Abstract
Study design: Assessed social support, life stress, and quality of life among degenerative spine disease patients.
Objective: To examine how social support and life stress relate to quality of life following spinal decompression surgery among patients with degenerative spine disease.
Setting: Neurosurgical clinic at Saint Michael's Hospital in Toronto, Canada.
Methods: A total of 19 patients with degenerative spine disease who had undergone spinal decompression surgery within the past 14 months filled out social support, life stress, and quality of life questionnaires. Correlational techniques were used to assess the relations among the variables.
Results: The correlations between social support scores and health-related and nonhealth-related quality of life scores were r=0.72, P=0.001, and r=0.50, P=0.028, respectively. The correlations between life stress scores and health-related and nonhealth-related quality of life scores were r=−0.83, P<0.001, and r=−0.72, P=0.001, respectively.
Conclusions: Degenerative spine disease patients experiencing more social support and less life stress tend to report greater satisfaction in medical outcome and overall quality of life following spinal decompression surgery than those with less social support and more life stress. Assessing social support and life stress in patients with degenerative spine disease and including a consideration of social support and life stress in the management of patients with degenerative spine disease could help to improve patients' satisfaction with their medical outcome and general quality of life following spinal decompression surgery.
Similar content being viewed by others
Introduction
Low back and neck pain are among the five most common reasons that people visit physicians.1,2,3,4 Mechanical disorders such as degenerative spine disease account for 90% of low back and neck pain cases.5 It is therefore clear that degenerative spine disease affects an enormous number of people. Furthermore, degenerative spine disease impacts many areas that have been identified by population health analysts as important determinants of well-being, including personal health practices, coping skills, employment and working conditions, income and social status, social support networks, and health services.6
Researchers have found increased depression, increased anxiety, greater dissatisfaction with one's financial situation, and greater dissatisfaction with relations, including increased family problems, among patients with degenerative spine disease relative to healthy or asymptomatic controls.7,8 The pain and immobility associated with degenerative spine disease can also decrease patients' ability to function at home and at their jobs.9 In fact, people with degenerative spine disease have a four-fold higher incidence of sick leave than healthy controls, and sometimes stop working entirely.10 The psychological distress associated with degenerative spine disease has also been found to decrease patients' motivation for rehabilitation and thus hinder their recovery.11 Patients who believe that their condition entails an incapacity to work have poorer postoperative recoveries regardless of objective medical findings.13 Furthermore, those patients who are unemployed at the time of surgery tend to have poorer postoperative outcomes.14,15
There may also be social incentives that negatively impact patients' recovery. Researchers have found increases in reported pain, disability, and psychological distress among those with chronic low back pain who are also receiving workers' compensation benefits compared to those not receiving benefits.2 Similar findings regarding the influence of secondary gain on the presentation of degenerative spine disease have also been reported by others.16,17,18 This association appears to be stronger among those with lumbar spine disease than among those with cervical spine disease.16
Given the disabling nature of the condition and potential secondary gain influences on recovery, it is not surprising that the economic costs associated with degenerative spine disease are substantial. It has been estimated that the direct health-care costs and indirect costs of lost productivity associated with mechanical back disorders total 8.1 billion dollars annually in Canada, roughly 10% of overall health expenditures.3
The findings described above highlight the significant personal and social impact of degenerative spine disease with respect to the broad determinants of health. In keeping with this broad perspective, some researchers have begun to explore how patients' psychosocial situation impacts their clinical outcomes. For example, life stress and social support have been identified as important variables influencing medical outcome in people with degenerative spine disease.7,8,14,19,20,21 In fact, some studies have shown that life stress and social support predict objective postoperative outcome better than clinical findings or radiologically identified morphological changes in the spine.21,22
Despite these intriguing findings, the relations between life stress, social support, and subjective quality of life among degenerative spine disease patients have not yet been directly studied. The purpose of this study was to examine explicitly those relations.
