Abstract
BACKGROUND: There are no proven, comprehensive treatments in primary care for patients with medically unexplained symptoms (MUS) even though these patients have high levels of psychosocial distress, medical disability, costs, and utilization. Despite extensive care, these common patients often become worse.
OBJECTIVE: We sought to identify an effective, research-based treatment that can be conducted by primary care personnel.
DESIGN: We used our own experiences and files, consulted with experts, and conducted an extensive review of the literature to identify two things: 1) effective treatments from randomized controlled trials for MUS patients in primary care and in specialty settings; and 2) any type of treatment study in a related area that might inform primary care treatment, for example, depression, provider-patient relationship.
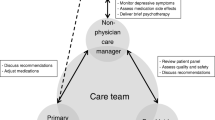
MAIN RESULTS: We developed a multidimensional treatment plan by integrating several areas of the literature: collaborative/stepped care, cognitive-behavioral treatment, and the provider-patient relationship. The treatment is designed for primary care personnel (physicians, physician assistants, nurse practitioners) and deployed intensively at the outset; visit intervals are progressively increased as stability and improvement occur.
CONCLUSION: Providing a comprehensive treatment plan for chronic, high-utilizing MUS patients removes one barrier to treating this common problem effectively in primary care by primary care personnel.
Similar content being viewed by others
References
Lipowski ZJ. Somatization: the concept and its clinical application. Am J Psychiatry. 1988;145:1358–68.
American Psychiatric Association. Diagnostic and Statistical Manual of Mental Disorders, 4th ed. Washington, DC: American Psychiatric Association; 1994.
Deyo RA. Pain and public policy. N Engl J Med. 2000;342:1211–3.
Cherkin D, Deyo RA. Nonsurgical hospitalization for low back pain: is it necessary? Spine. 1993;18:1728–35.
Hoffman RM, Wheeler KJ, Deyo RA. Surgery for herniated lumbar discs: a literature synthesis. J Gen Intern Med. 1993;8:487–96.
Deyo RA, Ciol MA, Cherkin DC, Loeser JD, Bigos SJ. Lumbar spinal fusion: a cohort study of complications, reoperations, and resource use in the Medicare population. Spine. 1993;1:1463–70.
Fink P. Surgery and medial treatment in persistent somatizing patients. J Psychosom Res. 1992;36:439–47.
Bass C, Benjamin S. The management of chronic somatization. Br J Psychiatry. 1993;162:472–80.
Lightfoot RW Jr, Luft BJ, Rahn DW, et al. Empiric parenteral antibiotic treatment of patients with fibromyalgia and fatigue and a positive serologic result for Lyme disease. Ann Intern Med. 1993;119:503–9.
Escobar JI, Waitzkin H, Silver RC, Gara M, Holman A. Abridged somatization: a study in primary care. Psychosom Med. 1998;60:466–72.
Bass C, Murphy M. Somatisation disorder in a British teaching hospital. Br J Clin Pract. 1991;45:237–44.
deGruy F, Columbia L, Dickinson P. Somatization disorder in a family practice. J Fam Pract. 1987;25:45–51.
deGruy F, Crider J, Hashimi DK, Dickinson P, Mullins HC, Troncale J. Somatization disorder in a university hospital. J Fam Pract. 1987;25:579–84.
Kroenke K, Mangelsdorff AD. Common symptoms in ambulatory care: incidence, evaluation, therapy, and outcome. Am J Med. 1989;86:262–6.
Barsky AJ, Borus JF. Somatization and medicalization in the era of managed care. JAMA. 1995;274:1931–4.
Katon WJ, Walker EA. Medically unexplained symptoms in primary care. J Clin Psychiatry. 1998;59(suppl 20):15–21.
Culpan R, Davies B. Psychiatric illness at a medical and a surgical outpatient clinic. Compr Psychiatry. 1960;1:228–35.
Hilkevitch A. Psychiatric disturbances in outpatients of a general medical outpatient clinic. Int J Neuropsychiatry. 1965;1:372–5.
