Abstract
Purpose
To compare the level of visual acuity with crowded and uncrowded versions of the logMAR acuity test and the Kay picture test in amblyopia.
Methods
A prospective study was carried out on 51 participants with amblyopia (strabismic n=17; anisometropic n=10; combined n=24), mean age 10 years 8 months. The amblyopia was defined as severe/moderate (<0.250 logMAR), n=41 or mild (⩾0.250 logMAR), n=10. Visual acuity was assessed uniocularly using the crowded and uncrowded logMAR acuity tests and the logMAR crowded and uncrowded Kay picture tests in random orders.
Results
The mean visual acuity outcome using the logMAR crowded Kay picture test (0.343±0.150) was comparable (P=0.084) with the mean outcome using the crowded logMAR acuity test (0.402±0.188). However, the mean acuity difference between these two tests in the subgroup with severe/moderate amblyopia (0.074±0.036) was statistically significant (P=0.0382). The uncrowded logMAR acuity test significantly overestimated visual acuity when compared with the logMAR crowded Kay picture test (P<0.005) by a mean of 0.088±0.008.
Conclusion
The logMAR crowded Kay picture test is a useful tool in clinical practice. The test design takes the crowding phenomenon into account. It provides visual acuity measures more comparable with the gold standard crowded logMAR acuity test than the uncrowded logMAR acuity test. However, the outcomes in poorer acuities should still be viewed with caution.
Similar content being viewed by others
Introduction
Visual acuity (VA) is the primary measure of visual function. An accurate recording of VA in the paediatric patient can result in earlier detection of visual defects and allows precise monitoring of the response to any treatment given.1, 2, 3, 4 Evidence suggests that there is an altered plasticity of the visual system4 indicating that response to treatment seems best when instituted at an early age but becoming poorer after the age of 8 years.1
The crowding phenomenon occurs when an optotype presented in isolation is more easily identified than one presented in a horizontal row of the same sized optotypes. Various theories have been put forward for the crowding phenomenon, for example, that it is the result of contour interaction whereby additional stimulation from adjacent optotypes causes confusion,5, 6, 7, 8 or that a reduction of lateral retinal inhibition may be a causal factor.9 Hess et al10 reported that the phenomenon was linked to the physical characteristics of the stimulus more than the inhibitory interaction. The physiological mechanism of crowding remains unknown. Crowding is suggested to be a part of normal visual development.11, 12 The phenomenon is exaggerated in the presence of amblyopia.5, 8
The sensitivity for amblyopia detection is improved by use of a crowded test.13, 14, 15 The crowded logMAR acuity test (CLT) is now accepted as the gold standard VA measure.16 However, due to ability it is often necessary to use an uncrowded letter test with younger children. Averbeck et al17 investigated two groups of nonamblyopic children: (1) aged 2–5.5 years (n=49), (2) aged 6–16 years (n=52), and found the logMAR crowded Kay picture test (CK) was easier to perform in children below 5 years with acuities comparable with the CLT. Despite this, no previous reports have examined the level of acuity with these two tests using a sample of amblyopic participants.
The principle goal of this study is to use a cross-sectional sample to evaluate the clinical value of the CK in detection of amblyopia.
Materials and methods
A convenient sample of 52 participants was obtained from the patients attending the Orthoptic Department at Sunderland Eye Infirmary between December 2005 and April 2006. Only those with adequate cognitive ability to name letters and a diagnosis of strabismic, anisometropic, or combined amblyopia were eligible. Amblyopia was defined as best corrected visual acuity of 0.1 logMAR or below in one eye and an interocular acuity difference of no less than 0.1 logMAR, when using the CLT. Anisometropia was defined as a difference of ⩾1.00 D best spherical equivalent between two eyes. Participants had all been refracted within the last 2 years.
The cover test was performed to assess ocular alignment. Following this, each participant had their VA assessed uniocularly with either eye using the Keeler crowded (CLT) and uncrowded (ULT) logMAR acuity tests, and logMAR crowded (CK) uncrowded (K) Kay picture tests. Each test was performed and recorded using manufacturers' instructions. A staircase method was used; if two or more optotypes in a line were named correctly the next card in the series was presented, if no optotypes were named correctly the observer reverted back to the previous line for the participant to name the remaining optotypes. Only one reversal took place at each acuity level. The VA was recorded in logMAR units for the number of optotypes the participant identified correctly. The standard test distance was increased or decreased to assess higher and lower acuities respectively by the use of a regular geometric progression ratio. The order in which these tests were performed was randomised using a random table of 16 orders. The random table also determined which eye was tested first for each participant. This remained constant throughout the four vision tests they performed.
Each participant performed all tests in one single session. All practical aspects of the study were carried out by one author (ME).
The sample was subdivided according to the aetiology of amblyopia (strabismic, anisometropic, and combined) and severity of amblyopia, based on the level of acuity of the amblyopic eye (severe ⩽0.6 logMAR, moderate >0.6 and <0.250 logMAR, mild ⩾0.250 logMAR).18
The study was approved by the Northumberland Local Research Ethics Committee and consent was taken from all participants prior to the commencement of the study. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during this research.
