-
PDF
- Split View
-
Views
-
Cite
Cite
M. Janice Gilliland, Michael Windle, Jo Anne Grunbaum, Antronette Yancey, Deanna Hoelscher, Susan R. Tortolero, Mark A. Schuster, Body Image and Children’s Mental Health Related Behaviors: Results from the Healthy Passages Study, Journal of Pediatric Psychology, Volume 32, Issue 1, January/February 2007, Pages 30–41, https://doi.org/10.1093/jpepsy/jsl008
Close - Share Icon Share
Abstract
Objective This study examined the relationship between body image discrepancy (BID) scores for actual versus ideal body image for children and indicators of child mental health. Methods Data were collected from 650 5th graders and their parents who participated in the Healthy Passages Phase I study. Participants were recruited through schools in Alabama, California, and Texas. Measures included the Collins Body Image to produce child- and parent-reported child BID scores, respectively, body mass index (BMI) for child and parent, the Strengths and Difficulties Questionnaire (SDQ), and the Positive and Negative Affect Scale for Children (PANAS-C). Results After controlling for potential confounders, children’s internalizing problems as rated by parents and negative affect as rated by children were significantly associated with discrepancies based on child- and parent-reported child BID scores, respectively. Conclusions Overall, higher child- and parent-reported child BID scores were significantly associated with more internalizing problems and negative affect among children. There were some inconsistencies in the associations between other mental health behaviors and child BID scores contingent on parent or child ratings. Early intervention may be indicated to prevent possible adverse consequences, especially for internalizing problems, from the effects of child- and parent-reported child BID scores on adolescent and adult mental health and well-being.
Research during the last two decades has demonstrated variability in body size preference and in body image dissatisfaction among children and adolescents based on age, pubertal status, gender, ethnicity, body mass index (BMI) or weight, and family relationships. Adolescents report greater body image dissatisfaction than younger children (Cohn et al., 1987; Kostanski, Fisher, & Gullone, 2004). In addition, dissatisfaction with one’s body image and the desire for thinness increases as youth approach puberty (Gardner, Sorter, & Friedman, 1997). Girls report greater dissatisfaction than boys (Hausenblas, Downs, Fleming, & Connaughton, 2002; Siegel, Yancey, Aneshensel, & Schuler, 1999) and a greater desire for thinness (Cohn et al., 1987; Collins, 1991; Kostanski & Gullone, 1998). Youth who are African American report greater body image satisfaction and prefer larger body sizes than other groups (Altabe, 1998; Gluck & Geliebter, 2002; Parnell et al., 1996; Siegel et al., 1999; Thompson, Corwin, & Sargent, 1997). Both BMI (which incorporates both weight and height) and at risk for overweight or overweight (as indicated by a high BMI) have positive associations with body image dissatisfaction among youth according to some studies (Gardner et al., 1997; Kostanski et al., 2004; Presnell, Bearman, & Stice, 2004). Among boys, underweight also has been associated with body image dissatisfaction (Kostanski et al., 2004), although boys appear primarily to desire greater muscularity, not just increased weight (Smolak, 2004).
Positive family relationships have been associated with body image satisfaction among children and adolescents (Archibald, Graber, & Brooks-Gunn, 1999; Byely, Archibald, Graber, & Brooks-Gunn, 2000). Studies suggest that children can detect a negative evaluation of their body size by parents, which can have serious long-term effects (Davison & Birch, 2001). In a study by Schwartz and colleagues (Schwartz, Phares, Tantleff-Dunn, & Thompson, 1999), negative parental feedback regarding appearance during childhood predicted poorer psychological functioning among college undergraduates, as measured by the Brief Symptom Inventory (BSI).
Studies of weight, body image dissatisfaction, and psychosocial problems among children have had inconsistent findings. Some studies have supported associations between higher BMI or body image dissatisfaction and internalizing problems such as depression, anxiety, hopelessness, and low self-esteem (Erermis et al., 2004; Falkner et al., 2001; Kostanski & Gullone, 1998; Siegel et al., 1999). Other studies have reported that the association between children’s BMI or body image dissatisfaction and mental health varied, by gender (Pierce & Wardle, 1993) and ethnicity (Strauss, 2000). Some studies, however, have found no or very weak associations between body size and measures of self-esteem among children (Kaplan & Wadden, 1986; Klesges et al., 1992).
Despite the large literature on body image and at risk for overweight or overweight among children and their possible association with mental health and problem behaviors, previous studies in this area have often been constrained by three methodological issues. First, the parent, a central agent in the child’s development, often has been omitted as an influential factor in these relationships. Second, much of the literature relies exclusively on children’s reports of their body image or their internalizing problems and does not take into account the moderating or mediating effect of parental appraisal of the child’s size. Finally, many studies have used self-reported rather than measured height and weight. This article expands the literature by proposing two research questions: (a) What is the association between the child’s prosocial behaviors, internalizing and externalizing problems, and positive and negative affect and the discrepancy between the child’s self-perceived body size and the size she/he believes a child that age should look like [child body image discrepancy (BID) score]? and (b) What is the association between the same set of factors for the child and the discrepancy between the parent’s assessment of the child’s actual body size and of the body size that is best for their child (the parent-reported child BID score)? Two hypotheses were tested. First, it was hypothesized that children who report greater BID scores would have lower (less desirable) scores on positive measures of mental health (prosocial behavior and positive affect) and higher (less desirable) scores on negative measures (internalizing and externalizing problems and negative affect). Second, it was hypothesized that similar to child results, greater parent-reported child BID scores would be associated with lower child scores on the positive measures of mental health and with higher child scores on measures of negative behaviors. Results from this study will add to our understanding of how the child’s and parent’s perception of the child’s body size is related to behaviors associated with children’s mental health.
