Abstract
Aims
To re-evaluate the cost-effectiveness of photodynamic therapy with verteporfin (Visudyne®, Novartis AG, Switzerland) in patients with predominantly classic and classic choroidal neovascularization (CNV) owing to age-related macular degeneration (AMD), using new evidence on the impact of contrast sensitivity on health status.
Method
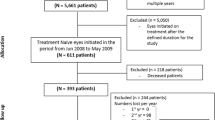
A health economic model is used to synthesise the evidence on contrast sensitivity and treatment rates from the TAP Investigation with health state utilities and costs. Impairment of visual function is estimated using a Markov model to predict transitions between states of contrast sensitivity. Each state is associated with costs and a health state utility. Total expected costs and benefits for a cohort of patients over a defined number of cycles are calculated. The expected health state utility for each disease state was estimated using results from a study of 209 patients with AMD in Sheffield. The model includes the costs associated with treatment and monitoring in the verteporfin treatment arm and costs offset by delaying the deterioration of visual function.
Results
Beyond 3 years, the annual costs of the verteporfin arm are estimated to be less than the annual costs of the control arm, owing to the cost associated with higher blindness prevalence in the control arm. Over time, the results show that both the incremental utility and cost decreases. By 10 years, the estimated incremental cost-effectiveness is approximately £20 996 per Quality-Adjusted Life Years.
Conclusion
The results of this study suggest that the verteporfin therapy in the treatment for patients with predominantly classic and classic CNV owing to AMD is encouraging.
Similar content being viewed by others
Introduction
Age-related macular degeneration (AMD) is characterised by damage to the central part of the retina, which causes severe and irreversible visual impairment resulting in the loss of central vision. AMD affects adults from the age of 50 years and is the leading cause of blindness in people older than 65 years in the developed world.1 The neovascular (or wet) form of the disease is the most serious and is characterised by choroidal neovascularization (CNV), which often quickly progresses to form a disciform scar.2 CNV may be one of two types: classic or occult; classic CNV has generally a poorer prognosis to sight and is associated with faster progression to blindness than occult CNV.2
Until the advent of photodynamic therapy (PDT) with verteporfin (Visudyne®, Novartis AG, Switzerland), there was no treatment option for a majority of patients with subfoveal CNV due to AMD. Laser photocoagulation was the only proven treatment at the time, although it led to damage of the retina associated with absolute scotoma and immediate visual acuity loss, and was therefore only made available for selected patients with very small classic subfoveal CNV.3 PDT with verteporfin has demonstrated efficacy in preventing disease progression in two randomised controlled trials,4, 5 and has been seen to be particularly effective in the subgroup of patients with predominantly classic CNV where the classic component covers at least 50% of the entire lesion.4
The annual costs of blindness to society in the UK have been estimated to be in the region of £4.9 billion.6 A therapy that substantially reduces the progression of visual impairment could be expected to lead to reductions in resource use as well as maintaining the population's quality of life. Given the cost of verteporfin therapy can be as much as £9000 per patient in the first year of treatment, there is a necessity for budget holders to consider the cost-effectiveness as well as the safety and efficacy of the treatment.
In September 2003, the National Institute for Health and Clinical (NICE) recommended the use of PDT for AMD in patients with classic CNV and with predominantly classic CNV (as part of ongoing or new clinical studies for the latter group). A number of published analyses on verteporfin therapy which calculated incremental cost-effectiveness ratios (ICERs) were used by the appraisal committee to inform their decision making.7, 8, 9, 10 To calculate an ICER, the efficacy of treatment is estimated using quality adjusted life years (QALYs) where both the quality and quantity of life is combined in a single unit. The benefit of using QALYs is that rational decisions about allocation of resources can be made across treatments and disease areas.11 Health professionals and the organisations that employ them are expected to implement clinical guidance from NICE. In this way, cost-effectiveness estimates can impact on the treatment decision made by clinicians. NICE is due to review its guidance on PDT in September 2006.
