-
PDF
- Split View
-
Views
-
Cite
Cite
Michele Brignole, Carlo Menozzi, Angelo Bartoletti, Franco Giada, Alfonso Lagi, Andrea Ungar, Irene Ponassi, Chiara Mussi, Roberto Maggi, Giuseppe Re, Raffaello Furlan, Gianni Rovelli, Patrizia Ponzi, Alessandro Scivales, for the Evaluation of Guidelines in Syncope Study 2 (EGSYS-2) group†, A new management of syncope: prospective systematic guideline-based evaluation of patients referred urgently to general hospitals, European Heart Journal, Volume 27, Issue 1, January 2006, Pages 76–82, https://doi.org/10.1093/eurheartj/ehi647
Close - Share Icon Share
Abstract
Aims The guidelines of the European Society of Cardiology (ESC) define the current standard for the management of syncope, but are still incompletely applied in the clinical setting.
Methods and results Prospective systematic evaluation, on strict adherence to the guidelines, of consecutive patients referred for syncope to the emergency departments of 11 general hospitals. In order to maximize the application, a decision-making guideline-based software was used and trained core medical personnel were designated—both locally in each hospital and centrally—to verify adherence to the diagnostic pathway and give advice on its correction. A diagnostic work-up consistent with the guidelines was completed in 465/541 patients (86%). A definite diagnosis was established in 98% (unexplained in 2%): neurally mediated syncope accounted for 66% of diagnosis, orthostatic hypotension 10%, primary arrhythmias 11%, structural cardiac or cardiopulmonary disease 5%, and non-syncopal attacks 6%, respectively. The initial evaluation (consisting of history, physical examination, and standard electrocardiogram) established a diagnosis in 50% of cases. Hospitalization for the management of syncope was appropriate in 25% and was required for other reasons in a further 13% of cases. The median in-hospital stay was 5.5 days (interquartile range, 3–9). Apart from the initial evaluation, a mean of 1.9±1.1 appropriate tests per patient was performed in 193 patients and led to a final diagnosis in 182 of these (94%).
Conclusion The results of this study assess the current standard for the management of syncope on the basis of a rigorous adherence to guidelines of the ESC and provide a frame of reference for daily activity when dealing with syncope.
See page 7 for the editorial comment on this article (doi:10.1093/eurheartj/ehi626)
Introduction
Current strategies for diagnosis of syncope vary widely among physicians and among hospitals. Evaluation and treatment of syncope are often haphazard and unstratified. This results in inappropriate use of diagnostic tests and in a high rate of misdiagnosed and still unexplained syncope. The consequence is over-utilization of medical resources and over-expenditure associated with syncope management.1–5
The earlier considerations have led to the development of several diagnostic and triaging pathways1,6–11 and expert consensus statements.12–14 The recent guidelines on Management of Syncope of the European Society of Cardiology (ESC)15,16 define the current standard for the management of patients with transient loss of consciousness, establish the most effective diagnostic pathway, give recommendations on indications and the interpretation of diagnostic tests, and provide indications for hospitalization and treatment. Presently, neither the ESC guidelines nor those of other organizations have been prospectively evaluated in clinical studies.
This study was a systematic population-based evaluation of management of syncope based on strict adherence to the ESC guidelines. It was aimed at providing all stakeholders (physicians, hospital and clinical governance managers, future research planners, etc.) with a frame of reference for their daily activity when dealing with syncope.
Methods
The study was prospective and included consecutive patients admitted to the emergency services of 11 general hospitals in Italy from 4 October 2004 to 5 November 2004 either because they were affected by transient loss of consciousness which, on initial evaluation, was attributed to a syncopal condition or because a syncopal condition could not be excluded (non-syncopal loss of consciousness). Patients with a definite non-syncopal cause of loss of consciousness on initial evaluation, those aged <18, and those referred >24 h after their episode were excluded.
The recruiting centres were public general hospitals with a median of 147 658 inhabitants per district of referral (interquartile range, 114 563–326 768). In the year 2004, these hospitals had a median of 44 995 admissions to the emergency room (interquartile range, 38 314–61 093). Together, they serve a population of 2 426 195 inhabitants, a figure which accounts for 4.3% of the total population of Italy. Each hospital has a 24 h emergency department and a cardiology ward with a coronary care unit and meets the requisites for the management of syncope set by the ESC guidelines.15,16 These include core equipment for syncope evaluation (i.e. phasic blood pressure monitoring, tilt table testing, external and implantable loop recorder, 24 h ambulatory blood pressure monitoring, 24 h ambulatory electrocardiographic monitoring, and autonomic function testing), on-site access to usual investigations (echocardiography, invasive electrophysiological testing, stress testing, cardiac imaging, computed tomography or magnetic resonance imaging, and electroencephalography), and on-site access to any therapy that may be required for syncope (i.e. pacemaker and ICD implantation, catheter ablation of arrhythmias, etc.). Moreover, in each hospital, intranet and internet networks were available in order to run the dedicated software used for the study (discussed subsequently).
The protocol was approved by the Ethics Committee of all participating hospitals, and all participants gave written informed consent.
Diagnostic pathway and management strategy
All patients underwent the diagnostic evaluation on strict adherence to the recommendations of the ESC guidelines.15,16 In order to maximize the application of those guidelines, two main issues were accomplished: the use of a decision-making software based on the ESC guidelines (EGSYS software, version 1.0) and the training of a designated physician in each hospital participating in the study who interacted with a central supervisor as far as the management of syncope according to ESC criteria was concerned.
The EGSYS software is a web-based on-line interactive decision-making system developed to help the physician to follow the diagnostic pathway and the recommendations of the ESC guidelines. After logging-in, the authorized physician first filled in the initial evaluation form, which collected standardized data concerning the patient's history, physical examination, including supine and standing blood pressure measurement, and standard electrocardiogram. Thereafter, physicians were asked whether loss of consciousness was attributable to syncope or to non-syncopal conditions and whether a likely diagnosis was possible on the basis of the available information. A ‘help’ command provided precise definitions from the guidelines in order to assist physicians with the appropriate pathway to be followed here and elsewhere when appropriate. If a diagnosis was impossible at this stage, the software provided a list of clinical features suggesting a possible diagnosis, which needed to be confirmed by further tests. According to the selected features, the software suggested the appropriate diagnostic test and its interpretation. Once the evaluation was completed and no cause of syncope could be determined, a re-appraisal form enabled the entire diagnostic process to be reconsidered. When a likely diagnosis was reached, this was classified according to the ESC classification.15,16 Finally, the software contained a form for collecting data on hospitalization, resource consumption, and therapeutic strategy. The EGSYS software was made available in intrahospital and interhospital networks in order to allow regular communication with all stakeholders (i.e. local and central investigators, clinical staff in the accident and emergency, cardiology, neurology, general medicine, orthopaedic surgery, geriatric medicine, psychiatry, and ear nose and throat departments, etc.) and ensure a consensus for, and understanding of, proposed management strategies.
In each hospital, an investigator usually involved in the management of syncope was designated and instructed to run the study. Each day, the investigators were informed of every new admitted patient affected by loss of consciousness. They followed the subsequent diagnostic flow of the patients and gave advice in order to maintain strict adherence to the standardized work-up. They were responsible for reviewing the patients' files and assigning the reported final diagnosis to one of the categories of the classification of loss of consciousness. Whenever discrepancies with the guidelines arose, they re-evaluated the case with the central clinical monitors. The central clinical monitors, cardiologists who were experts in syncope management (M.B. and R.M.), had on-line access to the database. They supervised the entire process daily, verified adherence to the diagnostic pathway for all patients, and gave advice on any corrections deemed necessary.
Drop-out criteria (patient's refusal, protocol violation, incomplete evaluation, and incomplete records) were pre-defined. Although minor deviations from the protocol, such as the execution of tests that were at risk of being inappropriate or that had been indicated for causes other than syncope (i.e. trauma, underlying comorbidities, usual routine of the centre, etc.), did not constitute a reason for drop-out, these were counted separately.
