Abstract
Study design:
Cross-sectional study 5 years after discharge from inpatient rehabilitation.
Objective:
To examine the psychometric properties of the Mental Health subscale (MHI-5) of the 36-Item Short Form Health Survey (SF-36) in persons with spinal cord injury (SCI).
Setting:
Eight Dutch rehabilitation centres with specialised SCI units.
Methods:
Possible floor and ceiling effects were assessed, and Cronbach′s α coefficient was calculated to assess internal consistency. Concurrent and divergent validity were assessed using Spearman correlations between the MHI-5 and measures of life satisfaction, neuroticism, vitality, general health, functional independence, participation, lesion characteristics and demographics.
Results:
There were no floor or ceiling effects, but the total MHI-5 score was slightly skewed (−1.15). Internal consistency was good (α=0.79). Concurrent validity was shown by significant Spearman correlations between the MHI-5 and life satisfaction (0.53), neuroticism (−0.55), vitality (0.53) and general health (0.37). Divergent validity was shown by weak and, in part, non-significant correlations between the MHI-5 and functional independence (0.09), participation (−0.28) and lesion characteristics (range −0.01–0.19).
Conclusion:
The MHI-5 showed reliability and validity as a measure of mood in persons with SCI, and is a promising measurement instrument to assess mental health problems in this population.
Similar content being viewed by others
Introduction
Spinal cord injury (SCI) has severe consequences for the quality of life of the person involved. There is convincing evidence that the prevalence of mental health disorders, such as depression, anxiety and post-traumatic stress syndrome, is elevated in persons with chronic SCI.1
A recent review assessed 13 measurement instruments, which are used to screen for mental health disorders or to measure the severity of symptoms in persons with SCI.2 This review showed that psychometric characteristics of most instruments were adequate or better than adequate.2 However, information was incomplete and no instrument showed superiority above other instruments.2 An instrument that was not included in this review is the five-item Mental Health Index (MHI-5). The MHI-5 is probably better known as the Mental Health subscale of the Medical Outcomes Study Short Form Health Survey (SF-36),3 which has often been used in SCI research.4, 5 The MHI-5 has a good specificity and sensitivity for detecting mental health disorder and depression in the general population6, 7 and in persons with various chronic conditions.8, 9 Compared with other depression and anxiety instruments, the MHI-5 is very brief, easy to administer and widely used as part of the SF-36.
In spite of these favourable characteristics, the MHI-5 has not been used as a separate measure of mental health in persons with SCI and its psychometric properties have not been examined in this population. Therefore, the aim of the present study was to examine the item-response distribution, internal consistency, concurrent and divergent validity of the MHI-5 in persons with SCI.
Methods
Participants
This study is a follow-up of the Dutch research programme ‘Restoration of mobility in the rehabilitation of persons with spinal cord injuries’.10 For this research programme, 225 persons admitted for initial inpatient rehabilitation, were selected consecutively in eight rehabilitation centres with specialised SCI units in the Netherlands between August 2000 and July 2003. Subjects were included if they fulfilled the following criteria: (1) a recently acquired SCI; (2) age between 18 and 65 years; (3) grade A, B, C, or D on the AIS (American Spinal Injury Association Impairment Scale); and (4) expected permanent wheelchair dependency. Participants were excluded if they had (1) an SCI caused by a malignant tumour, (2) a progressive disease, (3) psychiatric problems, or (4) insufficient command of the Dutch language to understand the goal of the study and test instructions.
Procedure
The assessment that provided data for the current study took place 5 years after discharge from inpatient rehabilitation and included a medical examination, physical tests, an oral interview with a trained research assistant and self-report questionnaires. Mental health, general health, vitality, life satisfaction and functional independence were measured during the oral interview. Neuroticism and participation were part of the self-report questionnaires. This follow-up assessment was approved by the Medical Ethics Committee of the University Medical Centre Utrecht. All persons gave written informed consent.