Health state utility values used to determine quality of life were not measured directly in the primary randomised controlled trial of verteporfin therapy, the TAP Investigation.4 Therefore, all previous cost-effectiveness studies have used the trial results of visual acuity to estimate the number of QALYs gained by verteporfin therapy by using a study by Brown et al12 which observed decreasing utility, measured using the Time Trade Off (TTO) technique, for worsening states of visual acuity in patients with AMD. However, the TAP Investigation demonstrated that verteporfin therapy was an effective treatment in halting the deterioration of contrast sensitivity as well as visual acuity.13 Whereas visual acuity measures the eye's ability to resolve fine detail at high contrast, contrast sensitivity measures the ability to perceive differences between light and dark.14 A recent study has demonstrated that reduced contrast sensitivity has not only an important impact on AMD patients' quality of life, but, that it may actually explain more of the impact on quality of life than visual acuity.15, 16 This new evidence superseded previous economic analyses of verteporfin therapy which looked solely at visual acuity. In addition, there are now data from an open-label extension study of patients remaining on verteporfin therapy beyond the initial 2 years of the controlled TAP Investigation, for a duration of up to 5 years.17 This paper explores how this new evidence impacts on the cost-effectiveness of treatment in AMD patients with predominantly classic CNV in the UK.
Method
A health economic model with health state utilities and costs was used to synthesise the evidence on contrast sensitivity and treatment rates from the TAP Investigation. As there is no other proven treatment for this patient group with long-term follow-up up to 5 years, verteporfin therapy was compared to a strategy of best supportive care.
The TAP Investigation included a total of 609 patients with subfoveal CNV caused by AMD which measured 5400 μm or less in greatest linear dimension with evidence of classic CNV, and a best corrected visual acuity of approximately 20/40 to 20/200 Snellen equivalent.4 A total of 242 patients presented with predominantly classic and classic CNV and their demographics are described in Table 1. In the TAP Investigation, patients were followed up at 3-month time intervals. At each follow-up, a fluorescein angiography was performed and treatment with verteporfin therapy was applied if fluorescein leakage from CNV was observed.
The progression of disease is described using a Markov model.18 In such models, distinct and mutually exclusive disease states are defined. The development of the disease is then represented by the movement of patients between these states over time (transition matrices), and changes due to treatment are calculated as the changes in the transitions between states. The states are associated with costs and a health state utility, and total expected costs and outcome for a cohort of patients over a defined number of cycles are calculated. A 10-year time-frame was chosen to adhere with guidelines that state the time horizon of an analysis should be long enough to capture all important differences in long-term effects and health-related resources between the target technology and its comparator.19
We chose states of contrast sensitivity which (i) distinguished between different levels of visual function, (ii) made sense in terms of clinical practice (ie based on the Pelli–Robson chart which is used to measure contrast sensitivity20), and (iii) were populated by sufficient patients to make estimates robust. The states were defined in terms of the contrast sensitivity of the study eye. The contrast sensitivity states and the distribution of patients between the states at baseline are described in Table 2. Transition matrices were developed for each 3-month time interval for the first 4 years and then a final transition from years 4 to 5. These transition matrices were based on patient level data from the TAP Investigation, which provided 5 years of patient follow-up. Detail on the extrapolation of data to 10 years for both strategies is discussed further in the Supplementary appendix.
Health-related quality of life was determined using the Health Utilities Mark III (HUI3), an instrument which produces societal health state utility scores, used in QALY calculations.21 In a study of 209 patients with AMD in Sheffield, patients' visual acuity, contrast sensitivity (measured with both eyes open), and demographics were measured and the HUI3 questionnaire was administered.15 Further analyses of the data were performed to populate the model.16 Using multivariate regressions, explanatory variables for the level of HUI3 utility were found to be contrast sensitivity (B=0.09, P=0.05) and age (B=−0.01, P<0.01).16 Visual acuity added no statistically significant further explanation (B=−0.02, P=0.69).16 These results were used to estimate HUI3 utility values for each contrast sensitivity state for the different ages in the TAP Investigation.
Two types of costs were included in the model; costs associated with treatment and monitoring in the verteporfin treatment arm and costs offset by delaying deterioration of visual function. The rate of verteporfin treatments was calculated from the 5-year data of the TAP Investigation and TAP extension study. Patients receiving further treatment incurred the costs of verteporfin infusion, laser use, fluorescein angiography, and an outpatient appointment (£1181 first visit, £1113 subsequent).8 When patients reach a state equivalent to a visual acuity of 20/200, we apply an annual cost of blindness estimated to be £6455 in the first year and £6295 in subsequent years.22 These blindness costs have been estimated for patients who are blind as a consequence of AMD and are assumed to apply equally to patients who are blind regardless of whether they received PDT or not.