In this study, ‘social support’ refers to people's network of relations that provide emotional, financial, and practical guidance, assistance, advice, or simply a caring ear. ‘Life stress’ refers to the minor and major hassles in people's lives that can produce feelings of harassment, being overwhelmed, irritability, fatigue, worry, or tension.23 ‘Quality of life’ is a broad concept and one that is increasingly recognized as an important consideration in the management of patients. ‘Quality of life’ can refer to objectively assessable features of a person's current situation such as employment status, salary, and living arrangements; or it can refer to a person's subjective satisfaction with finances, living situation, leisure, relations, and health.24 The emphasis in this study is on participants' subjective assessments of their quality of life.
Research rationale
This study was designed to expand previous findings by directly examining the associations between life stress, social support, and subjective postoperative quality of life in patients who had undergone spinal decompression surgery for degenerative spine disease. Increasing our understanding of how these psychosocial factors influence patients' satisfaction with their medical outcome and overall quality of life will expand our ability to optimize patients' outcomes.
We hypothesized that social support would be positively associated with health-related and nonhealth-related quality of life. That is, it was expected that the more social support that patients report in their lives, the more satisfied they are likely to be with their quality of life following surgery. Furthermore, we hypothesized that life stress would be negatively associated with health-related and nonhealth-related quality of life. That is, it was expected that the more life stress that patients report in their lives, the more dissatisfied they are likely to be with their quality of life following surgery.
Methods
Participants
A total of 19 people with degenerative spine disease who had undergone spinal decompression surgery were recruited to participate in this study between February and March 2000. Eight of the participants were women, and 11 of the participants were men. The participants ranged in age from 27 to 81 years (M=52.4; SD=15.3). Eight of the participants had cervical spine disease; 11 of the participants had lumbar spine disease. Among those with cervical spine disease, there were six cases of spondylosis and two cases of spinal stenosis. Among those with lumbar spine disease, there were 10 cases of spondylosis, two cases of spondylolisthesis, and three cases of spinal stenosis. Four of the participants had more than one type of degenerative lumbar spine disease. The time between surgery and participation in this study ranged from 1 week to 14 months (M=5.5 months; SD=3.7). The patients' participation was voluntary and was not financially compensated.
Measurement of social support
The Duke-UNC Functional Social Support Questionnaire (FSSQ) was used to assess social support.25 The FSSQ is a self-report questionnaire composed of 14 items. A strength of this scale is that it has been designed to assess four dimensions of social support. Items 1, 7, and 11 assess quantity of support (item example: ‘I get visits with friends and relatives’); items 8, 9, and 10 assess confidant support (item example: ‘I get chances to talk to someone I trust about my personal and family problems’); items 4, 5, and 6 assess affective support (item example: ‘I get love and affection’); and items 2, 3, 13, and 14 assess instrumental support (item example: ‘I get help around the house’). Responses were made on a 5-point Likert-type scale from ‘as much as I would like’ to ‘much less than I would like.’ Higher scores on the FSSQ indicate greater social support.
Measurement of life stress
Participants' life stress was assessed with the Perceived Stress Questionnaire (PSQ).23 The PSQ is a 30-item self-report questionnaire assessing the broad domain of life stress. Sample items include: ‘You feel that too many demands are being made on you’, ‘You feel tense’, and ‘Your problems seem to be piling up’. Responses are made on a 4-point scale (1=‘almost never’; 2=‘sometimes’; 3=‘often’; and 4=‘usually’). Higher scores on the PSQ reflect higher levels of life stress.
Measurement of quality of life
Health-related and nonhealth-related quality of life were examined in this study. To assess health-related quality of life, the 12-Item Short Form Health Survey (SF-12) was used.26 The SF-12 is a 12-item abridged version of the Medical Outcome Study 36-Item Short-Form Health Survey self-report questionnaire. The SF-12 provides an overall measure of health-related quality of life and is composed of two subscales. One 6-item subscale assesses physical health-related quality of life (sample item: ‘In general would you say your health is:’; responses are made on a 5-point Likert-type scale from ‘excellent’ to ‘poor’); the other 6-item subscale assesses mental health-related quality of life (sample item: ‘How much of the time during the last 4 weeks have you felt downhearted and blue?’; responses are made on a 6-point Likert-type scale from ‘all of the time’ to ‘none of the time’). Scores can be calculated for the overall scale and the individual subscales. Higher scores on the SF-12 reflect greater satisfaction in one's health-related quality of life.
