Key Points
-
The Wand technique seems to be of benefit during inferior alveolar injection of patients with low dental anxiety.
-
Most of the patients preferred inferior alveolar injection with the Wand than with conventional syringe for future dental injections.
-
The Wand technique not only lowers the pain of injection, but also eliminates the visual stimulus of dental syringes for patients with low dental anxiety.
Abstract
Objective This study compared a computerised device (the Wand) with a conventional syringe in terms of the pain of needle insertion and injection during inferior alveolar nerve (IAN) block injection.
Methods and materials The subjects were 40 patients between the ages of 18 and 30 years requiring local anaesthesia for dental restoration in the mandible. Before anaesthetic administration, the patients' anxiety levels were determined. Contralateral IAN injections were administrated at two separate appointments with random use of either the Wand or a conventional syringe. Following the injection, the patients used both the pain rating score (PRS) and a visual analogue scale (VAS) to assess the intensity of pain.
Results When pain was measured after the injection, the Wand was found to be less painful than the syringe for the pain of both needle insertion and injection (p <0.05).
Conclusion The Wand technique resulted in significantly lower pain scores during the IAN block injections. Most of the patients preferred the IAN injection with the Wand for future dental injections.
Similar content being viewed by others
Introduction
Local anaesthesia is used most widely for delivering dental care1 and although anaesthesia is necessary for a painless dental procedure, patients sometimes find the needle puncturing the mucosa or the delivery of local anaesthetic solutions to be painful or uncomfortable.2 Fear and anxiety associated with local anaesthesia injection can be a major impediment to dental care because it frequently causes patients to delay or even avoid treatment.3 To minimise the pain on injection, the use of topical anaesthesia, low-pressure injection,4 narrow sharp needles,5 a slow injection rate6 and solutions that are warmed7 and buffered8 have been suggested. Nevertheless, a totally painless injection is impossible to achieve under all circumstances.
A computerised injection device (the Wand) was developed as an alternative to the conventional syringe to alleviate pain and anxiety during intraoral injections. According to the manufacturer, the device is a computer-controlled system that maintains constant pressure and volume ratios, delivering local anaesthetic solutions at a constant rate regardless of tissue resistance. It is claimed that when advanced slowly, the drops of solution anaesthetise the tissue ahead of the needle, thereby resulting in a virtually painless needle insertion. In addition, the rate and aspiration cycle are both activated using a foot control.9
It is claimed that new computerised injection devices reduce pain and discomfort during intraoral injections. An earlier study found that dentists were very satisfied with the effectiveness and performance of a prototype computer-controlled dental local anaesthetic system and patients were satisfied with both the level of comfort with anaesthetic delivery and the effectiveness of the anaesthesia itself.10 Some studies showed a reduction in the pain of injection when using the Wand compared to conventional injection.11,12 However, another study showed no advantages of using a computerised injection unit and that conventional methods of anaesthetic delivery, when well performed, were superior.13
The differences between these results may be related to several factors, such as the patients' anxiety levels, injection technique, and tactile skill in syringe injections.11 Low-pressure, slow-delivery apparatus, such as the Wand, should be evaluated as a possible means of alleviating the perceived pain on injection.
Therefore, this study compared a computerised device (the Wand) with a conventional syringe in terms of the pain of needle insertion and injection during inferior alveolar nerve (IAN) block injection.
Methods and materials
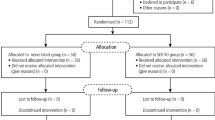
Forty adult patients scheduled for routine dental restorative treatment participated in this study. The participants were in good general health and were not taking any medication (eg alcohol or any analgesic medication) that would alter pain perception. Pregnant females were not eligible for the study. Nineteen women and 21 men, ranging in age from 18 to 30 years, were enrolled. All patients were selected based on their need for restorative dentistry in the right and left mandible requiring local anaesthesia. The Karadeniz Technical University (Trabzon, Turkey) Human Subjects Review committee approved the study, and written informed consent was obtained from each subject. After completing the medical history and consent form, the dental anxiety of the participants was measured using Corah's Dental Anxiety Scale (DAS).14 Pre-operatively, all of the subjects were asked to complete the questionnaire to rate their anxiety levels. A score of 4 corresponded to the least anxiety and 20 indicated the most. The basic DAS scale of each group was used with the aim of determining the patients with minimal anxiety. DAS scores of all the patients participating in the study were 12 or lower. The patients whose DAS scores were over 12 excluded from the study.