Escobar JI, Swartz M, Rubio-Stipec M, Manu P. Medically unexplained symptoms: distribution, risk factors, and comorbidity. In: Kirmayer LJ, Robbins JM, eds. Current Concepts of Somatization: Research and Clinical Perspectives. Washington, DC: American Psychiatric Press, Inc.; 1991:63–78.
Escobar JI, Canino G. Unexplained physical complaints: psychopathology and epidemiological correlates. Br J Psychiatry. 1989;154:24–7.
Escobar JI, Golding JM, Hough RL, Karno M, Burnam AM, Wells KB. Somatization in the community: relationship to disability and use of services. Am J Public Health. 1987;77:837–40.
Escobar JI, Burnam MA, Karno M, Forsythe A, Golding JM. Somatization in the community. Arch Gen Psychiatry. 1987;44:713–8.
Simon GE. Psychiatric disorder and functional somatic symptoms as predictors of health care use. Psychiatr Med. 1992;10:49–59.
Katon W, von Korff M, Lin E, et al. Distressed high utilizers of medical care: DSM-III-R diagnoses and treatment needs. Gen Hosp Psychiatry. 1990;12:355–62.
Smith GR Jr. The course of somatization and its effects on utilization of health care resources. Psychosomatics. 1994;35:263–7.
Raine R, Haines A, Sensky T, Hutchings A, Larkin K, Black N. Systematic review of mental health interventions for patients with common somatic symptoms: can research evidence from secondary care be extrapolated to primary care? BMJ. 2002;325:1–11.
Shepherd M. Primary care psychiatry. Health services research is not enough. Br J Psychiatry. 1995;166:1–3.
Rost KM, Smith GR Jr. Improving effectiveness of routine care for somatization. J Psychosom Res. 1997;43:463–5.
Sharpe M, Carson A. Unexplained somatic symptoms, functional syndromes, and somatization: do we need a paradigm shift? Ann Intern Med. 2001;134:926–30.
Barsky AJ. The patient with hypochondriasis. N Engl J Med. 2001;345:1395–9.
Smith GR Jr, Monson RA, Ray DC. Psychiatric consultation in somatization disorder. N Engl J Med. 1986;314:1407–13.
Smith GR Jr. Effectiveness of treatment for somatoform disorder patients. Psychiatr Med. 1991;9:545–58.
Smith GR Jr, Rost K, Kashner TM. A trial of the effect of a standardized psychiatric consultation on health outcomes and costs in somatizing patients. Arch Gen Psychiatry. 1995;52:238–43.
Kashner TM, Rost K, Smith GR, Lewis S. An analysis of panel data-the impact of a psychiatric consultation letter on the expenditures and outcomes of care for patients with somatization disorder. Med Care. 1992;30:811–21.
Rost K, Kashner TM, Smith GR Jr. Effectiveness of psychiatric intervention with somatization disorder patients: improved outcomes at reduced costs. Gen Hosp Psychiatry. 1994;16:381–7.
Kashner TM, Rost K, Cohen B, Anderson MA, Smith GR Jr. Enhancing the health of somatization disorder patients: effectiveness of short term group therapy. Psychosomatics. 1995;36:462–70.
Andrews G, Hadzi-Pavlovic D, Christensen H, Mattick R. Views of practicing psychiatrists on the treatment of anxiety and somatoform disorders. Am J Psychiatry. 1987;144:1331–4.
Kellner R. Treatment approaches to somatizing and hypochondriacal patients. In: Kirmayer LJ, Robbins JM, eds. Current Concepts of Somatization: Research and Clinical Perspectives. Washington, DC: American Psychiatric Press, Inc.; 1991:159–80.
Kellner R. Psychotherapeutic strategies in hypochondriasis: a clinical study. Am J Psychother. 1982;36:146–57.
Sanders D, Bass C, Mayou RA, Goodwin S, Bryant BM, Tyndel S. Non-cardiac chest pain: why was a brief intervention apparently ineffective? Psychol Med. 1997;27:1033–40.