Instruments
Mental health was assessed by using the MHI-5, consisting of five items concerning nervousness, sadness, peacefulness, mood and happiness.3 Respondents rated the frequency of each item during the previous 4 weeks on a 6-point Likert-response scale (1=all of the time, 2=most of the time, 3=a good bit of the time, 4=some of the time, 5=a little of the time, 6=none of the time), for example, ‘How much of the time, during the last month, have you felt downhearted and blue?' A total score was computed by summing and transforming the five-item scores into a score between 0 (lowest mental health) and 100 (highest mental health).11 A cutoff point of 72 or lower refers to mental health problems, and of 60 or lower refers to severe mental health problems.11, 12
Vitality was measured by using the vitality scale of the SF-36, consisting of four items concerning energy and fatigue.3 A total score was computed by summing and transforming the four-item scores into a score between 0 (lowest vitality) and 100 (highest vitality).3
General health was assessed by using the general health scale of the SF-36, consisting of five items assessing the subjective evaluation of the general health status.3 A total score was computed by summing and transforming the five-item scores into a score between 0 (lowest general health) and 100 (highest general health).3
Life satisfaction was measured by using the LiSat-9 (Life Satisfaction Questionnaire-9).13 The LiSat-9 consists of one question about satisfaction with life as a whole, and eight questions about satisfaction with various life domains. Each item is scored on a 6-point scale (very unsatisfied up to very satisfied). The total score is the average of all item scores and has a range of 1 (low level of well-being) to 6 (high level of well-being). The LiSat-9 is a valid measure of life satisfaction and has often been used in SCI research.13
Neuroticism is a personality trait reflecting emotional stability and was assessed by using the EPQ-RSS-N (Eysenk Personality Questionnaire-Revised Short Scale-Neuroticism).14 This scale consists of 12 dichotomous items (for example, ‘Does your mood often go up and down?’). The EPQ-RSS was shown to be reliable and valid in patients with cancer and healthy controls.14 Participation was measured by using the SIP68-MR (Mobility Range of the Sickness Impact Profile 68).15 A high score reflects poor participation. The SIP68 proved to be reliable and valid in patients with SCI.15
Functional independence was measured by using the motor score of the FIM (Functional Independence Measure), consisting of 13 items about self care, mobility, transfers and toileting. The FIM shows good reliability and validity.16 A high FIM motor score reflects a high level of functional independence.
Lesion characteristics were assessed according to the International Standards for Neurological Classification of Spinal Cord Injury.17 Neurological levels below T1 were defined as paraplegia, neurological levels at or above T1 were defined as tetraplegia. AIS grades A and B were considered motor complete, and grades C and D were considered motor incomplete. Cause of injury was dichotomised in traumatic versus non-traumatic.
Demographic characteristics included were age, gender, educational level (low: no or only vocational education, middle: high school, high: bachelor/master), marital status (being married or living together versus living alone) and having children (yes, no).
Statistical analysis
Statistical analyses were performed using SPSS version 18.0 for Windows (IBM Corporation, Armonk, NY, USA). List-wise deletion was used for missing data such that the primary analyses included only participants with complete data on the MHI-5. List-wise deletion was chosen owing to the small (<5%) and random nature of the missing data and because of the substantial sample of the present study.
Floor and ceiling effects were considered to be present if more than 15% of the respondents achieved the lowest or highest possible MHI-5 score, respectively.18 Skewness was considered to be present if the corresponding statistic was below −1.0 or above 1.0. To examine the internal consistency of the MHI-5, Cronbach α coefficient was assessed. If Cronbach α coefficient was at least 0.7018 and item–rest correlations were larger than 0.30, internal consistency was considered acceptable. To assess the concurrent validity of the MHI-5, Spearman correlations between the MHI-5 and the Lisat-9, the Neuroticism scale of the EPQ-RSS, the Vitality scale and the General Health scale of the SF-36 were calculated. Strong correlations (r>0.50)19 were expected. To assess the divergent validity of the MHI-5, Spearman correlations between the MHI-5 and the FIM, the SIP68-MR and lesion characteristics were calculated. Weak correlations (r<0.30)19 were expected, because these variables measure different concepts. If at least 75% of these expectations were met, the construct (concurrent/divergent) validity of the MHI-5 was confirmed.18
Results
Respondent characteristics
A total of 145 persons participated in the follow-up measurement 5 years after discharge from inpatient rehabilitation. Reasons for drop-out between the first and the last measurement of the research programme were that 30 persons died, 18 refused to collaborate, 5 moved out of the country, 12 could not be contacted and 15 had other reasons to decline further participation. The mean age of the participants was 45.4 years (s.d. 13.7). Other respondent characteristics are shown in Table 1. Participants did not significantly differ from drop-outs in gender, level of education, level and completeness of SCI, mental health or life satisfaction, but non-participants had a significantly greater proportion of non-traumatic injuries and a higher age than participants.
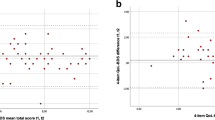
Distribution of MHI-5 scores
Table 2 shows the response distribution on all five items. The distribution of the total MHI-5 score is shown in Figure 1. Five respondents had very low scores, resulting in a slightly skewed score distribution (Skewness −1.15). However, the median (76; IQR (interquartile range) 68–88) was close to the mean (77.2; s.d. 15.1), which indicates that the distribution of the MHI-5 score was nearly symmetric. No participants scored 0 and 4.8% of the participants scored 100, indicating no floor or ceiling effects.
Internal consistency
Cronbach's α of the MHI-5 was higher than 0.70 (0.79) and all item–rest correlation were above 0.30 (range 0.37–0.68).
