Abstract
Women comprised 19% of new HIV diagnoses in the United States in 2014, with significant racial and ethnic disparities in infection rates. This cross-sectional analysis of women enrolled in a cohort study compares demographics, risk behaviour, and sexually transmitted infections (STI) in those undergoing HIV testing in San Diego County. Data from the most recent screening visit of women undergoing voluntary HIV screening April 2008 –July 2014 was used. HIV diagnosis, risk behaviour and self-reported STIs were compared among women aged ≤24, 25–49, and ≥50, as well as between HIV-infected and uninfected women and between Hispanic and non-Hispanic women. Among the 2535 women included, Hispanic women were less likely than other women to report unprotected vaginal intercourse (p = 0.026) or stimulant drug use (p = 0.026), and more likely to report one or fewer partners (p < 0.0001), but also more likely to report sex with an HIV-infected individual (p = 0.027). New HIV infection was significantly more prevalent among Hispanic women (1.6% vs. 0.2%; p < 0.001). Hispanic women were more likely than other women to be diagnosed with HIV despite significantly lower rates of risk behaviour. Culturally specific risk reduction interventions for Hispanic women should focus on awareness of partner risk and appropriate testing.
Similar content being viewed by others
Introduction
Although the number of new HIV cases in the US has stabilised in recent years, specific groups remain disproportionately affected. While both prevalence and incidence of HIV are higher among men, women accounted for 19% of new HIV diagnoses and 25% of Stage 3 (AIDS) diagnoses nationwide in 20141. While African American women carry the heaviest burden of HIV in the United States2,3,4,5,6, Hispanic women are also disproportionately affected with a prevalence 1.6 times that of White women in California, though sex-stratified prevalence among Hispanic people is not available at the county level for San Diego1,7. Whether this finding may be explained by increased risk behaviour remains unclear.
The objective of this study was to compare demographics, risk behaviour, and sexually transmitted infections (STI) in women in San Diego County undergoing community-based HIV testing with detection of acute and early HIV infection (AEH).
Results
Overview of participants
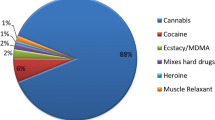
Demographics, self-reported behavioural and exposure risk are reported in Table 1. A total of 2538 women underwent Early Test enrolment and screening between April 2008 and July 2014, and three women were excluded from the analysis because they reported already having a diagnosis of HIV prior to testing. Included participants had a median age of 32 years (IQR 25–44), 39.4% self-identified as White, 36.3% as Hispanic/Latina, 11.8% as Black – African American. Overall 91.7% reported they had previously tested for HIV at a median of 9.3 months (IQR 3.3–25.9) before the current testing encounter. One or fewer sex partners in the last 12 months was reported by 44.6% of participants; women older than 50 reported the fewest partners (median 1, IQR 1–2); and women under 25 reported the highest number of partners (median 1, IQR 1–4; p < 0.001). Overall 84.6% of women reported unprotected receptive vaginal intercourse (URVI) and 7.9% of women reported sex with an HIV-infected partner (more frequent among women 25 years or older versus those 24 years or younger).
HIV test results, associated demographics and risk behaviour
Twenty women (0.7%) tested positive for HIV, and 7 (39%) of these had early stage infection with an estimated date of infection within the last 180 days. Of the 11 HIV + patients for whom data were available, the mean CD4 count at presentation was 348 (SD 179) cells/μL and mean viral load was 55,900 (SD 139,000) copies/mL. Demographic and risk behaviour associated with HIV infection are reported in Table 2. Women with HIV infection were significantly more likely to be Hispanic (82.4% vs. 36.0% p = 0.008), to have had sex with a known HIV-infected individual in the last 12 months (33.3% vs. 7.7%, p = 0.002), and to report a sexually transmitted infection in the last 12 months (23.5% vs. 8.3%, p = 0.047) than HIV-uninfected women. There was also a trend toward a higher proportion of HIV-infected women reporting one or fewer partners in the last 12 months (66.7% vs. 44.5%, p = 0.093). Reported stimulant use and injection drug use (IDU) was similar between HIV-infected and uninfected women, as was unprotected vaginal and anal intercourse, sex with injection drug users and sex with men who have sex with men. Very little exchange of sex for money or drugs was reported in our population, though more than half of participants declined to answer this question.