McCarberg B, Wolf J. Chronic pain management in a health maintenance organization. Clin J Pain. 1999;15:50–7.
Cutler RB, Fishbain DA, Rosomoff HL, Abdel-Maty E, Khalil TM, Rosomoff RS. Does nonsurgical pain center treatment of chronic pain return patients to work? A review and meta-analysis of the literature. Spine. 1994;19:643–52.
Peters J, Large RG, Elkind G. Follow-up results from a randomised controlled trial evaluating in- and outpatient pain management programmes. Pain. 1992;50:41–50.
Sharpe M, Peveler R, Mayou R. The psychological treatment of patients with functional somatic symptoms: a practical guide. J Psychosom Res. 1992;36:515–29.
Klimes I, Mayou RA, Pearce MJ, Coles L, Fagg JR. Psychological treatment for atypical noncardiac chest pain: a controlled evaluation. Psychol Med. 1990;20:605–11.
Sharpe M, Hawton K, Simkin S, et al. Cognitive behaviour therapy for the chronic fatigue syndrome: a randomized controlled trial. BMJ. 1996;312:22–6.
Warwick HMC, Clark DM, Cobb AM, Salkovskis PM. A controlled trial of cognitive-behavioural treatment of hypchondriasis. Br J Psychiatry. 1996;169:189–95.
Katon W, von Korff M, Lin E, et al. Collaborative management to achieve treatment guidelines: impact on depression in primary care. JAMA. 1995;273:1026–31.
Lin E, Katon W, Simon G, et al. Achieving guidelines for the treatment of depression in primary care: is physician education enough? Med Care. 1997;35:831–42.
von Korff M, Ormel J, Katon W, Lin EHB. Disability and depression among high utilizers of health care—a longitudinal analysis. Arch Gen Psychiatry. 1992;49:91–100.
Katon W, von Korff M, Lin E, et al. A randomized trial of psychiatric consultation with distressed high utilizers. Gen Hosp Psychiatry. 1992;14:86–98.
Fordyce WE. Behavioral Methods for Chronic Pain and Illness. Saint Louis: CV Mosby; 1976.
Speckens AEM, van Hemert AM, Spinhoven P, Hawton KE Jr, Bolk JH, Rooijmans GM. Cognitive behavioural therapy for medically unexplained physical symptoms: a randomised controlled trial. BMJ. 1995;311:1328–32.
Lee VC, Rowlingson JC. Chronic pain management. In: Spilker B, ed. Quality of Life Assessments in Clinical Trials. New York, NY: Raven Press; 1990.
Kroenke K, Swindell R. Cognitive-behavioral therapy for somatization and symptom syndromes: a critical review of controlled clinical trials. Psychother Psychosom. 2000;69:205–15.
Barsky AJ. Somatoform disorders. In: Kaplan HI, Sadock BJ, eds. Comprehensive Textbook of Psychiatry, 5th ed. Baltimore, Md: Williams and Wilkins; 1989:1009–27.
Regier D, Goldberg I, Taube C. The de facto mental health services system. Arch Gen Psychiatry. 1978;35:685–93.
Regier DA, Boyd JH, Burke JD Jr, et al. One-month prevalence of mental disorders in the United States: based on five epidemiologic catchment area sites. Arch Gen Psychiatry. 1988;45:977–86.
Bass CM. Assessment and management of patients with functional somatic symptoms. In: Bass CM, ed. Somatization: Physical Symptoms and Psychological Illness. Oxford, UK: Blackwell; 1990:40–72.
France RD, Weddington WW, Houpt JL. Referral of patients from primary care physicians to a community mental health center. J Nerv Ment Dis. 1978;166:594–8.
Speckens AEM, van Hemert A, Bolk JH, Hawton KE, Rooijmans HGM. The acceptability of psychological treatment in patients with medically unexplained physical symptoms. J Psychosom Res. 1995;7:855–63.