Methods
Overview
Data used for this report were collected from the phase I cross-sectional study of Healthy Passages. Data were collected on 650 5th-grade children and one of their parents, from May to September 2003 at three research sites: the University of Alabama at Birmingham; the University of California at Los Angeles/RAND; and the University of Texas, Houston. Healthy Passages was funded by the Centers for Disease Control and Prevention (CDC). Institutional Review Boards at the research sites and the CDC approved the study and all study recruitment, consent, and measurement materials. See Windle et al. (2004) for a full description of the study.
Sample
The sample frame included all 5th-grade students in three geographic areas, who were enrolled in public schools with 5th-grade class enrollments of at least 25 students. The three geographic areas included: (a) 10 contiguous public school districts in and around Birmingham, Alabama; (b) 25 contiguous public school districts in Los Angeles County, California; and (c) the largest public school district in Houston, Texas. Schools were selected using a two-stage probability sampling procedure. Schools were first randomly selected with a school’s probability of selection proportionate to a weighted measure of its size. Once selected, all 5th-grade students in regular classrooms in sampled schools were invited to participate.
Design weights were constructed to reflect different school selection probabilities based on racial/ethnic composition. Non-response weights were constructed to model non-response as a function of school, student gender, and student race/ethnicity. These two sets of weights were combined into a final probability of response weight variable that represented the population of 5th-grade students in the public schools in each site’s geographic area.
The selected schools (N = 21) yielded a potential pool of 1,848 5th-grade students. A total of 1,059 (56%) students and their primary caregivers gave written permission to be contacted about the study. Of these, 871 cases (82%) were fully pursued (others were not pursued in phase I of Healthy Passages because of limited time frame rather than other systematic characteristics), thus definitive response rates for the home interview component cannot be calculated. Among those cases that were pursued fully, the interview completion rate was 78% (n = 650). Incomplete anthropometric data reduced the sample size to 635 children (636 parents) for these analyses.
Procedures
Fifth-grade students and one of their parents were recruited through school classrooms. (A primary caregiver other than a parent responded in 5% of homes; for this article, ‘‘parent’’ is used to refer to all adult respondents.) Study materials, including a form requesting permission to contact parents, were sent home with students. Parents who gave their consent to be contacted were called to schedule a visit at home or other preferred location. At the interview, the parent provided signed informed consents for him/herself and their child, and the child gave signed assent. Interview and anthropometric data were collected by trained field staff. The parent and child interviews consisted of a computer-assisted personal interview (CAPI) and an audio-computer-assisted self-interview (A-CASI). Parents and children completed their interviews separately in private spaces. English and Spanish versions of all instruments were available and used as needed. On average, the home visit took about 3 hrs and included consent, anthropometrics, and CAPI and A-CASI interviews with the parent and child. Parents were paid US $50 and children were given a store gift card worth $20 for completing the interview.
Measures
Body Image
The Collins Body Image measure was used to assess parent and child perception of the child’s body size (Collins, 1991). The measure has seven sex-specific images for children, ranging from very thin to very heavy. Children and parents were provided with a card showing sex-specific images. Each child selected the image that reflected what a child his/her age should look like (ideal self) and the image that looked most like him/herself. Parents selected the image that most closely resembled their child’s current size and the image they thought would be best for their child (ideal child). Collins (1991), reported test–retest reliability coefficients of .71 for child selection of self-image and .59 for child selection of ideal self. The validity coefficient for comparison of child selection of self-image with the child’s BMI was .36 (Collins, 1991).
BMI
Parents’ and children’s weight and standing height were measured with standard anthropometric protocols (Armstrong & Welsman, 1997; Lohman, Roche, & Martorell, 1991; National Institutes of Health, 1998). Weight was measured to the nearest 0.1 kg using a Tanita electronic digital scale (BWB-800S). Height was measured to the nearest millimeter using a portable stadiometer (PE-AIM-101). Two independent measurements were taken for weight and height; if the measurements differed by 0.2 kg or more for weight or 0.5 cm or more for height, a third measurement was taken. The two weights or heights closest in agreement were averaged, and averages were used to calculate BMI [weight/height (kg/m)2]. BMI percentiles were calculated for children using the CDC gender- and age-specific charts (Kuczmarski et al., 2002).