Risk behaviours of Hispanic versus non-Hispanic women
Because HIV infection was significantly more prevalent among Hispanic women than other women (1.6% vs. 0.2%; p < 0.001), a comparison of risk behaviours in Hispanic versus non-Hispanic women was performed as summarized in Table 3. Hispanic women reported fewer partners in the last 12 months compared to non-Hispanic women, with a median of 1 (IQR 1–2.25) versus 2 (IQR 1–4) partners respectively, and were more likely to report 1 or fewer partners in the last 12 months compared with non-Hispanic women (56.8% vs. 37.8% p < 0.0001). Though a large majority of women in the study reported unprotected vaginal intercourse (84.6%, Table 1), this was significantly less prevalent among Hispanic women than non-Hispanic women (82.4% vs. 86.1%, respectively, p = 0.026). Hispanic women also reported less stimulant drug use (21.4% vs. 25.5%, p = 0.026) and had a trend toward less injection drug use (4.5% vs. 6.3%, p = 0.067). The only behavioural risk factor that was more prevalent among Hispanic women than non-Hispanic women was sex with an HIV-infected individual (9.7% vs. 7.0%, p = 0.027).
In a sub-analysis of Black versus White women, Black women had slightly fewer partners (median 2 for both, IQR 1–3 for Black and IQR 1–4 for White; Mann-Whitney-U test p = 0.01), and were less likely to report sex with an injection drug user (0.03 vs 0.16), or stimulant substance use (0.17 vs 0.30) or injection drug use (0.02 vs 0.09), all with p < 0.001. Additionally, no difference was found in the proportion of Black versus White women reporting unprotected vaginal intercourse (0.86 vs 0.87, p = 0.60), or sex with an HIV-infected partner (0.06 vs 0.09, p = 0.13).
Discussion
Among women undergoing HIV testing with our program, 0.7% were found to be HIV-infected and previously unaware of their status. Additionally, Hispanic women were disproportionately impacted, with more than double the HIV prevalence observed in non-Hispanic women, despite significantly less risky behaviour. The observed prevalence (0.7%) of HIV-infected and unaware women in the study is nearly 8-fold higher than the overall prevalence of HIV among women in San Diego of 0.09%7, suggesting women who presented for testing are a higher risk group than the general San Diego population. Previous venue-based or respondent-driven sampling studies targeting high risk women of colour in the eastern United States report a high prevalence of unaware HIV-infected women, ranging from 1.4% to 9.8%8,9,10,11. We observed a comparably high rate of 1.6% new HIV diagnoses among Hispanic women in our study.
Interestingly, although HIV-infected women reported unprotected intercourse at similar rates to those without infection, there was a trend toward a higher proportion of HIV-infected women reporting no more than one sex partner in the prior year. This is in contrast to previous work reporting high rate of concurrency among high-risk women and their partners12. The finding of lower risk behaviour among HIV-infected women in our study appears to be driven by the predominance of Hispanic women, who overall had fewer partners, engaged in significantly less unprotected sex than their non-Hispanic counterparts, reported significantly less stimulant drug use, and had a trend toward less reported IDU as well. However, Hispanic women were significantly more likely to report sex with an HIV-infected partner.
Taken together, these data suggest that the increased risk of HIV infection among Hispanic women presenting for HIV testing at Early Test sites in San Diego is primarily a reflection of their increased likelihood of exposure to HIV-infected men in their network of sexual contacts, rather than higher rates of sexual risk behaviour in the women. This finding is similar to reports in the community of men who have sex with men (MSM), where race has been shown to be a strong predictor of risk even though reported behaviours are similar among the groups13,14,15. Additionally, syndemic factors such as poverty, trauma, substance abuse, homelessness and incarceration as well as San Diego’s border location likely contribute to the high prevalence of undiagnosed infection among Hispanic women16,17,18,19,20,21,22,23,24,25,26. Similarly, the HPTN 064 study, which aimed to estimate the overall new HIV infection rate in women at risk for HIV in the United States, study subjects perceived their risk as due to structural and contextual factors27.
This study is subject to a number of limitations. First, high-risk women were not specifically targeted for recruitment, and this combined with the overall low prevalence of HIV among women in San Diego resulted in a small number of newly identified infections from which to draw comparisons. Other authors studying risk behaviours in US women have used targeted sampling in selected high-risk areas to obtain an enriched sample8,9,11,28,29 or focused their studies on a known high-risk group30,31,32. However, with more than 2500 women enrolled over 6 years, this is one of the largest HIV screening studies in US women published to date. Also, Hispanic and Black women were slightly over-represented in our sample at 36.3% and 11.8% respectively compared with 33.2% and 5.6% of the overall population in San Diego33. Additional limitations of our study include its single-centre retrospective design and reliance on self-reported risk behaviour.