To assess nonhealth-related quality of life, the Quality of Life Questionnaire (QLQ) was used.24 The QLQ is a 24-item self-report questionnaire covering seven dimensions of quality of life: living situation, finances, leisure, family, social life, health, and access to medical care. In this study, scores for the family, social life, health, and access to medical care dimensions were not calculated. These items were omitted so that the QLQ could provide a measure of nonhealth-related quality of life, and so that the QLQ's relation with the social support measure would not be spuriously inflated. As such, scores were only calculated for the living situation (item example: ‘The living arrangements where you live’), finances (item example: ‘The amount of money you get’), and leisure (item example: ‘The way you spend your spare time’) subscales. Responses were made on a 7-point Likert-type scale from ‘terrible’ to ‘delighted’. Higher scores on the QLQ reflect greater satisfaction with one's nonhealth-related quality of life.
Procedure
Patients attending a follow-up clinic who had recently undergone spinal decompression surgery for degenerative spine disease were asked if they would be willing to participate in this study. Patients who indicated an interest in participating were escorted to a private seating area. All participants were then informed orally and in writing about the nature of the study, that their participation would involve filling out questionnaire and providing the researchers with permission to review their medical files, that their participation was entirely voluntary, that their participation or nonparticipation would, in no way, affect their medical care, and that they could withdraw from the study at any time without consequence.
After answering their questions, we had participants read and sign consent forms.
Participants were provided with a questionnaire package, a clipboard to write on, and a pen or pencil. Participants took from 15 to 30 min to complete the questionnaire package. After they had completed the questionnaire package, we debriefed the participants. This entailed answering any questions they had. Once the participants’ questions had been addressed, we asked them about their experiences and thoughts regarding their condition and treatment. This final discussion period was particularly helpful in addressing the more qualitative and unique aspects of each participant's experience.
This study was reviewed and ethically approved by the Research Ethics Board at Saint Michael's Hospital, Toronto, Canada.
Results
Preliminary analyses
To assess internal consistency, Cronbach's coefficient alpha was calculated for all measures. To obtain an understanding of the general characteristics of the sample, descriptive statistics on all measures were calculated. The coefficient alphas, means, and standard deviations for each measure are listed in Table 1.
As can be seen in Table 1, all of the measures and subscales show high internal consistency. The means and standard deviations for each measure and subscale are similar to those reported in their respective validation studies.23,24,25,26
Main analyses
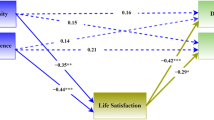
To assess the relations between social support scores, life stress scores, and quality of life scores, Pearson product–moment correlations were calculated with alpha set at 0.05 for each calculation (see Table 2). In accordance with predictions, social support was positively associated with health-related and overall nonhealth-related quality of life. The magnitude of these relations was substantial.
Social support scores accounted for 50% of the variance in the total scores on the SF-12 (r2=0.50, P=0.001), 41% of the variance in the SF-12 physical component summary scores (r2=0.41, P=0.003), and 50% of the variance in the SF-12 mental component summary scores (r2=0.50, P=0.001). Social support scores accounted for 25% of the variance in the total scores on the QLQ (r2=0.25, P=0.028), 31% of the variance in the finances subscale scores (r2=0.31, P=0.013), and 32% of the variance in the leisure subscale scores (r2=0.32, P=0.011). Contrary to predictions, social support scores were not associated with scores on the living situation subscale of the QLQ.
