Abstract
Study design:
A multicenter prospective cohort study.
Objective:
To compare the demographic data of the included population with other studied spinal cord injury (SCI) populations in the international literature.
Setting:
Eight Dutch rehabilitation centers with a specialized SCI unit.
Methods:
A total of 205 individuals with SCI participated in this study. Information about personal, lesion and rehabilitation characteristics were collected at the beginning of active rehabilitation by means of a questionnaire.
Results:
The research group mainly consisted of men (74%), of individuals with a paraplegia (59%), and had a complete lesion (68%). The SCI was mainly caused by a trauma (75%), principally due to a traffic accident (42%). The length of clinical rehabilitation varied between 2 months and more than a year, which seemed to be dependent on the lesion characteristics and related comorbidity.
Conclusions:
The personal and lesion characteristics of the subjects of the multi-center study were comparable to data of other studies, although fewer older subjects and subjects with an incomplete lesion were included due to the inclusion criteria ‘age’ and ‘wheelchair-dependent’. The length of stay in rehabilitation centers in The Netherlands was longer compared to Denmark but much longer than in eg Australia and the USA.
Similar content being viewed by others
Introduction
The life expectancy of people with a spinal cord injury has improved over the years due to improved medical treatment.1, 2, 3 In the past, research was mainly focused on the prevention and cure of health-threatening complications such as infections of the urinary tract and airways. Today, the focus of research has shifted much more towards restoration of mobility and optimization of the rest capacity of the individual to improve the quality of life.4, 5
Previous studies6, 7, 8, 9 concentrated on one particular aspect of rehabilitation and/or included only relatively small numbers of subjects. In 1970, the USA started the ‘Model Spinal Cord Injury Systems’,10 which in 1999 contained data of about 19 000 individuals with an acute traumatic SCI from different US centers. However, that database does not contain results of physical tests. In contrast the Dutch multicenter project ‘Restoration of mobility in SCI rehabilitation’ involves a relatively large group of patients with SCI (n=205) who performed an extensive test battery four times during (3 × ) and after (1 × ) rehabilitation with outcome measures covering the broad framework of the ICF model.11, 12, 13, 14, 15, 16, 17, 18, 19
We compare the demographic data of the included population with other studied SCI populations in the international literature.
Methods
Subjects inclusion
Persons with recent SCI, that is, not readmitted, were recruited from eight rehabilitation centers that specialize in SCI rehabilitation in the Netherlands between August 2000 and July 2003. Subjects were eligible to enter the project if they had an acute SCI and were classified as A, B, C, or D on the American Spinal Injury Association (ASIA)20 impairment scale. An age range of 18–65 years was chosen to avoid the possible confounding effect at a young (eg development) and older age. People older than 65 were excluded because they are more at risk during the maximal exercise test, which was one of the tests conducted in the multicenter study. Since mobility restoration means wheelchair mobility in most of the people with SCI, only subjects who were at least in part wheelchair-dependent were included. Potential participants with a progressive disease or psychiatric problem and those who did not have enough knowledge of the Dutch language were excluded, as these factors may have a possible confounding effect on testing of the restoration of mobility.
All subjects completed an informed consent form after they were given information about the study, which was approved by the local Medical Ethics Committee of rehabilitation center Hoensbroek.
Demographics
Personal and lesion characteristics, the cause of the spinal cord injury, the age and gender of the patients were collected at the start of active rehabilitation (when the patient was able to sit in a wheelchair for 3–4 h) by means of a questionnaire, which was administered by eight local research assistants. To determine the lesion characteristics (tetraplegia, paraplegia and complete or incomplete lesion) the ASIA form21 was used.
Patient selection
To evaluate possible consequences of patient selection bias, the registration of people with SCI between 18–65 years who did not enroll into the study was conducted in seven centers. Unfortunately, in one center the registration was not conducted sufficiently systematic.
Statistics
In addition to descriptive statistics, cross tables were used to describe personal characteristics. Differences between the participants of the multicenter project and those who did not participate due to exclusion criteria were tested with a χ2 test (gender, lesion level and completeness) and an independent t-test (age) (P<0.05).