Prosocial Behaviors and Internalizing and Externalizing Problems
The Strengths and Difficulties Questionnaire (SDQ) (Goodman, 1997) was used to collect information from the parents on psychological adjustments and emotional and behavioral problems of their child. The SDQ is a 25‐item scale that assesses children’s behaviors across five domains of psychological adjustment: hyperactivity, emotional problems, prosocial behaviors, conduct problems, and peer problems. Dickey and Blumberg (2004) analyzed data from the SDQ using principal components analysis and factor analysis and identified three factors, prosocial behaviors and internalizing and externalizing problems, that best accounted for the variability in observed responses. Alpha levels for these three dimensions were .76, .78, and .70, respectively. Although Dickey and Blumberg (2004) reverse-coded questions measuring prosocial behaviors to have higher scores indicating more problem behaviors, these variables were not reverse coded for this article. Thus, higher scores on prosocial behaviors indicate more positive behaviors.
Positive and Negative Affect
The Positive and Negative Affect Scale for Children (PANAS-C) (Laurent et al., 1999) was used to collect data on internalizing problems. The two subscales (positive and negative affect) in this instrument are associated with other measures of internalizing problems (e.g., depression and anxiety). The PANAS-C is a 30-item scale that measures children’s feelings and emotions during the previous month. Higher scores on positive affect indicate more positive feelings, and higher scores on negative affect indicate more negative feelings.
Statistical Analysis
The complex sample design and probability weights were accounted for in the statistical analyses using the SURVEYREG procedure in the Statistical Analysis System (SAS, version 9.1). Means and frequencies were computed for continuous and categorical variables. Analysis of covariance (ANCOVA) was used to examine relationships between the dependent variables of children’s behaviors and problems and the independent variables of child- and parent-reported BID score while controlling for parent and child BMI, ethnicity, and child gender. Limitations inherent in the SAS SURVEYREG required that unweighted data be used to calculate effect sizes and correlations. Probability weights were small, thus results obtained using unweighted data should closely approximate with those from weighted data.
Child BID scores for the primary analyses were computed as the absolute difference (Jacobi & Cash, 1994) between the score for the image children selected as looking most like themselves and the score for the image they should look like (range from 1 to 7 for both). The parent-reported child BID scores were calculated in a similar fashion using the parents’ selections of two images for their children (current size and ideal child). Thus, the range of possible BID scores for both children and parents was 0 to 6. Actual BID scores ranged from 0 to 5 for children and 0 to 3 for parents. Because there were so few BID scores of 3, 4, or 5 for children and of 3 for parents, those scores were combined with BID scores of two (the analytic categories became 0, 1, and ≥2). Post hoc comparisons were conducted between the referent group and each of the other scores (0–1, 0–2, and 1–2). Analyses were also conducted using the negative and positive values for the child BID score (≥–2, –1, 0, +1, and ≥+2) to examine the directionality of the outcomes.
Parent BMIs were grouped into three categories: <25 = normal weight, 25–<30 = overweight, and ≥30 = obese (National Institutes of Health, 1998). Children’s BMIs were categorized by gender- and age-specific percentiles into groups based on the CDC’s four categories for child BMI: <5th percentile = underweight, 5–<85th percentile = normal weight, 85–<95th percentile = at risk for becoming overweight, and ≥95th percentile = overweight. The CDC percentiles were used in all analyses of BMI.
Results
The average age of the children in the sample was 10.8 years and that of parents was 38.9 years. Ninety percent of the parents were female. Forty-three percent of children were Hispanic, 28.2% were non-Hispanic Black, 24.1% were non-Hispanic White, and 4.6% were of other race/ethnicities. Over half of the parents had at least some college education, but almost half had annual incomes of less than $25,000 per year (data not shown). Mean BMI for children and parents was 21.5 and 29.9, respectively. The mean child BMI is above the 85th percentile (at risk for overweight) for children (Kuczmarski et al., 2002), and the adult mean BMI approaches the cut-point for obesity among adults (BMI ≥30).
Correlation analysis of means (unweighted data) revealed statistically significant correlations between parent and child BMI (r = .34, p < .001) and between child- and parent-reported child BID scores (r = .27, p < .001). Both child- and parent-reported child BID scores were associated significantly with child BMI (r = .27 and r = .47, respectively, p < .001 for both). No statistically significant correlation was found between child BID and prosocial behavior, and child BMI was not significantly correlated with prosocial, internalizing or externalizing behaviors. Low-to-moderate correlations were found for all other variables (data not shown). Separate correlation analyses (data not shown) were run for mother and father caregivers to examine gender differences in parental reports of child BID scores and child and parent BMI. Child BID scores were significantly associated with mother’s BMI (r = .25, p < .001) but not for father’s BMI (r = .23, p < .08). The magnitude of the correlations was similar, measure and the differences in significance results from insufficient power. [The effect of parent and child BMI category on children’s behaviors was examined (data not shown), controlling for BID category, gender, and race/ethnicity. The model indicated significant overall group differences by child BMI for externalizing problems only. Analysis by parent BMI category indicated significant overall group differences in the model for prosocial behaviors and internalizing problems. Post hoc subgroup analysis indicated that overweight children differed significantly from low and normal weight children for externalizing problems, with overweight children reporting significantly lower (more desirable) mean scores for these behaviors. In contrast, post hoc subgroup comparisons indicate that normal weight parents rated their children significantly higher on prosocial behaviors compared with obese parents. Normal weight parents rated their children significantly lower on internalizing problems than did overweight parents, and obese parents rated their children significantly higher on internalizing problem compared to overweight parents.]
