Abstract
Objective: To investigate the impact of irregular meal frequency on circulating lipids, insulin, glucose and uric acid concentrations which are known cardiovascular risk factors.
Design: A randomised crossover dietary intervention study.
Setting: Nottingham, UK—Healthy free-living women.
Subjects: A total of nine lean healthy women aged 18–42 y recruited via advertisement.
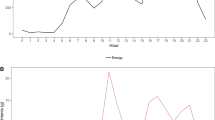
Intervention: A randomised crossover trial with two phases of 14 days each. In Phase 1, subjects consumed their normal diet on either 6 occasions per day (regular) or by following a variable meal frequency (3–9 meals/day, irregular). In Phase 2, subjects followed the alternative meal pattern to that followed in Phase 1, after a 2-week (wash-out) period. Subjects were asked to come to the laboratory after an overnight fast at the start and end of each phase. Blood samples were taken for measurement of circulating glucose, lipids, insulin and uric acid concentrations before and for 3 h after consumption of a high-carbohydrate test meal.
Results: Fasting glucose and insulin values were not affected by meal frequency, but peak insulin and AUC of insulin responses to the test meal were higher after the irregular compared to the regular eating patterns (P<0.01). The irregular meal frequency was associated with higher fasting total (P<0.01) and LDL (P<0.05) cholesterol.
Conclusion: The irregular meal frequency appears to produce a degree of insulin resistance and higher fasting lipid profiles, which may indicate a deleterious effect on these cardiovascular risk factors.
Sponsorship: The Ministry of Health and Medical Education, IR Iran.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$259.00 per year
only $21.58 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Arnold L, Ball M, Duncan A & Mann J (1993): Effect of isoenergetic intake of three or nine meals on plasma lipoproteins and glucose metabolism. Am. J. Clin. Nutr. 57, 446–451.
Beck A (1969): Depression inventory—clinical, Experimental, and Theoretical Aspects, pp 333–335. London: Staples Press.
Burstein M, Scholnick H & Morfin R (1970): Rapid method for the isolation of lipoproteins from human serum by precipitation with polyanions. J. Lipid Res. 11, 583–595.
Despres J, Lamarche B, Mauriege P, Cantin B, Dagenais G, Moorjani S & Lupien P (1996): Hyperinsulinemia as an independent risk factor for ischemic heart disease. N. Engl. J. Med. 11, 952–957.
Edelstein S, Barrett-Connor E, Wingard D & Cohn B (1992): Increased meal frequency associated with decreased cholesterol concentrations; Rancho Bernardo, CA, 1984–1987. Am. J. Clin. Nutr. 55, 664–669.
Fabry P, Fodor J, Hejl Z, Braun T & Zvolankova K (1964): The frequency of meals: its relation to overweight, hypercholesterolaemia, and decreased glucose tolerance. Lancet II, 614–615.
Fabry P, Fodor J, Hejl Z, Geizerova H & Balcarova O (1968): Meal frequency and ischaemic heart-disease. Lancet 27, 190–191.
Fábry P, Hejda S, Cerný K, Osancová K & Pechar J (1966): Effect of meal frequency in schoolchildren. Changes in weight–height proportion and skinfold thickness. Am. J. Clin. Nutr. 18, 358–361.
Friedewald W, Levy R & Fredrickson D (1972): Estimation of the concentration of low-density lipoprotein cholesterol in plasma, without use of the preparative ultracentrifuge. Clin. Chem. 18, 499–502.
Garner D & Garfinkel P (1979): The Eating Attitudes Test: an index of the symptoms of anorexia nervosa. Psychol. Med. 9, 273–279.
Grundy S (1998): Hypertriglyceridemia, atherogenic dyslipidemia, and the metabolic syndrome. Am. J. Cardiol. 26, 18B–25B.