Results
Subjects included
During the 3-year period 205 patients were included in the Dutch multicenter study. The personal characteristics of the participants at the start of active rehabilitation are presented in Table 1. Most of the participants were male (74%). The patients were reasonably spread over the age groups (Figure 1, Table 1), and had a mean age of 40.8±14.1 years.
Of the total group, 68% had a complete lesion and 59% were treated for paraplegia (Figure 2, Table 1). For 75% of the patients the cause of the spinal cord injury was a trauma. The main cause of the traumatic lesion was a traffic accident (42%), thereafter a fall (23%) and a sports accident (15%) (Table 1). The nontraumatic lesions were mainly caused by various other reasons not mentioned in the questionnaire (Table 1), namely spondylodiscitis, astrocytoma, tuberculous process, empyema, hernia nucleus pulposus, arthrosis, syringomyelia, echinococcus infection, osteoporosis.
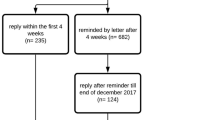
Subjects excluded
A total of 163 patients were excluded or did not enroll while 189 patients were included in those seven centers. Of the excluded group, 67% were male, 72% had a paraplegia, 20% had a complete lesion and the average age was 43.8±13.1 years. The excluded group contained significantly more patients with an incomplete lesion or paraplegia. Reasons for not participating in the study varied: refusal, would not remain wheelchair dependent, had a progressive disease or psychiatric problem, or did not have enough knowledge of the Dutch language (Figure 3).
Demographics
The time between the occurrence of the lesion and the start of active rehabilitation varied between 0 and 2 months and more than a year (Figure 4). Some patients performed the tests more than 8 months after incurrence of their injury. This was due to several secondary complications, such as decubitus, that led to bed rest (range: 20–240 days), which made it impossible to perform the tests earlier.
The clinical rehabilitation took longer than a year for 50% of the 39 patients with a complete tetraplegia (average: 387±174 days) (Figure 5). The average length of clinical rehabilitation varied between persons with an incomplete tetraplegia (243±138 days), incomplete paraplegia (221±145 days) and complete paraplegia (212±90 days).
Loss to follow-up
In all, 52 of the 205 included patients at the start of active rehabilitation dropped out during the project. There were different reasons for dropping out: some subjects were diseased, others moved away or refused to collaborate further, could not be reached, could walk again, were mistakenly included, or got psychological problems (Figure 3).
Discussion
Subjects included
In a study of Van Asbeck et al,22 the incidence of a traumatic lesion in The Netherlands was estimated to be 10.4 per million inhabitants per year. With 15.1 million inhabitants, that means an estimated 157 new individuals with a traumatic lesion per year from which 70% (110 people) will be admitted in a rehabilitation center22 (Figure 3). This is 48% (only traumatic) of the total number of patients with a SCI,23 that subsequently can be estimated on 229 patients per year. That means that during the inclusion period of the multicenter project (3 years) 687 potential subjects would have been available, with the assumption that almost everybody will be admitted to one of the eight rehabilitation centers. These numbers suggest that an estimated 30% (N=205) of the potential subjects satisfied the inclusion criteria and enrolled.
A total of 85% of the patients, who satisfied the inclusion criteria (189 patients plus those who refused and did not participate for unknown reasons), were included. This percentage is higher than the response on questionnaire studies among ex-patients of a Dutch rehabilitation center, respectively 60%20 and 67% response.24 The participants of the multicenter project are representative for the whole group of clinical patients regarding age and gender but the Dutch multi-center study included more persons with a tetraplegia and complete lesion compared to the group with excluded patients and drop-outs at the start of the project. Furthermore, it should be kept in mind that there were 52 drop-outs during the study, which might have led to a positive selection of subjects at the last test occasion.
Demographics compared
Although the results of the Dutch multicenter study project can be compared with epidemiological literature, which describe populations with a SCI in- and outside Europe,22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35 objectives among these studies and their tests do differ. The percentage male subjects (74%) in the multicenter project was in the range of percentages found in other studies (69–82%).22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35
The average age in the studies (Table 1) varied between 30–50 years.23, 26, 27, 28, 30, 31, 32, 34 The mean age of the subjects of the multicenter project (40.8 years) lies in this range. A quarter of the patients were between 20 and 30 years. This group was also quite large in other studies.22, 24, 25, 27, 28, 30, 32, 33, 34 In the Netherlands younger people are more at risk for a SCI, mainly due to traffic accidents.23 People older than 65 years were excluded from the multi-center project. Therefore, the percentage subjects in the 60 years and older group of the multicenter project will give an underestimation.22, 23, 35 It is important to realize that the older patient group is a special group with other demands on the rehabilitation program.