Study endpoints
The primary endpoint of the study was to assess the management of syncope (i.e. diagnostic pathway, resource consumption, final diagnosis, and treatment) in accordance with the ESC guidelines. The secondary endpoint was to evaluate the applicability of the ESC guidelines to clinical practice.
Sample size and incidence
A major priority was that the study population should be representative of the general population of patients referred to the emergency departments and that the recruitment period should be short in order to achieve better adherence to guidelines. On the basis of previous epidemiological data,3 we calculated that 10 medium- and large-volume hospitals would be enough to collect 500 patients affected by loss of consciousness during a 1-month period and that about 50 of these patients would have a diagnosis of primary cardiac arrhythmia, which constitutes the most challenging diagnosis of syncope.
The overall incidence rate and the incidence rate of the first episode of syncope were calculated by dividing the number of patients with syncope by the total number of persons admitted to the emergency department; assuming a constant incidence over time, the yearly incidence rate was then calculated.
Results
The clinical characteristics of the 541 patients enrolled are shown in Table 1.
Incidence
The overall incidence rate of admission for transient loss of consciousness was 2.6 per 1000 person-years and represented 1.1% of total admissions in the same period (Table 1). The incidence rate increased with age, rising sharply at 70 years; 25 and 22% of the overall population were in the age ranges of 70–79 and 80–89, respectively. The incidence rate of the first episode was 1.6 per 1000 person-years.
Diagnosis
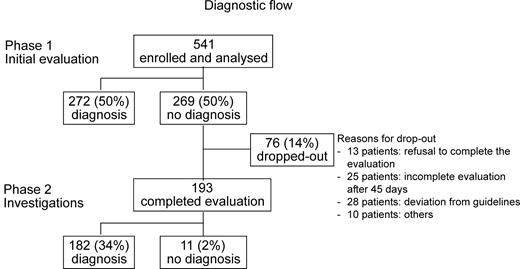
A diagnostic work-up consistent with that recommended by the ESC guidelines was achieved in 465 patients (86%); the reasons for the drop-out of the remaining 76 patients are listed in Figure 1. The central supervisor syncope expert had to provide recommendations to follow the diagnostic work-up for 150 patients (32%).
A diagnosis was established on initial evaluation in 50% of patients. Finally, a cause of syncope was established in all patients who completed the work-up with the exception of 11 subjects (2%). A neurally mediated cause of syncope was established in 66%, orthostatic hypotension in 10%, primary cardiac arrhythmias in 11%, structural cardiac or cardiopulmonary disease in 5%, and non-syncopal attacks in 6% (Table 2).
Among the 309 patients with neurally mediated syncope, the diagnosis was made on the basis of the initial evaluation in 202 (65%) of cases, vasovagal and situational being the most frequent forms. Carotid sinus massage established the diagnosis in 18 patients (6%) and tilt testing in 38 patients (12%). In 51 patients (17%), the diagnosis was suspected on the basis of the clinical features (non-classical form) and thereafter established by excluding other possible competing diagnoses and the absence of structural heart disease.
Syncope due to orthostatic hypotension was established during the initial evaluation in 36 patients in whom the assumption of the standing position caused a rapid symptomatic drop in systolic blood pressure from a value of 128±22 to 96±26 mmHg. A diagnosis of orthostatic hypotension was also subsequently established in 10 of 28 patients who showed an asymptomatic orthostatic fall in systolic blood pressure >20 mmHg during the initial evaluation (from a value of 143±26 to 114±24 mmHg) by means of tilt testing, which showed the typical pattern of late progressive orthostatic hypotension in eight cases, by 24 h blood pressure monitoring in one case, and by repeated orthostatic blood pressure measurement in one case. Finally, a diagnosis different from that of orthostatic hypotension was made at the end of the work-up in the remaining 18 patients with an asymptomatic orthostatic hypotension.
Syncope due to cardiac causes was established in 74 patients: in 34 of these by means of standard electrocardiogram during the initial evaluation and in the remaining 40 by means of other cardiological tests (Table 3).
In 26 patients, non-syncopal cause of loss of consciousness was confirmed by investigations. These were electroencephalography, brain computed tomographic scan and magnetic resonance imaging in the case of epilepsy, transient vertebro-basilar attack and laboratory blood tests in the case of hypoglycaemia and intoxication, and re-appraisal—including psychiatric consultancy—in the case of falls and psychogenic pseudo-syncope (Table 3). Carotid echo-Doppler never was useful for diagnosis.
Overall, among 823 tests, which were appropriate according to the recommended indications of the ESC guidelines, 171 (21%) provided a response that was consistent with class I diagnostic recommendations of those guidelines (Table 3). Excluding the standard electrocardiogram taken during the initial evaluation, 358 appropriate tests were performed in 193 patients (mean 1.9±1.1 tests per patient). One test was necessary in 94 patients, two tests in 53, and three or more tests in 46.
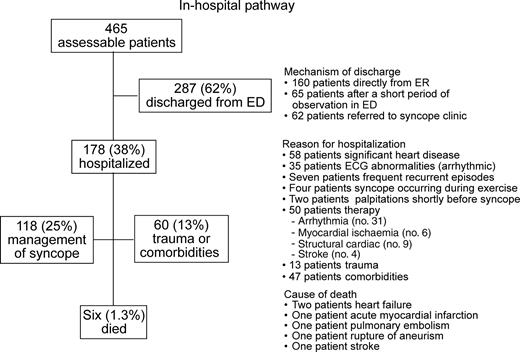
In-hospital pathway and treatment
Hospitalization for the management of syncope was appropriate in 118 patients (25%) and was required in 13% of cases for other reasons. The reasons for hospitalization are listed in Figure 2. The median in-hospital stay was 5.5 days (interquartile range, 3–9). Six patients (1.3%) died before discharge. The treatment assigned at the end of the work-up is summarized in Table 4.
Discussion
The present study was aimed at assessing the management of syncope, as recently defined by the ESC guidelines.15,16 The results of this study probably assess the current standard for the management of syncope.
Although the results of this study are difficult to reproduce in everyday practice, it was aimed at providing all stakeholders (physicians, hospital and clinical governance managers, future research planners, etc.) with a frame of reference for their daily activity when dealing with syncope.
Compared with previous studies in this field, the present study has the advantage of using a unique methodology. First, it utilizes the definitions and recommendations of the authoritative and generally accepted ESC guidelines.15,16 Syncope is a transient symptom and its diagnosis is often only presumptive. Uncertainty is further compounded by the fact that there is a great deal of variation in how physicians take a history and perform a physical examination, in the types of tests requested, and in how they are interpreted. Consequently, there is a need for specific criteria for making diagnoses on the basis of history and physical examination, choosing tests, interpreting test abnormalities, and using the results to establish the cause of syncope. Such criteria are provided by the consensus of a large international panel of experts. Secondly, an interactive decision-making software was used and highly trained medical personnel were identified, in order to obtain a close adherence to the protocol. Thirdly, owing to its design, this study involved a population-based sample of consecutive patients referred to emergency departments which was biased only by the access criteria. The age distribution of the patients, which peaked in the seventh and eighth decades, is in keeping with the data obtained in the Framingham study.17 The incidence rate of the first report of syncope in patients admitted to the emergency department (1.6 per 1000 person-years) was one-fourth of the incidence of 6.2 per 1000 person-years observed in the general population in the Framingham study,17 which means that ∼25% of the general population with syncope seek medical evaluation.
As a consequence of these methodological features, our results may markedly differ from those of previous investigations. For example, a comparative analysis of population-based studies2–6,18–23 shows, for example, a diagnosis of neurally mediated syncope ranging from 13 to 49% of patients and a diagnosis of cardiac syncope ranging from 6 to 46% of patients. We found neurally mediated syncope in 66% of patients and a likely diagnosis in virtually all patients, being syncope unexplained in only 2%. These values are by far the highest ever found.
