainment. The Hollingshead Four-Factor Index of Social Status, (Hollingshead, unpublished) an index of SES, was calculated for each household.
Caretaker Self-Efficacy Scale. This scale measures parent/caretaker perceived self-efficacy or confidence in asthma care activities (Grus et al., 2001). Parents completed the scale with the word “asthma” replaced with “cystic fibrosis”, “diabetes”, or “weight control” as appropriate for each diagnostic group. Higher scores indicate stronger self-efficacy. The alpha coefficient for this sample was .74. Parents of children with leukemia did not complete this scale because some items may imply unrealistically that they could control certain clinical outcomes.
Treatment Alliance Scale. The Treatment Alliance Scale (TAS; Gavin et al., 1999; Wissow et al., 2010) was completed by parents and youth ≥11 years of age to measure perceived treatment alliance with their physicians. The questionnaire includes three subscales, Goal Alliance, Affective Connection, and Satisfaction, with higher scores indicating more favorable status on each dimension. The alpha coefficient was .92 for youths and .94 for parents in this study.
Press-Ganey Medical Practice Survey. This is a widely used measure of health care satisfaction (Press-Ganey Research and Analytics, 2009). The 11-item “care provider” section was completed by parents after each visit, with higher scores indicative of more satisfaction. As recommended by the publisher, scores were calculated for each visit that consisted of the percentage of items on which the HCP received the highest allowable parental satisfaction rating. Coefficient alpha was .96 for this sample.
Communication Assessment Tool. The Communication Assessment Tool (CAT) is a 15-item questionnaire that was completed by parents and is used to measure communication skills of the physician (Mackoul, Krupat, & Chang, 2007). One item was dropped that pertains to the clinic staff, not the HCP, for 14 items, with higher scores indicative of more satisfaction. The alpha coefficient was .95 for this sample. Consistent with author recommendations, we calculated the percentage of items for each visit on which the HCP received the highest possible satisfaction rating.
Results
Hypotheses 1 and 2 were analyzed using χ2 tests to evaluate the null hypothesis that the distribution of scores of camcorder awareness obtained from HCPs and parents does not differ from a distribution characterized by equal selection of each response option. Oneway ANOVA revealed no significant differences among diagnosis groups in terms of either self-reported or directly observed behavioral effects of camcorder presence for parents, HCPs or children. Consequently, all of the analyses reported below were pooled across diagnosis groups.
Hypothesis 1
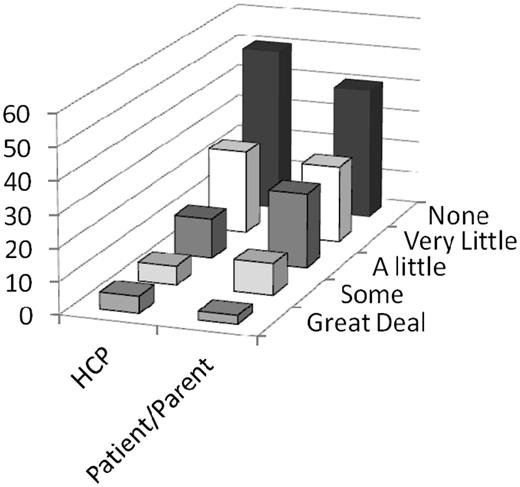
Figure 1 summarizes HCP responses on questionnaire items that measured their perceptions of the extent to which camcorder presence affected their own behavior and that of patients/parents relative to their previous visits with the same HCP. HCPs reported that, in 76.4% of visits, effects on their behavior due to camcorder presence were “none” or “very little” compared with 11% rated as “some” or “a great deal” [χ2 (4) = 74.5; p < .0001]. In 64.5% of visits, HCPs rated the effect on the behavior of patients/parents relative to their clinical encounters before this study as “none” or “very little” compared with 12.3% as “some” or “a great deal” [χ2 (4) = 73.1; p < .0001]. Because HCPs enrolled up to 15 patients each, it was possible to examine changes in how camcorder presence affected their own behavior over time as successive study visits were completed. HCP camcorder awareness scores during the second half of their study participation decreased significantly compared with their scores during the first half of their study participation (t = −2.096; p = .043), indicating lower estimates of camcorder effects on their own behavior.
Health care provider ratings of camcorder effects on their own behavior and that of patients/parents (% responses in each category).
Hypothesis 2
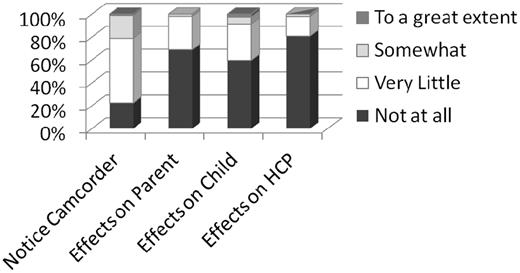
Figure 2 summarizes parents’ responses to four questionnaire items addressing their perceptions of how much they noticed the camcorder and how much its presence affected the behavior of the HCP, child, or themselves compared with clinic visits with the same HCP before this study. For these four questions, parental ratings of the effects of the camcorder that were rated as “very little” or “not at all” were 79% for “notice the camcorder” [χ2 (3) = 94.6; p < .0001], 92% for “effects on child’s behavior” [χ2 (3) = 102.5; p < .0001], and 98% for “effects on parent behavior” [χ2 (3) = 127.2; p < .0001] and “effects on HCP behavior” [χ2 (3) = 158.1; p < .0001].