The percentage patients with a paraplegia (59%) in the multicenter study was in the range of values found in the literature (40–75%)(Table 1).22, 23, 24, 25, 26, 27, 28, 29, 30, 31, 32, 33, 34, 35 The percentage people with a complete lesion varied considerably among studies (27–87%).22, 23, 24, 25, 26, 27, 29, 30, 31, 32, 33, 34, 35 The number of subjects with an incomplete lesion was relatively low in the multicenter project because the subjects had to be wheelchair-dependent.
A traffic accident was the most frequent cause of a traumatic lesion. Local factors appear to affect the cause of the SCI. Violence is for example the main cause (62%) of traumatic lesions in South Africa.29 The qualification of nontraumatic lesions was more difficult because studies used different group divisions. Table 1 indicates that the percentage patients with a traumatic lesion (75%) was relatively high compared to some other studies.23, 28, 30 According to the results of Schönherr et al,23 who studied 293 patients admitted to one Dutch rehabilitation center, the group with a nontraumatic lesion is larger (52%) in the general population with a SCI. Not all studies included both participants with a traumatic and non-traumatic lesion.22, 24, 31, 33, 34, 35 The studies that included both groups varied in the percentage nontraumatic lesions, ranging from 11 to 46%.25, 27, 28, 29, 30, 36 The relatively low number of participants with a nontraumatic lesion in the present study might be explained by two reason. Firstly, most patients with nontraumatic lesions are older (50–60 years of age)23, 25, 28 and might, due to the exclusion criteria ‘age’, be excluded from the study. Secondly, nontraumatic lesions might be caused by progressive diseases36 and these individuals were also excluded.
The time between the occurrence of the lesion and the first measurement varied enormously in the multicenter project. For some subjects the time since injury was <2 months at the start of active rehabilitation, for others longer than a year due to all kind of secondary complications.
On average per lesion group the length of stay in the rehabilitation center was 212–387 days in the multicenter study. This was higher than for example in Denmark (149–285 days)25 or Israel (239 days for patients with traumatic lesions and 106 days for patients with nontraumatic lesions).36 The length of stay in Australia is considerably shorter (43–206 days).37 In the USA the average length of stay between 1973 and 1977 was 145 days but 15 years later this was decreased to 78 days.38 In the Netherlands the length of stay is primarily determined in the successful attainment of the rehabilitation goals (optimal level of functional independence and daily functioning). However, it also happens that patients stay in the rehabilitation center longer than necessary because they have to wait for appropriate housing.
Conclusion
The results of the participant characteristics of the Dutch multicenter study ‘Restoration of mobility in SCI rehabilitation’ were in the range of what was found in other studies concerning age, gender and lesion level. However, due to the selection criteria (such as 18–65 years and wheelchair dependent) fewer elderly people and more patients with a complete and traumatic lesion were included in the project, which limits the generalization of some of the results. Outcome of restoration of mobility may – to a large extend – be viewed representative for the age group 18–65 years, and those who are (partly) wheelchair-dependent.
References
van Asbeck FWA . Functioneren met een dwarslaesie, 1987 RU Groningen.
Beck D, Buck M, Pons C . De Revalidatie van dwarslaesiepatienten. De Tijdstroom: Utrecht 1997.
Whiteneck G . Aging with spinal cord injury. Demos Publications: New York 1993.
Dearwater SR, LaPorte RE, Robertson RJ, Brenes G, Adams LL, Becker D . Activity in the spinal cord-injured patient: an epidemiologic analysis of metabolic parameters. Med Sci Sports Exerc 1986; 18: 541–544.
Noreau L, Shephard RJ . Spinal cord injury, exercise and quality of life. Sports Med 1995; 20: 226–250.
Dallmeijer AJ, van der Woude LH, Hollander AP, van As HH . Physical performance during rehabilitation in persons with spinal cord injuries. Med Sci Sports Exerc 1999; 31: 1330–1335.