The present guideline-based approach seems to be more effective than previously reported. In this study, no diagnostic test, apart the initial evolution, was necessary in many patients and few diagnostic tests per patient were needed in a minority of patients providing an excellent diagnostic yield (Table 3). Conversely, in a previous study,8 an extensive use of tests provided a diagnosis in only 25% of cases. An average of 2.1 and 3.5 tests was found in other two studies,3,6 but the cause of syncope remained unexplained in 54 and 19% of cases, respectively. In the present investigation, the hospitalization rate was lower than the 46–63% range reported in other studies,2,3,7,8 as was the duration of the in-hospital stay which, in other studies, ranged from 6.9 to 11.3 days.2,3,7 The ESC risk stratification for hospitalization allowed many patients to be discharged safely from the emergency department; indeed, 12% were discharged after having received continuous cardiac monitoring in a designated area of the observation unit for a few hours and another 12% were referred to a syncope clinic (Figure 2).
We do not provide data on the follow-up or prognosis of syncope, as it is out of the scopes of this study. Prognostic stratification has been dealt with in several studies, both old and recent.8,10,17,18,20,22,24,25 Our patients received the proper treatment recommended by guidelines. The assessment of efficacy of therapy is better evaluated by randomized controlled trials.
Conclusions and perspectives
The present study provides a systematic evaluation of the management of syncope on the basis of a rigorous adherence to guidelines of the ESC. The results of this study probably assess the current standard for the management of syncope and provide a frame of reference for daily activity when dealing with syncope.
Although the results of this study are difficult to reproduce in everyday practice, the study shows that ESC guidelines can be implemented in the clinical setting, provided the presence of trained medical personnel and the use of specifically designed decision-making software. Thus, these results support the creation of cohesive, structured syncope facilities, as in the model proposed by the ESC guidelines15,16 or by others,9,10,11 in order to provide optimal quality service on the basis of well-defined up-to-date diagnostic guidelines.
Acknowledgements
This study was supported by a grant from Gruppo Italiano per lo Studio della Sincope (GIMSI). Organizational support and cost analysis provided by Fondazione Medtronic Italia. Endorsed by Associazione Italiana Aritmologia e Cardiostimolazione (AIAC), Associazione Italiana studio Neurovegetativo (AINV), Società Italiana Medicina d'Emergenza e Urgenza (SIMEU), Società Italiana Gerontologia e Geriatria (SIGG), Federazione dell'Associazione dei Dirigenti Ospedalieri Internisti (FADOI), and Società Italiana di Medicina Interna (SIMI).
Conflict of interest: A.S. and P.P. are employes of Fondazione Medtronic.
Appendix
The following persons participated in the EGSYS-2 study. Steering Committee—F. Ammirati, M. Brignole, I. Casagranda, P. Cortelli, M. Disertori, R. Furlan, F. Giada, I. Iori, A. Lagi, M. Lunati, G. Mathieu, C. Menozzi, G. Miceli, C. Mussi, P. Ponzi, A. Raviele, G. Re, M.A. Ribani, G. Sandrone, A. Scivales, and A. Ungar; EGSYS 2 Database Production—M. Brignole, M. Montagni, and R. Maggi; EGSYS 2 Database Management—M. Montagni; Monitoring and EndPoint Committee—M. Brignole and R. Maggi; Analysis of data—M. Brignole and R. Maggi; Cost analysis—A. Scivales and P. Ponzi; Investigators—L. Bagnoli, G. Baldi, A. Bartoletti, M. Borella, M. Brignole, I. Casagranda, S. Cencetti, S. Colombo, S. Dassi, S. De Ceglia, M. Del Greco, A. Del Rosso, S. Dell'Orto, P.G. Demarchi, R. di Leo, M. Disertori, O. Durin, P. Fabiani, F. Ferrari, A. Foffa, G. Foglia Manzillo, R. Furlan, U. Gargano, F. Giada, S. Grifoni, A. Lagi, F. Locati, M. Lunati, R. Maggi, M. Marenco, G. Masotti, C. Menozzi, C. Moro, C. Mussi, G. Noro, E. Occhetta, S. Perdetti, A. Poggi, I. Ponassi, F. Quartieri, A. Raviele, G. Re, M.A. Ribani, G. Rovelli, P.M. Saggese, G. Salvioli, G. Tava, A. Ungar, A. Vado, R. Vecchi, F. Vicari, A. Vincenti, and G. Vita.
The Evaluation of Guidelines in Syncope Study 2 (EGSYS-2) investigators is listed in the appendix.
Figure 1 Diagnostic flow of 541 patients affected bytransient loss of consciousness which, on initial evaluation, was attributed to a syncopal condition or because a syncopal condition could not be excluded (non-syncopal loss of consciousness). There were several reasons for drop-out in 76 patients. The most frequent were: some patients decided to leave the emergency room against the physician's intention; some patients could not complete the evaluation within 45 days because of dominant comorbidities or severe trauma secondary to syncope; in some cases, the physician in charge refuted to follow the recommendations of the guidelines and/or the suggestions of the syncope expert; and finally, there were few cases of incorrect insertion in the database.
Figure 2 In-hospital pathway. Some patients had more than one reason for hospitalization.
Characteristics of the patients with transient loss of consciousness (LOC)
| Total patients attending the emergency room | 51 049 |
| Total patients with LOC attending the emergency room (%) | 541 (1.1) |
| Patients with LOC per hospital (mean±SD) | 49±12 |
| Time between LOC and arrival at emergency room <6 h (%) | 385 (71) |
| Median age (interquartile range) | 71 (48–81) |
| Male gender (%) | 289 (53) |
| Normal electrocardiogram (%) | 327 (60) |
| No structural heart disease (%) | 341 (63) |
| Comorbidities | |
| Hypertension (%) | 221 (41) |
| Any neurological disease (%) | 110 (20) |
| Diabetes (%) | 47 (9) |
| Any therapy at the time of LOC (%) | 272 (50) |
| History of LOC: first episode (%) | 313 (58) |
| Recurrent LOCs: median number per patient (interquartile range) | 2 (2–4) |
| Interval between first and last episode – year (interquartile range) | 3 (1–8) |
| History of pre-syncope (%) | 109 (20) |
| Injuries related to fainting (%) | 138 (25) |
| Major injuries (fractures, brain concussion) (%) | 60 (11) |
| Minor injuries (bruises, etc.) (%) | 78 (14) |
| No warning at the onset of the attack (%) | 163 (30) |
| Circumstances just prior to the attacka | |
| Standing (%) | 363 (67) |
| Rest (no activity) (%) | 286 (53) |
| Any pre-disposing factors (%) | 474 (87) |
| Total patients attending the emergency room | 51 049 |
| Total patients with LOC attending the emergency room (%) | 541 (1.1) |
| Patients with LOC per hospital (mean±SD) | 49±12 |
| Time between LOC and arrival at emergency room <6 h (%) | 385 (71) |
| Median age (interquartile range) | 71 (48–81) |
| Male gender (%) | 289 (53) |
| Normal electrocardiogram (%) | 327 (60) |
| No structural heart disease (%) | 341 (63) |
| Comorbidities | |
| Hypertension (%) | 221 (41) |
| Any neurological disease (%) | 110 (20) |
| Diabetes (%) | 47 (9) |
| Any therapy at the time of LOC (%) | 272 (50) |
| History of LOC: first episode (%) | 313 (58) |
| Recurrent LOCs: median number per patient (interquartile range) | 2 (2–4) |
| Interval between first and last episode – year (interquartile range) | 3 (1–8) |
| History of pre-syncope (%) | 109 (20) |
| Injuries related to fainting (%) | 138 (25) |
| Major injuries (fractures, brain concussion) (%) | 60 (11) |
| Minor injuries (bruises, etc.) (%) | 78 (14) |
| No warning at the onset of the attack (%) | 163 (30) |
| Circumstances just prior to the attacka | |
| Standing (%) | 363 (67) |
| Rest (no activity) (%) | 286 (53) |
| Any pre-disposing factors (%) | 474 (87) |
LOC, loss of consciousness.
aSee definition in Table 2.1, Guidelines on Syncope, Europace 2004a; 6: 467–537.