Given the small number of patients used to populate the model, we incorporated the uncertainty in all model parameters by fitting appropriate probability distributions. Probabilistic sensitivity analysis is performed by using Monte Carlo simulation to randomly sample each parameter from its described uncertainty distribution.23 Further details on quality of life, resource use, and model formulation are given in the Supplementary appendix.
Results
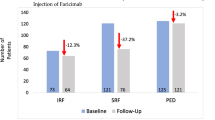
The model formulation allowed for a robust estimate of cost-effectiveness to be made at 10 years. Figure 1 shows the results of the model alongside the actual trial data. The number of patients on treatment is shown below the x axis. As seen in the trial, patients on verteporfin therapy remain around the contrast sensitivity score of 1 log unit, whereas the control group shows a rapid deterioration in the first 6 months before stabilising at a contrast sensitivity close to 0.7 log units. The model predicts that in the verteporfin treatment arm, at year 5 (60 months), half of the surviving cohort (60% of the starting cohort) has withdrawn from treatment (this was expected as half of the patients initially enrolled in the verteporfin arm of the TAP trial had withdrawn by 5 years and mortality in the trial was very low at 5 years). The mean contrast sensitivity for the treatment arm includes contributions from patients who have withdrawn, and are assumed to follow control transitions, and from patients who have not withdrawn and are assumed to follow verteporfin transitions. It is therefore intuitively sensible that it lies halfway between the mean contrast sensitivity for the control arm and the mean contrast sensitivity of the treatment arm when excluding withdrawn patients. At 10 years, all but 15 patients in the verteporfin treatment arm have withdrawn from treatment. This is partly due to the modelled mortality, as by 10 years only 52% of the starting cohort modelled are alive.
Estimated costs are shown in Figure 2. Treatment costs fall off over time as fewer patients require additional treatment at each 3-month visit and more patients withdraw from treatment. By 5 years, treatment costs are predicted to be below 1% of their initial value. Blindness costs increase in both arms during the first 2 years owing to declining vision. In the control arm, the proportion of patients estimated to have become blind has increased to above 68% by the second year, whereas in the treatment group this value reaches 68% only by the ninth year. The increase in costs in both study arms halts after 2 years when mortality within the cohort is greater than the increase in blindness, causing blindness costs to decrease. Beyond 3 years, the costs of blindness in the placebo arm are greater than the total cost of the verteporfin treatment arm.
Over time, the results show that both incremental utility and cost decrease. The difference in utility between the two arms is largest at 2 years (0.044) but has narrowed by 10 years (0.021). Importantly, the ratio between incremental cost and incremental QALY decreases over time. The central cost-effectiveness results are given in Table 3. By 10 years, the estimated incremental cost-effectiveness is approximately £20 996 per QALY.
The cost-effectiveness plane in Figure 3 shows the results of the probabilistic sensitivity analysis at 2 and 10 years. Each point represents what the mean cost-effectiveness ratio could be. The uncertainty we have over the longer term effectiveness of treatment is demonstrated in the larger spread of results at 10 years in comparison to a smaller spread at 2 years. At 10 years, 42% of the sample lies below the £20 000/QALY threshold, whereas 79% lies below the £30 000/QALY threshold. One-way sensitivity analyses are shown in Table 4.
Cost-effectiveness plane of incremental costs and QALYs for PDT with verteporfin vs best supportive care at 2 and 10 years. Each point represents a sample. The proportion of points under the willingness to pay thresholds (30 000/QALY, 20 000/QALY, and 20 000/QALY) represent the probability the intervention is cost effective. The midpoint of the samples represents the central estimate.