The anaesthetic agent was 1.7 ml of 4% articaine (68 mg) with 1:100,000 epinephrine (17 μg) (Ultracaine D-S forte; Aventis Pharma San. ve Tic, Istanbul, Turkey). Before any injections were given, 10% lidocaine (Xylocaine; AstraZeneca, Lund, Sweden) topical anaesthetic spray on a cotton applicator was applied to the injection area under both techniques. The 40 subjects randomly received contralateral inferior alveolar nerve (IAN) block injections at two separate appointments spaced at most five days apart. The subjects received IAN block injections of articaine with epinephrine using the Wand Plus® local anaesthesia system with a 27 gauge/0.4 mm diameter needle (The Wand, Tudor Health Care Ltd., Nottingham, UK) at one appointment and the same amount of articaine with epinephrine, using a conventional syringe with a 27 gauge/0.4 mm diameter needle (Ayset Co., Adana, Turkey), at the other appointment. Forty sets of IAN block injections were administered on each side and each subject served as his or her own control. The right or left side was chosen randomly for the first injection, and the opposite side was used for the second injection. All dental injections were administered by the same operator. The dental anxiety of the participants was again measured at the second appointment.
The Wand injections were given according to the manufacturer's instructions for the injection technique, time of each injection and needle gauge. The slower mode was used during anaesthesia deposition, which took 100 s for the mandibular injections. The conventional syringe injection was given according to the standard operator technique used under normal clinical practice in terms of injection technique and time of injection. The traditional injections took approximately half the time required for the Wand injections.
Immediately following the injection, the subjects used both the pain rating score (PRS) and visual analogue scale (VAS) to assess the intensity of pain during both needle insertion and injection. The PRS has four levels of pain: no, slight, moderate, and severe pain. The VAS is a 100 mm-long horizontal line, the far-left end indicating no pain and the far-right indicating intolerable pain. The subjects placed a mark on the scale where it best described their pain level. In addition, the subjects were asked to indicate which injection technique they preferred after the second appointment.
Statistical analysis was performed using commercial software (SPSS 14.0; SPSS, Chicago, IL). Between-anaesthesia technique differences in pain ratings for needle insertion and injection were analysed using Wilcoxon's signed-ranks test. The VAS and DAS data were analysed using the paired t-test.
Results
The mean DAS was 8.9 ± 4.1 for the first appointment and 7.3 ± 3.4 for the second appointment, and these differed significantly (p = 0.002). The mean injection discomfort ratings with the Wand were lower than with the conventional syringe (p <0.05). For needle insertion with the Wand system, 19 of 40 subjects reported no pain, 21 reported mild pain and none reported moderate or severe pain. For needle insertion with the conventional technique, 2 of 40 subjects reported no pain, 29 reported mild pain, 6 reported moderate pain and none reported severe pain.
For the Wand system during injection, 24 of 40 subjects reported no pain, 13 reported mild pain, and 3 reported moderate pain. For the conventional technique during injection, 10 of 40 subjects reported no pain, 26 reported mild pain, and 4 reported moderate pain. No one reported severe pain during injection.
Statistically significant differences were found between the Wand system and the conventional technique (p <0.05). Table 1 shows the results of the PRS during needle insertion and injection.