Characteristics of the patients with transient loss of consciousness (LOC)
| Total patients attending the emergency room | 51 049 |
| Total patients with LOC attending the emergency room (%) | 541 (1.1) |
| Patients with LOC per hospital (mean±SD) | 49±12 |
| Time between LOC and arrival at emergency room <6 h (%) | 385 (71) |
| Median age (interquartile range) | 71 (48–81) |
| Male gender (%) | 289 (53) |
| Normal electrocardiogram (%) | 327 (60) |
| No structural heart disease (%) | 341 (63) |
| Comorbidities | |
| Hypertension (%) | 221 (41) |
| Any neurological disease (%) | 110 (20) |
| Diabetes (%) | 47 (9) |
| Any therapy at the time of LOC (%) | 272 (50) |
| History of LOC: first episode (%) | 313 (58) |
| Recurrent LOCs: median number per patient (interquartile range) | 2 (2–4) |
| Interval between first and last episode – year (interquartile range) | 3 (1–8) |
| History of pre-syncope (%) | 109 (20) |
| Injuries related to fainting (%) | 138 (25) |
| Major injuries (fractures, brain concussion) (%) | 60 (11) |
| Minor injuries (bruises, etc.) (%) | 78 (14) |
| No warning at the onset of the attack (%) | 163 (30) |
| Circumstances just prior to the attacka | |
| Standing (%) | 363 (67) |
| Rest (no activity) (%) | 286 (53) |
| Any pre-disposing factors (%) | 474 (87) |
| Total patients attending the emergency room | 51 049 |
| Total patients with LOC attending the emergency room (%) | 541 (1.1) |
| Patients with LOC per hospital (mean±SD) | 49±12 |
| Time between LOC and arrival at emergency room <6 h (%) | 385 (71) |
| Median age (interquartile range) | 71 (48–81) |
| Male gender (%) | 289 (53) |
| Normal electrocardiogram (%) | 327 (60) |
| No structural heart disease (%) | 341 (63) |
| Comorbidities | |
| Hypertension (%) | 221 (41) |
| Any neurological disease (%) | 110 (20) |
| Diabetes (%) | 47 (9) |
| Any therapy at the time of LOC (%) | 272 (50) |
| History of LOC: first episode (%) | 313 (58) |
| Recurrent LOCs: median number per patient (interquartile range) | 2 (2–4) |
| Interval between first and last episode – year (interquartile range) | 3 (1–8) |
| History of pre-syncope (%) | 109 (20) |
| Injuries related to fainting (%) | 138 (25) |
| Major injuries (fractures, brain concussion) (%) | 60 (11) |
| Minor injuries (bruises, etc.) (%) | 78 (14) |
| No warning at the onset of the attack (%) | 163 (30) |
| Circumstances just prior to the attacka | |
| Standing (%) | 363 (67) |
| Rest (no activity) (%) | 286 (53) |
| Any pre-disposing factors (%) | 474 (87) |
LOC, loss of consciousness.
aSee definition in Table 2.1, Guidelines on Syncope, Europace 2004a; 6: 467–537.
Causes of loss of consciousness in 465 patients (according to the ESC classification)
| Causes of syncopes . | Initial evaluationa . | Investigations b . | Total . |
|---|---|---|---|
| Neurally mediated (reflex) (%) | 202 (43) | 107 (23) | 309 (66) |
| Vasovagal syncope | 101 (22) | 89 (19) | 190 (41) |
| Classical form: fear, pain, emotion, instrumentation | 82 (18) | – | |
| Classical form: prolonged standing and typical prodromal symptoms | 19 (4) | – | |
| Non-classical form: tilt-positive | – | 38 (8) | |
| Likely vasovagal (non-classical form) after exclusion of other causes and absence of heart disease | – | 51 (11) | |
| Carotid sinus syncope | 0 (0) | 18 (4) | 18 (4) |
| Situational syncopec | 71 (15) | – | 71 (15) |
| Single/rare syncopes, no heart disease | 30 (6) | – | 30 (6) |
| Orthostatic hypotension (%) | 36 (8) | 10 (2) | 46 (10) |
| Cardiac arrhythmias as primary cause (%) | 30 (6) | 23 (5) | 53 (11) |
| Sinus node dysfunction (including bradycardia/tachycardia syndrome) (%) | 5 (1) | 7 (1) | 12 (3) |
| Atrioventricular conduction system disease (%) | 15 (3) | 8 (2) | 23 (5) |
| Paroxysmal supraventricular tachycardias (%) | 8 (2) | 3 (1) | 11 (2) |
| Paroxysmal ventricular tachycardias (%) | 2 (0) | 5 (1) | 7 (1) |
| Structural cardiac or cardiopulmonary diseased (%) | 4 (1) | 17 (4) | 21 (5) |
| Cerebrovascular (%) | 0 (0) | 0 (0) | 0 (0) |
| Unknown (%) | – | – | 11 (2) |
| Causes of non-syncopal attacks (commonly misdiagnosed as syncope) (%) | – | 25 (6) | 25 (6) |
| Metabolic disorders (hypoglycaemia) | – | 1 (0) | 1 (0) |
| Epilepsy | – | 8 (2) | 8 (2) |
| Intoxication | – | 2 (0) | 2 (0) |
| Vertebro-basilar transient ischaemic attack — no. (%) | – | 4 (1) | 4 (1) |
| Falls — no. (%) | – | 6 (1) | 6 (1) |
| Psychogenic pseudo-syncope (%) | – | 4 (1) | 4 (1) |
| Causes of syncopes . | Initial evaluationa . | Investigations b . | Total . |
|---|---|---|---|
| Neurally mediated (reflex) (%) | 202 (43) | 107 (23) | 309 (66) |
| Vasovagal syncope | 101 (22) | 89 (19) | 190 (41) |
| Classical form: fear, pain, emotion, instrumentation | 82 (18) | – | |
| Classical form: prolonged standing and typical prodromal symptoms | 19 (4) | – | |
| Non-classical form: tilt-positive | – | 38 (8) | |
| Likely vasovagal (non-classical form) after exclusion of other causes and absence of heart disease | – | 51 (11) | |
| Carotid sinus syncope | 0 (0) | 18 (4) | 18 (4) |
| Situational syncopec | 71 (15) | – | 71 (15) |
| Single/rare syncopes, no heart disease | 30 (6) | – | 30 (6) |
| Orthostatic hypotension (%) | 36 (8) | 10 (2) | 46 (10) |
| Cardiac arrhythmias as primary cause (%) | 30 (6) | 23 (5) | 53 (11) |
| Sinus node dysfunction (including bradycardia/tachycardia syndrome) (%) | 5 (1) | 7 (1) | 12 (3) |
| Atrioventricular conduction system disease (%) | 15 (3) | 8 (2) | 23 (5) |
| Paroxysmal supraventricular tachycardias (%) | 8 (2) | 3 (1) | 11 (2) |
| Paroxysmal ventricular tachycardias (%) | 2 (0) | 5 (1) | 7 (1) |
| Structural cardiac or cardiopulmonary diseased (%) | 4 (1) | 17 (4) | 21 (5) |
| Cerebrovascular (%) | 0 (0) | 0 (0) | 0 (0) |
| Unknown (%) | – | – | 11 (2) |
| Causes of non-syncopal attacks (commonly misdiagnosed as syncope) (%) | – | 25 (6) | 25 (6) |
| Metabolic disorders (hypoglycaemia) | – | 1 (0) | 1 (0) |
| Epilepsy | – | 8 (2) | 8 (2) |
| Intoxication | – | 2 (0) | 2 (0) |
| Vertebro-basilar transient ischaemic attack — no. (%) | – | 4 (1) | 4 (1) |
| Falls — no. (%) | – | 6 (1) | 6 (1) |
| Psychogenic pseudo-syncope (%) | – | 4 (1) | 4 (1) |
aDiagnostic criteria on Initial Evaluation are those defined in the section ‘Recommendations: diagnostic criteria based on the initial evaluation’, page 2058 of the Guidelines on Syncope, Eur Heart J 2004; 25, 2054–2072.