Discussion
Contrast sensitivity is recognised as an important measure of visual function in patients with subfoveal CNV secondary to AMD.24 It is also a better indicator of impairment in quality of life in comparison to visual acuity,15 outdating previous economic analyses of verteporfin which are all based on visual acuity. We subsequently revaluated the cost-effectiveness of verteporfin. The results suggest that verteporfin therapy is potentially not only an effective, but also a cost-effective treatment for patients with predominantly classic and classic CNV due to AMD. The analysis uses the Health Utilities Index to estimate QALY gain, and so is the first analysis of verteporfin therapy to use a social estimate of health state utility as apposed to a direct evaluation using the TTO or Standard Gamble. Social estimates are preferred by many decision makers across the world.19, 25 NICE prefer English and Welsh measures of this social value, that is, the EQ5D or SF6D, whereas the HUI3 has been evaluated on a Canadian general population sample. However, it has been demonstrated that while the HUI3 can discriminate between changes in visual impairment, the EQ5D and SF6D cannot.15
Whether verteporfin is indeed a cost-effective use of resources depends on the perspective of the health-care payers. Whether an effective yet expensive intervention is cost effective is dependent on the decision makers' willingness to pay for additional health benefit (eg QALYs). The value of this threshold should reflect a societal judgement, but in practise this is difficult to quantify. In the UK, NICE informally uses values of between £20 000 and £30 000 per QALY.19 Even if the treatment is deemed cost effective, it is likely that affordability will limit the use of these treatments. Given the high cost of treatment combined with the relatively high incidence of AMD, decision makers will have to decide whether the budget used for verteporfin could provide more additional QALYs if spent elsewhere.
There are a number of limitations to this study. Firstly, the results of this study are based on a single trial with a limited number of patients. This means that some transition states are based on very few patient numbers. However, it was more appropriate to model the full range of health states and associated utility values seen in the study, than to limit the range and potentially underestimate the benefit of treatment. Secondly, the result is also based on extrapolating benefit beyond the currently available evidence. This is justified given that at 5 years, the point at which we currently have data, the model suggests that some patients are still benefiting from treatment. If the model was stopped at 5 years, it would make the unlikely assumption that all benefits after this time point were lost instantaneously. There are some assumptions in the model whose accuracy is unknown and would be difficult to verify through future data collection. For example, we have assumed that verteporfin-treated patients withdrew from the trial due to a lack of efficacy, whereas this could have been due to other reasons. We have explored many of these weaknesses in the sensitivity analysis, and incorporated the uncertainty in many parameters within the model. Consequently, the results show a large amount of uncertainty, particularly at 10 years. However, the probability that treatment is cost-effective remains high (Figure 3).
Thirdly, apart from the probabilistic sensitivity analysis, we performed a one-way sensitivity analysis on important variables (Table 4), which showed that the model is particularly sensitive to changes in the costs of blindness. The lower estimate demonstrates a 48% increase in the ICER, whereas the upper estimate suggests that verteporfin might be cost saving. The model is less sensitive to changes in treatment costs and is not particularly sensitive to the duration of follow-up after leakage ceases. The effect of using the TTO to estimate the QALY gain instead of the HUI-3 was explored using TTO data from the Sheffield study. This decreased the incremental QALY, increasing the ICER by some 80%. Comparing this figure with previous cost-effectiveness studies is difficult, as the type of TTO used in the Sheffield study differs to that reported by Brown et al.12 Previous analyses of verteporfin therapy have analysed different subgroups, in particular according to their visual acuity at baseline of the study. Although intuitively it makes sense that treating patients earlier before impairment progresses would be a more cost-effective strategy, we found that the model became unstable in predicting such outcomes due to the very small patient numbers in certain subgroups.
Finally, another important assumption we made was that contrast sensitivity measured with both eyes open is equivalent to the contrast sensitivity of the better seeing eye, and that the treated eye is the better seeing eye. In subjects with normal vision, binocular contrast sensitivity is generally better than monocular contrast sensitivity indicating summation of contrast in the two eyes.26 However, in patients with AMD this summation is reduced and can even be reversed.27 There is evidence to suggest that around one-half of older people with AMD have lower contrast sensitivity when measured with both eyes open than when measured for their better eye alone,27 which is known as binocular inhibition. By using best eye CS as a proxy for binocular CS, our model will overestimate the utility benefit of treating those with binocular inhibition and underestimate the benefit of treating those with binocular summation by a factor given by the square of the ratio of binocular CS to best eye CS (where these are measured in log units).28 This is unlikely to have a large impact on the cost-effectiveness results if half of the patients have binocular summation and half have binocular inhibition as these have opposite effects.