The individual VAS scores for the injections are shown in Figures 1 and 2. The mean VAS for needle insertion using the Wand and conventional system was 8 ± 8.9 and 18 ± 16.3 mm, respectively. The mean VAS during injection using the Wand and conventional system was 8.5 ± 14.5 and 15.9 ± 18.9 mm, respectively. A significant difference was observed between the Wand and conventional system according to the VAS (p <0.05).
Regarding technique preference, 70% (28/40) preferred the Wand injection system, 22.5% (9/40) preferred the conventional syringe and 7.5% (3/40) had no preference. Significant differences in preference were detected between the two techniques (p <0.005).
Discussion
The measurement of pain during injection can be quite difficult. Pain perception is highly subjective and influenced by many factors, such as anxiety, fear and past experiences.15 The use of questionnaire measures of anxiety related to dental pain is well established and one of the most widely used for measuring dental anxiety is Corah's DAS. It has satisfactory reliability and validity and is easy to administer.16 Therefore, in this study, Corah's DAS14 was used for the objective estimation of dental anxiety, as in previous studies.11,17,18
Specific procedures or steps in dental treatment tend to arouse anxiety. When considering dental anxiety in relation to the various types of treatment, anxiety was found to be the highest before root canal therapy, followed by extraction and filling.19 This study examined patients about to undergo routine tooth filling, since subjects with minimal anxiety might be included in clinical studies to improve the reliability of the measurements of pain.17 The mean DAS scores of the participants were 8.9 ± 4.1 for the first appointment and 7.3 ± 3.4 for the second. Corah's DAS considered that the most anxious patients scored 13 or higher on the scale.20 If more anxious patients had participated in this study, the pain scores may have changed.
Kaufman et al.5 reported that the area in the oral cavity being injected was directly related to the pain and perceived discomfort. Palatal injection and inferior alveolar nerve (IAN) block injection are more painful than local infiltration, mental nerve block, or periodontal ligament injection.5,21 However, the IAN block is the most frequently used injection technique for achieving local anaesthesia during mandibular restoration and surgical procedures. Therefore, we used the IAN block injection to compare anaesthesia techniques in this study.
Topical anaesthetic is the most widely used method to reduce pain associated with dental injections. Most patients are accustomed to having a topical agent applied before injections and they can taste and feel the effect on their soft tissue.22 However, the clinical effectiveness of topical anaesthesia is debated.17,23,24 Topical anaesthetic can increase the subjective anaesthetic effects23 and can serve to reduce the anticipatory anxiety associated with dental injections.25 The use of topical anaesthesia is optional, according to the Wand manufacturer's instructions. We used topical anaesthetic for both techniques, since the psychological effect of using topical anaesthetic may be important for minimising patient anxiety.
In this study, when pain was measured after the injections, the Wand was found to be less painful than injections with a syringe. According to previous reports, the Wand system generally seemed to result in less painful injections compared to a conventional syringe.10,11,12 The Wand provides comfortable anaesthesia for patients and can be a good alternative to conventional manual syringe injection.26 However, discrepancies exist concerning the effectiveness of the Wand technique. Sumer et al.11 reported that although the anxiety levels of patients were higher with the Wand technique than with conventional syringe injection, the Wand resulted in lower pain scores. Conversely, Goodell et al.13 reported higher pain ratings with the Wand system, while Nusstein et al.17 reported lower pain ratings during anaesthetic solution deposition using the Wand system, but similar pain ratings for needle insertion. The different results across similar studies may be attributable to the patients, operators, or injection area.
One way to potentially decrease the pain of needle placement would be to advance the needle more slowly.4 The Wand injection system creates a continuous positive solution pressure to deliver an anaesthetic solution that precedes the needle path. The Wand manual states, This anaesthetic pathway is believed to assist in virtually eliminating discomfort as the needle penetrates through the tissue.'9,21 In our study, the slow rate was used for the Wand local anaesthetic system. Therefore, Wand injections might be less painful than syringe injections for IAN blocks. Unfortunately, even with these techniques and a slow deposition rate, needle insertion was not painless.