Deale A, Husain K, Chalder T, Wessely S. Long-term outcome of cognitive behavior therapy versus relaxation therapy for chronic fatigue syndrome: a 5-year follow-up study. Am J Psychiatry. 2001;158:2038–42.
Whiting P, Bagnall A-M, Snowden AJ, Cornell JE, Mulrow CD, Ramirez G. Interventions for the treatment and management of chronic fatigue syndrome—a systematic review. JAMA. 2001;286:1360–8.
Kleinman A. Explanatory models in health-care relationships: a conceptual frame for research on family-based health-care activities in relation to folk and professional forms of clinical care. In: Stoeckle JD, ed. Encounters Between Patients and Doctors. Cambridge, Mass: The MIT Press; 1987:273–83.
Sharpe M. Cognitive behavioural therapies in the treatment of functional somatic symptoms. In: Mayou R, Bass C, Sharpe M, eds. Treatment of Functional Somatic Symptoms. Oxford, UK: Oxford University Press; 1995:122–43.
Smith RC, Lyles JS, Mettler J, et al. The effectiveness of intensive training for residents in interviewing. A randomized, controlled study. Ann Intern Med. 1998;128:118–26.
Katon W, Von Korff M, Lin E, et al. Stepped collaborative care for primary care patients with persistent symptoms of depression: a randomized trial. Arch Gen Psychiatry. 1999;46:1109–15.
Wagner EH, Austin BT, Von Korff M. Organizing care for patients with chronic illness. Millbank Q. 1996;74:511–44.
Von Korff M, Gruman J, Schaefer J, Curry SJ, Wagner EH. Collaborative management of chronic illness. Ann Intern Med. 1997;127:1097–102.
DeBusk RF, Miller NH, Superko HR, et al. A case-management system for coronary risk factor modification after acute myocardial infarction. Ann Intern Med. 1994;120:721–9.
Odderson IR, McKenna BS. A model for management of patients with stroke during the acute phase: outcome and economic implications. Stroke. 1993;24:1823–7.
Von Korff M. Individualized stepped care of chronic illness. West J Med. 2000;172:133–7.
Kendell RE. The distinction between personality disorder and mental illness. Br J Psychiatry. 2002;180:110–5.
Williams DDR, Garner J. The case against ‘the evidence’: a different perspective on evidence-based medicine. Br J Psychiatry. 2002;180:8–12.
Fink P, Rosendal M, Toft T. How the physician becomes more comfortable with the somatizing patient. Psychosomatics. 2002;43:111–2.
Heymann-Monnikes I, Arnold R, Florin I, Herda C, Melfsen S. The combination of medical treatment plus multicomponent behavioral therapy is superior to medical treatment alone in the therapy of irritable bowel syndrome. Am J Gastroenterol. 2000;95:981–94.
Andreason NC, Black DW. Introductory Textbook of Psychiatry. Washington, DC: American Psychiatric Press, Inc.; 1991.
Smith RC. Somatization disorder: defining its role in clinical medicine. J Gen Intern Med. 1991;6:168–75.
Creed G, Guthrie E. Techniques for interviewing the somatising patient. Br J Psychiatry. 1993;162:467–71.
Smith GR Jr. Treatment of patients with multiple symptoms. In: Mayou R, Bass C, Sharpe M, eds. Treatment of Functional Somatic Symptoms. Oxford, UK: Oxford University Press; 1995:175–187.
Smith RC. Patient-Centered Interviewing: An Evidence-Based Method, 2nd ed. Philadelphia, Pa: Lippincott Williams and Wilkins; 2001.
Smith RC. Videotape of Evidence-Based Interviewing. Available at: http://www.msuvmall.msu.edu/imc. Accessed May 14, 2003.
Smith RC, Lyles JS, Mettler JA, et al. A strategy for improving patient satisfaction by the intensive training of residents in psychosocial medicine: a controlled, randomized study. Acad Med. 1995;70:729–32.
