-
PDF
- Split View
-
Views
-
Cite
Cite
Julie N. Germann, Daniel S. Kirschenbaum, Barry H. Rich, Child and Parental Self-Monitoring as Determinants of Success in the Treatment of Morbid Obesity in Low-Income Minority Children, Journal of Pediatric Psychology, Volume 32, Issue 1, January/February 2007, Pages 111–121, https://doi.org/10.1093/jpepsy/jsl007
Close - Share Icon Share
Abstract
Objective To examine self-monitoring by children and parents as related to weight control over 6 months within a long-term multidisciplinary program for low-income minority children with morbid obesity. Methods The weight changes of 228 children with obesity were evaluated according to frequency of child and parental self-monitoring. Predictors of self-monitoring were also evaluated. Results Children who self-monitored on most days lost more weight over 6 months of treatment compared with less-consistent self-monitors. Children whose parents self-monitored were also more likely to self-monitor and lose weight. Conclusions Self-monitoring seems just as critical for successful weight control among low-income minority children with obesity as it is in the middle-class populations. Although lower education and higher levels of psychosocial stress may decrease self-monitoring and participation by these families, they might still benefit from targeting highly consistent self-monitoring (by parents and children) as a primary goal in weight-control programs.
The global epidemic of obesity takes its greatest toll on low-income minority children and adolescents (World Health Organization, 1998). These are the people whose rate of weight problems has accelerated the most in the last decade [23% compared with 13% for Caucasians (Ogden, Flegal, Carroll, & Johnson, 2002)] and who have the greatest risk of developing serious co-morbid conditions, such as diabetes and hypertension, and related psychological sequelae (Young-Hyman, Schlundt, Herman-Wenderoth, & Bozylinski, 2003). Unfortunately, most weight-loss interventions are less successful with minorities than they are with Caucasians (Kumanyika, 2002). This makes it especially urgent to evaluate comprehensive approaches to treat obesity in this very high-risk (and virtually unstudied) population.
In studies involving almost exclusively middle- and upper-class Caucasian participants in university clinics, consistency of self-monitoring (systematic observation and recording of target behaviors) has frequently correlated with weight loss (Flanery & Kirschenbaum, 1986; Salaens & McGrath, 2003). Consistency of self-monitoring early in the treatment also predicted weight loss many months later (Baker & Kirschenbaum, 1993; Wadden et al., 1997). Two studies have also shown that increasing consistency of self-monitoring of eating and exercising behaviors can actually cause significant improvements in weight control (Boutelle, Kirschenbaum, Baker, & Mitchell, 1999; Sperduto, Thompson, & O’Brien, 1986). These and the related findings have led researchers to view self-monitoring as the “cornerstone” (Wadden, 1993) and the most effective technique used to help people lose weight and keep it off (Perri, Nezu, & Viegener, 1993).
There are reasons to believe that self-monitoring may not be the cornerstone to effective weight control for low-income minority children who are morbidly obese. This is a population that chronically experiences far more stress, instability in the home, poor nutritional habits, and greater acceptance of obesity (Anderson, Winett, & Wojcik, 2000). Schmeichel and Baumeister (2004) have shown that “strength of self-regulation” can weaken when weight controllers are subjected to stressors. In other words, financial and familial crises could overtax normal self-regulatory processes. If this happens within a treatment program for morbid obesity among low-income minority children (the present context), consistency of self-monitoring may not emerge as a significant correlate or predictor of success. On the contrary, perhaps consistency of self-monitoring is so critical to the development of effective weight control that, even within a high-stress environment, consistency of self-monitoring may emerge as a significant correlate of success, as it has in the middle- and upper-class Caucasian populations.
Another factor that generally improves weight-loss outcomes when treating obesity in children is parental involvement (Epstein, Valoski, Wing, & McCurley, 1990; Golan & Crow, 2004). High levels of parental involvement should produce more favorable outcomes with low-income minority groups as it has with the Caucasian middle-class populations. One potentially highly relevant form of parental involvement pertains to self-monitoring. If parents can self-monitor their own eating and exercising behaviors, thereby modeling the appropriate “healthy obsession” (Kirschenbaum, 1987, 2000) for their children, the children involved in such a program may be more likely to self-monitor and succeed. Accordingly, parents in the present treatment program were asked to commit to self-monitor their own eating and exercising behaviors, and better outcomes were expected for children whose parents fulfilled this commitment.
This study provided continuation of an initial study (Kirschenbaum, Germann, & Rich, 2005) evaluating the role of self-monitoring in a population of low-income minority children with morbid obesity and their parents. The initial study provided evidence that child and parental self-monitoring during early treatment (the first 3 months) was as important for initial weight-loss success in this population as it has been in populations from higher socioeconomic communities. The purpose of this study was to replicate and extend those findings by evaluating the impact of child and parental self-monitoring among low-income minority families during a longer treatment period (3–6 months). We expected that children who self-monitored relatively consistently and who had parents who self-monitored more consistently would be more likely to lose weight throughout the 6 months of treatment.
Methods
Participants
This study utilized retrospective chart review of 342 program participants. Participants were children and adolescents who were obese and at least one of their parents/caregivers, most often the mother. These were volunteer families who had enrolled in a long-term (target = 1 year or more) cognitive behavioral and multidisciplinary program for the treatment of obesity, primarily morbid obesity. Of the 342 study families, 56 (16.3%) dropped out after the initial assessment. An additional 58 families (16.9%) dropped out before completing 1 month of treatment. These early dropouts could not provide sufficient self-monitoring data for analyses; consequently, only those families who completed the specified treatment interval were used for the respective analyses (frequency of self-monitoring, effects on weight loss, and discriminant function analyses at 1 month, 3 months, and 6 months). Attrition was evident over time, as only 228 of the overall 342 families (67%) completed at least 1 full month of treatment, 160 (47%) completed at least 3 months of treatment, and only 101 (30%) completed at least 6 months of treatment.