Statistical analysis
The number of participants required to obtain a power of 80% at the 5% level (two tailed) for an effect size of 0.2 log units was calculated as 48.
Paired t-tests were used to evaluate the comparison in acuity measures between the vision tests, and the Pearson's product–moment correlation coefficient was used to evaluate the strength of association between tests.
Results
Fifty-two participants (22 women, 30 men) aged between 5 years 1 month and 45 years 10 months (mean age 10 years 8 months) took part in the study. Forty-seven participants wore glasses. One participant was excluded from the analysis because the interocular acuity difference was less than required. Results for 51 participants are therefore reported.
Table 1 shows the mean VA outcomes with the CLT, ULT, CK and the K.
When comparing CLT and CK (Table 1), the mean difference was 0.059, this was not statistically significant (t=1.74; d.f.=100; P=0.084).
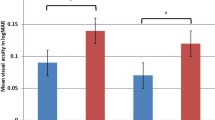
Seven participants had severe amblyopia. For statistical analysis, they were combined with the moderate amblyopic group. Table 2 shows the mean VA with CLT, ULT, CK, and K in severe/moderate amblyopia (n=41) and mild amblyopia (n=10).
When comparing CLT and CK, the difference between the two tests was not statistically significant in mild amblyopia (t=0.818; d.f.=18; P=0.94) but was statistically significant in severe/moderate amblyopia (F=4.562; d.f.=1; P=0.0382).
The correlation between CLT and CK is significant (P<0.001). Figure 1 shows the correlation with the line of association indicating that as acuity deteriorates the level of VA with CLT is worse.
The mean difference between CK and ULT (Table 1) was 0.088. This was found to be statistically significant (t=−2.84; d.f.=100; P=0.005), with the lower acuity being obtained with CK.
Table 3 shows the mean VA outcomes with CLT, ULT, CK, and K in three aetiologies of amblyopia, strabismic (n=17), anisometropic (n=10), and combined (n=24). Statistical analysis was not performed due to the low numbers in groups.
Discussion
The aim of this study was to evaluate the use of the logMAR acuity and Kay picture tests in uncrowded and crowded forms in amblyopic participants. We found no difference in the levels of acuity with the two crowded tests for the group of amblyopic participants as a whole, but did find a slight overestimation of about three optotypes by the CK when we excluded the participants with mild amblyopia. This level of difference is only bordering on clinical significance. Two lines difference in visual acuity is frequently considered as the criterion for diagnosis of amblyopia, but we would consider one line (4 optotypes) to be clinically significant and suggestive that the review of acuity is required. As children ‘progress’ through the vision tests our data suggest that the level of acuity gained on the CK is much more similar to the gold standard of CLT than the uncrowded letter test. This suggestion is also sensible for the participants with mild amblyopia where no difference was found between the two crowded tests, but mean acuity was better with the ULT.
Previous literature describing comparison between these two vision tests is sparse. The results of our study support the suggestions of Averbeck et al,17 who found mean monocular acuities were higher with the CK (0.01), but reported to be comparable with the CLT (0.08, 0.09). However, their study differed from our research as the population sample consisted of nonamblyopic participants with a different age range (2–16 years).
To our knowledge, no other research has concentrated on the factors described in this study. However, as previously stated, there is literature to support the suggestion that the magnitude of the crowding effect increases with poorer acuity.5, 6 Rodier et al19 evaluated 35 amblyopic participants using a jumbled picture array test and a single picture test. Acuities were poorer with the jumbled array and this was found to be related to the acuity level, with an increase in the crowding effect with decreased acuity level. Morad et al8 studied mild amblyopia where the worst acuity was 6/16 on a crowded test. They acknowledge that studying deeper amblyopia may produce an even more pronounced crowding effect when comparing chart, line, and single optotype acuity.
The visual acuity outcomes we found with the various tests do not appear to be affected by the aetiology of amblyopia. Other literature has stated that the crowding effect is similar in all types of amblyopia.20 Rodier et al19 found that the type of amblyopia had no effect on the crowding phenomenon but acknowledge the sample studied was small (n=35), and unevenly distributed between the aetiologies studied possibly resulting in any interaction being masked. Similar limitations to those described by these authors are evident in this study. A larger sample size would be required to increase the external validity and reliability of this study.
The study also found that the ULT significantly overestimates acuity when compared with the CK. There is no other evidence to support this finding although the suggestion is clinically significant as the two tests are recommended for the same age group. Therefore, progression directly from a crowded picture test to a crowded letter test may provide more comparable acuity measures when assessing young children, particularly where there is poorer acuity.
Large amblyopia treatment trials have been carried out to establish the effectiveness of occlusion therapy.1, 2, 4 These studies rely on an accurate measure of VA at specific intervals within the trial to provide information on optimum patching and factors predictive of improvement in the amblyopic eye.1 Often the studies have a lower age limit of 3 years because of the vision tests used. However, if the CK is comparable with the tests used, it may be possible to collect evidence from younger children also. This may result in a shorter duration of occlusion therapy making the implementation of patching easier for parents.