The primary analyses were conducted using the absolute values for child- and parent-reported child BID scores. Secondary analyses were conducted to determine whether the directionality of the discrepancy affected the results found (data not shown). The models were run with all five possible categories of discrepancy included (≥–2, –1, 0, +1, and ≥+2). These results were similar to results using the absolute value of the child BID score, and indicated that both negative and positive child- and parent-reported child BID scores were significantly associated with the mental health variables, primarily at the extreme negative or positive child BID scores (≥–2 or ≥+2) compared with no discrepancy. The focus of this study is on whether a discrepancy between children’s perceived ideal and perceived self or between parents’ perceived ideal child and own child was associated with child mental health outcomes, regardless of the directionality of the discrepancy. Therefore, only the absolute value results are reported in detail here.
The weighted means for prosocial behaviors, internalizing and externalizing problems, and negative and positive affect by child BID score are summarized in Table I. The results provide some support for the hypothesis that a higher self-assessed child BID score would be associated with poorer scores on the mental health outcomes; however, the results were not consistent across all outcome variables. For all five variables, there was a statistically significant difference by child BID score. Children with a BID score of 0 had the most desirable scores for prosocial behaviors (i.e., highest score), internalizing problems, externalizing problems, and negative affect (i.e., lowest scores). Children in this group had the second most desirable scores for positive affect. Unexpectedly, children with a BID score of ≥2 had the highest (most desirable) mean score for positive affect, and the second highest (most desirable) score for prosocial behaviors, which was contrary to the hypothesized direction. Although statistically significant (p < .001), the actual differences in scores for prosocial behaviors were small and were limited to overall group differences; no statistically significant differences were found in the post hoc analyses of pairwise comparisons. Children with a BID score of ≥2 had the highest (least desirable) score for internalizing problems and negative affect. Children with a BID score of 1 had the highest (least desirable) mean score for externalizing problems. Post hoc comparisons of differences between groups demonstrated statistically significant differences by BID category for some measures. Children with a BID score of 1 had the highest mean score for externalizing behaviors, and the difference was statistically significant for the category of child BID score = 0, which was inconsistent with the hypothesized relationship. Children with a BID score of ≥2 differed significantly from those with BID scores of 0 or 1 for negative affect. In addition, for positive affect, children with a BID score of 1 differed significantly from those with a BID score of ≥2. There were no statistically significant subgroup differences among children for prosocial behaviors or internalizing problems. Overall, larger child-reported BID was associated with poorer scores on negative outcomes (with the exception of a higher mean for BID score 1 versus BID score ≥2 for externalizing problems), but the results were mixed in regard to more positive outcomes.
Child Behavior and Problem Means, by Child BID Scorea
| . | BID score . | . | . | ||
|---|---|---|---|---|---|
| . | . | . | . | ||
| . | 0 (N = 309) . | 1 (N = 282) . | ≥2 (N = 44) . | F-Statistic . | Post hoc test . |
| Child behavior and problem |  |  |  | ||
| Prosocial behaviorb | 20.25 | 20.08 | 20.20 | 2.66* | |
| Internalizing problemb | 11.26 | 11.43 | 11.93 | 2.51* | |
| Externalizing problemb | 13.35 | 14.20 | 13.56 | 5.71** | 0:1 |
| Negative affectc | 29.67 | 30.93 | 36.35 | 4.00** | 0:2, 1:2 |
| Positive affectc | 52.16 | 49.10 | 54.12 | 3.07** | 1:2 |
| . | BID score . | . | . | ||
|---|---|---|---|---|---|
| . | . | . | . | ||
| . | 0 (N = 309) . | 1 (N = 282) . | ≥2 (N = 44) . | F-Statistic . | Post hoc test . |
| Child behavior and problem |  |  |  | ||
| Prosocial behaviorb | 20.25 | 20.08 | 20.20 | 2.66* | |
| Internalizing problemb | 11.26 | 11.43 | 11.93 | 2.51* | |
| Externalizing problemb | 13.35 | 14.20 | 13.56 | 5.71** | 0:1 |
| Negative affectc | 29.67 | 30.93 | 36.35 | 4.00** | 0:2, 1:2 |
| Positive affectc | 52.16 | 49.10 | 54.12 | 3.07** | 1:2 |
BID, body image discrepancy.
Weighted sample adjusted for parent and child BMI, child ethnicity and child gender.
Assessed by parental report.
Assessed by child report.
*p ≤ .01. **p ≤ .001.