Validating the results of the analysis with other published economic analyses is particularly difficult given the differences in the instrument for obtaining estimates of QALY gain and methodology for extrapolation. However, in terms of the costs, Smith et al9 found similar costs of £4590 in the placebo arm and £8878 in the verteporfin treatment arm at 2 years (mean starting visual acuity of 20/100). At 5 years, the Smith model has higher costs reflecting the way blindness costs dominate analyses at this point and as the Smith model includes transfer payments, which are generally excluded from cost-effectiveness evaluations as they do not reflect resource use, contributing to higher blindness costs.
The results of this study highlight a number of areas requiring further research. We have not looked at adverse events and their impact on costs and quality of life. Although the number of adverse events in the TAP Investigation was very low, this could affect the cost-effectiveness. In addition, we have not examined other social costs and utilities. Recent research suggests that lost productivity owing to visual impairment equals £1.1 billion and the cost of care provided by friends and family could be as much as £1.5 billion.6
Of greatest importance is the further research required on the epidemiology of contrast sensitivity. Many studies have focussed on the deterioration of visual acuity and its relationship with clinical markers, whereas contrast sensitivity has so far received much less attention. As new treatments for AMD emerge, understanding the long-term effect of altering the patient's impairment in contrast sensitivity will become more important. At present, with the data that we have available to us, the cost-effectiveness of verteporfin therapy appears encouraging.
References
Fine SL, Berger JW, Maguire MG, Ho AC . Age-related macular degeneration. N Engl J Med 2000; 342: 483–492.
Arnold JJ, Sarks JP, Killingsworth MC, Kettle EK, Sarks SH . Adult vitelliform macular degeneration: a clinicopathological study. Eye 2003; 17 (6): 717–726.
Macular Photocoagulation Study Group. Visual outcome after laser photocoagulation for subfoveal choroidal neovascularization secondary to age-related macular degeneration. The influence of initial lesion size and initial visual acuity. Arch Ophthal 1994; 112 (4): 480–488.
Bressler NM, Treatment of Age-Related Macular Degeneration with Photodynamic Therapy (TAP) Study Group. Photodynamic therapy of subfoveal choroidal neovascularization in age-related macular degeneration with verteporfin: two-year results of 2 randomized clinical trials—TAP report 2. Arch Ophthal 2001; 119 (2): 198–207.
Verteporfin in Photodynamic Therapy Study Group. Verteporfin therapy of subfoveal choroidal neovascularization in age-related macular degeneration: two-year results of a randomized clinical trial including lesions with occult with no classic choroidal neovascularization—verteporfin in photodynamic therapy report 2. Am J Ophthalmol 2001; 131 (5): 541–560.
Winyard S . Campaign Report 23: The Cost of Sight Loss in the UK. RNIB. 2004.
Sharma S, Brown GC, Brown MM, Hollands H, Shah GK . The cost-effectiveness of photodynamic therapy for fellow eyes with subfoveal choroidal neovascularization secondary to age-related macular degeneration. Ophthalmology 2001; 108 (11): 2051–2059.
Meads C, Salas C, Roberts T, Moore D, Fry-Smith A, Hyde C . Clinical effectiveness and cost-utility of photodynamic therapy for wet age-related macular degeneration: a systematic review and economic evaluation. Health Technol Assess 2003; 7 (9): 1–98.
Smith DH, Fenn P, Drummond M . Cost effectiveness of photodynamic therapy with verteporfin for age related macular degeneration: the UK case. Br J Ophthalmol 2004; 88 (9): 1107–1112.
Hopley C, Salkeld G, Mitchell P . Cost utility of photodynamic therapy for predominantly classic neovascular age related macular degeneration. Br J Ophthalmol 2004; 88 (8): 982–987.
Drummond MF, O'Brien BJ, Stoddart GL, Torrance GW . Methods for the Economic Evaluation of Health Care Programmes. Oxford University Press: Oxford, 1997.
Brown GC, Sharma S, Brown MM, Kistler J . Utility values and age-related macular degeneration. Arch Ophthal 2000; 118 (1): 47–51.
Rubin GS, Bressler NM, Treatment of Age-Related Macular Degeneration with Photodynamic Therapy (TAP) Study Group. Effects of verteporfin therapy on contrast sensitivity: results from the Treatment of Age-Related Macular Degeneration with Photodynamic Therapy (TAP) investigation—TAP Report no 4. Retina 2002; 22 (5): 536–544.