Grundy SM, Balady GJ, Criqui MH, Fletcher G, Greenland P, Hiratzka LF, Houston-Miller N, Kris-Etherton P, Krumholz HM, LaRosa J, Ockene IS, Pearson TA, Reed J, Washington R & Smith Jr SC (1998): Primary prevention of coronary heart disease: guidance from Framingham: a statement for healthcare professionals from the AHA task force on risk reduction. Circulation 97, 1876–1887.
Gwinup G, Bryon R, Rousch W, Kruger F & Hamwi G (1963): Effect of nibbling versus gorging on serum lipids in man. Am. J. Clin. Nutr. 13, 209–213.
Hoglund D, Samuelson G & Mark A (1998): Food habits in Swedish adolescents in relation to socioeconomic conditions. Eur. J. Clin. Nutr. 52, 784–789.
Jenkins D, Khan A, Jenkins A, Illingworth R, Pappu A, Wolever T, Vuksan V, Buckley G, Rao A, Cunnane S, Brighenti F, Hawkins M, Abdolell M, Corey P, Patten R & Josse RG (1995): Effect of nibbling versus gorging on cardiovascular risk factors: serum uric acid and blood lipids. Metabolism 44, 549–555.
Jenkins D, Wolever T, Vuksan V, Brighenti F, Cunnane S, Rao A, Jenkins A, Buckley G, Patten R, Singer W, Corey P & Josse RG (1989): Nibbling versus gorging: metabolic advantages of increased meal frequency. N. Engl. J. Med. 5, 929–934.
Kageyama N (1971): A direct colorimetric determination of uric acid in serum and urine with uricase-catalase system. Clin. Chim. Acta. 31, 421–426.
Matthews D, Hosker J, Rudenski A, Naylor B, Treacher D & Turner R (1985): Homeostasis model assessment: insulin resistance and beta-cell function from fasting plasma glucose and insulin concentrations in man. Diabetologia 28, 412–419.
McGuire E, Helderman J, Tobin J, Andres R & Berman M (1976): Effects of arterial versus venous sampling on analysis of glucose kinetics in man. J. Appl. Physiol. 41, 565–573.
Murata M (2000): Secular trends in growth and changes in eating patterns of Japanese children. Am. J. Clin. Nutr. 72, 1379S–1383S.
Samuelson G (2000): Dietary habits and nutritional status in adolescents over Europe. An overview of current studies in the Nordic countries. Eur. J. Clin. Nutr. 54, S21–S28.
Solberg L & Strong J (1983): Risk factors and atherosclerotic lesions. A review of autopsy studies. Arteriosclerosis 3, 187–198.
Trivedi R, Rebar L, Berta E & Stong L (1978): New enzymatic method for serum uric acid at 500 nm. Clin. Chem. 24, 1908–1911.
Waring W, Webb D & Maxwell S (2000): Uric acid as a risk factor for cardiovascular disease. Q. J. Med. 93, 707–713.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Farshchi, H., Taylor, M. & Macdonald, I. Regular meal frequency creates more appropriate insulin sensitivity and lipid profiles compared with irregular meal frequency in healthy lean women. Eur J Clin Nutr 58, 1071–1077 (2004). https://doi.org/10.1038/sj.ejcn.1601935
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.ejcn.1601935
Keywords
This article is cited by
-
The effects of meal patterns on liver steatosis, fibrosis, and biochemical factors in patients with nonalcoholic fatty liver disease: a randomized controlled clinical trial
Journal of Diabetes & Metabolic Disorders (2024)
-
Association between breakfast frequency and metabolic syndrome among young adults in South Korea
Scientific Reports (2023)
-
Nutrizione e sindrome dell’ovaio policistico
L'Endocrinologo (2019)
-
Die familiäre Essumgebung im ersten Lebensjahr
Prävention und Gesundheitsförderung (2018)
-
Effect of meal frequency on glucose and insulin levels in women with polycystic ovary syndrome: a randomised trial
European Journal of Clinical Nutrition (2016)