Child Behavior and Problem Means, by Child BID Scorea
| . | BID score . | . | . | ||
|---|---|---|---|---|---|
| . | . | . | . | ||
| . | 0 (N = 309) . | 1 (N = 282) . | ≥2 (N = 44) . | F-Statistic . | Post hoc test . |
| Child behavior and problem |  |  |  | ||
| Prosocial behaviorb | 20.25 | 20.08 | 20.20 | 2.66* | |
| Internalizing problemb | 11.26 | 11.43 | 11.93 | 2.51* | |
| Externalizing problemb | 13.35 | 14.20 | 13.56 | 5.71** | 0:1 |
| Negative affectc | 29.67 | 30.93 | 36.35 | 4.00** | 0:2, 1:2 |
| Positive affectc | 52.16 | 49.10 | 54.12 | 3.07** | 1:2 |
| . | BID score . | . | . | ||
|---|---|---|---|---|---|
| . | . | . | . | ||
| . | 0 (N = 309) . | 1 (N = 282) . | ≥2 (N = 44) . | F-Statistic . | Post hoc test . |
| Child behavior and problem |  |  |  | ||
| Prosocial behaviorb | 20.25 | 20.08 | 20.20 | 2.66* | |
| Internalizing problemb | 11.26 | 11.43 | 11.93 | 2.51* | |
| Externalizing problemb | 13.35 | 14.20 | 13.56 | 5.71** | 0:1 |
| Negative affectc | 29.67 | 30.93 | 36.35 | 4.00** | 0:2, 1:2 |
| Positive affectc | 52.16 | 49.10 | 54.12 | 3.07** | 1:2 |
BID, body image discrepancy.
Weighted sample adjusted for parent and child BMI, child ethnicity and child gender.
Assessed by parental report.
Assessed by child report.
*p ≤ .01. **p ≤ .001.
Table II summarizes the weighted means for child prosocial behaviors, internalizing and externalizing problems, and negative and positive affect by parent-reported child BID score. Again, there were statistically significant overall group differences by parent-reported child BID score for all variables, and the results overall support the hypotheses that parent-assessed child BID is associated with poorer child mental health outcomes. Children of parents who reported a child BID score of 0 had the most desirable scores for prosocial behaviors (i.e., highest mean score), internalizing problems, externalizing problems, and negative affect (i.e., lowest mean score) compared to children with a parent-reported child BID score of 1 or ≥2. In addition to significant differences across the groups, post hoc analysis indicated significant pairwise differences between child BID scores for BID 0 versus BID scores 1 and ≥2 for prosocial behavior and internalizing and externalizing problems. Parent-reported child BID 1 was statistically different also from BID ≥2 for externalizing behaviors and positive affect. Parent-reported child BID 0 also differed significantly from BID ≥2 for positive affect. Children whose parents reported a child BID score of one had the highest (most desirable) mean score for positive affect, and children with a BID score of 0 had the second highest score. Overall, parents who rated their child as having a BID score of 0 also rated their children as being more prosocial and as having fewer internalizing and externalizing problems. Children whose parents rated them as having no discrepancy (BID 0) had lower self-reported scores for negative affect. Children with parent-reported BID scores of 1 reported the highest (most desirable) scores for positive affect, and children with a parent-reported BID score of 0 had the second highest score, but the differences were not statistically significant. Children with parent-assessed BID scores of ≥2 reported significantly lower mean scores for positive affect and significantly higher mean scores for negative affect. This group also reported the least desirable mean scores for parent-reported prosocial behaviors and positive affect (lowest scores) and for internalizing and externalizing behavior (highest scores). There were no significant pairwise differences by BID score for negative affect.
Child Behavior and Problem Means by Parent’s Report on Child BIDa
| . | Parent BID score . | . | . | ||
|---|---|---|---|---|---|
| . | . | . | . | ||
| . | 0 (N = 312) . | 1 (N = 253) . | ≥2 (N = 71) . | F-Statistic . | Post hoc test . |
| Child behavior and problem |  |  |  | ||
| Prosocial behaviorb | 20.54 | 19.95 | 19.54 | 4.02** | 0:1, 2 |
| Internalizing problemb | 10.88 | 11.57 | 12.52 | 5.18** | 0:1, 2 |
| Externalizing problemb | 13.21 | 13.90 | 15.04 | 7.21** | 0:1, 2; 1:2 |
| Negative affectc | 29.47 | 31.79 | 32.50 | 3.09** | |
| Positive affectc | 51.18 | 52.29 | 46.23 | 2.28* | 0:2; 1:2 |
| . | Parent BID score . | . | . | ||
|---|---|---|---|---|---|
| . | . | . | . | ||
| . | 0 (N = 312) . | 1 (N = 253) . | ≥2 (N = 71) . | F-Statistic . | Post hoc test . |
| Child behavior and problem |  |  |  | ||
| Prosocial behaviorb | 20.54 | 19.95 | 19.54 | 4.02** | 0:1, 2 |
| Internalizing problemb | 10.88 | 11.57 | 12.52 | 5.18** | 0:1, 2 |
| Externalizing problemb | 13.21 | 13.90 | 15.04 | 7.21** | 0:1, 2; 1:2 |
| Negative affectc | 29.47 | 31.79 | 32.50 | 3.09** | |
| Positive affectc | 51.18 | 52.29 | 46.23 | 2.28* | 0:2; 1:2 |
BID, body image discrepancy.
Weighted sample adjusted for parent and child BMI, parent ethnicity and child gender.