Rubin GS . Assessment of visual function in eyes with visual loss. Ophthalmol Clin North Am 1989; 2: 357–367.
Espallargues M, Czoski-Murray C, Bansback N, Carlton J, Lewis GM, Hughes LA et al. The impact of age related macular degeneration on health state utility values. Invest Ophthalmol Vis Sci 2005; 46 (11): 4016–4023.
Bansback N, Czoski-Murray C, Carlton J, Lewis GM, Espallargues M, Hughes LA et al. Determinants of health related quality of life and health state utility in patients with age related macular degeneration: the association of contrast sensitivity and visual acuity. Qual Life Res 2006, (in press).
Blumenkranz MS, Bressler NM, Bressler SB et al. Verteporfin therapy for subfoveal choroidal neovascularization in age-related macular degeneration: three-year results of an open-label extension of 2 randomized clinical trials—TAP Report no. 5. Arch Ophthalmol 2002; 120 (10): 1307–1314.
Briggs A, Sculpher M . An introduction to Markov modelling for economic evaluation. Pharmacoeconomics 1998; 13 (4): 397–409.
National Institute for Clinical Excellence. Guide to the Methods of Technology Appraisal. National Institute for Clinical Excellence: London, UK, 2004.
Pelli DG, Robson JG, Wilkins AJ . The design of a new letter chart for measuring contrast sensitivity. Clin Vision Sci 1988; 2: 187–199.
Feeny D, Furlong W, Torrance GW, Goldsmith CH, Zhu Z, DePauw S et al. Multiattribute and single-attribute utility functions for the health utilities index mark 3 system. Med Care 2002; 40: 113–128.
Meads C, Hyde C . What is the cost of blindness? Br J Ophthalmol 2003; 87: 1202–1204.
Briggs A . Handling uncertainty in cost-effectiveness models. Pharmacoeconomics 2000; 17 (5): 479–500.
Mones J, Rubin GS . Contrast sensitivity as an outcome measure in patients with subfoveal choroidal neovascularisation due to age-related macular degeneration. Eye, advance online publication, 1 October 2004 (DOI 10.1038/sj.eye.6701717).
Gold MR, Siegel JE, Russell LB, Weinstein MC . Cost-Effectiveness in Health and Medicine. Oxford University Press: Oxford, 1996.
Rabin J . Two eyes are better than one: binocular enhancement in the contrast domain. Ophthalmic Physiol Opt 1995; 15 (1): 45–48.
Valberg A, Fosse P . Binocular contrast inhibition in subjects with age-related macular degeneration. JOpt Soc Am A Opt Image Sci Vision 2002; 19 (1): 223–228.
Faubert J, Overbury O . Binocular vision in older people with adventitious visual impairment: sometimes one eye is better than two. J Am Geriatr Soc 2000; 48 (4): 375–380.
Acknowledgements
We thank Martin McKibbon (Leeds) for help in determining clinical pathway. NOVARTIS provided financial support for this project.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on Eye website (http://www.nature.com/eye).
Supplementary information
Rights and permissions
About this article
Cite this article
Bansback, N., Davis, S. & Brazier, J. Using contrast sensitivity to estimate the cost-effectiveness of verteporfin in patients with predominantly classic age-related macular degeneration. Eye 21, 1455–1463 (2007). https://doi.org/10.1038/sj.eye.6702636
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.eye.6702636
Keywords
This article is cited by
-
Cost-Effectiveness Analysis of Ranibizumab Biosimilar for Neovascular Age-Related Macular Degeneration in Japan
Ophthalmology and Therapy (2023)
-
Health State Utility Values for Age-Related Macular Degeneration: Review and Advice
Applied Health Economics and Health Policy (2017)
-
Cost-Effectiveness Models in Age-Related Macular Degeneration: Issues and Challenges
PharmacoEconomics (2016)
-
Modelling Cost Effectiveness in Neovascular Age-Related Macular Degeneration: The Impact of Using Contrast Sensitivity vs. Visual Acuity
Applied Health Economics and Health Policy (2014)
-
Utility values in Japanese patients with exudative age-related macular degeneration
Japanese Journal of Ophthalmology (2011)