bDiagnosis suspected on initial evaluation (n=147), confirmed by test. For definition, see Tables 3 and 4. Guidelines on Syncope, Eur Heart J 2004; 25, 2054–2072.
cSituational syncope included micturition (no. 23), gastrointestinal stimulation (swallowing, defecation, visceral pain) (no. 29), acute haemorrhage (no. 7), coughing (no. 3), post-prandial and typical prodromal symptoms (no. 8), and post-exercise and typical prodromal symptoms (no. 1).
dStructural cardiac or cardiopulmonary syncope included acute myocardial ischaemia (no. 11), aortic stenosis (no. 4); pulmonary embolism (no. 4); pulmonary hypertension (no. 1), and pericardial tamponade (no. 1).
Causes of loss of consciousness in 465 patients (according to the ESC classification)
| Causes of syncopes . | Initial evaluationa . | Investigations b . | Total . |
|---|---|---|---|
| Neurally mediated (reflex) (%) | 202 (43) | 107 (23) | 309 (66) |
| Vasovagal syncope | 101 (22) | 89 (19) | 190 (41) |
| Classical form: fear, pain, emotion, instrumentation | 82 (18) | – | |
| Classical form: prolonged standing and typical prodromal symptoms | 19 (4) | – | |
| Non-classical form: tilt-positive | – | 38 (8) | |
| Likely vasovagal (non-classical form) after exclusion of other causes and absence of heart disease | – | 51 (11) | |
| Carotid sinus syncope | 0 (0) | 18 (4) | 18 (4) |
| Situational syncopec | 71 (15) | – | 71 (15) |
| Single/rare syncopes, no heart disease | 30 (6) | – | 30 (6) |
| Orthostatic hypotension (%) | 36 (8) | 10 (2) | 46 (10) |
| Cardiac arrhythmias as primary cause (%) | 30 (6) | 23 (5) | 53 (11) |
| Sinus node dysfunction (including bradycardia/tachycardia syndrome) (%) | 5 (1) | 7 (1) | 12 (3) |
| Atrioventricular conduction system disease (%) | 15 (3) | 8 (2) | 23 (5) |
| Paroxysmal supraventricular tachycardias (%) | 8 (2) | 3 (1) | 11 (2) |
| Paroxysmal ventricular tachycardias (%) | 2 (0) | 5 (1) | 7 (1) |
| Structural cardiac or cardiopulmonary diseased (%) | 4 (1) | 17 (4) | 21 (5) |
| Cerebrovascular (%) | 0 (0) | 0 (0) | 0 (0) |
| Unknown (%) | – | – | 11 (2) |
| Causes of non-syncopal attacks (commonly misdiagnosed as syncope) (%) | – | 25 (6) | 25 (6) |
| Metabolic disorders (hypoglycaemia) | – | 1 (0) | 1 (0) |
| Epilepsy | – | 8 (2) | 8 (2) |
| Intoxication | – | 2 (0) | 2 (0) |
| Vertebro-basilar transient ischaemic attack — no. (%) | – | 4 (1) | 4 (1) |
| Falls — no. (%) | – | 6 (1) | 6 (1) |
| Psychogenic pseudo-syncope (%) | – | 4 (1) | 4 (1) |
| Causes of syncopes . | Initial evaluationa . | Investigations b . | Total . |
|---|---|---|---|
| Neurally mediated (reflex) (%) | 202 (43) | 107 (23) | 309 (66) |
| Vasovagal syncope | 101 (22) | 89 (19) | 190 (41) |
| Classical form: fear, pain, emotion, instrumentation | 82 (18) | – | |
| Classical form: prolonged standing and typical prodromal symptoms | 19 (4) | – | |
| Non-classical form: tilt-positive | – | 38 (8) | |
| Likely vasovagal (non-classical form) after exclusion of other causes and absence of heart disease | – | 51 (11) | |
| Carotid sinus syncope | 0 (0) | 18 (4) | 18 (4) |
| Situational syncopec | 71 (15) | – | 71 (15) |
| Single/rare syncopes, no heart disease | 30 (6) | – | 30 (6) |
| Orthostatic hypotension (%) | 36 (8) | 10 (2) | 46 (10) |
| Cardiac arrhythmias as primary cause (%) | 30 (6) | 23 (5) | 53 (11) |
| Sinus node dysfunction (including bradycardia/tachycardia syndrome) (%) | 5 (1) | 7 (1) | 12 (3) |
| Atrioventricular conduction system disease (%) | 15 (3) | 8 (2) | 23 (5) |
| Paroxysmal supraventricular tachycardias (%) | 8 (2) | 3 (1) | 11 (2) |
| Paroxysmal ventricular tachycardias (%) | 2 (0) | 5 (1) | 7 (1) |
| Structural cardiac or cardiopulmonary diseased (%) | 4 (1) | 17 (4) | 21 (5) |
| Cerebrovascular (%) | 0 (0) | 0 (0) | 0 (0) |
| Unknown (%) | – | – | 11 (2) |
| Causes of non-syncopal attacks (commonly misdiagnosed as syncope) (%) | – | 25 (6) | 25 (6) |
| Metabolic disorders (hypoglycaemia) | – | 1 (0) | 1 (0) |
| Epilepsy | – | 8 (2) | 8 (2) |
| Intoxication | – | 2 (0) | 2 (0) |
| Vertebro-basilar transient ischaemic attack — no. (%) | – | 4 (1) | 4 (1) |
| Falls — no. (%) | – | 6 (1) | 6 (1) |
| Psychogenic pseudo-syncope (%) | – | 4 (1) | 4 (1) |
aDiagnostic criteria on Initial Evaluation are those defined in the section ‘Recommendations: diagnostic criteria based on the initial evaluation’, page 2058 of the Guidelines on Syncope, Eur Heart J 2004; 25, 2054–2072.
bDiagnosis suspected on initial evaluation (n=147), confirmed by test. For definition, see Tables 3 and 4. Guidelines on Syncope, Eur Heart J 2004; 25, 2054–2072.
cSituational syncope included micturition (no. 23), gastrointestinal stimulation (swallowing, defecation, visceral pain) (no. 29), acute haemorrhage (no. 7), coughing (no. 3), post-prandial and typical prodromal symptoms (no. 8), and post-exercise and typical prodromal symptoms (no. 1).
dStructural cardiac or cardiopulmonary syncope included acute myocardial ischaemia (no. 11), aortic stenosis (no. 4); pulmonary embolism (no. 4); pulmonary hypertension (no. 1), and pericardial tamponade (no. 1).
