Abstract
Study design:
Longitudinal, multiple wave panel design.
Objectives:
To investigate the degree to which current thinking in terms of early appraisals and coping predicts adjustment and quality of life outcomes after spinal cord injury, and to what degree social and demographic variables are involved.
Setting:
Data were analysed from 266 patients recruited as part of an ongoing study from specialist units in selected British, Swiss, German and Irish spinal centres.
Method:
Questionnaire booklets were administered as soon as possible after injury onset and after 12 weeks to patients with newly acquired spinal cord injuries. Individuals included had sustained their injury between the ages of 16 and 83.
Results:
Significant improvements in outcome measures were found across the data set within the first 12 weeks after spinal cord injury and changes observed in the appraisals and coping strategies employed. Significant differences were found between participating centres on both outcome measures and in the coping and appraisal processes used. Coping and appraisal processes at 6 weeks after injury were found to contribute significantly to the variation in psychological well-being at 12 weeks after injury.
Conclusion:
This study shows the process of adjustment to spinal cord injury to begin in the early stages of rehabilitation, and initial appraisals are important to how an individual will cope with their injury and to their psychological well-being. Support is also given to the importance of psychological factors to functional outcomes.
Similar content being viewed by others
Introduction
The occurrence of a spinal cord injury (SCI) will affect most major life areas and necessitate profound lifestyle changes. There is growing consensus that quality of life (QOL) is a fundamental issue for persons with SCI, principally because life expectancy of SCI individuals has increased substantially over the past 30 years. The majority of the literature suggests that QOL is markedly lower than that of non-disabled persons,1 and medical complications arising from SCI such as pressure sores, autonomic dysreflexia and respiratory problems have also been associated with lower QOL scores.
These findings have not only been evident in Europe, as shown in a recent paper by Barker et al.2 They focused on people with spinal cord injuries in an Australian community sample, and found that people with SCI rated themselves significantly lower on measures of QOL compared with able-bodied controls. These lower scores were associated with secondary conditions and lower levels of participation. A second study with paraplegic persons in Brazil found participants to report low physical, functioning and emotional QOL and low self-esteem scores.3
However, social factors such as employment have been found to have a positive influence on QOL in SCI individuals, with research showing significant differences in QOL scores found between employed and unemployed individuals.3, 4 Similarly, SCI individuals employed at least part time were found to perceive more control, experience less handicap and perceive more satisfaction with life.1
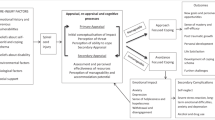
As cultures tend to vary in the value placed on attainments and goals,5 acceptance of disability6 and willingness to seek social support,7 variation in ratings of QOL would not be surprising. The importance of psychosocial factors on reported QOL have been replicated in a number of studies, finding educational level, financial security, social support8 and involvement in social activities9 to be significant predictors of QOL scores. However, despite the contribution of sociodemographic factors in explaining variance in QOL measures, SCI-related coping strategies have been found to be the most important correlate of QOL ratings in people with SCI. Furthermore, this finding remained true even when a large range of sociodemographic variables and social support were controlled for.10, 11 In respect to personality and cognitive factors influencing QOL, perceived control is integral. Specifically, persons with SCI who took sole responsibility for instructing their personal assistance services were found to perceive more control over their lives and reported greater life satisfaction.1
Adaptive coping strategies focusing on problems and acceptance of the injury have been implicated in psychological adjustment to SCI,12 and the use of ‘social reliance’ has been found to increase distress.10
In addition to the relationship between coping strategies and rehabilitation outcomes, coping variables are found to remain relatively stable across time. When demographically matched with an able-bodied control group, no differences were found in the coping strategies used over the course of 2 years.13 As such, the stability of coping measures suggests that there may be a dispositional component to coping, possibly accounting for the variability in how people adjust to SCI, and a finding with potential for clinical application when predicting adjustment difficulties.
The way in which an individual thinks about or ‘appraises’ a situation will influence the coping strategies employed,14 and therefore have an effect on psychological well-being. In relation to people with SCI, not only have appraisals been indicated in long-term psychological adjustment15 but also in terms of functional outcome measures. Using the Appraisals of Disability: Primary and Secondary Scale,16 Kennedy et al.17 found appraisals to explain 49.4% of the variance of Functional Independence Measure (FIM) scores.
The current research builds on findings from an earlier cohort study that investigated appraisals, coping and QOL across four community samples.18 The objectives of this study were to provide data on psychological responses, cognitive appraisals and coping strategies after SCI with patients during the first 12 weeks of rehabilitation; obtain information about the psychological situation of newly injured persons across specialist SCI centres from European countries, and assess the potential differences between countries; and to establish the extent to which appraisals and coping variables influence psychological well-being and QOL. In line with empirical findings,12, 14, 15 it is expected that early appraisals will be related to subsequent coping styles and that this will have an effect on ratings of psychological well-being and QOL.
