Abstract
OBJECTIVE: To study the attitudes of preclinical and clinical medical students toward the importance of telling patients they are students, and to compare their attitudes with those of patients.
METHODS: We conducted a cross-sectional survey of medical students from five Philadelphia medical schools, and a longitudinal follow-up in one medical school, to assess the importance students place on telling patients they are medical students before interacting with them. We asked similar questions of 100 general medical outpatients from two academically affiliated hospitals.
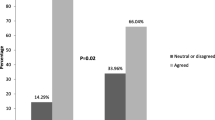
MAIN RESULTS: In total, 2,603 students (58%) responded to the cross-sectional survey, 74 (50%) responded to the longitudinal survey, and 100 patients responded to our interview survey (94% response rate). In the cross-sectional survey, there were negligible differences in the importance that patients and medical students placed on informing alert patients that they are interacting with students in nonsurgical settings. In surgical settings involving anesthetized patients, patients placed significantly more importance on being informed of students’ roles in their surgery than did students, and preclinical students placed more importance on this than did clinical students. Results from the cross-sectional survey were supported by the longitudinal survey, in which fourth-year medical students placed significantly less importance on informing patients of their student status than the same cohort had done 2 years previously.
CONCLUSIONS: Medical students place less importance on informing patients about their student status than patients desire, especially in surgical settings in which the patient is to be anesthetized. Medical students already having completed a clinical rotation stray further from patient ideals than preclinical medical students. These findings suggest that, as medical students advance in their training, they suffer an erosion in their attitudes about telling patients they are students.
Similar content being viewed by others
References
Dworkin G, Cassell EJ. The “student doctor” and the wary patient. Hastings Cent Rep. 1982;12:27–8.
Simpson CL. Misrepresentation of medical students in teaching hospitals. Med Trial Technique Q. 1977;23(3):233–70.
Christakis D, Feudtner C. Ethics in a short white coat: the ethical dilemmas that medical students confront. Acad Med. 1993;68(4):249–54.
Cohen DL, McCullough LB, Kessel RWI. Apostolides AY, Heiderich KJ, Alden ER. A national survey concerning the ethical aspects of informed consent and role of medical students. J Med Educ. 1988;63:821–9.
Cohen DL, Kessel RWI, McCullough LB. Pelvic examinations by medical students. Am J Obstet Gynecol. 1989;161(4):1013–4.
Feudtner C, Christakis D, Christakis NA. Do clinical clerks suffer ethical erosion? Students’ perceptions of their ethical environment and personal development. Acad Med. 1994;69(8):670–9.
Cohen DL, McCullough LB, Kessel R, Apostolides AY, Alden ER, Heiderich KJ. Informed consent policies governing medical students’ interactions with patients. J Med Educ. 1987;62:789–98.
Lawton FG, Redman CWE, Luesley DM. Patient consent for gynaecological examination. Br J Hosp Med. 1990;44(5):326–9.
Bibby J, Boyd N, Redman CWE. Consent for vaginal examination by students on anaesthetized patients. Lancet. 1988;2(8620):1150. Letter.
Silver-Isenstadt A. Times of a medical student activist. JAMA. 1996;276(17):1435.
Annas GJ. The Rights of Patients: The Basic ACLU Guide to Patient Rights. 2nd ed. Totowa, NJ: Humana Press; 1992.
Silver-Isenstadt A, Ubel PA. Medical student name tags: identification or obfuscation? J Gen Intern Med. 1997;12:669–71.
Howell JD. Why medical students are “medical students.” J Gen Intern Med. 1997;12:718–9.
Cohen J. Statistical Power Analysis for the Behavioral Sciences. New York, NY: Academic Press; 1977.
Asch DA, Jedreziewski MK, Christakis NA. Response rates to mail surveys published in medical journals. J Clin Epidemiol. 1997;50(10):1129–36.
Author information
Authors and Affiliations
Additional information
Dr. Ubel is a Robert Wood Johnson Generalist Physician Faculty Scholar and a recipient of a career development award in health services research from the Department of Veterans Affairs.
This research was funded by the Annenberg Public Policy Foundation through its support of the Center for Bioethics’ Project on Informed Consent.
Rights and permissions
About this article
Cite this article
Silver-Isenstadt, A., Ubel, P.A. Erosion in medical students’ attitudes about telling patients they are students. J GEN INTERN MED 14, 481–487 (1999). https://doi.org/10.1046/j.1525-1497.1999.09298.x
Issue Date:
DOI: https://doi.org/10.1046/j.1525-1497.1999.09298.x