In accordance with predictions, life stress was negatively associated with health-related and overall nonhealth-related quality of life. Like the associations between social support and quality of life, the magnitude of the associations between life stress and quality of life was substantial. Life stress scores accounted for 69% of the variance in the total scores on the SF-12 (r2=0.69, P<0.001), 45% of the variance in the SF-12 physical component summary scores (r2=0.45, P=0.002), and 76% of the variance in the SF-12 mental component summary scores (r2=0.076, P<0.001). Life stress scores accounted for 52% of the variance in the total scores on the QLQ (r2=0.52, P=0.001), 42% of the variance in the finances subscale scores (r2=0.42, P=0.003), and 53% of the variance in the leisure subscale scores (r2=0.53, P<0.001). Contrary to predictions, life stress scores were not associated with scores on the living situation subscale of the QLQ.
Discussion
The results of this study indicate that the more social support and less life stress that patients with degenerative spine disease report in their lives, the more satisfied they are likely to be with their medical outcome and overall quality of life following spinal decompression surgery. These results were consistent across various quality of life domains, including general health, physical health, and mental health, as well as quality of life relating to finances and leisure activities.
Previous research has found that, among people with radiologically identified vertebral disc herniation, life stress tends to be higher in symptomatic participants (those suffering pain and neurological impairments) than in asymptomatic participants.7 Life stress has also been found to be associated with poor objective medical outcomes following spinal decompression surgery.15,21,27 For example, occupational stress has been negatively associated with the likelihood that patients will return to work following spinal decompression surgery for lumbar spondylosis.21
A lack of social support has also been associated with poor objective medical outcomes in patients with degenerative spine disease. For example, among patients who have undergone lumbar disc surgery, those with postoperative medical complaints reported lower satisfaction in family and social support than those patients with no postoperative medical complaints.8,14 More generally, social support has been negatively associated with morbidity among patients with musculoskeletal disorders.7 On a more positive note, social support from a spouse has been positively associated with pain relief up to 2 years after spinal decompression surgery.21
Previous research examining how quality of life relates to spinal decompression surgery highlights the potential benefits of surgery. One study investigated the self-reported postoperative quality of life in patients receiving surgical or nonsurgical treatment for compressive lumbar spine disease. In that study, quality of life was higher in patients undergoing decompression of the Jumbar spine relative to patients who were treated nonsurgically.20
Clearly, the research described above emphasizes the association between life stress, social support, and objective postoperative outcome, as well as the potential benefits of surgery on quality of life. The results of the current study align with and extend these previous findings by increasing our understanding of how life stress and social support relate to subjective satisfaction with medical outcome and overall quality of life among patients with degenerative spine disease.
Limitations
Despite the strong associations found in this study, there are several limitations that need mentioning. First, because the study sample contained only 19 individuals, the results of the study may not be generalizable. That is, although they were statistically significant (suggesting reliability), fortuitous sampling may underlie the results. A larger sample would increase the chance that a representative sample of degenerative spins disease patients was included in the study. The more representative the sample, the more gereralizable the inferences based on that sample will be.
Another limitation of the study is the lack of preoperative social support and life stress information. Including preoperative measurements would help to provide evidence that variation in postoperative objective medical outcome did not influence people's assessment of the social support and stress in their lives. That is, because all of the information was obtained postoperatively, it could be argued that postoperative medical outcome dictated participants’ responses on the social support and life stress questionnaires. If social support and life stress were assessed preoperatively, it could not be argued that participants’ social support find life stress scores were influenced by postoperative medical outcome.
Finally, because this study was correlational, it is important to realize that causal conclusions cannot be drawn. To say that social support causes greater satisfaction in quality of life, or that life stress causes less satisfaction in quality of life, would be inappropriate based on these results.
Future studies
To overcome some of the limitations of this study in future research, a number of considerations are relevant. First, it would be valuable to include more participants in any similar study in the future. Including more participants could help to increase the generalizability of future research findings as described above. It would also be useful to collect data on the patients before and after surgery. This would help to avoid the possibility that variations in medical outcome accounts for differences in social support and life stress self-evaluations. Another valuable addition to future studies would be the inclusion of objective assessments of patients' medical outcome. This information could be used to statistically control for the association between objective medical outcome and quality of life scores. Finally, including the patients of only one surgeon in this study described the possibility that variations in treatment approach or technique accounted for differences in patients' treatment satisfaction. This is a strength of the study. However, future studies involving other surgeons’ patients would help to support generalizability of this study's findings.