In conclusion, our study showed that Hispanic women presenting for free HIV testing at Early Test sites in San Diego are disproportionately affected by HIV infection, and that this increased risk is not linked to higher risk behaviours in this group but rather higher likelihood of having an HIV-infected partner. Culturally-specific HIV risk reduction interventions for Hispanic women are needed which emphasize awareness of partner-risk, knowledge of partner status and prevention methods for serodiscordant couples, including those trying to conceive, such as antiretroviral therapy to suppress viral load and pre-exposure prophylaxis (PrEP). This could provide Hispanic women with the necessary knowledge, skills and services to protect themselves against HIV.
Methods
Study design and population
This is a cross-sectional analysis of a cohort study comprised women from a convenience sample of self-selected adults undergoing voluntary HIV screening (single and repeat testers) in San Diego, California, with the Early Test34 between April 2008 and July 2014. During this time period, 2535 women were tested and the most recent testing encounter for each is included in the analysis. Data on MSM35,36 and transgender women and transgender men37 testing with the Early Test have been published previously.
The Early Test: HIV testing, demographic and risk behaviour data collection
Starting in February 2007, the Early Test program (https://theearlytest.ucsd.edu) offered HIV testing, free of charge, to all adults who presented for testing at multiple sites in San Diego County including the San Diego County Health Department; Christie’s Place (a centre for women and families affected by HIV); the University of California, San Diego (UCSD) Antiviral Research Center; several community health centres; the Lesbian, Gay, Bisexual, Transgender Center; and substance abuse treatment centres. Women were also recruited at Planned Parenthood by flyers and provider referral to our testing sites34,38,39. Demographic as well as sexual risk behaviour, STIs, and substance use for the prior 12 months was recorded on a paper case report form by bilingual study personnel performing interviews in English or Spanish. Survey questions were assessed by the testing staff before each HIV testing encounter38.
Statistical analysis
For statistical analysis, SPSS 23 (SPSS Inc., Chicago, IL, USA) was used. Outcome measures included risk behaviour and STIs reported for the previous 12 months at every testing encounter, as well as HIV diagnoses. Outcome measures were compared among women aged ≤24, 25–49, and ≥50, as well as between HIV-infected and uninfected women and between Hispanic and non-Hispanic women using the chi-squared test (for proportions), the Mann Whitney U test (for continuous variables, such as numbers of partners between two groups), and the Kruskal-Wallis test (for continuous variables, such as numbers of partners among three groups). A p-value < 0.05 was considered statistically significant.
Ethics approval
The University of California, San Diego (UCSD) Human Research Protections Program approved the study protocol and consent, and the methods were carried out in accordance with the UCSD Institutional Review Board’s approved guidelines and regulations. All study participants provided voluntary, written informed consent before any study procedures.
Additional Information
How to cite this article: Graves, S. K. et al. Risk profile and HIV testing outcomes of women undergoing community-based testing in San Diego 2008–2014. Sci. Rep. 7, 42183; doi: 10.1038/srep42183 (2017).
Publisher's note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
References
Centers for Disease Control and Prevention. Diagnoses of HIV Infection in the United States and Dependent Areas, 2014. HIV Surveill. Rep. 26 (2015).
Koblin, B. A. et al. Feasibility of identifying a cohort of US women at high risk for HIV infection for HIV vaccine efficacy trials: longitudinal results of HVTN 906. J. Acquir. Immune Defic. Syndr. 1999 63, 239–244 (2013).
Eshleman, S. H. et al. Use of a multifaceted approach to analyze HIV incidence in a cohort study of women in the United States: HIV Prevention Trials Network 064 Study. J. Infect. Dis. 207, 223–231 (2013).
Haley, D. F. et al. Retention strategies and factors associated with missed visits among low income women at increased risk of HIV acquisition in the US (HPTN 064). AIDS Patient Care STDs 28, 206–217 (2014).
Chen, I. et al. Antiretroviral Drug Use in a Cohort of HIV-Uninfected Women in the United States: HIV Prevention Trials Network 064. PloS One 10, e0140074 (2015).
Jennings, L. et al. Prevalence and Correlates of Knowledge of Male Partner HIV Testing and Serostatus Among African-American Women Living in High Poverty, High HIV Prevalence Communities (HPTN 064). AIDS Behav. 19, 291–301 (2015).