Tests: diagnostic yield in 465 patients
| . | Diagnostic purposes . | Trauma or comorbidities or routine . | Total . | |
|---|---|---|---|---|
| . | Appropriatea . | Of which diagnostica . | . | . |
| Electrocardiography (%) | 465 (100) | 34 (7) | 0 (0) | 465 (100) |
| Basic laboratory tests (%) | 52 (11) | 21 (40)b | 114 (25) | 166 (36) |
| Echocardiography (%) | 49 (11) | 5 (10)c | 25 (5) | 74 (16) |
| Tilt testing (%) | 76 (16) | 46 (61) | 2 (0) | 78 (17) |
| Carotid sinus massage (%) | 65 (14) | 18 (28) | 4 (1) | 69 (15) |
| 24 h blood pressure monitoring (%) | 1 (0) | 1 (100) | 0 (0) | 1 (0) |
| ATP test (%) | 1 (0) | 0 (0) | 0 (0) | 1 (0) |
| In-hospital ECG monitoring (%) | 21 (5) | 13 (62) | 0 (0) | 21 (5) |
| 24 h Holter monitoring (%) | 12 (3) | 3 (25) | 8 (1) | 20 (4) |
| External loop recorder (%) | 4 (1) | 2 (50) | 0 (0) | 4 (1) |
| Exercise test (%) | 10 (2) | 3 (30)d | 5 (1) | 15 (3) |
| Electrophysiological study (%) | 15 (3) | 5 (33)e | 1 (0) | 16 (3) |
| Coronary angiography (%) | 8 (2) | 5 (62) | 1 (0) | 9 (2) |
| Pulmonary computed tomography/Scintigraphy (%) | 5 (1) | 4 (80) | 0 (0) | 5 (1) |
| Electroencephalography (%) | 16 (3) | 5 (31) | 7 (2) | 23 (5) |
| Brain computed tomography (%) | 16 (3) | 3 (19) | 51 (11) | 67 (14) |
| Brain magnetic resonance imaging (%) | 6 (1) | 2 (33) | 3 (1) | 9 (2) |
| Carotid echo-Doppler (%) | 0 (0) | 0 (0) | 26 (6) | 26 (6) |
| Chest X-ray (%) | 0 (0) | 0 (0) | 51 (11) | 51 (11) |
| Other X-ray (%) | 0 (0) | 0 (0) | 22 (5) | 22 (5) |
| Abdominal ultrasound examination (%) | 0 (0) | 0 (0) | 11 (2) | 11 (2) |
| Gastroscopy (%) | 1 (0) | 1 (100)f | 2 (1) | 3 (1) |
| Other echographies (%) | 0 (0) | 0 (0) | 3 (1) | 3 (1) |
| Total number of tests | 823 | 171 | 346 | 1156 |
| Mean no. of tests per patient (±SD) | 1.8±1.2 | 2.5±1.8 | ||
| . | Diagnostic purposes . | Trauma or comorbidities or routine . | Total . | |
|---|---|---|---|---|
| . | Appropriatea . | Of which diagnostica . | . | . |
| Electrocardiography (%) | 465 (100) | 34 (7) | 0 (0) | 465 (100) |
| Basic laboratory tests (%) | 52 (11) | 21 (40)b | 114 (25) | 166 (36) |
| Echocardiography (%) | 49 (11) | 5 (10)c | 25 (5) | 74 (16) |
| Tilt testing (%) | 76 (16) | 46 (61) | 2 (0) | 78 (17) |
| Carotid sinus massage (%) | 65 (14) | 18 (28) | 4 (1) | 69 (15) |
| 24 h blood pressure monitoring (%) | 1 (0) | 1 (100) | 0 (0) | 1 (0) |
| ATP test (%) | 1 (0) | 0 (0) | 0 (0) | 1 (0) |
| In-hospital ECG monitoring (%) | 21 (5) | 13 (62) | 0 (0) | 21 (5) |
| 24 h Holter monitoring (%) | 12 (3) | 3 (25) | 8 (1) | 20 (4) |
| External loop recorder (%) | 4 (1) | 2 (50) | 0 (0) | 4 (1) |
| Exercise test (%) | 10 (2) | 3 (30)d | 5 (1) | 15 (3) |
| Electrophysiological study (%) | 15 (3) | 5 (33)e | 1 (0) | 16 (3) |
| Coronary angiography (%) | 8 (2) | 5 (62) | 1 (0) | 9 (2) |
| Pulmonary computed tomography/Scintigraphy (%) | 5 (1) | 4 (80) | 0 (0) | 5 (1) |
| Electroencephalography (%) | 16 (3) | 5 (31) | 7 (2) | 23 (5) |
| Brain computed tomography (%) | 16 (3) | 3 (19) | 51 (11) | 67 (14) |
| Brain magnetic resonance imaging (%) | 6 (1) | 2 (33) | 3 (1) | 9 (2) |
| Carotid echo-Doppler (%) | 0 (0) | 0 (0) | 26 (6) | 26 (6) |
| Chest X-ray (%) | 0 (0) | 0 (0) | 51 (11) | 51 (11) |
| Other X-ray (%) | 0 (0) | 0 (0) | 22 (5) | 22 (5) |
| Abdominal ultrasound examination (%) | 0 (0) | 0 (0) | 11 (2) | 11 (2) |
| Gastroscopy (%) | 1 (0) | 1 (100)f | 2 (1) | 3 (1) |
| Other echographies (%) | 0 (0) | 0 (0) | 3 (1) | 3 (1) |
| Total number of tests | 823 | 171 | 346 | 1156 |
| Mean no. of tests per patient (±SD) | 1.8±1.2 | 2.5±1.8 | ||
aAccording to recommendations in Part 2, Guidelines on Syncope, Europace 2004; 6: 467–537.
bDiagnosis: anaemia (no. 13), hypoglycemia (no. 1), intoxication (no. 2), myocardial necrosis (no. 3), embolism (no. 3).
cDiagnosis: aortic stenosis (no. 4), pericardial tamponade (no. 1).
dDiagnosis: AV block (no. 1), hypotension (no. 2).
eDiagnosis: AV block (no. 2), supraventricular tachycardia (no. 3), ventricular tachycardia (no. 1).
fDiagnosis: bleeding.
Tests: diagnostic yield in 465 patients
| . | Diagnostic purposes . | Trauma or comorbidities or routine . | Total . | |
|---|---|---|---|---|
| . | Appropriatea . | Of which diagnostica . | . | . |
| Electrocardiography (%) | 465 (100) | 34 (7) | 0 (0) | 465 (100) |
| Basic laboratory tests (%) | 52 (11) | 21 (40)b | 114 (25) | 166 (36) |
| Echocardiography (%) | 49 (11) | 5 (10)c | 25 (5) | 74 (16) |
| Tilt testing (%) | 76 (16) | 46 (61) | 2 (0) | 78 (17) |
| Carotid sinus massage (%) | 65 (14) | 18 (28) | 4 (1) | 69 (15) |
| 24 h blood pressure monitoring (%) | 1 (0) | 1 (100) | 0 (0) | 1 (0) |
| ATP test (%) | 1 (0) | 0 (0) | 0 (0) | 1 (0) |
| In-hospital ECG monitoring (%) | 21 (5) | 13 (62) | 0 (0) | 21 (5) |
| 24 h Holter monitoring (%) | 12 (3) | 3 (25) | 8 (1) | 20 (4) |
| External loop recorder (%) | 4 (1) | 2 (50) | 0 (0) | 4 (1) |
| Exercise test (%) | 10 (2) | 3 (30)d | 5 (1) | 15 (3) |
| Electrophysiological study (%) | 15 (3) | 5 (33)e | 1 (0) | 16 (3) |
| Coronary angiography (%) | 8 (2) | 5 (62) | 1 (0) | 9 (2) |
| Pulmonary computed tomography/Scintigraphy (%) | 5 (1) | 4 (80) | 0 (0) | 5 (1) |
| Electroencephalography (%) | 16 (3) | 5 (31) | 7 (2) | 23 (5) |
| Brain computed tomography (%) | 16 (3) | 3 (19) | 51 (11) | 67 (14) |
| Brain magnetic resonance imaging (%) | 6 (1) | 2 (33) | 3 (1) | 9 (2) |
| Carotid echo-Doppler (%) | 0 (0) | 0 (0) | 26 (6) | 26 (6) |
