Key Points
-
Describes how the likely final restorations and maintenance of appearance and function should be given early consideration in the management of AI.
-
Outlines the importance of conservative restorations to AI patients.
-
Highlights the need to emphasise the importance of a long term preventive maintenance programme to the patient early in the treatment process.
Abstract
This paper considers the role of the restorative dentist in the interdisciplinary management of patients with amelogenesis imperfecta. General restorative considerations as well as the techniques available are reviewed. Two clinical cases are described to illustrate this.
Similar content being viewed by others
Introduction
The restorative dentist further makes up the multidisciplinary team in the management of patients with amelogenesis imperfecta (AI). AI was first explained in 1890 but it was not until 1938 when Finn classified it as a separate entity to dentinogenesis imperfecta.1 The treatment in the adult patient is varied and dependent upon many factors including the type and severity of the disease, desires of the patient and intra-oral presentation at the time treatment is planned.2 There are many common presenting features which may pose a challenge to dental surgeons when managing a patient with AI. The treatment plan needs to be reviewed and revised as the treatment and the age of the patient progresses. Dental features seen in AI patients that can present such a challenge are:
-
Compromised periodontal health due to the rough surfaces retaining plaque
-
Asymmetric gingival contour
-
Hypersensitive teeth
-
Higher risk of cavities
-
Discoloured and pitted surfaces
-
Diminutive teeth with short clinical crown height
-
Malformed teeth
-
Congenitally missing teeth
-
Pulp calcifications
-
Taurodontism
-
Root malformations
-
Anterior and posterior open bite
-
Multiple posterior spacing
-
Loss of occlusal vertical dimension.3
Aims of treatment
The aim of treatment is to improve the malocclusion (for example, an anterior open bite), restore masticatory function, reduce tooth sensitivity and improve the appearance and therefore psychological wellbeing of the patient. The treatment of the patient depends upon the severity of the problem.
Historically, treatment in a severely compromised patient is comprised of a complete dental clearance and the provision of a prosthesis.4 The modern management of a patient with AI requires the full armamentarium at the disposal of a restorative dentist in the application of this and to combat difficulties that may be encountered.
Although the definitive restorative treatment is carried out once the patient is into adulthood, early liaising with colleagues from the other specialities of paediatric, surgical and orthodontic disciplines is imperative, as well as keeping the general dental practitioner informed. This has been highlighted and discussed in the previous papers of the series. The importance of attaining the end result should be kept in mind during all aspects of treatment and discussed at an early stage. Simple restorations can help to maintain space before orthodontic treatment. Consequently treatment required in adulthood to restore the teeth would ideally involve the removal of the interim/transitional restorative material thereby being more conservative to the natural tooth structure. As complex and comparatively extensive treatment for this cohort of patients is usually achieved in early adulthood, conservative preparations and restorations of little biological cost, as with all dental treatment, are of great importance as this will minimise the loss of tooth structure. It should be remembered that further replacements of the restorations throughout the life of the individual will undoubtedly be required.
Treatment
The treatment for such patients should include, as with any other, a preventive phase, the planning of the restorative phase, execution of the restorative phase, and finally the maintenance phase.
Preventive phase
The enamel surfaces of AI patients are usually rough and pitted and therefore a source for plaque accumulation. The preventive therapy should aim at teaching both parents and patients the importance of and the various techniques required for self-performed plaque control at home. This information can be supplemented using leaflets, DVDs or other visual/written aids that help reinforce oral hygiene measures. The choice of toothpaste in an adult patient should include a high fluoride concentration to increase the strength of enamel. The importance of plaque control for prevention of both caries and periodontal disease should be reinforced regularly. The use of warm water to rinse the mouth can be advised in areas of sensitivity.
Professional assistance at regular intervals is also imperative (by their dentists, hygienists or dental therapists) and ranges from simple oral hygiene instructions such as tooth brushing/flossing techniques, scaling and polishing, fluoride supplements and detection of primary/secondary caries. Again, the use of warm water during scaling may be advocated to prevent sensitivity. The recall interval for such patients should be initially every 3 months and following a period of dental health stability, changed to every 6-12 months.