Because of significant nonlinear variations in body mass index (kg/m2, BMI) throughout childhood, BMI z-scores were computed from the child’s BMI at assessment and national BMI norms according to gender, ethnicity, and age (Rosner, Prineas, Loggie, & Daniels, 1998). Of those who completed at least 1 month of treatment (228), the mean child weight at assessment was 261.93 pounds (SD = 80.65), mean child height was 63.49 inches (SD = 4.03), the mean child BMI at assessment was 45.1 (SD = 12.2, above the 97th percentile), mean BMI z-score was 6.1 (SD = 3.0); mean age was 13.2 (SD = 2.2); 55% were female; 88.3% were African-American, 8.1% were Hispanic, 3.6% were Non-Hispanic white; and 63% received public assistance. The mean BMI of maternal caregivers at assessment was 35.0 (SD = 8.9), and mean age of the maternal caregivers was 47.8 (SD = 9.4). Maternal caregivers consisted of 77% biological mothers, 5% grandmothers, 2% adoptive mothers, 2% aunts, 2% sisters, 1% foster mothers, .5% cousins, and 11% unknown. Demographic data were only available for 13 paternal caregivers (12 biological fathers and 1 stepfather): The mean BMI of paternal caregivers at assessment was 31.7 (SD = 4.2), and the mean age of the paternal caregivers was 42.1 (SD = 9.2).
Measures
A thorough initial psychological assessment was conducted with each family and focused on hypothesized correlates of success. Specifically, intellectual, behavioral, emotional, and family functioning were assessed. Information on demographic variables was also collected. Height and weight measures were collected at initial assessment, as well as at weekly group therapy sessions. Program process measures were also documented at weekly group therapy sessions. Table I summarizes the baseline measures of child subsets who completed at least 3 and 6 months of treatment.
Potential Predictors (Baseline Demographics and Measures) of Families Completing Treatment Interval
| Potential predictors [M (SD)] (unless otherwise indicated) . | 3 months (n = 160) . | 6 months (n = 101) . |
|---|---|---|
| Demographic factors | ||
| Gender (%) | ||
| Female | 55.6 | 58 |
| Ethnicity (%) | ||
| African-American | 90 | 92 |
| Hispanic | 7 | 4 |
| Non-Hispanic White | 3 | 4 |
| Medicaid dependent (%) | 58 | 57.4 |
| Hollingshead SES | 38.58 (14.6) | 38.97 (14.4) |
| Age in years | 13.33 (2.1) | 13.26 (2.1) |
| Maternal age in years | 41.71 (9.0) | 40.70(8.2) |
| Weight measures | ||
| Child body mass index (BMI) (kg/m2) | 45.76 (12.4) | 46.64 (13.2) |
| Child BMI z-score | 6.16 (3.0) | 6.40 (3.2) |
| Child BMI percentile | >97th | >97th |
| Maternal BMI | 34.68 (9.1) | 34.76 (9.5) |
| Psychological measures | ||
| Intellectual functioning (K-BIT standard score) | 91.74 (14.6) | 90.10 (14.8) |
| Child Behavior Checklist (T-scores)—mother ratings | ||
| Somatic | 68.79 (10.6) | 70.00 (10.8) |
| Anxious/depressive | 59.44 (9.3) | 59.84 (10.0) |
| Aggressive | 59.95 (8.7) | 60.77 (9.3) |
| Youth Self-Report (T-scores)—child ratings | ||
| Somatic | 57.73 (5.1) | 57.88 (5.2) |
| Depressive | 55.46 (2.4) | 55.39 (2.5) |
| Aggressive | 58.66 (7.0) | 58.98 (7.2) |
| Conflict Behavior Questionnaire (percentile) | ||
| Child rating mother | 61.71 (26.3) | 62.37 (26.6) |
| Mother rating child | 70.20 (28.1) | 70.18 (28.3) |
| Weight control habits (11 items, 5-point Likert scale) | 29.67 (6.0) | 28.98 (6.3) |
| Current Exercise Survey (self-reported calories in exercise during previous week) | 2774.52 (4153.11) | 2766.97 (4322.89) |
| Eating self-efficacy (25 items, 7-point Likert scale) | 70.13 (34.5) | 71.17 (37.3) |
| Binge-eating scale (9 items, 0–3 points) | 6.38 (4.6) | 6.48 (4.4) |
| Process measures | ||
| Attended orientation session (%) | 42.5 | 47.5 |
| Length of treatment (months in program) | 9.11 (6.7) | 12.2 (6.6) |
| Maternal weekly self-monitoring for treatment interval | .41 (.9) | .40 (.74) |
| Potential predictors [M (SD)] (unless otherwise indicated) . | 3 months (n = 160) . | 6 months (n = 101) . |
|---|---|---|
| Demographic factors | ||
| Gender (%) | ||
| Female | 55.6 | 58 |
| Ethnicity (%) | ||
| African-American | 90 | 92 |
| Hispanic | 7 | 4 |
| Non-Hispanic White | 3 | 4 |
| Medicaid dependent (%) | 58 | 57.4 |
| Hollingshead SES | 38.58 (14.6) | 38.97 (14.4) |
| Age in years | 13.33 (2.1) | 13.26 (2.1) |
| Maternal age in years | 41.71 (9.0) | 40.70(8.2) |
| Weight measures | ||
| Child body mass index (BMI) (kg/m2) | 45.76 (12.4) | 46.64 (13.2) |
| Child BMI z-score | 6.16 (3.0) | 6.40 (3.2) |
| Child BMI percentile | >97th | >97th |
| Maternal BMI | 34.68 (9.1) | 34.76 (9.5) |
| Psychological measures | ||
| Intellectual functioning (K-BIT standard score) | 91.74 (14.6) | 90.10 (14.8) |
| Child Behavior Checklist (T-scores)—mother ratings | ||
| Somatic | 68.79 (10.6) | 70.00 (10.8) |
| Anxious/depressive | 59.44 (9.3) | 59.84 (10.0) |
| Aggressive | 59.95 (8.7) | 60.77 (9.3) |
| Youth Self-Report (T-scores)—child ratings | ||
| Somatic | 57.73 (5.1) | 57.88 (5.2) |
| Depressive | 55.46 (2.4) | 55.39 (2.5) |
| Aggressive | 58.66 (7.0) | 58.98 (7.2) |