| Chest X-ray (%) | 0 (0) | 0 (0) | 51 (11) | 51 (11) |
| Other X-ray (%) | 0 (0) | 0 (0) | 22 (5) | 22 (5) |
| Abdominal ultrasound examination (%) | 0 (0) | 0 (0) | 11 (2) | 11 (2) |
| Gastroscopy (%) | 1 (0) | 1 (100)f | 2 (1) | 3 (1) |
| Other echographies (%) | 0 (0) | 0 (0) | 3 (1) | 3 (1) |
| Total number of tests | 823 | 171 | 346 | 1156 |
| Mean no. of tests per patient (±SD) | 1.8±1.2 | 2.5±1.8 | ||
| . | Diagnostic purposes . | Trauma or comorbidities or routine . | Total . | |
|---|---|---|---|---|
| . | Appropriatea . | Of which diagnostica . | . | . |
| Electrocardiography (%) | 465 (100) | 34 (7) | 0 (0) | 465 (100) |
| Basic laboratory tests (%) | 52 (11) | 21 (40)b | 114 (25) | 166 (36) |
| Echocardiography (%) | 49 (11) | 5 (10)c | 25 (5) | 74 (16) |
| Tilt testing (%) | 76 (16) | 46 (61) | 2 (0) | 78 (17) |
| Carotid sinus massage (%) | 65 (14) | 18 (28) | 4 (1) | 69 (15) |
| 24 h blood pressure monitoring (%) | 1 (0) | 1 (100) | 0 (0) | 1 (0) |
| ATP test (%) | 1 (0) | 0 (0) | 0 (0) | 1 (0) |
| In-hospital ECG monitoring (%) | 21 (5) | 13 (62) | 0 (0) | 21 (5) |
| 24 h Holter monitoring (%) | 12 (3) | 3 (25) | 8 (1) | 20 (4) |
| External loop recorder (%) | 4 (1) | 2 (50) | 0 (0) | 4 (1) |
| Exercise test (%) | 10 (2) | 3 (30)d | 5 (1) | 15 (3) |
| Electrophysiological study (%) | 15 (3) | 5 (33)e | 1 (0) | 16 (3) |
| Coronary angiography (%) | 8 (2) | 5 (62) | 1 (0) | 9 (2) |
| Pulmonary computed tomography/Scintigraphy (%) | 5 (1) | 4 (80) | 0 (0) | 5 (1) |
| Electroencephalography (%) | 16 (3) | 5 (31) | 7 (2) | 23 (5) |
| Brain computed tomography (%) | 16 (3) | 3 (19) | 51 (11) | 67 (14) |
| Brain magnetic resonance imaging (%) | 6 (1) | 2 (33) | 3 (1) | 9 (2) |
| Carotid echo-Doppler (%) | 0 (0) | 0 (0) | 26 (6) | 26 (6) |
| Chest X-ray (%) | 0 (0) | 0 (0) | 51 (11) | 51 (11) |
| Other X-ray (%) | 0 (0) | 0 (0) | 22 (5) | 22 (5) |
| Abdominal ultrasound examination (%) | 0 (0) | 0 (0) | 11 (2) | 11 (2) |
| Gastroscopy (%) | 1 (0) | 1 (100)f | 2 (1) | 3 (1) |
| Other echographies (%) | 0 (0) | 0 (0) | 3 (1) | 3 (1) |
| Total number of tests | 823 | 171 | 346 | 1156 |
| Mean no. of tests per patient (±SD) | 1.8±1.2 | 2.5±1.8 | ||
aAccording to recommendations in Part 2, Guidelines on Syncope, Europace 2004; 6: 467–537.
bDiagnosis: anaemia (no. 13), hypoglycemia (no. 1), intoxication (no. 2), myocardial necrosis (no. 3), embolism (no. 3).
cDiagnosis: aortic stenosis (no. 4), pericardial tamponade (no. 1).
dDiagnosis: AV block (no. 1), hypotension (no. 2).
eDiagnosis: AV block (no. 2), supraventricular tachycardia (no. 3), ventricular tachycardia (no. 1).
fDiagnosis: bleeding.
Treatment and measures prescribed
| Neurally mediated (reflex)a | 309 |
| Education, reassurance, and avoidance of triggers alone (%) | 260 (84) |
| Modification or discontinuation of hypotensive drugs (%) | 37 (12) |
| Physical manoeuvres (tilt training or counterpressure manoeuvres) (%) | 5 (2) |
| Vasoconstrictor drugs (%) | 2 (1) |
| Pacemaker (%) | 7 (2) |
| Orthostatic hypotensiona | 46 |
| Education and avoidance of triggers (%) | 36 (78) |
| Modification or discontinuation of hypotensive drugs (%) | 28 (61) |
| Physical manoeuvres (counterpressure manoeuvres, elastic stockings) (%) | 6 (13) |
| Volume expansion (%) | 17 (37) |
| Vasoconstrictor drugs (%) | 6 (13) |
| Cardiac arrhythmias as primary causea | 53 |
| Cardiac pacing (%) | 36 (68) |
| Antiarrhythmic drug therapy (%) | 11 (21) |
| Cardioverter-defibrillator implantation (%) | 5 (9) |
| Catheter ablation (%) | 3 (9) |
| Structural cardiac or cardiopulmonary disease | 21 |
| Coronary revascularization (angioplasty, by-pass) (%) | 7 (33) |
| Valvular surgery (%) | 4 (19) |
| Drug therapy (%) | 3 (14) |
| No specific therapy (%) | 7 (33) |
| Syncope of unknown origin | 11 |
| Implantable loop recorder (%) | 3 (27) |
| No specific therapy (%) | 8 (73) |
| Non-syncopal attacks | 25 |
| Anti-epileptic drugs (%) | 8 (31) |
| Antidepressant drugs (%) | 3 (12) |
| No specific therapy (%) | 14 (45) |
| Neurally mediated (reflex)a | 309 |
| Education, reassurance, and avoidance of triggers alone (%) | 260 (84) |
| Modification or discontinuation of hypotensive drugs (%) | 37 (12) |
| Physical manoeuvres (tilt training or counterpressure manoeuvres) (%) | 5 (2) |
| Vasoconstrictor drugs (%) | 2 (1) |
| Pacemaker (%) | 7 (2) |
| Orthostatic hypotensiona | 46 |
| Education and avoidance of triggers (%) | 36 (78) |
| Modification or discontinuation of hypotensive drugs (%) | 28 (61) |
| Physical manoeuvres (counterpressure manoeuvres, elastic stockings) (%) | 6 (13) |
| Volume expansion (%) | 17 (37) |
| Vasoconstrictor drugs (%) | 6 (13) |
| Cardiac arrhythmias as primary causea | 53 |
| Cardiac pacing (%) | 36 (68) |
| Antiarrhythmic drug therapy (%) | 11 (21) |
| Cardioverter-defibrillator implantation (%) | 5 (9) |
| Catheter ablation (%) | 3 (9) |
| Structural cardiac or cardiopulmonary disease | 21 |
| Coronary revascularization (angioplasty, by-pass) (%) | 7 (33) |
| Valvular surgery (%) | 4 (19) |
| Drug therapy (%) | 3 (14) |
| No specific therapy (%) | 7 (33) |
| Syncope of unknown origin | 11 |
| Implantable loop recorder (%) | 3 (27) |
| No specific therapy (%) | 8 (73) |
| Non-syncopal attacks | 25 |
| Anti-epileptic drugs (%) | 8 (31) |
| Antidepressant drugs (%) | 3 (12) |
| No specific therapy (%) | 14 (45) |
aMore than one treatment was assigned to some patients of this group.