Previously, studies reported that the pain can result from the mechanical trauma of needle introduction into the site of injection, or from the sudden distension of the tissues resulting from a rapid discharge of the contents of the syringe.12 Since the Wand handpiece is held in a pen grasp, it can be rotated continuously during needle insertion. By rotating the needle 180° right-left between the thumb and forefinger, the bi-directional rotation of the needle and the controlled slow anaesthesia deposition rate would reduce the sensation of needle insertion. Therefore, the differences in pain perception during injection administered with the Wand and the conventional syringe may be both the result of different techniques and as a result of the slower injection of the Wand. Furthermore, the results could be influenced by the operator's experience differences, their skill in giving injections, the learning curve associated with the use of the Wand, and types of nerve blocks. Therefore, the clinical significance of the results of the study should be interpreted with caution.
Regarding technique preference, 70% (28/40) preferred the computer-assisted injection, 22.5% (9/40) preferred the conventional syringe and 7.5% (3/40) had no preference. Significant differences in preference were observed between the two techniques. Most of the patients preferred the IAN injection with the Wand apparatus. Similarly, Nicholson et al.27 studied maxillary injections and inferior alveolar nerve blocks in adult patients and found that 50% of the patients preferred the computer-assisted injection, 20% preferred the conventional syringe, and 30% had no preference. The Wand technique not only lowers the pain of injection, but also eliminates the visual stimulus of dental syringes. This may be another reason for the preference for the Wand technique.
At the present time, the dental community has been slow to adopt this technology, which could be attributable to several reasons. The expense of buying the new syringes and disposable attachments, the length of injection time, the need to change work routines and the additional space needed for the device remain limiting factors.28
Conclusion
In conclusion, the mean pain rating was slight or no pain for both injection techniques. Overall, under the conditions used in this study, the Wand seemed to cause less pain during the IAN block injections. The clinical significance of the results should be interpreted with caution since we studied a young adult population and our results might not apply to children or the elderly. It would be beneficial to compare the Wand across multiple operators and a broader population in the future.
References
Primosch R E, Brooks R . Influence of anesthetic flow rate delivered by the Wand Local Anesthetic System on pain response to palatal injections. Am J Dent 2002; 15: 15–20.
Wahl M J, Schmitt M M, Overton D A, Gordon M K . Injection pain of bupivacaine with epinephrine vs. prilocaine plain. J Am Dent Assoc 2002; 133: 1652–1656.
Milgrom P, Coldwell S E, Getz T, Weinstein P, Ramsay D S . Four dimensions of fear of dental injections. J Am Dent Assoc 1997; 128: 756–766.
Kudo M . Initial injection pressure for dental local anesthesia: effects on pain and anxiety. Anesth Prog 2005; 52: 95–101.
Kaufman E, Epstein J B, Naveh E, Gorsky M, Gross A, Cohen G . A survey of pain, pressure, and discomfort induced by commonly used oral local anesthesia injections. Anesth Prog 2005; 52: 122–127.
Rood J P . The pressures created by inferior alveolar injections. Br Dent J 1978; 144: 280–282.
Rogers K B, Fielding A F, Markiewicz S W . The effect of warming local anesthetic solutions prior to injection. Gen Dent 1989; 37: 496–499.
Primosch R E, Robinson L . Pain elicited during intraoral infiltration with buffered lidocaine. Am J Dent 1996; 9: 5–10.
Milestone Scientific. The Wand computer controlled anesthesia delivery system user manual. pp 1–27. Livingston, NJ: Milestone Scientific, 1998.
Grace E G, Barnes D M, Macek M D, Tatum N . Patient and dentist satisfaction with a computerized local anesthetic injection system. Compend Contin Educ Dent 2000; 21: 746–752.
Sumer M, Misir F, Koyuturk A E . Comparison of the Wand with a conventional technique. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2006; 101: e106–e109.