Emory University, Rollins School of Public Health. AIDSVu. AIDSVu Available at: www.aidsvu.org. (Accessed: 5th June 2016).
Metch, B. et al. Recruitment of Urban US Women at Risk for HIV Infection and Willingness to Participate in Future HIV Vaccine Trials. AIDS Behav. 17, 760–772 (2013).
Hodder, S. L. HIV Acquisition Among Women From Selected Areas of the United States: A Cohort Study. Ann. Intern. Med. 158, 10 (2013).
Haley, D. F. et al. Venue-based recruitment of women at elevated risk for HIV: an HIV Prevention Trials Network study. J. Womens Health 2002 23, 541–551 (2014).
Reilly, K. H. et al. High HIV Prevalence Among Low-Income, Black Women in New York City with Self-Reported HIV Negative and Unknown Status. J. Womens Health 22, 745–754 (2013).
Adimora, A. A. et al. Characteristics of multiple and concurrent partnerships among women at high risk for HIV infection. J. Acquir. Immune Defic. Syndr. 1999 65, 99–106 (2014).
Sullivan, P. S. et al. Understanding Racial HIV/STI Disparities in Black and White Men Who Have Sex with Men: A Multilevel Approach. PLoS ONE 9, e90514 (2014).
Millett, G. A. et al. Comparisons of disparities and risks of HIV infection in black and other men who have sex with men in Canada, UK, and USA: a meta-analysis. The Lancet 380, 341–348 (2012).
Beer, Li., Oster, A. M., Mattson, C. L. & Sarbinski, J. Disparities in HIV transmission risk among HIV-infected black and white men who have sex with men, United States, 2009. AIDS Lond. Engl. AIDS Lond. Engl. 28, 105–114 (2014).
Singer, M. & Clair, S. Syndemics and public health: reconceptualizing disease in bio-social context. Med. Anthropol. Q. 17, 423–441 (2003).
Strathdee, S. A. et al. Characteristics of Female Sex Workers With US Clients in Two Mexico-US Border Cities. Sex. Transm. Dis. 35, 263–268 (2008).
Martinez-Donate, A. P. et al. HIV Prevention Among Mexican Migrants at Different Migration Phases: Exposure to Prevention Messages and Association With Testing Behaviors. AIDS Educ. Prev. 27, 547–565 (2015).
Koblin, B. A. et al. HIV Sexual Risk and Syndemics among Women in Three Urban Areas in the United States: Analysis from HVTN 906. J. Urban Health 92, 572–583 (2015).
Golin, C. E. et al. Post-traumatic Stress Disorder Symptoms and Mental Health over Time among Low-Income Women at Increased Risk of HIV in the U.S. J. Health Care Poor Underserved 27, 891–910 (2016).
Montgomery, B. E. E. et al. Violence Against Women in Selected Areas of the United States. Am. J. Public Health 105, 2156–2166 (2015).
Kuo, I. et al. Substance use patterns and factors associated with changes over time in a cohort of heterosexual women at risk for HIV acquisition in the United States. Drug Alcohol Depend. 139, 93–99 (2014).
Wyatt, G. E. et al. Does a History of Trauma Contribute to HIV Risk for Women of Color? Implications for Prevention and Policy. Am. J. Public Health 92, 660–665 (2002).
Zierler, S. et al. Adult survivors of childhood sexual abuse and subsequent risk of HIV infection. Am. J. Public Health 81, 572–575 (1991).
Zhang, X. et al. Risk behaviours for HIV infection among travelling Mexican migrants: The Mexico-US border as a contextual risk factor. Glob. Public Health 1–19, doi: 10.1080/17441692.2016.1142591 (2016).
El-Bassel, N., Witte, S. S., Wada, T., Gilbert, L. & Wallace, J. Correlates of partner violence among female street-based sex workers: substance abuse, history of childhood abuse, and HIV risks. AIDS Patient Care STDs 15, 41–51 (2001).
Blackstock, O. J. et al. Perceptions of Community HIV/STI Risk Among U.S Women Living in Areas with High Poverty and HIV Prevalence Rates. J. Health Care Poor Underserved 26, 811–823 (2015).
Polk, S., Ellen, J. M., Fichtenberg, C., Huettner, S. & Jennings, J. M. HIV Prevalence Overall and among High-HIV-Risk Behaviorally Defined Subgroups among Heterosexuals at Community-Based Venues in a Mid-Atlantic, US City. J. Urban Health Bull. N. Y. Acad. Med. 90, 747–757 (2013).