Treatment and measures prescribed
| Neurally mediated (reflex)a | 309 |
| Education, reassurance, and avoidance of triggers alone (%) | 260 (84) |
| Modification or discontinuation of hypotensive drugs (%) | 37 (12) |
| Physical manoeuvres (tilt training or counterpressure manoeuvres) (%) | 5 (2) |
| Vasoconstrictor drugs (%) | 2 (1) |
| Pacemaker (%) | 7 (2) |
| Orthostatic hypotensiona | 46 |
| Education and avoidance of triggers (%) | 36 (78) |
| Modification or discontinuation of hypotensive drugs (%) | 28 (61) |
| Physical manoeuvres (counterpressure manoeuvres, elastic stockings) (%) | 6 (13) |
| Volume expansion (%) | 17 (37) |
| Vasoconstrictor drugs (%) | 6 (13) |
| Cardiac arrhythmias as primary causea | 53 |
| Cardiac pacing (%) | 36 (68) |
| Antiarrhythmic drug therapy (%) | 11 (21) |
| Cardioverter-defibrillator implantation (%) | 5 (9) |
| Catheter ablation (%) | 3 (9) |
| Structural cardiac or cardiopulmonary disease | 21 |
| Coronary revascularization (angioplasty, by-pass) (%) | 7 (33) |
| Valvular surgery (%) | 4 (19) |
| Drug therapy (%) | 3 (14) |
| No specific therapy (%) | 7 (33) |
| Syncope of unknown origin | 11 |
| Implantable loop recorder (%) | 3 (27) |
| No specific therapy (%) | 8 (73) |
| Non-syncopal attacks | 25 |
| Anti-epileptic drugs (%) | 8 (31) |
| Antidepressant drugs (%) | 3 (12) |
| No specific therapy (%) | 14 (45) |
| Neurally mediated (reflex)a | 309 |
| Education, reassurance, and avoidance of triggers alone (%) | 260 (84) |
| Modification or discontinuation of hypotensive drugs (%) | 37 (12) |
| Physical manoeuvres (tilt training or counterpressure manoeuvres) (%) | 5 (2) |
| Vasoconstrictor drugs (%) | 2 (1) |
| Pacemaker (%) | 7 (2) |
| Orthostatic hypotensiona | 46 |
| Education and avoidance of triggers (%) | 36 (78) |
| Modification or discontinuation of hypotensive drugs (%) | 28 (61) |
| Physical manoeuvres (counterpressure manoeuvres, elastic stockings) (%) | 6 (13) |
| Volume expansion (%) | 17 (37) |
| Vasoconstrictor drugs (%) | 6 (13) |
| Cardiac arrhythmias as primary causea | 53 |
| Cardiac pacing (%) | 36 (68) |
| Antiarrhythmic drug therapy (%) | 11 (21) |
| Cardioverter-defibrillator implantation (%) | 5 (9) |
| Catheter ablation (%) | 3 (9) |
| Structural cardiac or cardiopulmonary disease | 21 |
| Coronary revascularization (angioplasty, by-pass) (%) | 7 (33) |
| Valvular surgery (%) | 4 (19) |
| Drug therapy (%) | 3 (14) |
| No specific therapy (%) | 7 (33) |
| Syncope of unknown origin | 11 |
| Implantable loop recorder (%) | 3 (27) |
| No specific therapy (%) | 8 (73) |
| Non-syncopal attacks | 25 |
| Anti-epileptic drugs (%) | 8 (31) |
| Antidepressant drugs (%) | 3 (12) |
| No specific therapy (%) | 14 (45) |
aMore than one treatment was assigned to some patients of this group.
References
Kenny RA, O'Shea D, Walker HF. Impact of a dedicated syncope and falls facility for older adults on emergency beds.
Ammirati F, Colivicchi F, Minardi G, De Lio L, Terranova A, Scaffidi G, Rapino S, Proietti F, Bianchi C, Uguccioni M, Carunchio A, Azzolini P, Neri R, Accogli S, Sunseri L, Orazi S, Mariani M, Fraioli R, Calcagno S, De Luca F, Santini M. Hospital management of syncope: the OESIL study.
Disertori M, Brignole M, Menozzi C, Raviele A, Rizzon P, Santini M, Proclemer A, Tomasi C, Rossillo A, Taddei F, Scivales A, Migliorini R, De Santo T. Management of syncope referred for emergency to general hospitals.
Farwell DJ, Sulke AN. Does the use of a syncope diagnostic protocol improve the investigation and management of syncope?
Blanc JJ, L'Her C, Touiza A, Garo B, L'Her E, Mansourati J. Prospective evaluation and outcome of patients admitted for syncope over 1 year period.
Ammirati F, Colivicchi F, Santini M. Diagnosing syncope in the clinical practice. Implementation of a simplified diagnostic algorithm in a multicentre prospective trial – the OESIL 2 study (Osservatorio Epidemiologico della Sincope nel Lazio).
Del Greco M, Cozzio S, Scillieri M, Caprari F, Scivales A, Disertori M. The ECSIT study (Epidemiology and Costs of Syncope in Trento). Diagnostic pathway of syncope and analysis of the impact of guidelines in a district general hospital.
Sarasin F, Louis-Simonet M, Carballo D, Slama S, Rajeswaran A, Metzger JT, Lovis C, Unger PF, Junod AF. Prospective evaluation of patients with syncope: a population-based study.
Brignole M, Disertori M, Menozzi C, Raviele A, Alboni P, Pitzalis MV, Delise P, Puggioni E, Del Greco M, Malavasi V, Lunati M, Pepe M, Fabrizi D. The management of syncope referred for emergency to general hospitals with and without syncope unit facility.
Shen W, Decker W, Smars P, Goyal DG, Walker AE, Hodge DO, Trusty JM, Brekke KM, Jahangir A, Brady PA, Munger TM, Gersh BJ, Hammill SC, Frye RL. Syncope evaluation in the emergency department study (SEEDS): a multidisciplinary approach to syncope management.
Croci F, Brignole M, Alboni P, Menozzi C, Raviele A, Del Rosso A, Dinelli M, Solano A, Bottoni N, Donateo P. The application of a standardized strategy of evaluation in patients with syncope referred to three syncope units.
Linzer M, Yang EH, Estes NA III, Wang P, Vorperian VR, Kapoor WN. Clinical Efficacy Assessment Project of the American College of Physicians. Diagnosing syncope, part 1: value of history, physical examination, and electrocardiography.
Linzer M, Yang EH, Estes NA III, Wang P, Vorperian VR, Kapoor WN. Clinical Efficacy Assessment Project of the American College of Physicians. Diagnosing syncope, part 2: unexplained syncope.
American College of Emergency Physicians. Clinical policy: critical issues in the evaluation and management of patients presenting with syncope.
Brignole M, Alboni P, Benditt D, Bergfeldt L, Blanc JJ, Bloch Thomsen PE, van Dijk JG, Fitzpatrick A, Hohnloser S, Janousek J, Kapoor W, Kenny RA, Kulakowski P, Masotti G, Moya A, Raviele A, Sutton R, Theodorakis G, Ungar A, Wieling W. Guidelines on management (diagnosis and treatment) of syncope – Update 2004.
Brignole M, Alboni P, Benditt D, Bergfeldt L, Blanc JJ, Bloch Thomsen PE, van Dijk JG, Fitzpatrick A, Hohnloser S, Janousek J, Kapoor W, Kenny RA, Kulakowski P, Masotti G, Moya A, Raviele A, Sutton R, Theodorakis G, Ungar A, Wieling W. Guidelines on management (diagnosis and treatment) of syncope – Update 2004 - executive summary and recommendations.
Soteriades E, Evans J, Larson M, Chen MH, Chen L, Benjamin EJ, Levy D. Incidence and prognosis of syncope.
Martin GJ, Adams SL, Martin HG, Mathews J, Zull D, Scanlon PJ. Prospective evaluation of syncope.
Eagle KA, Black HR. The impact of diagnostic tests in evaluating patients with syncope.
Ben-Chetrit E, Flugeiman M, Eliakim M. Syncope: a retrospective study of 101 hospitalized patients.
Day SC, Cook EF, Funkenstein H, Goldma L. Evaluation and outcome of emergency room patients with transient loss of consciousness.
Oh JH. Hanusa BH. Kapoor WN. Do symptoms predict cardiac arrhythmias and mortality in patients with syncope?
Kapoor W, Karpf M, Wieand S, Peterson JR, Levey GS. A prospective evaluation and follow-up of patients with syncope.