Concurrent and divergent validity
Table 3 shows that 75% of the concurrent validity expectations and 100% of the divergent validity expectations were met, showing validity of the MHI-5. Moreover, Spearman correlations between the MHI-5 and demographic characteristics were weak and non-significant.
Discussion
The aim of the present study was to examine the psychometric properties of the MHI-5 in persons with SCI. There were no ceiling and floor effects, but the total MHI-5 score was slightly skewed. The internal consistency and the concurrent and divergent validity of the MHI-5 were good.
Validity of the MHI-5 in persons with SCI compared with the general Dutch population
In the present study, the MHI-5 score showed no floor or ceiling effects. This is in accordance with studies in the general Dutch population, which also showed minimal floor and ceiling effects.20 The negative skewness of the MHI-5 in our sample was also found in two Dutch general population samples, which indicates that respondents scored towards the positive end of the mental health spectrum.20 The mean score on the MHI-5 (77.2) in our sample was high in comparison with other studies in persons with SCI, reporting mean mental health scores in the range of 68.9–75.4.5 The reliability of the MHI-5 (0.79) in our sample was satisfactory. In the general Dutch population, slightly higher figures were found (0.82–0.87).20 Cronbach's α was also somewhat lower than what have been reported for other mental health measures in persons with SCI.2 This can probably be attributed to the few items in the MHI-5. Finally, concurrent and divergent validity were good according to established criteria.18
The use of the MHI-5 in persons with SCI
Different methods have been used to find a cutoff point for the MHI-5 to determine a case of depression.11, 12 A cutoff point of 72 or lower refers to mental health problems, and of 60 or lower refers to severe mental health problems.11, 12 If we use these cutoff points, the prevalence of persons with SCI having mental health problems in our sample would be 37.2% and 13.8%, respectively. Percentages in the range of 20–60% have been found in studies using the Beck Depression Inventory or the Older Adults Health and Mood Questionnaire for persons with SCI scoring in the clinical range.1 Percentages between 8.8 and 12% have been found in studies using the Patient Health Questionnaire-9 for persons with SCI who have a probable major depression disorder.1 In other words, the MHI-5 shows prevalence rates in the same range as other validated and reliable instruments to measure depression in persons with SCI. Therefore, the MHI-5 might be useful as a depression screen in persons with SCI.
Limitations of the present study
A limitation to the present study was that only Dutch persons with SCI between 18 and 65 years with expected permanent wheelchair dependency admitted to a rehabilitation centre were included. Moreover, persons who had a non-traumatic injury or a higher age had a higher chance of dropping out of the study. This influences the degree to which the results of our study can be generalized to the whole population of persons with SCI. A second limitation is that we did not include another mental health instrument or use clinical diagnostic interviews to assess depression. This would have improved the assessment of the concurrent validity of the MHI-5 and allowed for assessment of its properties as a screener in this population. A third limitation is that we were not able to assess the test-retest reliability and the responsiveness of the MHI-5. The test-retest reliability of the SF-36 is, however, acceptable in persons with SCI.5 Further longitudinal studies are needed to examine the test-retest reliability and the responsiveness of the MHI-5 in persons with SCI.
Conclusion
The MHI-5 is a brief, and easy to score self-administered measure. The results of this study show good validity of the MHI-5 as a measure of mood in persons with SCI. Because the SF-36 is already a popular instrument in persons with SCI, the MHI-5 has great potential to become an often used mental health measure in this diagnostic group.
Data archiving
There were no data to deposit.
References
Post MW, van Leeuwen CM . Psychosocial issues in spinal cord injury: a review. Spinal Cord 2012; 50: 382–389.
Sakakibara BM, Miller WC, Orenczuk SG, Wolfe DL . SCIRE Research Team. A systematic review of depression and anxiety measures used with individuals with spinal cord injury. Spinal Cord 2009; 47: 841–851.
Ware JE, Snow KK, Kosinski M, Gandek B . SF-36 Health Survey: Manual & Interpretation Guide. The Health Institute, New England Medical Center: Boston. 1993.
Wood-Dauphinée S, Exner G, Bostanci B, Exner G, Glass C, Jochheim KA et al. SCI Consensus Group. Quality of life in patients with spinal cord injury--basic issues, assessment, and recommendations. Restor Neurol Neurosci 2002; 20: 135–149.
Ku JH . Health-related quality of life in patients with spinal cord injury: review of the short form 36-health questionnaire survey. Yonsei Med J 2007; 48: 360–370.
Cuijpers P, Smits N, Donker T, ten Have M, de Graaf R . Screening for mood and anxiety disorders with the five-item, the three-item, and the two-item Mental Health Inventory. Psychiatry Res 2009; 168: 250–255.
Rumpf HJ, Meyer C, Hapke U, John U . Screening for mental health: validity of the MHI-5 using DSM-IV Axis I psychiatric disorders as gold standard. Psychiatry Res 2001; 105: 243–253.