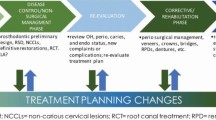
Planning the restorative phase
This is the most difficult phase of treatment and is planned on an individual case-by-case basis. Ideally a provisional plan would have been discussed with orthodontic and/or paediatric colleagues at earlier stages but should be re-evaluated at the start of the restorative treatment and preferably before debonding any fixed appliances.
The planning stage includes a detailed dental and occlusal examination. The need for a reorganised or conformative approach to restoring the occlusion should also be considered. The reader is advised to read the BDJ series on occlusion by Davis and Gray et al. for further information.5,6,7,8,9,10,11,12,13 Study models mounted on an articulator transferred with a facebow transfer at the proposed occlusal vertical dimension will aid planning along with appropriate clinical photographs and radiographs. If extracoronal restorations are required then their retention and resistance forms should also be assessed and this could be improved by either allowing for an increased occlusal vertical dimension or carrying out crown-lengthening surgery. These decisions will be based upon the patient's facial height, extent of any anterior open bite present, the freeway space, gingival contour and smile-line. In some cases where the occlusal vertical dimension is increased, the posterior teeth are planned to over-erupt without the need for placing any restorations (as in the report of case one).
Execution of the restorative phase
The execution of the restorative phase begins by discussion of a diagnostic wax up of the proposed restorations with the patient. This can be supplemented using an intra-oral mock up for the patient to visualise what their end product would roughly look like.14 The range of treatment options available in the armamentarium of the restorative dentist are briefly described below:
Crown lengthening surgery
Once the patient exhibits good motivation for oral hygiene and the periodontal health is stable, then consideration can be given for crown lengthening surgery. This technique can be used to correct the gingival architecture, improve the retention form for any future indirect restorations, improve the smile by reducing the amount of gingiva on show, or a combination of the above.
Temporisation of the occlusal scheme
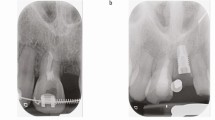
Due to the rough pitted tooth surface that often presents, even if the patient shows the motivation for good oral hygiene there may still be large supra– and sub-gingival deposits of calculus present. The provision of interim restorations can aid with this by providing a smoother surface for oral hygiene maintenance. By observing the diagnostic wax up the dentition can be built with provisional restorations either directly (chair-side) or indirectly (laboratory-based) depending upon the amount of restorative material required and clinical decision of the dentist (Figs 1a and b).
The patient can then be allowed to trial their new smile and occlusion for a suitable period of time and any changes to the restorations can be made to establish acceptable guidance. Mounted study models of this established occlusion can then be used for the construction of a guidance index. Equally the models can be mounted on a verticulator.
Anterior and premolar restorations
By using the interim restorations as a guide, each individual tooth can be restored using the most conservative option that will achieve the planned end result. Definitive direct composite restorations can be considered where the enamel is not too compromised or the discolouration not too severe. If definitive crowns on the anterior teeth are required then porcelain dentine bonded crowns can provide an excellent aesthetic result and require minimal preparation. Care must be taken not to have sharp line angles. All ceramic restorations bonded to tooth structure with adhesive resin cements enhance the fracture resistance of the material.15,16 This may also help to prevent postoperative sensitivity.17 Porcelain fused to metal crowns and even more aggressive preparations should be avoided in the first instance but may need to be considered where previous preparations have already been carried out.
When restoring mandibular anterior teeth, composite build-ups or veneers provide a more conservative option. If retention is a concern then dentine bonded crowns may be preferred. Bleaching of teeth for patients with severe discolouration may not provide a great deal of benefit and may further exacerbate any hypersensitivity already present.
Molar restorations
If the enamel is not too compromised then molar teeth may be allowed to over erupt back into the occlusion. If protection of the tooth structure is required then either type IV heat treated gold onlays bonded with a resin-based material or full coverage gold veneer crowns can be provided. Direct restoration with composite on the occlusion of molar teeth may not be ideal due to the poorer wear characteristics, although this may be an invaluable option in the interim phase.
Maintenance phase
The maintenance in the long term should be aimed at oral hygiene reinforcement, periodontal stability, and occlusal stability. This can be maintained by the general dental practitioner at regular appointments. The provision of a suitable protective occlusal guard to be worn at night time may be advocated due to the number of restorations placed. Any future restorative work would then be aimed at maintaining the occlusion using a conformative approach.