Saloum F S, Baumgartner J C, Marshall G, Tinkle J . A clinical comparison of pain perception to the Wand and a traditional syringe. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000; 89: 691–695.
Goodell G G, Gallagher F J, Nicoll B K . Comparison of a controlled injection pressure system with a conventional technique. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2000; 90: 88–94.
Corah N L . Development of a dental anxiety scale. J Dent Res 1969; 48: 596.
McGrath P A . Pain control in dentistry: psychologic factors that modify the perception of pain. Compend Contin Educ Dent 1985; 8: 574–582.
Newton J T, Buck D J . Anxiety and pain measures in dentistry: a guide to their quality and application. J Am Dent Assoc 2000; 131: 1449–1457.
Nusstein J, Lee S, Reader A, Beck M, Weaver J . Injection pain and postinjection pain of the anterior middle superior alveolar injection administrated with the Wand or conventional syringe. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004; 98: 124–131.
Nusstein J, Burns Y, Reader A, Beck M, Weaver J . Injection pain and postinjection pain of the palatal-anterior superior alveolar injection, administered with the Wand Plus system, comparing 2% lidocaine with 1:100,000 epinephrine to 3% mepivacaine. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 2004; 97: 164–172.
Udoye C I, Oginni A O, Oginni F O . Dental anxiety among patients undergoing various dental treatments in a Nigerian teaching hospital. J Contemp Dent Pract 2005; 15: 91–98.
Corah N L . Dental anxiety. Assessment, reduction and increasing patient satisfaction. Dent Clin North Am 1988; 32: 779–790.
Malamed S F . Handbook of local anesthesia. 4th ed. pp 149–160. St. Louis: Mosby, 1997.
Quarnstrom F, Libed E N . Electronic anesthesia versus topical anesthesia for the control of injection pain. Quintessence Int 1994; 25: 713–716.
Gill C J, Orr D L . A double-blind crossover comparison of topical anesthetics. J Am Dent Assoc 1979; 98: 213–214.
Kincheloe J E, Mealiea W L Jr, Mattison G D, Seib K . Psychophysical measurement on pain perception after administration of a topical anesthetic. Quintessence Int 1991; 22: 311–315.
Martin M D, Ramsay D S, Whitney C, Fiset L, Weinstein P . Topical anesthesia: differentiating the pharmacological and psychological contributions to efficacy. Anesth Prog 1994; 41: 40–47.
Fukayama H, Yoshikawa F, Kohase H, Umino M, Suzuki N . Efficacy of anterior and middle superior alveolar (AMSA) anesthesia using a new injection system: the Wand. Quintessence Int 2003; 34: 537–541.
Nicholson J W, Berry T G, Summitt J B, Yuan C H, Witten T M . Pain perception and utility: a comparison of the syringe and computerized local injection techniques. Gen Dent 2001; 49: 167–173.
Ram D, Peretz B . The assessment of pain sensation during local anesthesia using a computerized local anesthesia (Wand) and a conventional syringe. J Dent Child (Chic) 2003; 70: 130–133.
Author information
Authors and Affiliations
Corresponding author
Additional information
Refereed paper
Rights and permissions
About this article
Cite this article
Yesilyurt, C., Bulut, G. & Taşdemir, T. Pain perception during inferior alveolar injection administered with the Wand or conventional syringe. Br Dent J 205, E10 (2008). https://doi.org/10.1038/sj.bdj.2008.757
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.bdj.2008.757
This article is cited by
-
Pain perception following computer-controlled versus conventional dental anesthesia: randomized controlled trial
BMC Oral Health (2022)
-
Blood pressure monitoring following individual carpules of anesthetic utilizing computer-controlled anesthetic delivery
BDJ Open (2020)
-
Single tooth anesthesia versus conventional anesthesia: a cross-over study
Clinical Oral Investigations (2018)
-
Comparing the onset of maxillary infiltration local anaesthesia and pain experience using the conventional technique vs. the Wand in children
British Dental Journal (2012)