Hypothesis 3
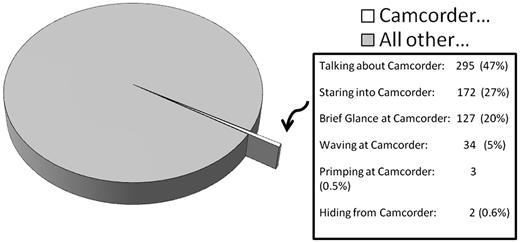
Figure 3 summarizes the results of observational coding of the five categories of camcorder awareness behaviors that were coded. Of the 107,668 total utterances that were coded during the study, only 634 (0.59%) of the events were coded as one of the camcorder awareness behaviors, confirming Hypothesis 3. At least one instance of camcorder awareness was coded in 74% of all study visits, yet the modal number of such events was 0 for children, HCPs, and parents. As a proportion of all coded events for each category of participants, camcorder awareness behaviors were significantly more common [F (2, 151) = 6.47; p < .0001] among children (mean = 3.8% of all of their coded events) than among either HCPs or parents (mean for both = 0.4%). (In many study visits, no camcorder awareness behaviors were coded for children [n = 67; 43.2%], HCPs [n = 83 visits; 53.5%], or parents [n = 101; 65.2%].) Relatively few visits reflected frequent camcorder awareness behaviors, as the occurrence of four or more coded events in a given visit was uncommon among children (n = 31; 20%), HCPs (n = 17; 9.0%), and parents (n = 9; 5.8%). In eight visits (5.3%), ≥10 camcorder awareness behaviors were coded for all participants combined. Camcorder awareness behaviors in youth were most common among the youngest children in the sample and decreased with child age (r = −0.34; p < .0001). Camcorder awareness was coded over six times more often among 5–7 year olds (8.2% of all of their coded events) compared with children over the age of 13 years (1.2% of all of their coded events).
Frequency and proportion of each type of camcorder awareness behavior that was coded. The 634 coded camcorder awareness events constituted 0.59% of the total of 107,668 coded events.
Hypothesis 4
Pearson correlations were calculated to evaluate whether directly observed camcorder awareness behaviors were related significantly to total scores on the RIAS composite scores, Global Affect Rating scale, OPTION scale, Clinician/Physician Satisfaction scale, Caretaker Self-Efficacy scale, Press-Ganey Medical Practice Survey, CAT, TAS, and PVR. Only two RIAS composite scores (of 33 possible) were associated significantly with the frequency of camcorder awareness behavior. These were children’s scores for Giving Medical Information (r = −.20; p = .014) and HCPs’ scores for Negative Communication (r = .16; p = .043). Visits typified by more camera awareness behaviors were associated with less giving of medical information by children and more expressions of negativity by HCPs. Both of these categories of communication were coded very uncommonly during study visits. None of the other measures listed above were associated significantly with the frequencies of observed camera awareness behaviors or with scores on self-reported camera awareness completed by HCPs and by parents. Hypothesis 4 was thus substantially supported in that the great majority of directly observed communication behaviors were not associated significantly with the frequency of directly observed camcorder awareness.
Discussion
All four of the hypotheses evaluated for this article received substantial support and similar conclusions can be reached from the results of two distinct methods of assessing observational reactivity (self-report and direct observation) in this observational study of communication during pediatric health care encounters. Both methods suggest that participants remained aware of the presence of the camcorder, but that this awareness had relatively weak associations with their overt communication behavior or their respective ratings of the quality of the health care encounters. The self-report measures (Figures 1 and 2) showed that both HCPs and parents reported that parents’ behavior was perhaps slightly more affected than that of HCPs, but that both parents and HCPs were relatively unaffected by this recognition. For HCP reports, the degree of behavioral change attributed to camcorder presence peaked at “none” for parents and HCPs, and the proportion of responses of “a great deal” or “some” represented a small minority of all responses. For parent report, behavioral effects of camcorder presence were rated as “very little” or “not at all” by 98% of parents for effects on both HCP and parent behavior and ∼92% for effects on children’s behavior.