Case reports
The following two case reports describe the multidisciplinary approach with orthodontic, surgical and paediatric colleagues with the additional speciality of restorative dentistry in restoring patients with AI.
Case one
This case demonstrates crown lengthening of the maxillary dentition, an increase in the occlusal vertical dimension and allowing over-eruption of the posterior teeth.
A 20-year-old female diagnosed with AI was referred by her general dental practitioner regarding her concerns about her 'crooked gums and teeth' and wish to improve the look of her smile (Fig. 2). Her medical history was non-contributory, and there was no history of smoking. Extra oral examination was unremarkable and the patient had a high smile line. Intra-oraly, the clinical crown height was reduced with a thick gingival biotype and inharmonious gingival margin. Anterior guidance was provided by the posterior teeth and lateral excursions were provided by group function. Intra-oral periapical radiographs revealed no significant findings and a favourable crown-root ratio.
Following detailed examination, study models were mounted using a facebow transfer with a retruded pre-contact occlusal record on a semi adjustable articulator. A diagnostic wax up at an increased occlusal vertical dimension of 3 mm was carried out, apically repositioning the gingival margins of the maxillary anterior and premolar teeth.14 The principles of golden ratio18,19 and average values for inciso-gingival and mesiodistal crown dimensions were used.20,21 It was elected to retain the upper right lateral incisor and protect any proposed restoration from loading in excursive movements (Fig. 2).
After a three month period of gingival and osseous healing the anterior and premolar teeth were prepared for the interim restorations. No occlusal reduction was carried out for the mandibular teeth as any space required for restorations was to be gained from increasing the occlusal vertical dimension. This was assessed on the interim restorations placed on the premolar and canine teeth following the diagnostic wax up. Definitive direct amalgam restorations were placed on the posterior teeth. Following a period of adaptation and over-eruption of the molar teeth, in this case six months, the definitive premolar canine and maxillary incisor crowns and mandibular incisor veneer restorations were placed (Fig. 3).
An upper hard occlusal guard (of Michigan design) was provided for nightwear to protect teeth from risk of para-function and occlusal loading and the patient was very satisfied with the final outcome (Fig. 4).
Case two
This case describes full mouth discolouration and relapse of orthodontic and orthagnathic surgery to correct a bilateral crossbite and overjet.
A 29-year-old male was self-conscious of his discoloured teeth and wanted to improve the appearance of them (Fig. 5). His medical history was non-contributory and there was no history of smoking. On extra oral examination nothing abnormal was detected and when smiling severe tooth and composite restoration discolouration was noted. Intra-oral periapical radiographs revealed no significant findings. The patient had previously undergone fixed orthodontic treatment to align the arches and orthognathic surgery to correct the skeletal discrepancies. Unfortunately the treatment had relapsed due to lack of compliance in retainer wear, eventually regressing back to the pre-operative bilateral buccal cross-bite and severe Class II division 1 incisor relationship.
Oral hygiene techniques were reinforced and hygiene phase therapy provided to restore gingival health. Study models mounted on a semiadjustable articulator at the existing vertical dimension using an intercuspal position occlusal record were used to carry out a diagnostic wax up, providing a canine protected occlusion and attempting to correct the posterior cross bite. Provisional acrylic crowns were placed on all teeth except for the mandibular incisor teeth, which were planned for porcelain labial veneers. This was for both conservation of tooth structure and establishing sound occlusal contacts. The provisional restorations were worn for a period of six months to allow for any adjustments and to assess tolerance by the patient to the proposed change in tooth morphology, occlusal contacts, guidance and aesthetics.
Definitive full veneer gold crowns were placed on all molars and on the mandibular second premolar teeth; porcelain dentine bonded crowns on the remainder of the premolar teeth, all canine teeth and maxillary incisor teeth; and porcelain veneers on the mandibular incisor teeth. Figure 6 illustrates the right lateral views of the intermin acrylic crown restorations, while Figure 7 shows the intraoral appearance immediately following placement of definitive restorations. An occlusal guard of Michigan design was provided for nightwear and the patient was very satisfied with the final outcome.
Summary
The treatment of patients with amelogenesis imperfecta requires a multidisciplinary approach from a very early age with the treatment plan constantly reviewed and updated until early adulthood is reached. The protracted nature of treatment while addressing the patient's aesthetic and functional concerns can be a challenge and patient motivation can vary during this time. Serial photographs can help with encouragement and motivation of the patient before achievement of the final result. The role of primary care then becomes critical in oral maintenance and replacement of restorations as required.