Smith RC, Mettler JA, Stoffelmayr BE, et al. Improving residents’ confidence in using psychosocial skills. J Gen Intern Med. 1995;10:315–20.
Wohlfarth TD, Van Den Brink W, Ormel J, Koeter MWJ, Oldehinkel AJ. The relationship between social dysfunctioning and psychopathology among primary care attenders. Br J Psychiatry. 1993;163:37–44.
Kleinman A. Writing at the Margin: Discourse between Anthropology and Medicine. Berkeley, Calif: University of California Press; 1995.
Ware NC. Toward a model of social course in chronic illness: the example of chronic fatigue syndrome. Cult Med Psychiatry. 1999;23:303–31.
Tresolini CP. Pew-Fetzer Task Force: Health Professions Education and Relationship-Centered Care. San Francisco, Calif: Pew Health Professions Commission; 1994.
Ware NC, Kleinman A. Culture and somatic experience: the social course of illness in neurasthenia and chronic fatigue syndrome. Psychosom Med. 1992;54:546–60.
Quill TE. Partnerships in patient care: a contractual approach. Ann Intern Med. 1983;98:228–34.
Merrill JM, Laux LF, Lorimor RJ, Thornby HI, Vallbona C. Measuring social desirability among senior medical students. Psychol Rep. 1995;77:859–64.
Prochaska JO, DiClemente CC. Towards a comprehensive model of change. In: Miller WR, Heather N, eds. Treating Addictive Behaviors: Processes of Change. New York, NY: Plenum Press; 1986:3–27.
Stoffelmayr B, Hoppe RB, Weber N. Facilitating patient participation: the doctor-patient encounter. Prim Care. 1989;16:265–78.
Lipsitt DR. Medical and psychological characteristics of “crocks”. Psychiatry Med. 1970;1:15–25.
Lipsitt DR. The “rotating” patient: a challenge to psychiatrists. J Geriatr Psychiatry. 1968;2:51–61.
Salmon P, Peters S, Stanley I. Patients’ perceptions of medical explanations for somatisation disorders: qualitative analysis. BMJ. 1999;318:372–6.
Kravitz RL. Measuring patients’ expectations and requests. Ann Intern Med. 2001;134:881–8.
Hahn SR. Physical symptoms and physician-experienced difficulty in the physician-patient relationship. Ann Intern Med. 2001;134:897–904.
Kirmayer LJ, Robbins JM. Conclusion: prospects for research and clinical practice. In: Kirmayer LJ, Robbins JM, eds. Current Concepts of Somatization: Research and Clinical Perspectives. Washington, DC: American Psychiatric Press, Inc.; 1991:201–25.
Kaplan SH, Greenfield S, Ware JE. Impact of the doctor-patient relationship on the outcomes of chronic disease. In: Stewart M, Roter D, eds. Communicating with Medical Patients. London, UK: Sage Publications; 1989:228–45.
Lembo T, Rink R. Current pharmacologic treatments of irritable bowel syndrome. Published in Participate (volume 11, no. 2) by International Foundation for Functional Gastrointestinal Disorders. Available at: http://www.iffgd.org. Accessed 1996.
Benson H. The Relaxation Response. New York, NY: William Morrow and Company, Inc.; 1975.
Keefer L, Blanchard EB. The effects of relaxation response meditation on the symptoms of irritable bowel syndrome: results of a controlled treatment study. Behav Res Ther. 2001;39:801–11.
Keel PJ, Bodoky C, Gerhard U, Muller W. Comparison of integrated group therapy and group relaxation training for fibromyalgia. Clin J Pain. 1998;14:232–8.
Jacobson E. Progressive Relaxation. Chicago, Ill: University of Chicago Press; 1929.
Mannerkorpi K, Nyberg B, Ahlmen M, Ekdahl C. Pool exercise combined with an education program for patients with fibromyalgia syndrome. A prospective, randomized study. J Rheumatol. 2000;27:2473–81.