Jenness, S. M. et al. Patterns of Exchange Sex and HIV Infection in High-Risk Heterosexual Men and Women. J. Urban Health Bull. N. Y. Acad. Med. 88, 329–341 (2011).
Sionean, C. et al. HIV risk, prevention, and testing behaviors among heterosexuals at increased risk for HIV infection–national HIV behavioral surveillance system, 21 US Cities, 2010. MMWR Surveill Summ 63, 1–39 (2014).
Parvez, F., Katyal, M., Alper, H., Leibowitz, R. & Venters, H. Female sex workers incarcerated in New York City jails: prevalence of sexually transmitted infections and associated risk behaviors. Sex. Transm. Infect. 89, 280–284 (2013).
Inciardi, J. A., Surratt, H. L. & Kurtz, S. P. HIV, HBV, and HCV infections among drug-involved, inner-city, street sex workers in Miami, Florida. AIDS Behav. 10, 139–147 (2006).
US Census Bureau. U.S. Census Bureau QuickFacts. Available at: //www.census.gov/quickfacts/table/HSG030210/06073 (Accessed: 5th June 2016) (2010).
Morris, S. R. et al. Evaluation of an HIV Nucleic Acid Testing Program With Automated Internet and Voicemail Systems to Deliver Results. Ann. Intern. Med. 152, 778–785 (2010).
Hoenigl, M., Green, N., Mehta, S. R. & Little, S. J. Risk Factors for Acute and Early HIV Infection Among Men Who Have Sex With Men (MSM) in San Diego, 2008 to 2014: A Cohort Study. Medicine (Baltimore) 94, e1242 (2015).
Hoenigl, M., Chaillon, A., Morris, S. R. & Little, S. J. HIV Infection Rates and Risk Behavior among Young Men undergoing community-based Testing in San Diego. Sci. Rep. 6, 25927 (2016).
Green, N., Hoenigl, M., Morris, S. & Little, S. J. Risk Behavior and Sexually Transmitted Infections Among Transgender Women and Men Undergoing Community-Based Screening for Acute and Early HIV Infection in San Diego. Medicine (Baltimore) 94, e1830 (2015).
Hoenigl, M. et al. Repeat HIV-testing is associated with an increase in behavioral risk among men who have sex with men: a cohort study. BMC Med. 13, 218 (2015).
Hoenigl, M., Graff-Zivin, J. & Little, S. J. Costs per Diagnosis of Acute HIV Infection in Community-based Screening Strategies: A Comparative Analysis of Four Screening Algorithms. Clin. Infect. Dis. Off. Publ. Infect. Dis. Soc. Am. 62, 501–511 (2016).
Acknowledgements
This work was supported by funds from the following: the Interdisciplinary Research Fellowship in NeuroAIDS (R25-MH081482), a Translational Methamphetamine AIDS Research Center (TMARC) (NIDA award number P50DA026306) pilot grant, the Max Kade Foundation, New York (Max Kade Postdoctoral Research grant), the Department of Veterans Affairs and grants from the National Institutes of Health: AI106039, AI043638, AI074621, AI108351, and MH100974. The funders had no role in study design, data collection and analysis, decision to publish, or preparation of the manuscript.
Author information
Authors and Affiliations
Contributions
S.G., S.L. and M.H. designed the study. S.L. and M.H. designed and implemented the data collection instruments. S.G. performed data analysis. S.G., S.L. and M.H. all contributed to interpretation of the analysis. S.G. prepared the manuscript and S.L. and M.H. revised it critically for intellectual content. All authors have given final approval of the version to be published.
Corresponding authors
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
This work is licensed under a Creative Commons Attribution 4.0 International License. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in the credit line; if the material is not included under the Creative Commons license, users will need to obtain permission from the license holder to reproduce the material. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/
About this article
Cite this article
Graves, S., Little, S. & Hoenigl, M. Risk profile and HIV testing outcomes of women undergoing community-based testing in San Diego 2008–2014. Sci Rep 7, 42183 (2017). https://doi.org/10.1038/srep42183
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/srep42183
This article is cited by
-
Longitudinal predictors of male sexual partner risk among Black and Latina women in their late thirties: ethnic/racial identity commitment as a protective factor
Journal of Behavioral Medicine (2021)
-
Universal HIV and Birth Cohort HCV Screening in San Diego Emergency Departments
Scientific Reports (2019)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.