Lucke KT, Coccia H, Goode JS, Lucke JF . Quality of life in spinal cord injured individuals and their caregivers during the initial 6 months following rehabilitation. Qual Life Res 2004; 13: 97–110.
MacPhee AH, Kirby RL, Coolen AL, Smith C, MacLeod DA, Dupuis DJ . Wheelchair skills training program: A randomized clinical trial of wheelchair users undergoing initial rehabilitation. Arch Phys Med Rehabil 2004; 85: 41–50.
Seelen HA, Potten YJ, Drukker J, Reulen JP, Pons C . Development of new muscle synergies in postural control in spinal cord injured subjects. J Electromyogr Kinesiol 1998; 8: 23–34.
Becker BE, DeLisa JA . Model Spinal Cord Injury System trends, and implications for the future. Arch Phys Med Rehabil 1999; 80: 1514–1521.
Dallmeijer AJ et al. Hand-rim wheelchair propulsion capacity during rehabilitation of persons with spinal cord injury. J Rehabil Res Dev 2005; 42: 55–64.
de Groot S et al. Course of gross mechanical efficiency in handrim wheelchair propulsion during rehabilitation of people with spinal cord injury: a prospective cohort study. Arch Phys Med Rehabil 2005; 86: 1452–1460.
Kilkens OJ, Post MW, Van Der Woude LH, Dallmeijer AJ, van den Heuvel WJ . The wheelchair circuit: reliability of a test to assess mobility in persons with spinal cord injuries. Arch Phys Med Rehabil 2002; 83: 1783–1788.
Kilkens OJ, Post MW, Dallmeijer AJ, Seelen HA, Van Der Woude LH . Wheelchair skills tests: a systematic review. Clin Rehabil 2003; 17: 418–430.
Kilkens OJ, Dallmeijer AJ, De Witte LP, Van Der Woude LH, Post MW . The Wheelchair Circuit: Construct validity and responsiveness of a test to assess manual wheelchair mobility in persons with spinal cord injury. Arch Phys Med Rehabil 2004; 85: 424–431.
Kilkens OJ, Post MW, Dallmeijer AJ, Van Asbeck FW, Van Der Woude LH . Relationship between manual wheelchair skill performance and participation of persons with spinal cord injuries 1 year after discharge from inpatient rehabilitation. J Rehabil Res Dev 2005; 42: 65–74.
Kilkens OJ, Dallmeijer AJ, Nene AV, Post MW, Van Der Woude LH . The longitudinal relation between physical capacity and wheelchair skill performance during inpatient rehabilitation of people with spinal cord injury. Arch Phys Med Rehabil 2005; 86: 1575–1581.
Kilkens OJ, Dallmeijer AJ, Angenot E, Twisk JW, Post MW, Van Der Woude LH . Subject- and injury-related factors influencing the course of manual wheelchair skill performance during initial inpatient rehabilitation of persons with spinal cord injury. Arch Phys Med Rehabil 2005; 86: 2119–2125.
van Drongelen S et al. Upper extremity musculoskeletal pain during and after rehabilitation in wheelchair-using persons with a spinal cord injury. Spinal Cord 2006; 44: 152–159 [E-pub ahead of print: 6 September 2005; doi:10.1038/sj.sc.3101826].
Post MWM . Living with spinal cord injury. A study of health status and life satisfaction of independently living people with a spinal cord injury. Universiteit Utrecht 1997.
Marino R et al. International Standards for Neurological Classification of spinal cord injury, vol. revised 2000. American Spinal Injury Association: Chicago, IL 2000.
van Asbeck FW, Post MW, Pangalila RF . An epidemiological description of spinal cord injuries in The Netherlands in 1994. Spinal Cord 2000; 38: 420–424.
Schönherr MC, Groothoff JW, Mulder GA, Eisma WH . Rehabilitation of patients with spinal cord lesions in The Netherlands: an epidemiological study. Spinal Cord 1996; 34: 679–683.
Raadsen HP, van Asbeck FWA . Over leven met een dwarslaesie. Revalidatiecentrum De Hoogstraat: Utrecht 1990.
Biering-Sorensen E, Pedersen V, Clausen S . Epidemiology of spinal cord lesions in Denmark. Paraplegia 1990; 28: 105–118.