Assessed by parental report.
Assessed by child report.
*p ≤ .01. **p ≤ .001.
Child Behavior and Problem Means by Parent’s Report on Child BIDa
| . | Parent BID score . | . | . | ||
|---|---|---|---|---|---|
| . | . | . | . | ||
| . | 0 (N = 312) . | 1 (N = 253) . | ≥2 (N = 71) . | F-Statistic . | Post hoc test . |
| Child behavior and problem |  |  |  | ||
| Prosocial behaviorb | 20.54 | 19.95 | 19.54 | 4.02** | 0:1, 2 |
| Internalizing problemb | 10.88 | 11.57 | 12.52 | 5.18** | 0:1, 2 |
| Externalizing problemb | 13.21 | 13.90 | 15.04 | 7.21** | 0:1, 2; 1:2 |
| Negative affectc | 29.47 | 31.79 | 32.50 | 3.09** | |
| Positive affectc | 51.18 | 52.29 | 46.23 | 2.28* | 0:2; 1:2 |
| . | Parent BID score . | . | . | ||
|---|---|---|---|---|---|
| . | . | . | . | ||
| . | 0 (N = 312) . | 1 (N = 253) . | ≥2 (N = 71) . | F-Statistic . | Post hoc test . |
| Child behavior and problem |  |  |  | ||
| Prosocial behaviorb | 20.54 | 19.95 | 19.54 | 4.02** | 0:1, 2 |
| Internalizing problemb | 10.88 | 11.57 | 12.52 | 5.18** | 0:1, 2 |
| Externalizing problemb | 13.21 | 13.90 | 15.04 | 7.21** | 0:1, 2; 1:2 |
| Negative affectc | 29.47 | 31.79 | 32.50 | 3.09** | |
| Positive affectc | 51.18 | 52.29 | 46.23 | 2.28* | 0:2; 1:2 |
BID, body image discrepancy.
Weighted sample adjusted for parent and child BMI, parent ethnicity and child gender.
Assessed by parental report.
Assessed by child report.
*p ≤ .01. **p ≤ .001.
The SDQ and PANAS-C measures used in the study do not have cut-off scores to provide a clinical diagnosis of mental health disorders. Effect sizes were calculated (using unweighted data) to provide information on the magnitude of the differences for pairwise comparisons. Effect sizes for child-reported BID score for the mental health measures ranged from very small (0.004) to moderate (0.27). A similar range was seen for parent-reported measures (0.006–0.28). Among children, the largest effect sizes were between BID 0 and BID 2 for comparisons for internalizing problems and negative affect (0.23 and 0.27, respectively), although similar effect sizes were found for BID 1 versus BID 0, also (0.22 versus 0.21). Among parents, the largest effect sizes were for internalizing and externalizing problems (0.28 and 0.22, respectively) between child BID 0 and BID 1. Effect sizes by mental health measure across BID groups for children and parents were all below 0.20 (effect sizes for child and parent respectively: prosocial 0.04, 0.14; internalizing problems 0.15, 0.16; externalizing problems 0.07, 0.15, negative affect 0.19, 0.11; and positive affect 0.11, 0.09).
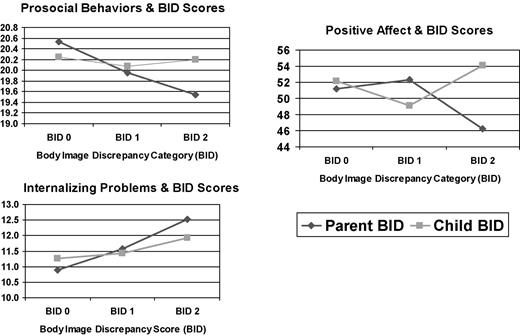
To examine possible statistical interactions between child mental health behaviors and BID scores, a linear model was specified, in which each of the five mental behaviors was predicted by child- and parent-reported child BID scores and a two–way interaction term (child-reported BID score × parent-reported BID score). The model also controlled for child and parent BMI, child ethnicity, and child gender. There were no significant interactions for either externalizing problems or negative affect. However, there were three statistically significant interactions for prosocial behaviors, internalizing problems, and positive affect, and these interactions are displayed in Fig. 1. For parent-rated prosocial behaviors, there were decreases in the ratings of prosocial behaviors as the parent-rated child BID scores increased (i.e., lower ratings of prosocial behavior were associated with greater BID discrepancies). This pattern was not indicated for the child-rated BID scores as few differences were indicated in prosocial behavior ratings across the levels of BID scores. For parent-rated internalizing problems, greater discrepancies in parent-rated child BID scores were linearly related to increases in internalizing problems. For child-rated BID scores, there was also a linear increase in internalizing problems that was associated with greater discrepancies, but the slope was not as steep (with regard to the linear increase) as it was for the parent-rated BID (see Fig. 1). For child-rated positive affect, there was a substantial decrease for parent-rated child BID scores of 2 (i.e., this greater parent-rated BID discrepancy was associated with lower child-rated positive affect). For the child-rated BID score of 2, children rated their positive affect the highest (i.e., a greater child-rated BID discrepancy was associated with higher child-rated positive affect).