Conclusions
The following conclusions are based on the quantitative findings reported in this study and the qualitative findings obtained through patient interviews during the debriefing period. First, the results of this study warrant a consideration among physicians of the possible contribution that social support and life stress make to the natural history and postoperative course of degenerative spine disease. We, therefore, recommend that physicians assess patients' social support and life stress prior to surgery. Furthermore, we recommend that physicians attempt to optimize their patients' social support and decrease their patients' life stress. We obtained a few suggestions on how to do this from patients.
Some patients felt that it would be helpful to include family members in discussions of their condition, needs, progress, and management. These patients felt that they might receive more social support if their families understood their condition better. Similarly, some patients stated that they would have experienced less stress following surgery if they had been provided clear information including reading material on the expected postoperative course of the disease and recovery. Several patients also indicated that family members’ expectations that they continue to conduct housework and food preparation contributed to their stress levels. We recommend that physicians assess the extent to which patients' receive instrumental support at home. It may then be appropriate to arrange home care assistance for patients without adequate support. In speaking to participants, it also became clear that some could benefit from the support of other health-care providers, including mental health practitioners. Broadly assessing patients' needs, and then making appropriate referrals may therefore also help to provide patients the support they require. Finally, we were struck by how much simply listening to patients' concerns helped to diminish their stress and make them feel supported. Our final recommendation is therefore that physicians listen to patients, not just to their reports of localizing neurological symptoms, but also to their unique descriptions of their experience and concerns. By actively listening to patients, physicians will be better able to collaboratively develop individualized strategies to maximize their patients' social support and minimize their life stress.
Summary
The more social support that people with degenerative spine disease experience, the better they feel about their medical outcome and general quality of life following spinal decompression surgery. The less the life stress people with degenerative spine disease experience, the better they feel about their medical outcome and quality of life following spinal decompression surgery. Physicians treating patients with degenerative spine disease should consider how social support and life stress relate to their patients' outcomes following spinal decompression surgery. Physicians should attempt to address social support and life stress issues in the management of patients with degenerative spine disease.
References
Abenhaim L, Suissa S . Importance and economic burden of occupational back pain: a study of 2500 cases representative of Quebec. J Occup Med 1987; 29: 670–674.
Cassisi JE et al. Pain, disability, and psychological functioning in chronic low back pain subgroups: myofascial versus herniated disc syndrome. Neurosurgery 1993; 33: 379–385; discussion 385–386.
Coyte PC, Asche CV, Croxford R, Chan B . The economic cost of musculoskeletal disorders in Canada. Arthritis Care Res 1998; 11: 315–325.
Hart LG, Deyo RA, Cherkin DC . Physician office visits for low back pain: frequency, clinical evaluation, and treatment patterns from a US national survey. Spine 1995; 20: 11–19.
Borenstein DG . Disorders of the low back and neck, In: Klippel JH, Weyand CM, Wortmann RL (eds). Primer on the Rheumatic Diseases, 11th edn. Arthritis Foundation: Atlanta, GA 1997, pp 130–136.
Hamilton N, Bhatti T . Population health promotion: an integrated model of population health and health promotion. Health Promotion Developmemt Division: Ottawa, ON 1996.
Boos N et al. 1995 Volvo Award in clinical sciences. The diagnostic accuracy of magnetic resonance imaging, work perception, and psychosocial factors in identifying symptomatic disc herniations. Spine 1995; 20: 2613–2625.
Dvorak J, Valach L, Fuhrimann P, Heim E . The outcome of surgery for lumbar disc herniation. II. A 4–17 years' follow-up with emphasis on psychosocial aspects. Spine 1988; 13: 1423–1427.
Atlas SJ et al. The Main Lumbar Spine Study, Part II, 1-year outcomes of surgical and nonsurgical management of sciatica. Spine 1996; 21: 1777–1786.