| Conflict Behavior Questionnaire (percentile) | ||
| Child rating mother | 61.71 (26.3) | 62.37 (26.6) |
| Mother rating child | 70.20 (28.1) | 70.18 (28.3) |
| Weight control habits (11 items, 5-point Likert scale) | 29.67 (6.0) | 28.98 (6.3) |
| Current Exercise Survey (self-reported calories in exercise during previous week) | 2774.52 (4153.11) | 2766.97 (4322.89) |
| Eating self-efficacy (25 items, 7-point Likert scale) | 70.13 (34.5) | 71.17 (37.3) |
| Binge-eating scale (9 items, 0–3 points) | 6.38 (4.6) | 6.48 (4.4) |
| Process measures | ||
| Attended orientation session (%) | 42.5 | 47.5 |
| Length of treatment (months in program) | 9.11 (6.7) | 12.2 (6.6) |
| Maternal weekly self-monitoring for treatment interval | .41 (.9) | .40 (.74) |
Potential Predictors (Baseline Demographics and Measures) of Families Completing Treatment Interval
| Potential predictors [M (SD)] (unless otherwise indicated) . | 3 months (n = 160) . | 6 months (n = 101) . |
|---|---|---|
| Demographic factors | ||
| Gender (%) | ||
| Female | 55.6 | 58 |
| Ethnicity (%) | ||
| African-American | 90 | 92 |
| Hispanic | 7 | 4 |
| Non-Hispanic White | 3 | 4 |
| Medicaid dependent (%) | 58 | 57.4 |
| Hollingshead SES | 38.58 (14.6) | 38.97 (14.4) |
| Age in years | 13.33 (2.1) | 13.26 (2.1) |
| Maternal age in years | 41.71 (9.0) | 40.70(8.2) |
| Weight measures | ||
| Child body mass index (BMI) (kg/m2) | 45.76 (12.4) | 46.64 (13.2) |
| Child BMI z-score | 6.16 (3.0) | 6.40 (3.2) |
| Child BMI percentile | >97th | >97th |
| Maternal BMI | 34.68 (9.1) | 34.76 (9.5) |
| Psychological measures | ||
| Intellectual functioning (K-BIT standard score) | 91.74 (14.6) | 90.10 (14.8) |
| Child Behavior Checklist (T-scores)—mother ratings | ||
| Somatic | 68.79 (10.6) | 70.00 (10.8) |
| Anxious/depressive | 59.44 (9.3) | 59.84 (10.0) |
| Aggressive | 59.95 (8.7) | 60.77 (9.3) |
| Youth Self-Report (T-scores)—child ratings | ||
| Somatic | 57.73 (5.1) | 57.88 (5.2) |
| Depressive | 55.46 (2.4) | 55.39 (2.5) |
| Aggressive | 58.66 (7.0) | 58.98 (7.2) |
| Conflict Behavior Questionnaire (percentile) | ||
| Child rating mother | 61.71 (26.3) | 62.37 (26.6) |
| Mother rating child | 70.20 (28.1) | 70.18 (28.3) |
| Weight control habits (11 items, 5-point Likert scale) | 29.67 (6.0) | 28.98 (6.3) |
| Current Exercise Survey (self-reported calories in exercise during previous week) | 2774.52 (4153.11) | 2766.97 (4322.89) |
| Eating self-efficacy (25 items, 7-point Likert scale) | 70.13 (34.5) | 71.17 (37.3) |
| Binge-eating scale (9 items, 0–3 points) | 6.38 (4.6) | 6.48 (4.4) |
| Process measures | ||
| Attended orientation session (%) | 42.5 | 47.5 |
| Length of treatment (months in program) | 9.11 (6.7) | 12.2 (6.6) |
| Maternal weekly self-monitoring for treatment interval | .41 (.9) | .40 (.74) |
| Potential predictors [M (SD)] (unless otherwise indicated) . | 3 months (n = 160) . | 6 months (n = 101) . |
|---|---|---|
| Demographic factors | ||
| Gender (%) | ||
| Female | 55.6 | 58 |
| Ethnicity (%) | ||
| African-American | 90 | 92 |
| Hispanic | 7 | 4 |
| Non-Hispanic White | 3 | 4 |
| Medicaid dependent (%) | 58 | 57.4 |
| Hollingshead SES | 38.58 (14.6) | 38.97 (14.4) |
| Age in years | 13.33 (2.1) | 13.26 (2.1) |
| Maternal age in years | 41.71 (9.0) | 40.70(8.2) |
| Weight measures | ||
| Child body mass index (BMI) (kg/m2) | 45.76 (12.4) | 46.64 (13.2) |
| Child BMI z-score | 6.16 (3.0) | 6.40 (3.2) |
| Child BMI percentile | >97th | >97th |
| Maternal BMI | 34.68 (9.1) | 34.76 (9.5) |
| Psychological measures | ||
| Intellectual functioning (K-BIT standard score) | 91.74 (14.6) | 90.10 (14.8) |
| Child Behavior Checklist (T-scores)—mother ratings | ||
| Somatic | 68.79 (10.6) | 70.00 (10.8) |
| Anxious/depressive | 59.44 (9.3) | 59.84 (10.0) |
| Aggressive | 59.95 (8.7) | 60.77 (9.3) |
| Youth Self-Report (T-scores)—child ratings | ||
| Somatic | 57.73 (5.1) | 57.88 (5.2) |
| Depressive | 55.46 (2.4) | 55.39 (2.5) |
| Aggressive | 58.66 (7.0) | 58.98 (7.2) |
| Conflict Behavior Questionnaire (percentile) | ||
| Child rating mother | 61.71 (26.3) | 62.37 (26.6) |
| Mother rating child | 70.20 (28.1) | 70.18 (28.3) |
| Weight control habits (11 items, 5-point Likert scale) | 29.67 (6.0) | 28.98 (6.3) |
| Current Exercise Survey (self-reported calories in exercise during previous week) | 2774.52 (4153.11) | 2766.97 (4322.89) |
| Eating self-efficacy (25 items, 7-point Likert scale) | 70.13 (34.5) | 71.17 (37.3) |
| Binge-eating scale (9 items, 0–3 points) | 6.38 (4.6) | 6.48 (4.4) |
| Process measures | ||
| Attended orientation session (%) | 42.5 | 47.5 |
| Length of treatment (months in program) | 9.11 (6.7) | 12.2 (6.6) |
| Maternal weekly self-monitoring for treatment interval | .41 (.9) | .40 (.74) |
Demographics
Information on demographic variables collected at assessment included gender, ethnicity, socioeconomic status (SES) [measured by public assistance versus private insurance and the Hollingshead Index of SES (Hollingshead, 1982)], age, and initial BMI, as well as parental age and BMI.