Interactions between children’s mental health behaviors and child and parent reported child body image discrepancy (BID) scores.
Discussion
This study used assessment of both children and a parent to explore the associations of child BID scores with characterizations of the children’s behaviors and affect. For all of these variables, statistically significant differences were seen by child BID score assessed by children and parents. Consistent, however, with the extensive literature on low-to-moderate correspondence between mother and child ratings of behaviors (Achenbach, McConaughy, & Howell, 1987), there were some differences in associations with children’s mental health contingent on child BID or parent BID ratings. For example, the highest (≥2) child BID score among children was associated with the highest child rating of positive affect, whereas the highest child BID score among parents was associated with the lowest child rating of positive affect. While these differences related to positive affect were unexpected, it is possible that parent-rated BID discrepancy scores were associated with a more generalized response tendency by parents toward perceiving lower mental health functioning by their children. By contrast, child-rated BID discrepancy scores may reflect a more differentiated view by children in which there is an association with higher negative affect (internalizing problems), but not necessarily a reduction in positive affect. In essence, higher BID discrepancy scores by children at this age may not yet yield associations with lower positive affect, but whether this is a trait-like or an ephemeral phenomenon awaits further study as children grow older.
With one exception, these differences were restricted to the positive behaviors of prosocial behaviors and positive affect. For the exception, children with a BID score of 1 had parent-reported higher mean scores for externalizing behaviors, a pattern not duplicated in the parent-reported child BID results. All other scores of negative behaviors/problems were similar across child and parent BID categories. Parents and children may each be subject to reporting bias, but children may be more reluctant to report poorer functioning on positive self-referencing characteristics, which could bias their classifications (e.g., make them less likely to report lower prosocial functioning or less positive affect). It is possible also that at risk for overweight and overweight children at this age are able to feel more positive about themselves, despite being aware of discrepancies in their ideal versus current body image. However, they may also simultaneously have more negative feelings as indicated by the significant associations between child-rated BID scores and internalizing problems and negative affect. Thus, at risk for overweight and overweight children may experience a wider range of positive and negative affect when self-referencing than normal weight children.
In general, the association between the mean score for parent-reported child BID and the mean score for all five behavioral measures was in the expected direction. A parent BID score of 0, which indicates no discrepancy between what the parent thinks the child’s body is versus what the parent thinks it should be, was associated with significantly higher mean scores for prosocial behavior and positive affect compared with a BID score of ≥2, although the highest score for positive affect unexpectedly was found in the BID score 1 group. It is possible that boys with a BID score of 1 may be larger and stronger (more athletic), and girls with this score may be thinner compared with their same sex peers, and these gender-specific desirable characteristics may result in enhanced positive affect among these children. A parent BID score of ≥2 was associated with significantly higher mean scores for children’s internalizing and externalizing problems. Furthermore, the secondary analysis results indicated that regardless of the directionality, parental discrepancies in body image were associated with less desirable children’s mental health outcomes. Children who did not fit their parents’ ideal body image, whether they were thinner or heavier, were assessed more negatively by themselves and by their parents. Thus, parents who thought their child’s body size was not optimal had children who exhibited more problem behaviors, regardless of whether the children were heavier or thinner than what parents considered ideal for them. This finding is consistent with some other studies that found children’s behavioral and psychosocial outcomes were associated with their parents’ assessments of their size (Pierce & Wardle, 1993; Stanford & McCabe, 2005; Young-Hyman, Schlundt, Herman-Wenderoth, & Bozylinski, 2003).
In some cases, significant differences associated with weight and mental health measures are small and may not be clinically significant (Young-Hyman et al., 2003), although a meta-analysis found moderate effect sizes between heavier weight and self-esteem (Miller & Downey, 1999). Lumeng, Gannon, Cabral, Frank, and Zuckerman, 2003 reported clinically significant associations between behavior problems as measured by the Behavior Problems Index and previous and concurrent overweight among children. Relatively small effect sizes were found in the present study for child mental health behaviors associated with both child- and parent-reported BID; unfortunately, our mental health measures did not permit an evaluation of the clinical significance of these findings.
The mechanism by which parent-rated child BID score affects child behaviors and mental health is complex and multi-faceted, and research on this association has been limited. A partial explanation for the effect may lie in the broader negative evaluation of overweight and obesity in the US culture. In general, overweight people are judged more negatively than those of normal weight (Hebl & Mannix, 2003), and the negative assessment begins at an early age (Collins, 1991; Davison & Birch, 2004). This more general cultural bias against overweight may play a role in the association between parent-rated child BID score and children’s behaviors. The results also indicated, however, that some children and parents rated themselves or their children as too thin, even though few children were categorized as underweight. The negative reactions found against children who were judged to be too thin may result partially from a cultural preference for heavier or more robust body sizes that has been documented among African Americans (Altabe, 1998; Gluck & Geliebter, 2002) and underweight males (Kostanski et al., 2004).