Methods
Participants
All newly acquired injuries were taken from selected British, Swiss, German and Irish spinal centres with injuries representative of the SCI population. Individuals included had sustained their injury between the ages of 16 and 83 years and were fluent in the language of the country from which they were recruited. Individuals with a known head injury or communication disorder were excluded from the study, as such difficulties would prevent the comprehension and completion of the questionnaires.
Design
Longitudinal, multiple wave panel design was used for the study. Questionnaires were administered as soon as possible after injury onset and repeated after 12 weeks. Each country collected the data for one or more specific centres and entered into a standardized template. Data were entered using coded strings and stored in accordance to ethical guidelines. Ethical approval for this study was obtained from each Centre's local research ethics committee.
Materials
A double translation method was used for all questionnaires.
QOL (WHOQoL-BREF; 0–100)19, 20
An international, cross-culturally comparable QOL assessment instrument comprising of 26 items in four domains: physical health, psychological health, social relationships and environment. Higher scores on each subscale indicate a greater perceived QOL in that area. It has previously been used in the SCI population.20
Hospital anxiety and depression scale (HADS; 0–21)21
HADS enables detection of clinical cases and assessment of severity without contamination of scores through physical symptomology. Scores on Anxiety and Depression subscales can be obtained separately with higher scores indicating more psychopathology.
Functional independence measure (18–126)22
FIM assesses degree of independence in activities of daily living in six areas of function; higher scores indicate a higher level of independence.
Appraisal of life events (ALE; 0–30)23
A checklist of 16 adjectives was designed to elicit respondents’ cognitive appraisals of stressful life events in terms of threat, challenge and loss, with higher scores on subscales indicating the individual to appraise the current situation in this way. It has been shown to have a good factor structure, good test–retest reliability, internal reliabilities and construct validity.
Spinal cord lesion-related coping strategies questionnaire (SCL CSQr subscales; 1–4)24
SCL CSQr subscale was developed specifically for use with individuals with SCI to explore coping processes, it contains 12 items measuring 3 coping strategies: acceptance, fighting spirit and social reliance, higher scores indicate that the individual tends to use that coping strategy in the given situation. The scale has good psychometric properties, with acceptable internal validity correlations and internal reliability coefficients for the three strategies. The questionnaire used in this study contained amended wording of some questionnaire items, based on the findings of earlier research.25
Selected subscales from the COPE (4–16)26
The COPE is a generic coping measure, which measures coping styles as opposed to situation-specific coping strategies. This measure has been successfully used with a SCI population.27 Three subscales found in previous research to be associated with adjustment will be used: positive reinterpretation, behavioural disengagement and planning; again, higher scores indicate the greater use of a particular coping style.
Perceived manageability scale (PMnac; 6–24)28
This is a newly developed subscale of the Needs Assessment Checklist (NAC).29 The perceived manageability subscale of the NAC consists of six items measuring how often a participant has certain feelings or beliefs about their injury and/or situation on a 4-point scale. The scale aims to measure the extent to which an individual believes their situation is manageable, indicated by higher scores, and is designed to be sensitive to change.
The sense of coherence scale (SOC; 13–91)30
The SOC scale measures comprehensibility, manageability and meaningfulness in stressful life situations with greater scores indicating a higher SOC.
Procedure
Participants were approached shortly after admission to the rehabilitation centres and once medically stabilized provided with an information leaflet about the study. In practice, administration occurred at around 6 weeks after injury. For inpatients, questionnaires were administered by a psychologist in a face-to-face basis. A double-translation method was used for the questionnaires. At 12 weeks after injury, questionnaire booklets were re-administered.
Data included in this study is part of a longitudinal study looking at adjustment and coping during the first 2 years of injury.
Data analysis
Data were analysed using the Statistical Package for Social Sciences (SPSS). Data quality checks were performed to examine the distribution of measures and internal consistencies within scales.
Changes in measures were examined using paired sample t-tests. Because of the data from the Ireland population violating assumptions of normal distribution, the between centre analyses of variance were performed using a Kruskal–Wallis procedure.
Stepwise hierarchical regression analyses were performed on the outcome measures controlling for the effects of sociodemographic variables. Recent developments in the theoretical understanding of how appraisals can affect coping strategies and psychological well-being 31, 32 provided the rationale to use appraisals and perceived manageability as soon as possible after injury and coping strategies at 12 weeks after injury for these regression analyses.
Data quality
Descriptive statistics, including means, confidence intervals, skewness and kurtosis were computed for each variable. Scale distributions approximated normal distribution in the total sample, skewness and kurtosis were not outside an interval of ±1 for most scales. Scales that deviated from normal distribution were transformed to normality and used in the multi-variate analyses.