Psychological Functioning
Potential mediators of behavior change were assessed during the initial psychological evaluation. These included intellectual functioning [Kaufman Brief Intelligence Test (Kaufman & Kaufman, 1990)], behavioral and emotional stability of the child [Child Behavior Checklist/Youth Self-Report (Achenbach, 1991)], and degree of perceived conflict in the family [Conflict Behavior Questionnaire (Robin & Foster, 1988)]. Pretreatment weight control and health behaviors were also assessed, including current weight-control habits [Weight Control Habits Survey (O’Neil et al., 1979; Stalonas & Kirschenbaum, 1985)], ratings of exercise levels [Current Exercise Survey (Paffenbarger, Wing, & Hyde, 1978)], and eating behaviors [Eating Self-Efficacy Scale (Glynn & Ruderman, 1986); Binge Eating Scale (Hawkins & Clement, 1980)]. The parents were administered the Child Behavior Checklist (Achenbach, 1991) and the parent version of the Conflict Behavior Questionnaire (Robin & Foster, 1988). All other measures were administered to the child.
Process Measures
These were the variables that were expected to change to produce the desired weight-loss outcomes. They included attendance at an orientation session [a program component implemented in December 2002 to provide families detailed information about the program before enrollment in an effort to decrease attrition; (Germann, Kirschenbaum, & Rich, 2006)], consistency of self-monitoring [i.e., documentation of the number of days per week that foods and exercise were recorded by children and their parents (Baker & Kirschenbaum, 1993; Boutelle et al., 1999)], and length of treatment.
Procedures
Self-Monitoring and Weight
Children were provided with self-monitoring booklets in which they were strongly encouraged to record all food consumed during each week and to count the calories and fat grams in these foods. They also self-monitored the number of steps taken per day (via a pedometer) and the exercises done. Children signed a behavioral contract committing to self-monitor at least 50% of the time.
A similar procedure was used with the parents/caregivers, usually mothers, who signed a contract committing to self-monitor their own eating and exercising behaviors for the first month of treatment. Parents were also encouraged to continue self-monitoring after the first month. Thus, self-monitoring was an integral part of treatment (in addition to behavioral contracting, training and decision making, problem solving, planning, and relapse prevention), which additionally included nutritional education sessions and a 12-week structured physical therapy/exercise program.
Statistics
Statistical analyses were carried out using SPSS. Analyses of variance (ANOVAs) were conducted to determine differences between groups of children and parents (based on level of self-monitoring) on child weight change (as measured by BMI z-score change). To examine the distinct associations of child and parental self-monitoring with child weight loss, separate analyses were conducted using level of child self-monitoring and level of parental self-monitoring. Next, intellectual functioning, individual and family measures of behavioral and emotional stability, pretreatment weight control and exercise behaviors, process measures, and demographic variables were examined as potential predictor variables (Table I). Discriminant function analyses were conducted to identify predictor variables that discriminated between self-monitoring groups, with separate analyses for child self-monitoring and parental self-monitoring.
This study involved retrospective chart review of the variables described above. The procedures followed were in accordance with the ethical standards of the University of Chicago Institutional Review Board for Human Subjects.
Results
Results of the self-monitoring analyses are presented separately for children and parents and include frequency of self-monitoring, effects on weight loss, and predictors of self-monitoring. Child results are presented for 6 months of treatment. Because of a lack of power for the parent analyses at 6 months, parent results include 3 months of treatment.
Child Self-Monitoring
Frequency
During the first complete month of treatment, 45 of the 228 children (19.7%) failed to self-monitor, 83 (36.4%) averaged less than 3.5 days per week, and 100 (43.9%) averaged 3.5 days per week or more (overall M = 2.94, SD = 2.29). To have sufficient sample size and statistical power for the purposes of these analyses, the children were divided into two self-monitoring groups: Low Monitors (an average of less than 3.5 days weekly) and High Monitors (3.5 days or more weekly). The cut-point of 3.5 days per week was chosen as it was consistent with the program behavioral contracting for self-monitoring 50% of the time, and it approximated the median-split analyses used in prior self-monitoring research (Baker & Kirschenbaum, 1993; Boutelle & Kirschenbaum, 1998; Salaens & McGrath, 2003). The same dichotomous cut-point was used for the overall child self-monitoring averages over 3 and 6 months of treatment. Of those completing at least 3 months of treatment (n = 160), 60 children were High Monitors (overall 3‐month self-monitoring M = 2.79, SD = 1.85), whereas at 6 months of treatment (n = 101), 25 children were High Monitors (overall 6-month self-monitoring M = 2.70, SD = 1.48).
As attrition from the program was evident over time, it is possible that those children with more consistent self-monitoring early in the program tended to stay in the program for a longer duration (i.e., they were the same study participants with more consistent self-monitoring at a later time in the program). To examine this, the first month’s high and low self-monitoring groups were compared according to their overall length of treatment. High self-monitors attended significantly more months of treatment (M = 8.12, SD = 7.12) than the low self-monitors [M = 5.87, SD = 5.8; ANOVA F(1, 225) = 6.84, p = .011], indicating that high self-monitors were more likely to stay in the program for longer periods.
Effects on Weight Loss
During the first month of treatment, no significant differences in weight change were found between the Low and High self-monitoring groups. However, the self-monitoring groups had significant differences in weight change over 3 months of treatment [repeated measures ANOVA F(1, 155) = 9.149, p = .003, η2 = .056] and 6 months of treatment [F(1, 97) = 8.26, p = .005, η2 = .078]. Table II summarizes the BMI z-scores and pound equivalents for the self-monitoring groups at initial assessment and the end of the specified treatment interval (3 and 6 months). Only the High monitors lost a significant amount of weight over both time periods, p < .01.