Houde SC, Melillo KD. Physical activity and exercise counseling in primary care. Nurse Pract. 2000;25:10–37.
Sharpe M, Bass C, Mayou R. An overview of the treatment of functional somatic symptoms. In: Mayou R, Bass C, Sharpe M, eds. Treatment of Functional Somatic Symptoms. Oxford, UK: Oxford University Press; 1995:66–86.
Kirmayer LJ, Robbins JM, Dworkind M, Yaffe MJ. Somatization and the recognition of depression and anxiety in primary care. Am J Psychiatry. 1993;150:734–41.
Katon W, Lin E, von Korff M, Russo J, Lipscomb P, Bush T. Somatization: a spectrum of severity. Am J Psychiatry. 1991;148:34–40.
Smith GR. The epidemiology and treatment of depression when it coexists with somatoform disorders, somatization, or pain. Gen Hosp Psychiatry. 1992;14:265–72.
O’Malley PG, Jackson JL, Tomkins G, Santoro J, Balden E, Kroenke K. Antidepressant therapy for unexplained symptoms and symptom syndromes: a critical review. J Fam Pract. 1999;48:980–93.
Jung AC, Staiger T, Sullivan M. The efficacy of selective serotonin reuptake inhibitors for the management of chronic pain. J Gen Intern Med. 1997;12:384–9.
Fishbain DA, Cutler RB, Rosomoff HL, Rosomoff RS. Do antidepressants have an analgesic effect in psychogenic pain and somatoform pain disorder? A meta-analysis. Psychosom Med. 1998;60:503–9.
Schulberg HC, Katon W, Simon GE, Rush AJ. Treating major depression in primary care practice. Arch Gen Psychiatry. 1998;55:1121–7.
Schulberg HC, Katon WJ, Simon GE, Rush JA. Best clinical practice: guidelines for managing major depression in primary medical care. J Clin Psychiatry. 1999;60(suppl):19–26.
Depression Guideline Panel. Depression in Primary Care: Volume 1. Detection and Diagnosis. Rockville, Md: US Dept. of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research; AHCPR Publication No. 93-0550, April 1993.
Depression Guideline Panel. Depression in Primary Care: Volume 2. Treatment of Major Derpession. Rockville, Md: US Dept. of Health and Human Services, Public Health Service, Agency for Health Care Policy and Research; 1993.
Whooley MA, Simon GE. Managing depression in medical outpatients. N Engl J Med. 2000;343:1942–50.
Simon GE, vonKorff M, Heiligenstein JH, et al. Initial antidepressant choice in primary care—effectiveness and cost of fluoxetine vs tricyclic antidepressants. JAMA. 1997;275:1897–902.
Mulrow CD, Williams JW, Chiquette E, et al. Efficacy of newer medications for treating depression in primary care patients. Am J Med. 2000;108:54–64.
Thapa PB, Gideon P, Cost TW, Milam AB, Ray WA. Antidepressants and the risk of falls among nursing home residents. N Engl J Med. 1998;339:875–82.
National Institute of Mental Health, Katon W. Panic Disorder in the Medical Setting. Washington, DC: US Government Printing Office; 1989. DHHS Pub. No. (ADM)89-1629.
Knesper DJ, Riba MB, Schwenk TL. Primary Care Psychiatry. Philadelphia, Pa: WB Saunders; 1997.
Benjamin S, Mawer J, Lennon S. The knowledge and beliefs of family care givers about chronic pain patients. J Psychosom Res. 1992;36:211–7.
Wasson J, Gaudette C, Whaley F, Sauvigne A, Baribeau P, Welch HG. Telephone care as a substitute for routine clinic follow-up. JAMA. 1992;267:1788–93.
Engel GL. The clinical application of the biopsychosocial model. Am J Psychiatry. 1980;137:535–44.
Engel GL. The need for a new medical model: a challenge for biomedicine. Science. 1977;196:129–36.
deGruy F III. Mental health care in the primary care setting. In: Donaldson MS, Yordy KD, Lohr KN, Vanselow NA, eds. Primary Care—America’s Health in a New Era. Washington, DC: National Academy Press; 1996;285–311.