Campos da Paz A, Beraldo PS, Almeida MC, Neves EG, Alves CM, Khan P . Traumatic injury to the spinal cord. Prevalence in Brazilian hospitals. Paraplegia 1992; 30: 636–640.
Celani MG, Spizzichino L, Ricci S, Zampolini M, Franceschini M . Spinal cord injury in Italy: a multicenter retrospective study. Arch Phys Med Rehabil 2001; 82: 589–596.
Garcia-Reneses J, Herruzo-Cabrera R, Martinez-Moreno M . Epidemiological study of spinal cord injury in Spain 1984–1985. Paraplegia 1991; 28: 180–190.
Hart C, Williams E . Epidemiology of spinal cord injuries: a reflection of changes in South African society. Paraplegia 1994; 32: 709–714.
Maharaj JC . Epidemiology of spinal cord paralysis in Fiji: 1985–1994. Spinal Cord 1996; 34: 549–559.
Martins F, Freitas F, Martins L, Dartigues JF, Barat M . Spinal cord injuries – epidemiology in Portugal's central region. Spinal Cord 1998; 36: 574–578.
Nobunaga AI, Go BK, Karunas RB . Recent demographic and injury trends in people served by the Model Spinal Cord Injury Care Systems. Arch Phys Med Rehabil 1999; 80: 1372–1382.
Post MW, De Witte LP, van Asbeck FW, van Dijk AJ, Schrijvers AJ . Predictors of health status and life satisfaction in spinal cord injury. Arch Phys Med Rehabil 1998; 79: 395–401.
Silberstein B, Rabinovich S . Epidemiology of spinal cord injuries in Novosibirsk, Russia. Paraplegia 1995; 33: 322–325.
Soopramanien A . Epidemiology of spinal injuries in Romania. Paraplegia 1994; 32: 715–722.
Ronen J et al. Length of stay in hospital following spinal cord lesions in Israel. Spinal Cord 2004; 42: 353–358.
Tooth L, McKenna K, Geraghty T . Rehabilitation outcomes in traumatic spinal cord injury in Australia: functional status, length of stay and discharge setting. Spinal Cord 2003; 41: 220–230.
Eastwood EA, Hagglund KJ, Ragnarsson KT, Gordon WA, Marino RJ . Medical rehabilitation length of stay and outcomes for persons with traumatic spinal cord injury – 1990–1997. Arch Phys Med Rehabil 1999; 80: 1457–1463.
Acknowledgements
We thank the eight participating rehabilitation centers and especially the research assistants for collecting all the data: Sacha van Langeveld (De Hoogstraat, Utrecht), Annelieke Niezen/Peter Luthart (Rehabilitation Center Amsterdam), Marijke Schuitemaker (Het Roessingh, Enschede), Karin Postma (Rijndam Revalidatiecentrum, Rotterdam), Jos Bloemen (Hoensbroeck Revalidatiecentrum, Hoensbroek), Hennie Rijken (Sint Maartenskliniek, Nijmegen), Ferry Woldring (Beatrixoord, Haren), and Linda Valent (Heliomare, Wijk aan Zee). This study was supported by the Dutch Health Research and Development Council, ZON-MW Rehabilitation program, Grant no. 1435.0003.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
de Groot, S., Dallmeijer, A., Post, M. et al. Demographics of the Dutch multicenter prospective cohort study ‘Restoration of mobility in spinal cord injury rehabilitation’. Spinal Cord 44, 668–675 (2006). https://doi.org/10.1038/sj.sc.3101906
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101906
Keywords
This article is cited by
-
Eye-tracking control of an adjustable electric bed: construction and validation by immobile patients with multiple sclerosis
Journal of NeuroEngineering and Rehabilitation (2023)
-
Real-time motion onset recognition for robot-assisted gait rehabilitation
Journal of NeuroEngineering and Rehabilitation (2022)
-
Risk indicators of length of acute hospital stay after traumatic spinal cord injury in South Africa: a prospective, population-based study
Spinal Cord (2019)
-
Mental health and life satisfaction of individuals with spinal cord injury and their partners 5 years after discharge from first inpatient rehabilitation
Spinal Cord (2018)
-
Prevalence of parenthood in wheelchair-dependent persons with long-term spinal cord injury in the Netherlands
Spinal Cord (2018)