Child Weight Change According to Child Self-Monitoring Group over Specified Treatment Intervals
| . | Assessment z-score (SD) (pound equivalent) . | End of interval z-score (SD) (pound equivalent) . | Significance (p) . |
|---|---|---|---|
| 3 months | |||
| Low monitors (n = 98) | 6.534 (3.16) (291.86) | 6.530 (3.20) (291.80) | .907 |
| High monitors (n = 59) | 5.575 (2.60) (267.15) | 5.388 (2.51) (262.33) | .000 |
| 6 months | |||
| Low monitors (n = 74) | 6.603 (3.26) (293.64) | 6.534 (3.20) (291.86) | .276 |
| High monitors (n = 25) | 5.813 (3.05) (273.28) | 5.384 (2.94) (262.21) | .000 |
| . | Assessment z-score (SD) (pound equivalent) . | End of interval z-score (SD) (pound equivalent) . | Significance (p) . |
|---|---|---|---|
| 3 months | |||
| Low monitors (n = 98) | 6.534 (3.16) (291.86) | 6.530 (3.20) (291.80) | .907 |
| High monitors (n = 59) | 5.575 (2.60) (267.15) | 5.388 (2.51) (262.33) | .000 |
| 6 months | |||
| Low monitors (n = 74) | 6.603 (3.26) (293.64) | 6.534 (3.20) (291.86) | .276 |
| High monitors (n = 25) | 5.813 (3.05) (273.28) | 5.384 (2.94) (262.21) | .000 |
Child Weight Change According to Child Self-Monitoring Group over Specified Treatment Intervals
| . | Assessment z-score (SD) (pound equivalent) . | End of interval z-score (SD) (pound equivalent) . | Significance (p) . |
|---|---|---|---|
| 3 months | |||
| Low monitors (n = 98) | 6.534 (3.16) (291.86) | 6.530 (3.20) (291.80) | .907 |
| High monitors (n = 59) | 5.575 (2.60) (267.15) | 5.388 (2.51) (262.33) | .000 |
| 6 months | |||
| Low monitors (n = 74) | 6.603 (3.26) (293.64) | 6.534 (3.20) (291.86) | .276 |
| High monitors (n = 25) | 5.813 (3.05) (273.28) | 5.384 (2.94) (262.21) | .000 |
| . | Assessment z-score (SD) (pound equivalent) . | End of interval z-score (SD) (pound equivalent) . | Significance (p) . |
|---|---|---|---|
| 3 months | |||
| Low monitors (n = 98) | 6.534 (3.16) (291.86) | 6.530 (3.20) (291.80) | .907 |
| High monitors (n = 59) | 5.575 (2.60) (267.15) | 5.388 (2.51) (262.33) | .000 |
| 6 months | |||
| Low monitors (n = 74) | 6.603 (3.26) (293.64) | 6.534 (3.20) (291.86) | .276 |
| High monitors (n = 25) | 5.813 (3.05) (273.28) | 5.384 (2.94) (262.21) | .000 |
Predictors of Child Self-Monitoring
Discriminant function analyses were conducted to identify predictors that discriminated between the High and the Low self-monitoring groups at the end of 3 and 6 months. Predictor variables were selected from demographic factors, measures of psychological functioning, and program process variables (see Table I for a complete listing) that correlated significantly with overall average child self-monitoring during both time periods of analysis (3 and 6 months). Accordingly, predictor variables included orientation attendance; child’s BMI z-score at assessment; mother’s ratings of the children’s anxious/depressive symptoms (CBCL Anxious/Depressive Symptoms T-score), children’s aggressive behaviors (CBCL Aggressive Symptoms T-score), and conflict with the child (Conflict Behavior Questionnaire); and mother’s level of self-monitoring for that time period.
The within-group correlations between the predictors of child self-monitoring and the discriminant function as well as the standardized weights are summarized in Table III. At the end of 3 months, the discriminant function differentiated the two self-monitoring groups [Wilks’ Λ = .87, χ2(6, n = 127) = 17.05, p = .009]. Based on the coefficients, mothers’ self-monitoring demonstrated the strongest relationship with the discriminant function. The means on the discriminant functions indicate that the High self-monitors were likely to have mothers who self-monitored more during the first 3 months [M = .84 (SD = 1.40)] than the low self-monitors [M = .17 (SD = .39)]. Group membership was classified correctly for 69.3% of the individuals in the sample (κ = .285).
Standardized Coefficients and Correlations of Predictor Variables with the Discriminant Functions
| . | 3 months . | 6 months . | ||
|---|---|---|---|---|
| . | . | . | ||
| Predictor variable . | Correlation coefficients . | Standardized coefficients . | Correlation coefficients . | Standardized coefficients . |
| Child self-monitoring | ||||
| Orientation attendance | .413 | .163 | −.336 | −.098 |
| Initial body mass index z-score | −.352 | −.297 | .146 | −.037 |
| Mother’s rating of child’s aggressive behaviors | −.254 | .109 | .745 | .563 |
| Mother’s rating of child’s anxious/depressed behaviors | −.237 | −.007 | .045 | −.040 |
| Mother’s rating of conflict with child | −.333 | −.247 | .579 | .234 |
| Mother’s self-monitoring | .912 | .846 | −.738 | −.587 |
| Parental self-monitoring | ||||
| Orientation attendance | 0.773 | 0.780 | na | na |
| Months in program | 0.419 | 0.559 | na | na |
| Mother’s rating of child anxiety/depression | −0.195 | −0.133 | na | na |
| Mother’s rating of child aggression | −0.312 | −0.440 | na | na |
| Mother’s rating of conflict with child | −0.002 | 0.249 | na | na |
| . | 3 months . | 6 months . | ||
|---|---|---|---|---|
| . | . | . | ||
| Predictor variable . | Correlation coefficients . | Standardized coefficients . | Correlation coefficients . | Standardized coefficients . |
| Child self-monitoring | ||||
| Orientation attendance | .413 | .163 | −.336 | −.098 |
| Initial body mass index z-score | −.352 | −.297 | .146 | −.037 |
| Mother’s rating of child’s aggressive behaviors | −.254 | .109 | .745 | .563 |
| Mother’s rating of child’s anxious/depressed behaviors | −.237 | −.007 | .045 | −.040 |
| Mother’s rating of conflict with child | −.333 | −.247 | .579 | .234 |
| Mother’s self-monitoring | .912 | .846 | −.738 | −.587 |
| Parental self-monitoring | ||||
| Orientation attendance | 0.773 | 0.780 | na | na |
| Months in program | 0.419 | 0.559 | na | na |
| Mother’s rating of child anxiety/depression | −0.195 | −0.133 | na | na |
| Mother’s rating of child aggression | −0.312 | −0.440 | na | na |
| Mother’s rating of conflict with child | −0.002 | 0.249 | na | na |
na = not applicable.