References
Finn S B. Hereditary opalescent dentition I: an analysis of the literature on hereditary anomalies of tooth colour. J Am Dent Assoc 1938; 25: 1240–1249.
Sari T, Usumez A. Restoring function and esthetics in a patient with amelogenesis imperfecta: a clinical report. J Prosthet Dent 2003; 90: 522–525.
Seow W K. Clinical diagnosis and management strategies of amelogenesis imperfecta variants. Pediatr Dent 1993; 15: 384–393.
Olsen J J. Hereditary aplasia of the enamel. J Am Dent Assoc 1938; 25: 830–831.
Davies S J, Gray R M. What is occlusion? Br Dent J 2001; 191: 235–238, 241–245.
Davies S J, Gray R J, Qualtrough A J. Management of tooth surface loss. Br Dent J 2002; 192: 11–16, 19–23.
Davies S J, Gray R J, Young M P. Good occlusal practice in the provision of implant borne prostheses. Br Dent J 2002; 192: 79–88.
Davies S J, Gray R J, Mackie I C. Good occlusal practice in children's dentistry. Br Dent J 2001; 191: 655–659.
Davies S J, Gray R J, Linden G J, Hames J A. Occlusal considerations in periodontics. Br Dent J 2001; 191: 597–604.
Davies S J, Gray R M, Sandler P J, O'Briend K D. Orthodontics and occlusion. Br Dent J 2001; 191: 539–542, 545–549.
Davies S J, Gray R M, McCord J F. Good occlusal practice in removable prosthodontics. Br Dent J 2001; 191: 491–494, 497–502.
Davies S J, Gray R M, Smith P W. Good occlusal practice in simple restorative dentistry. Br Dent J 2001; 191: 365–368, 371–374, 377–381.
Davies S J, Gray R M. The examination and recording of the occlusion: why and how. Br Dent J 2001; 191: 291–296, 299–302.
Malik K, Tabiat-Pour S. The use of a diagnostic wax set-up in aesthetic cases involving crown lengthening – a case report. Dent Update 2010; 37: 303–304, 306–307.
Blatz M B. Long-term clinical success of all-ceramic posterior restorations. Quintessence Int 2002; 33: 415–426.
Malament K A, Socransky S S. Survival of Dicor glass-ceramic dental restorations over 16 years. Part III: effect of luting agent and tooth or tooth-substitute core structure. J Prosthet Dent 2001; 86: 511–519.
Sensat M L, Brackett W W, Meinberg T A, Beatty M W. Clinical evaluation of two adhesive composite cements for the suppression of dentinal cold sensitivity. J Prosthet Dent 2002; 88: 50–53.
Lombardi R E. The principles of visual perception and their clinical application to denture esthetics. J Prosthet Dent 1973; 29: 358–382.
Levin E I. Dental esthetics and the golden proportion. J Prosthet Dent 1978; 40: 244–252.
Gillen R J, Schwartz R S, Hilton T J, Evans D B. An analysis of selected normative tooth proportions. Int J Prosthodont 1994; 7: 410–417.
Ahmad I. Anterior dental aesthetics: dental perspective. Br Dent J 2005; 199: 135–141.
Acknowledgements
The authors would like to acknowledge Messrs Kevin Fairbrother and Anthony Summerwill, the chair side assistance of Alison Aberdeen and Kirsty Nightingale and the laboratory support of Robert Harrisson, Vijay Soni and Louise Carey.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Malik, K., Gadhia, K., Arkutu, N. et al. The interdisciplinary management of patients with amelogenesis imperfecta – restorative dentistry. Br Dent J 212, 537–542 (2012). https://doi.org/10.1038/sj.bdj.2012.469
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2012.469
This article is cited by
-
Oral health-related quality of life before and after crown therapy in young patients with amelogenesis imperfecta
Health and Quality of Life Outcomes (2015)
-
Correction of malocclusion and oral rehabilitation in a case of amelogenesis imperfecta by insertion of dental implants followed by Le Fort I distraction osteogenesis of the edentulous atrophic maxilla
BMC Oral Health (2014)