Parents who view their child as having a less-than-ideal body size may engage in more negative interactions with their child and have elevated levels of criticism and other detrimental exchanges, and thus may trigger unhealthy behaviors in their child. Messages may be more subtle, however. Parents who think their children are too thin may encourage them to eat or make other comments that communicate the message to the child that something is wrong with his or her body compared with other children. Although speculative, it may be that minor deviations in BID do not necessarily result in greater negative self-assessment among heavier boys or thinner girls. Boys who are slightly heavier than their self- or parent-assessed ideal size may regard their size as positive if they perceive themselves as stronger, or more athletic, than their peers. For girls, the reaction may be just the opposite in that among white girls at least, thinness is desirable. It may be further speculated that children who are at risk for overweight, overweight, or underweight may experience more teasing and bullying than normal weight children, which may result in more negative affect and internalizing and externalizing behaviors but may also force them to develop better social skills to deal with these situations, and thus may lead to increased prosocial skills and feelings of positive affect.
Studies of discrepancies in the ideal body versus that of self have found differences, but the meaning of the differences is not always clear. Most children and adults consider their body size acceptable or ‘‘good enough’’, even when reporting a discrepancy between self and ideal body size (Rand & Resnick, 2000). Even when children are overweight (i.e., ≥95th percentile), most parents are satisfied with their children’s appearance (Striegel-Moore & Kearney-Cooke, 1994), and either do not perceive that their child is overweight (Etelson, Brand, Patrick, & Shirali, 2003) or do not see their child’s weight as a health problem (Young-Hyman, Herman, Scott, & Schlundt, 2000). Cultural differences in body size preferences (Padgett & Biro, 2003; Parnell et al., 1996) also make interpretation of results difficult. Nevertheless, this study indicates that children may experience distress and unhappiness in situations of body image discrepancies either self or other imposed.
An alternative explanation for our findings is rater bias, that is, parents who are more depressed may be more likely to rate their children as functioning more poorly. We evaluated this possibility by including the parental score from the depression subscale of the Hopkins Behavioral Symptom Checklist (Derogatis, Lipman, Rickels, Uhlenhuth, & Covi, 1974). The inclusion of this measure did not alter the statistical significance levels of either the overall F-statistics or the post hoc comparisons. Therefore, parental rater bias associated with depression does not appear to be an alternative explanation for our findings. Parental BMI was also included as a covariate, and hence is not an alternative explanation for the findings.
The findings of this study underscore the importance of broadening perspectives on psychosocial development in children to include parental assessment of children’s body size and BID scores. It is important in subsequent studies to examine more thoroughly the mechanisms that account for the way in which these factors influence the development of childhood weight concerns and mental health across time. A focus on parent–child relationships and social interactions would be useful to evaluate patterns of conflict expression and resolution and to identify targets of intervention to foster constructive exchanges toward healthier outcomes.
This study has several limitations. The sample is not representative of the US population, and thus the results are not generalizable to that population or to racial/ethnic groups other than African Americans, Hispanics, and non-Hispanic Whites. Although the response rate was not as high as preferred and varied across race/ethnic groups, it was consistent with response rates from other recent school-based studies (Ji, Porkorny, & Jason, 2004). Also, most parents participating in the study were mothers. Future research would benefit from the inclusion of fathers’ perceptions of child BID in relation to children’s mental health. The study was cross-sectional, so causal inferences cannot be made based on the results. Future research should include longitudinal studies to examine the effects of BID on child and adolescent mental health outcomes.
Despite these limitations, the study had several strengths. The sampling algorithm selected a probability sample for each area based on school and student characteristics, and the sample data were weighted based on the probability of selection. Thus, the community-based sample should accurately represent 5th-grade students from the three largest race/ethnic groups in the study catchment areas. The measurement of weight and height of both parent and child was completed by trained field interviewers, which eliminated error from self-reported heights and weights. Finally, the study used interview data from both the parent and the child to assess children’s behavioral problems, affect, and prosocial behaviors, and, with a few exceptions (e.g., positive affect and prosocial behaviors), the data from parents and children revealed generally similar results regarding the associations between body image discrepancies (perceived actual versus ideal) and mental health variables, thereby reinforcing the findings.
The findings have implications for the prevention of mental health problems among children. Attitudes and assessments of important others strongly influence children’s psychosocial and emotional development, and negative assessments of children’s bodies may start a series of events that result in less optimal adult psychosocial functioning. Interventions with parents and children may help to improve the mental health of children who are assessed by themselves or others as having a less-than-ideal body size. The interventions may be most effective if started early in the child’s life and are family-focused or contain a strong parent and school component. Early interventions are important in that negative parental, peer and significant other influences on early child mental health outcomes may have lasting effects on children.
The findings and conclusions in this report are those of the authors and do not necessarily represent the views of the CDC. An earlier version of this article was presented at the 26th annual meeting of the Society of Behavioral Medicine, Boston, Massachusetts, April 2005.
Acknowledgments
Healthy Passages is funded by the Centers for Disease Control and Prevention, Prevention Research Centers through Cooperative Agreement Numbers CCU409679, CCU609653, and CCU915773. The authors thank study participants and other Healthy Passages investigators and staff at each site. Special thanks to Sijian Zhang, MD, MS, for assistance with statistical analysis.