Standardized Coefficients and Correlations of Predictor Variables with the Discriminant Functions
| . | 3 months . | 6 months . | ||
|---|---|---|---|---|
| . | . | . | ||
| Predictor variable . | Correlation coefficients . | Standardized coefficients . | Correlation coefficients . | Standardized coefficients . |
| Child self-monitoring | ||||
| Orientation attendance | .413 | .163 | −.336 | −.098 |
| Initial body mass index z-score | −.352 | −.297 | .146 | −.037 |
| Mother’s rating of child’s aggressive behaviors | −.254 | .109 | .745 | .563 |
| Mother’s rating of child’s anxious/depressed behaviors | −.237 | −.007 | .045 | −.040 |
| Mother’s rating of conflict with child | −.333 | −.247 | .579 | .234 |
| Mother’s self-monitoring | .912 | .846 | −.738 | −.587 |
| Parental self-monitoring | ||||
| Orientation attendance | 0.773 | 0.780 | na | na |
| Months in program | 0.419 | 0.559 | na | na |
| Mother’s rating of child anxiety/depression | −0.195 | −0.133 | na | na |
| Mother’s rating of child aggression | −0.312 | −0.440 | na | na |
| Mother’s rating of conflict with child | −0.002 | 0.249 | na | na |
| . | 3 months . | 6 months . | ||
|---|---|---|---|---|
| . | . | . | ||
| Predictor variable . | Correlation coefficients . | Standardized coefficients . | Correlation coefficients . | Standardized coefficients . |
| Child self-monitoring | ||||
| Orientation attendance | .413 | .163 | −.336 | −.098 |
| Initial body mass index z-score | −.352 | −.297 | .146 | −.037 |
| Mother’s rating of child’s aggressive behaviors | −.254 | .109 | .745 | .563 |
| Mother’s rating of child’s anxious/depressed behaviors | −.237 | −.007 | .045 | −.040 |
| Mother’s rating of conflict with child | −.333 | −.247 | .579 | .234 |
| Mother’s self-monitoring | .912 | .846 | −.738 | −.587 |
| Parental self-monitoring | ||||
| Orientation attendance | 0.773 | 0.780 | na | na |
| Months in program | 0.419 | 0.559 | na | na |
| Mother’s rating of child anxiety/depression | −0.195 | −0.133 | na | na |
| Mother’s rating of child aggression | −0.312 | −0.440 | na | na |
| Mother’s rating of conflict with child | −0.002 | 0.249 | na | na |
na = not applicable.
After 6 months of treatment, both mothers’ self-monitoring and mothers’ rating of the child’s aggressive behaviors differentiated between the two child self-monitoring groups (Low and High) [Wilks’ Λ = .74, χ2(6, n = 82) = 23.23, p = .001]. The High self-monitors were more likely to have mothers who self-monitored more frequently [High self-monitors mother self-monitoring M = .93 (SD = 1.28), Low self-monitors mother self-monitoring M = .22 (SD = .38)] and to be rated by their mothers as less aggressive [High self-monitors Aggressive T-score M = 54.57 (SD = 4.61), Low self-monitors Aggressive T-score M = 63.21 (SD = 9.61)]. Group membership was classified correctly for 79.3% of the individuals in the sample (κ = .317).
Parental Self-Monitoring
Frequency
Although parents signed contracts committing to self-monitor for the first month, only 21.1% (48/228) of those remaining in treatment for at least 1 month self-monitored at least once. Of those remaining in treatment for at least 3 months, 28.8% (46/160) of parents self-monitored at least once, whereas 40.6% (41/101) of parents self-monitored during 6 months of treatment (see Table I for overall self-monitoring averages). Percentages of parents who self-monitored half or more of the days were 10% (22/228) for the first month, 2.5% (4/160) for 3 months of treatment, and 2.0% (2/101) for 6 months of treatment. Although higher levels of parental self-monitoring (3.5 days or more per week) would be expected to produce more substantial weight changes (Boutelle & Kirschenbaum, 1998), few parents monitored at this level of consistency that statistical comparisons between such consistent self-monitors and other monitoring groups would be severely under-powered. Also, whether or not parents self-monitored predicted weight changes in children, the importance of this behavioral index of parental involvement for both assessment and treatment would be reinforced; therefore, analyses of parental self-monitoring for this study focused on whether or not parents self-monitored.
Effects on Weight Loss
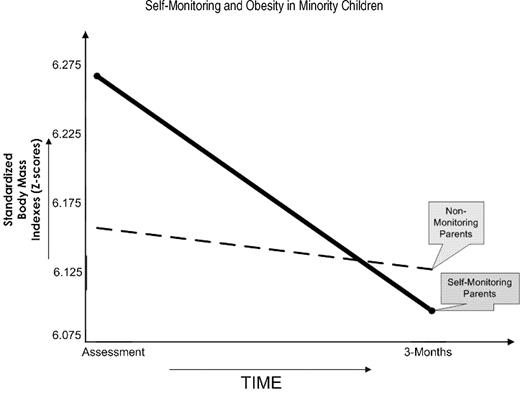
Repeated measures ANOVA revealed significant differences between parental self-monitoring groups (None versus Any) on child weight change during the first month [F(1, 223)= 4.21, p = .041, η2 = .019] and after 3 months of treatment [F(1, 154) = 4.83, p = .030, η2 = .030]. At the end of 1 month of treatment, the children of parents who self-monitored had lost a significant amount of weight [initial BMI z-score M=6.17 (SD = .44), 1 month BMI z-score M=6.09 (SD = .44), Tukey LSD p = .003), whereas the children of parents who did not self-monitor did not lose significant weight [initial BMI z-score M=6.10 (SD = .23), 1 month BMI z-score M=6.08 (SD = .23), Tukey LSD p = .221]. Figure 1 demonstrates the change in child weight over 3 months according to the level of parental self-monitoring and shows that the children of parents who self-monitored at least once during the first 3 months of treatment also were more likely to lose weight than the children of parents who did not self-monitor (Tukey LSD p < .003). Parental self-monitoring did not have a significant effect on child weight loss at 6 months, which may have been affected by decreased power in the latter analysis (observed power in the first 3 months = 4.825 versus observed power at 6 months = .191).