Means-Christensen AJ, Arnau RC, Tonidandel AM, Bramson R, Meagher MW . An efficient method of identifying major depression and panic disorder in primary care. J Behav Med 2005; 28: 565–572.
Friedman B, Heisel M, Delavan R. . Validity of the SF-36 five-item Mental Health Index for major depression in functionally impaired, community-dwelling elderly patients. J Am Geriatr Soc 2005; 53: 1978–1985.
de Groot S, Dallmeijer AJ, Post MW, van Asbeck FW, Nene AV, Angenot EL et al. Demographics of the Dutch multicenter prospective cohort study ‘Restoration of mobility in spinal cord injury rehabilitation’. Spinal Cord 2006; 44: 668–675.
Hoeymans N, Garssen AA, Westert GP, Verhaak PF . Measuring mental health of the Dutch population: a comparison of the GHQ-12 and the MHI-5. Health Qual Life Outcomes 2004; 2: 23.
Perenboom R, Oudshoorn K, van Herten L, Hoeymans N, Bijl R . Life Expextancy in Good Mental Health: Establishing Cut-offs for the MHI-5 and GHQ-12 (in Dutch). TNO-report: Leiden. 2000.
Fugl-Meyer AR, Eklund M, Fugl-Meyer KS . Vocational rehabilitation in northern Sweden. III. Aspects of life satisfaction. Scand J Rehabil Med 1991; 23: 83–87.
Eysenck H, Eysenck SB . Manual of the Eysenck Personality Scales (EPS Adult). Hodder & Stoughton: London. 1991.
Post MW, de Bruin AF, de Witte LP, Schrijvers AJ . The SIP68: a measure of health-related functional status in rehabilitation medicine. Arch Phys Med Rehabil 1996; 77: 440–445.
Hall KM, Cohen CE, Wright J, Call M, Werner P . Characteristics of the Functional Independence Measure in traumatic spinal cord injury. Arch Phys Med Rehabil 1999; 80: 1471–1476.
Maynard FM, Bracken MB, Creasey G, Ditunno JF, Donovan WH, Ducker TB et al. International standards for neurological and functional classification of spinal cord injury. Spinal Cord 1997; 35: 266–274.
Terwee CB, Bot SD, de Boer MR, van der Windt DA, Knol DL, Dekker J et al. Quality criteria were proposed for measurement properties of health status questionnaires. J Clin Epidemiol 2007; 60: 34–42.
Cohen J . Statistical Power Analysis for the Behavioural Sciences, 2nd edn Lawrence Erlbaum Associates: Hillsdale, NJ. 1988.
Aaronson NK, Muller M, Cohen PD, Essink-Bot ML, Fekkes M, Sanderman R et al. validation, and norming of the Dutch language version of the SF-36 Health Survey in community and chronic disease populations. J Clin Epidemiol 1998; 51: 1055–1068.
Acknowledgements
The authors would like to thank the participating Dutch rehabilitation centres, and the research assistants in these centres who collected all data: Rehabilitation Center De Hoogstraat (Utrecht), Reade, centre for rehabilitation and rheumatology (Amsterdam), Rehabilitation Center Het Roessingh (Enschede), Adelante (Hoensbroek), Rehabilitation Center Sint Maartenskliniek (Nijmegen), Center for Rehabilitation - Location Beatrixoord (Haren), Rehabilitation Center Heliomare (Wijk aan Zee), and Rehabilitation Center Rijndam (Rotterdam). This study was supported by the Dutch Health Research and Development Council, ZON-MW Rehabilitation program, grant no. 1435.0003 and 1435.0025.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
van Leeuwen, C., van der Woude, L. & Post, M. Validity of the mental health subscale of the SF-36 in persons with spinal cord injury. Spinal Cord 50, 707–710 (2012). https://doi.org/10.1038/sc.2012.33
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2012.33
Keywords
This article is cited by
-
The effect of breathing exercises and mindset with or without cold exposure on mental and physical health in persons with a spinal cord injury—a protocol for a three-arm randomised-controlled trial
Spinal Cord (2024)
-
Relationships between cardiovascular disease risk, neuropathic pain, mental health, and autonomic function in chronic spinal cord injury
Spinal Cord (2023)
-
The Effects of Physical Exercise on Depression for Individuals with Spinal Cord Injury: a Systematic Review
Current Physical Medicine and Rehabilitation Reports (2022)
-
Mental health, quality of life, self-efficacy, and social support of individuals living with spinal cord injury in Switzerland compared to that of the general population
Spinal Cord (2021)
-
Reliability, validity and responsiveness of the Dutch version of the AOSpine PROST (Patient Reported Outcome Spine Trauma)
European Spine Journal (2021)