Seferlis T, Nemeth G, Carlsson AM, Gillstrom P . Acute low-back-pain patients exhibit a fourfold increase in sick leave for other disorders: a case–control study. J Spinal Discord 1999; 12: 280–286.
Alaranta H, Hurme M, Miettinen ML . Handicap 1 year following surgery for lumbar disc herniation: special reference to social and vocational factors. Int Rehabil Med 1986; 8: 39–43.
Vucetic N, de Bri E, Svensson O . Clinical history in lumbar disc herniation. A prospective study in 160 patients. Acta Orthop Scand 1997; 68: 116–120.
Nykvist F et al. Clinical, social, and psychological factors and outcome in a 5-year follow-up study of 276 patients hospitalized because of suspected lumbar disc herniation. Int Disabil Stud 1990; 12: 107–112.
Sorensen LV, Mors O . A two-year prospective follow-up study of the outcome after surgery in patients with slipped lumbar disk operated upon for the first time. Acta Neurochir (Wien) 1989; 96: 94–99.
Sorensen LV, Mors O, Skovlund O . A prospective study of the importance of psychological and social factors for the outcome after surgery in patients with slipped lumbar disk operated upon for the first time. Acta Neurochir (Wien) 1987; 88: 119–125.
Kaptain GJ et al. Secondary gain influences the outcome of lumbar but not cervical surgery. Surg Neurol 1999; 52: 217–225.
Keel PJ . Psychosocial criteria for patient selection: review of studies and concepts for understanding chronic back pain. Neurosurgery 1984; 15: 935–941.
Young JN, Shaffrey CI, Laws Jr ER, Lovell LR . Lumbar disc surgery in a fixed compensation population: a model for influence of secondary gain on surgical outcome. Surg Neurol 1997; 48: 552–558; discussion 558–559.
Lang DA, Neil-Dwyer G, Garfield J . Outcome after complex neurosurgery: the caregiver's burden is forgotten. J Neurosurg 1999; 91: 359–363.
Atlas SJ et al. The Main Lumbar Spine Study, Part III. 1-year outcomes of surgical and nonsurgical management of lumbar spinal stenosis. Spine 1996; 21: 1787–1795.
Schade V et al. The impact of clinical, morphological, Psychosocial and work-related factors on the outcome of lumbar discectomy. Pain 1999; 80: 239–249.
Hurme M, Alaranta H . Factors predicting the result of surgery for lumbar intervertebral discherniation. Spine 1987; 12: 933–938.
Levenstein S et al. Development of the Perceived Stress Questionnaire: a new tool for psychosomatic research. J Psychosom Res 1992; 37: 19–32.
Greenley JR, Greenberg JS, Brown R . Measuring quality of life: a new and practical survey instrument. Soc Work 1997; 42: 244–254.
Broadhead WE, Gehlbach SH, de Gruy FV, Kaplan BH . The Duke-UNC Functional Support Questionnaire. Med Care 1988; 26: 709–723.
Ware JE, Kosinski M, Keller SD . A 12-item short form health survey: construction of scales and preliminary tests of reliability and validity. Med Care 1996; 34: 220–233.
Rasmussen C . Lumbar disc herniation: social and demographic factors determining duration of disease. Eur Spine J 1996; 5: 225–228.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Laxton, A., Perrin, R. The relations between social support, life stress, and quality of Life following spinal decompression surgery. Spinal Cord 41, 553–558 (2003). https://doi.org/10.1038/sj.sc.3101432
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101432
Keywords
This article is cited by
-
The Psychological Evaluation of Patients with Chronic Pain: a Review of BHI 2 Clinical and Forensic Interpretive Considerations
Psychological Injury and Law (2014)
-
Psychometric properties of the Patient Activation Measure among individuals presenting for elective lumbar spine surgery
Quality of Life Research (2009)
-
Quality of life after spinal cord injury: a meta-synthesis of qualitative findings
Spinal Cord (2007)