Parental self-monitoring and child weight change during the first 3 months of treatment.
Predictors and Correlates of Parental Self-Monitoring
Discriminant function analyses were conducted to identify predictors that discriminated between the Any and No parental self-monitoring groups at the end of 3 months of treatment (based on above analyses). Predictor variables were selected from demographic factors, measures of psychological functioning, and program process variables (see Table I for a complete listing) that correlated significantly with the overall average parental self-monitoring over 3 months of treatment, which included orientation attendance (a program component added in 2002; consequently, families who enrolled in the program before the implementation of this component did not attend orientation); length of treatment; and mother’s ratings of the children’s anxious/depressive symptoms (CBCL Anxious/Depressive Symptoms T-score), children’s aggressive behaviors (CBCL Aggressive Symptoms T-score), and conflict with the child (Conflict Behavior Questionnaire). The second half of Table III summarizes the within-group correlations between the predictors of parental self-monitoring and the discriminant function as well as the standardized weights. The discriminant function differentiated the two parental self-monitoring groups [Wilks’ Λ = .83, χ2(4, n = 131) = 23.17, p = .000]. Based on these coefficients, orientation attendance (a dichotomous variable with nonorientation = 1, orientation = 2) demonstrated the strongest relationship with the discriminant function. The means on the discriminant functions indicate that the parents who did Any self-monitoring were more likely to have attended orientation (M = 1.74) than the parents who did not self-monitor (M = 1.38). Group membership was classified correctly for 71% of the individuals in the sample (κ = .210).
Finally, the relationship between parental and child self-monitoring was assessed. ANOVA using the Brown-Forsythe statistic to control for inequality of error variances revealed that parents who self-monitored were much more likely to have children who self-monitored [F(1,158) = 22.03, p = .000, partial η2 = .123]. The self-monitoring by children of parents who self-monitored was 60% greater [M days weekly = 3.81 (SD = .247)] than the self-monitoring by children of parents who did not self-monitor [M days weekly = 2.38 (SD = .164)].
Impact of Orientation on Self-Monitoring
Orientation attendance was a significant predictor of parental self-monitoring over the first 3 months of treatment, and parental self-monitoring was significantly related to child weight loss and child self-monitoring over 3 months of treatment; however, not all families had the opportunity to attend orientation (as it was a program component added in December 2002). It is possible that parental self-monitoring could have had a differential impact on child weight loss and child self-monitoring according to whether families attended orientation; if so, the orientation session could be viewed as an intervention in itself, and the subgroups should be evaluated separately. To examine the potential impact of orientation attendance on parental self-monitoring (as it relates to child weight loss and child self-monitoring), patterns of self-monitoring (parent and child) and child weight loss over the first 3 months of treatment were explored within subgroups of families who attended orientation (n = 69) and those families who enrolled in the program before the implementation of the orientation sessions (n = 93). Within both subgroups (orientation and nonorientation), parental self-monitoring was significantly correlated with child weight loss [orientation subgroup: r(64) = −.24, p < .05; non-orientation subgroup: r(87) = −.23, p < .05] and child self-monitoring [orientation subgroup: r(64) = .51, p < .001; non-orientation subgroup: r(90) = .47, p < .001]. However, those parents who attended orientation were more likely to self-monitor at some level during the treatment interval [Pearson χ2(1, n = 162) = 22.32, p = .000]. Specifically, 48% of parents who attended orientation self-monitored at some level (the Any monitoring subgroup) during the initial 3 months of treatment compared with only 14% of parents who did not attend orientation. Although the parents who attended orientation were more likely to self-monitor, the significant correlations between parental self-monitoring and child weight loss/child self-monitoring regardless of whether families attended orientation indicate that the orientation subgroups show similar self-monitoring and weight-loss relationships, justifying evaluation of these effects by combining the subgroups (those who did and did not attend orientation).
Discussion
This study was a continuation of an initial study (Kirschenbaum et al., 2005) which provided evidence that child and parental self-monitoring during early treatment (the first 3 months) was as important for initial weight-loss success in a low-income minority population as it is in more stable middle-class populations. The purpose of this study was to replicate and extend those findings over a longer period of time (6 months of treatment) in a population of low-income minority children.
Approximately half (43.9%) of the children self-monitored on most days over the first month of this evaluation. By the end of the first 6 months of treatment, however, only one-quarter of the children were self-monitoring on most days. This level of child self-monitoring is somewhat less than has been noted among middle-class adults, with about 50% of weight controllers self-monitoring most of the time over several months and only 10–20% self-monitoring quite inconsistently (Baker & Kirschenbaum, 1993; Schlundt, Sbrocco, & Bell, 1989). Nevertheless, as expected, consistent child self-monitoring was associated with significant child weight loss over the 6-month period, whereas those children who self-monitored less consistently did not show significant weight changes. This is consistent with results found in populations of middle-class adolescents (Flanery & Kirschenbaum, 1986; Salaens & McGrath, 2003) and middle-class adults (Baker & Kirschenbaum, 1993; Boutelle et al., 1999).
In addition to weight loss, child self-monitoring was associated with the length of treatment, with higher self-monitors remaining in treatment for longer periods. Longer treatment intervals have been associated with greater weight loss (Craighead, Stunkard, & O’Brien, 1981; Epstein, Wing, Koeske, Andrasik, & Ossip, 1981; Kirschenbaum, Harris, & Tomarken, 1984), as have regular program attendance (Carels, Cacciapaglia, Douglass, Rydin, & O’Brien, 2003) and continuing care over a period of years (Latner, Wilson, Stunkard, & Jackson, 2002). It is possible that a greater commitment to success is expressed behaviorally by both self-monitoring and attending treatment for longer periods. In the case of a family-focused intervention for child weight loss, child commitment relies on parental commitment; for example, parents are responsible for bringing the family to treatment each week, and ideally, parents supervise the completion of the child’s self-monitoring booklets, much as they would oversee the completion of their child’s school homework. Greater parental commitment could result in children monitoring more consistently, making greater changes in diet and activity at home and reinforcing children’s efforts more directly. Improved weight changes certainly would be expected from such enhanced commitments.