This study shows that the CK is a useful tool when assessing the VA of young children in clinical practice as detection of the crowding phenomenon is reflected in its design. The research suggests that consideration be given to the use of the CK in preference to the ULT to provide acuity measures more comparable with the gold standard acuity test. However, the clinician should be aware that the true density of amblyopia might still be masked when using this test with patients who have poorer acuities.
References
Pediatric Eye Disease Investigator Group. A randomized trial of prescribed patching regimens for treatment of severe amblyopia in children. Ophthalmol 2003; 110: 2075–2087.
Pediatric Eye Disease Investigator Group. A randomized trial of patching regimens for treatment of moderate amblyopia in children. Arch Ophthalmol 2003; 121: 603–611.
Pediatric Eye Disease Investigator Group. A randomized trial of atropine vs patching for treatment of moderate amblyopia in children. Arch Ophthalmol 2002; 120: 268–278.
Stewart CE, Stephens DA, Fielder AR, Moseley MJ . Modelling dose–response in amblyopia: toward a child-specific treatment plan. Invest Ophthalmol Vis Sci 2007; 48: 2589–2594.
Stuart JA, Burian HM . A study of separation: its relationship to visual acuity in normal and amblyopic eyes. Am J Ophthalmol 1962; 53: 471–477.
Flom MC, Weymouth FW, Kahenman D . Visual resolution and contour interaction. J Opt Soc Am 1963; 53: 1026–1032.
Flom MC . Contour interaction and the crowding effect. Prob Optom 1991; 3: 237–257.
Morad Y, Werker K, Nemet P . Visual acuity tests using chart, line, and single optotype in healthy and amblyopic children. J AAPOS 1999; 3: 94–97.
Kavassy A, Kaufmann H In: Von Noorden GK, Campos EC (eds). Binocular Vision and Ocular Motility: Theory and Management of Strabismus. 6th ed. Mosby: St Louis, 2001, p 226.
Hess RF, Dakin SC, Kapoor N . The foveal ‘crowding’ effect: physics or physiology. Vision Res 2000; 40: 365–370.
Atkinson J, Anker S, Evans C, McIntyre A . The Cambridge crowding cards for pre-school visual acuity testing. In: Lenk-Schafer M (ed). Orthoptic Horizons. Trans Sixth Internat Orthopt Congress 1987, pp 482–486.
Atkinson J, Anker S, Evans C, Hall R, Pimm-Smith E . Visual acuity testing in young children with the Cambridge crowding cards at 3 and 6 years. Acta Ophthalmol 1988; 66: 505–508.
Simmers AJ, Gray LS, Spowart K . Screening for amblyopia: a comparison of paediatric letters tests. Br J Ophthalmol 1997; 81: 465–469.
Simmers AJ, Gray LS, McGraw PV . Comparison between methods of threshold estimation in the measurement of visual acuity. Br Orthopt J 1999; 56: 37–44.
Stewart C . Comparison of snellen and log-based acuity scores for school-aged children. Br Orthopt J 2000; 57: 32–38.
Stewart C . Use of logMAR charts for the measurement of visual acuity in orthoptic departments throughout the UK. Br Orthopt J 2002; 59: 53–56.
Averbeck K, Jones D, Westall C . A comparison of two logMAR-based crowded visual acuity tests for the assessment of vision in children (Poster). Optom Vis Sci 2000; 77: 280.
Stewart CE, Fielder AR, Stephen DA, Moseley MJ . Treatment of unilateral amblyopia: factors influencing visual outcome. Inves Ophthal Vis Sci 2005; 46: 3152–3160.
Rodier DW, Mayer DL, Fulton AB . Assessment of young amblyopes: array vs single picture acuities. Ophthalmol 1985; 92: 1197–1202.
Ansons AM, Davis H . Chapter 4—visual function. In: Diagnosis and Management of Ocular Motility Disorders. 3rd ed. Blackwell Science: Oxford, 2001, pp 41–73.
Acknowledgements
We would like to thank Dr David Buckley and Mr Paul McKeen for statistical advice, and Glenys Smithson and the orthoptic team at Sunderland Eye Infirmary for support throughout the study and involvement in the recruitment of participants.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Elliott, M., Firth, A. The logMAR Kay picture test and the logMAR acuity test: a comparative study. Eye 23, 85–88 (2009). https://doi.org/10.1038/sj.eye.6702990
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702990
Keywords
This article is cited by
-
Use of log-scaled crowded visual acuity charts in clinical studies regarding amblyopia
Graefe's Archive for Clinical and Experimental Ophthalmology (2019)
-
Prescribed computer games in addition to occlusion versus standard occlusion treatment for childhood amblyopia: a pilot randomised controlled trial
Pilot and Feasibility Studies (2015)
-
Visual attention to print-salient and picture-salient environmental print in young children
Reading and Writing (2015)
-
Initial Ophthalmic Findings in Turkish Children with Autism Spectrum Disorder
Journal of Autism and Developmental Disorders (2015)
-
Validation of printed and computerised crowded Kay picture logMAR tests against gold standard ETDRS acuity test chart measurements in adult and amblyopic paediatric subjects
Eye (2012)