Many of the above self-report findings were substantiated by the results of independent observational coding of camcorder awareness behaviors among patients, parents, and HCPs. First, camcorder awareness behaviors occurred in a majority of visits (74%), yet Figure 3 shows that the relative frequency of those events was low, (634 events of 107,668 coded events; 0.59%) affirming the self-report findings showing that both HCPs and parents reported that presence of the camcorder appeared to have weak effects on participants’ behaviors. A substantial percentage of participants demonstrated none of these behaviors and the frequencies of these behaviors were low when they did occur. Talking about the camcorder, brief glances at the camcorder, and staring into the camcorder accounted for 94% of all of the coded camcorder awareness behaviors. Second, aligned with parent reports that their children’s behavior was more strongly affected by camcorder presence than that of parents’ or HCPs’, camcorder awareness behaviors accounted for 3.8% of all coded child behaviors and only 0.4% of all coded parent and HCP behaviors. These behaviors were most common among younger children and were progressively less common as child age increased. Although it is possible that the coding scheme constructed for this study did not capture all of the relevant behaviors, the low observed frequencies of these behaviors suggest that any omissions would have negligible effects on the present results or conclusions.
The general conclusion that observational reactivity was relatively uncommon and rated overall as a weak influence on the nature of the health care encounters is important in its own right. But perhaps more important is a determination of whether the observational reactivity that was documented exerted differential influences on the quality or quantity of communication during the health care encounters, which was the subject matter of interest in this study. To explore this question, we conducted analyses of the frequency of directly observed camcorder awareness behaviors as correlates of the various measures of communication and visit quality that were collected, including the RIAS summary scores, the Global Affect Rating Scale, OPTION Scale, Clinician/Physician Satisfaction Scale, TAS, Press-Ganey Medical Practice Survey, CAT, and Caretaker Self-Efficacy Scale. Frequency of camcorder awareness behaviors was associated significantly with scores on only two of these measures (children’s RIAS scores for Giving Medical Information and for HCP Negative comments). No other indices of directly observed camcorder awareness and the other measures were significantly associated. We conclude that the modest degree of observational reactivity that was identified in this study had a negligible influence on the subject matter of interest and the quantity and quality of communication among HCPs, parents, and patients.
There are limitations of this study and some resulting constraints on the conclusions that can be reached. Most importantly, the sample of HCPs, youth, and parents who enrolled in the study may not be representative of their respective populations. Those who might be most prone to observational reactivity might have been unwilling to enroll in a study of this type. It is plausible to assume that people who are highly apprehensive about participating in a recorded conversation in this typically private setting might have been more affected by camcorder presence. The relatively low recruitment rate (45% of those eligible and reached by phone) amplifies this concern. Participation in such research must be completely voluntary, and so it may not be possible to address this concern completely. Nonetheless, with the range of camcorder awareness that was measured in this study, there were minimal effects of that awareness on multiple measures of communication and the quality of the care process. A limited portion (∼4%) of camcorder awareness ratings were assessed for interrater reliability, which is a limitation. Few were assessed because of acceptable rater agreement and the burden associated with multiple rater coding. Another limitation is that the measures of communication and of visit quality/satisfaction may not be sensitive to affective elements of observational reactivity. Study participants may have been reluctant to express themselves fully about sensitive or private issues during the recorded visits. Adults, in particular, may be more likely to regulate their behavior in response to camcorder presence than are children. Because many of the measures were based on observational coding, private thoughts, or feelings that are not expressed are not detectable by such methods. The rated influence of camcorder awareness by HCP and parent reports suggest that such effects were both uncommon and of modest importance, but it remains possible that the measures that we collected were simply insensitive to individual differences in how camcorder presence affected the participants’ private reactions to these procedures.
The findings reported here are from the baseline visits of a longitudinal investigation in which each child/parent has agreed to participate in the study over three successive routine clinic visits at ∼3–6-months intervals between visits. Once all data collection for the study is complete, it will be possible to perform additional analyses of changes in observational reactivity over time among this sample of participants.
Alternative designs could be considered for future similar studies such as randomizing participants to clinic visits that are or are not recorded, or comparing clinic visits that incorporate either actual or simulated recording of the health care encounters. Although such designs may have certain advantages over the observational design strategy used here, either of these approaches may introduce new problems related to specification and measurement of the mechanisms and outcomes of interest.
The above limitations do not change the fact that the methods used in this study to detect observational reactivity and to evaluate its influence on communication during pediatric subspecialty care encounters suggest strongly and consistently that these intrusions into a typically private and sensitive social interaction do not appear to appreciably change the nature of those interactions. These findings support the use of direct observation methods in studies of the relationships between characteristics of pediatric health care encounters and a wide variety of objective and subjective outcomes of the care process. Additional reports from this ongoing study will be forthcoming.
Acknowledgments
We thank all 16 colleagues who helped plan the study, the 8 research specialists and coordinators who conducted the study, and all of the children, parents, and HCPs who took part and allowed us to intrude into their clinic visits.
Funding
This work was supported by a Nemours Foundation Research Cluster Grant entitled “Clinician-Parent-Patient Communication in Pediatrics” awarded to the last author.
Conflicts of interest: One of the co-authors is on the editorial board of Journal of Pediatric Psychology.