Another important indicator of parental commitment to child weight loss appears to be parental self-monitoring. This study found that parental self-monitoring was a significant predictor of child self-monitoring. This result emerged despite a relatively low level of parental self-monitoring (e.g., only 29% self-monitoring at least once over the first 3 months of treatment). One possible explanation is that just as caregivers shape eating and activity habits (Birch & Davison, 2001; Birch & Fisher, 1998; Kohl & Hobbs, 1998), parents who self-monitor might also be shaping the target behavior of self-monitoring in their children. It is also possible that the role-modeling by self-monitoring parents increases their children’s efforts to self-monitor. Even a very low level of parental self-monitoring (only once or a few times over the treatment period) may demonstrate to children the critical importance of self-monitoring and also help children through any initial confusion about how to complete the self-monitoring booklet, which likely reduces obstacles to the child’s self-monitoring.
Not only did parents who self-monitored have children who self-monitored more, but their children also lost significantly more weight over the initial 3 months, as compared with the children of parents who did not self-monitor. Parental self-monitoring was not significantly related to child weight loss at the end of 6 months of treatment, but so few parents continued to self-monitor for 6 months that the power to detect a significant result was limited (observed power = .191). Nevertheless, the association of parental monitoring with child weight loss over the initial 3 months of treatment is consistent with and expands the results of our initial evaluation study of this program (Kirschenbaum et al., 2005), which found parental self-monitoring over just the first month of treatment to be related to significant child weight loss over the entire first 3 months of treatment. Just as a treatment program focused solely on parents improved weight loss by children (Golan & Crow, 2004) compared with an intervention focused on the children alone, it is possible that the added focus of parental self-monitoring could help parents become even more aware of the family’s eating and exercise choices and consequently target areas for change more consistently. It is also possible that because many of the mothers in this program were themselves obese [mean BMI of mother = 35.42 (SD = 9.35)], and endeavoring to lose weight, self-monitoring helped the mothers to focus on their own behavioral change (such as becoming more active or buying and preparing healthier foods) which extended to the other household members.
Given the influential role of parental self-monitoring on child weight loss and self-monitoring, methods to increase parental self-monitoring should be considered. In this study, attendance of a program orientation session was the significant predictor of parental self-monitoring. The orientation session was a program component added in December 2000 in an attempt to decrease attrition by providing potential participants detailed information about the program. While the orientation session was shown to be related to decreased attrition (Germann et al., 2006), the orientation session also may have had an impact on parental self-monitoring: 48% of parents who attended orientation self-monitored at some level during the initial 3 months of treatment compared with only 14% of parents who did not attend orientation. It is possible that the information provided during the orientation session (e.g., program structure as well as expectations for family involvement) provided extra encouragement for parental behaviors such as self-monitoring or that families who were not ready to commit to the target family behaviors self-selected themselves away from enrollment in the program. The exact influence of the orientation session on parental self-monitoring, as well as other targeted weight loss behaviors (such as child self-monitoring), warrants further study.
Overall, these findings indicate that despite the substantial challenges faced by low-income minority children with morbid obesity, consistent self-monitoring emerged, once again, as a cornerstone in effective weight control. To manage the notoriously resistant biological barriers to weight loss and maintenance (Brownell, Kelman, & Stunkard, 1983; Kirschenbaum, 2000; Wadden, 1993; Wadden & Stunkard, 2002), weight controllers who focus very consistently on the details of their eating and activity/exercising behaviors fare much better than those who do not. Self-monitoring engages critical self-regulatory processes including self-evaluation (comparisons to goals) and self-reinforcement (Kanfer & Karoly, 1972) when affective and cognitive states (e.g., attributions, expectations) allow that to happen (Baumeister, Heatherton, & Tice, 1994; Carver & Scheier, 1990; Kanfer & Gaelick-Buys, 1991). This may culminate over time in the development of a “healthy obsession” (Kirschenbaum, 1987; Kirschenbaum, 2000) that can produce lifelong weight control (Wing & Hill, 2001).
Regardless of the causes of the modest levels observed of both child and parental self-monitoring, these behaviors deserve to be primary targets in all weight-control programs (Baker & Kirschenbaum, 1993). One option would be to use parental self-monitoring as a motivational screening device. For families with an initial low level of self-monitoring, more intensive or structured interventions for increasing child and parental self-monitoring could be considered, such as structured contingency systems for parents who self-monitor or enhanced CBT programs with more contact and reminders about self-monitoring (e.g., Internet, phone calls) (Perri et al., 1993; Tate, Wing, & Winett, 2001). With more consistent self-monitoring, the impact of parent and child self-monitoring over longer periods could be evaluated in this psychosocially challenged population to determine whether self-monitoring is as important to long-term weight loss success as it is in the initial stages of treatment.
The overall modest weight losses and relatively high attrition observed in this evaluation reinforce prior findings showing poorer outcomes for low-income minorities (Beliard, Kirschenbaum, & Fitzgibbon, 1992). Specific measures of perceived stress, stressful events, and daily hassles could be used in future studies to clarify whether self-monitoring (and weight loss) diminishes in this population under more stressful circumstances, as suggested here. In addition, the present results suggest that more intensive or enhanced versions of CBT as well as more intensive treatments [e.g., immersion programs such as camps or boarding schools (see healthylivingacademies.com)] and more biologically oriented treatments (e.g., medications, surgery) may be warranted for low-income minority children with morbid obesity.
Acknowledgments
The evaluation of the FitMatters Weight Control Program is an ongoing study conducted at La Rabida Children’s Hospital. The study is supported in part by grants from the Galter Foundation, Foundation for Health Enhancement, Northern Trust Charitable Trust, Circle of Service Foundation, Vital Community Healthcare Foundation, Frederick E. and Ida M. Hummel Foundation, and the Max Goldenberg Foundation. The authors greatly appreciate the clinical skills and commitment of Beth Eliadis, LCSW; Aimee Henrikson, RD; Megan Aronson, RD; Sandra Barlow, DPT; and Leslie Reynolds; and the support and encouragement of Neil Hochstadt, PhD and Paula Jaudes, MD.