Hahn SR, Kroenke K, Spitzer RL, et al. The difficult patient: prevalence, psychopathology, and functional impairment. J Gen Intern Med. 1996;11:1–8.
Smith RC. The difficult patient [CD-ROM, vol 7, no. 3]. In: BD Rose, ed. UpToDate. Aronson MD, Fletcher SW, Fletcher RH, eds. Primary Care Series. Available at: 34 Washington St., Suite 320, Wellesley, MA 02181.
Platt FW, Gordon GH. Field Guide to the Difficult Patient Interview. Philadelphia: Lippincott Williams and Wilkins; 1999.
Kroenke K, Arrington ME, Mangelsdorff AD. The prevalence of symptoms in medical outpatients and the adequacy of therapy. Arch Intern Med. 1990;150:1685–9.
Connelly JE, Smith GR, Philbrick JT, Kaiser DL. Healthy patients who perceive poor health and their use of primary care services. J Gen Intern Med. 1991;6:47–51.
Barsky AJ, Saintfort R, Rogers MP, Borus JF. Nonspecific medication side effects and the nocebo phenomenon. JAMA. 2002;287:622–7.
Barsky AJ, Ahern EK, Baileyh ED, Saintfort R, Liu EB, Peekna NM. Hypochondriacal patients’ appraisal of health and physical risks. Am J Psychiatry. 2001;158:783–7.
Klinkman MS. Competing demands in psychosocial care. A model for the identification and treatment of depressive disorders in primary care. Gen Hosp Psychiatry. 1997;19:98–111.
Escobar JI, Manu P, Matthews D, Lane T, Swartz M, Canino G. Medically unexplained physical symptoms, somatization disorder and abridged somatization: studies with the Diagnostic Interview Schedule. Psychiatr Dev. 1989;3:235–45.
Kroenke K, Spitzer RL, deGruy FV, Swindle R. A symptom checklist to screen for somatoform disorders in primary care. Psychosomatics. 1998;39:263–72.
Rief W, Hiller W, Geissner E, Fichter MM. A two-year follow-up study of patients with somatoform disorders. Psychosomatics. 1995;36:376–86.
Fink P. Physical complaints and symptoms of somatizing patients. J Psychosom Res. 1992;36:125–36.
Simon GE, Gureje O. Stability of somatization disorder and somatization symptoms among primary care patients. Arch Gen Psychiatry. 1999;56:90–5.
Cloninger CR, Martin RL, Guze SB, Clayton PJ. A prospective follow-up and family study of somatization in men and women. Am J Psychiatry. 1986;143:873–8.
Klinkman MS, Coyne JC, Gallo S, Schwenk TL. False positives, false negatives, and the validity of the diagnosis of major depression in primary care. Arch Fam Med. 1998;7:451–61.
Muehrer P. Research on co-morbidity, contextual barriers, and stigma. J Psychosom Res. 2002;53:843–5.
Nutting PA, Rost K, Smith J, Werner JJ. Competing demands from physical problems: effect on initiating and completing depression care over 6 months. Arch Fam Med. 2000;9:1059–64.
Rost K, Nutting P, Smith J, Coyne JC, Cooper-Patrick L, Rubenstein L. The role of competing demands in the treatment provided primary care patients with major depression. Arch Fam Med. 2000;9:150–4.
Author information
Authors and Affiliations
Corresponding author
Additional information
This work was supported by National Institute of Mental Health grant MH57099.
Rights and permissions
About this article
Cite this article
Smith, R.C., Lein, C., Collins, C. et al. Treating patients with medically unexplained symptoms in primary care. J GEN INTERN MED 18, 478–489 (2003). https://doi.org/10.1046/j.1525-1497.2003.20815.x
Issue Date:
DOI: https://doi.org/10.1046/j.1525-1497.2003.20815.x