The assumptions of linearity and homoscedasticity were performed on the variables deviating from normality with no curvilinear relationships identified. Scale internal consistencies were mostly found to be >0.70; WHOQoL-BREF subscales ‘social’ and ‘environmental’ were found to deviate from this criteria and were therefore not included in the regression analyses.
Results
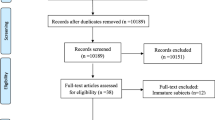
Response rates
For the initial stage of the study, 113 patients were approached to participate from the UK centre, of which 100 consented and completed the initial questionnaire booklet, giving a response rate of 88.5%. Of the German-speaking patients, the initial response rates were 62.5% for Basel, 100% for both Bad Wildungen and Berlin, 52% for Hamburg, 60% for Kreischa and 37.2% for Nottwil.
Demographics
The sample N=266 consisted of 208 males and 58 females. The sample age ranged between 16 and 83 years, with a mean age of 37.54 years (s.d.=14.55). Most of the samples were single (N=120) or married/cohabiting (N=112), followed by divorced (N=20), with four individuals widowed at the time of assessment 1.
Of the 252 responses, 38.1% (N=96) were in paid or voluntary employment at the time of injury. The majority of participants sustained a traumatic injury after a road traffic accident, 35.7% (N=95), followed by ‘fall’, 30.5% (N=81), ‘sporting accident’ 17.3% (N=46), ‘non-traumatic’ 8.3% (N=22) ‘other’ 6% (N=16) and ‘assault’ 2.3% (N=6). From the responses given, the sample contained more patients with paraplegia (N=125, 72 complete, 53 incomplete) than tetraplegia (N=106, 41 complete, 65 incomplete).
Differences in were compared for those employed and not employed at initial assessment. Significant differences were found in the outcome measures environmental QOL, t(217)=−2.106, P=0.036; social QOL t(218)=−2.262, P=0.025; and HADS depression subscale t(218)=2.1, P=0.037. Those in employment scored significantly higher on the SOC scale.
Effects of time
Means and standard deviations of measures at 6 weeks post-injury and 12 weeks post-injury for the total data set are displayed in Table 1.
QOL (WHOQoL-BREF, 4–20)
There was a significant increase in the QOL subscales ‘physical’, t(195)=8.534, P<0.001, and ‘psychological’, t(195)=2.528, P=0.012, between the two time points. There was no significant change in the QOL subscales ‘social’ and ‘environmental’.
Anxiety and depression (HADS, 0–21)
Scores for HADS anxiety and depression were grouped as ‘non-clinical’ (0–7), ‘possible case’ (8–10) and ‘clinical case’ (11–21). Less than 20% of the sample at 6 weeks (19.7% N=45) reached clinical criteria for anxiety, which decreased at 12 weeks after injury (13.2%, N=35). At 6 weeks after injury, 26.3% of the sample reached clinical criteria for depression (N=60). The percentage of people reaching clinical criteria for depression decreased at the 12-week time point to 16.9% (N=45).
No significant change in anxiety scores was observed between the two time points. There was a significant reduction in mean scores for depression from the 6 weeks after injury to 12 weeks after injury, t(195)=4.644, P<0.001.
Functional independence (FIM, 18–126)
There was a significant increase in the mean score of functional independence, as measured by the FIM, across the total sample between the two time points, t(190)=14.229, P<0.001.
Appraisal of life events (ALE subscales, 0–30)
Across the sample, there was a significant change in scores for ‘threat’, t(200)= 3.132, P=0.002 and ‘loss’ t(200)=3.233, P=0.001.
Spinal cord lesion coping strategies questionnaire (SCLCSQr subscales, 1–4)
Across the sample, there was a significant difference between the two time points for scores on ‘acceptance’, t(197)=−2.922, P=0.004 and ‘social reliance’, t(195)=7.277, P<0.001.
Coping orientations to problems experienced (COPE subscales, 4–16)
In the total sample, there was no significant change in scores between the two time points.
Perceived manageability (6–24)
Across the whole sample, there was a significant increase in scores for perceived manageability t(200)=−2.831, P=0.005.
Sense of coherence (13–91)
In the total sample, there was no significant change in scores between the two time points.
Effects of country
Following the rationale of previous research, data were analysed to investigate differences in scores between countries on appraisals, perceived manageability and SOC scores at initial time point; coping strategies and outcome measures were compared at 12 weeks after injury.
The means for each participating country for scores on perceived manageability, SOC and appraisal measures at 6 weeks after injury are displayed in Table 2. Means for each participating country on measures of coping strategies used at 12 weeks after injury are displayed in Table 3.
ALE
There were significant between country differences on the three ALE subscales ‘threat’ H=8.5, P=0.037, ‘challenge’ H=37.9, P<0.001 and ‘loss’ H=10.1, P=0.018.
PMnac
There was a significant difference between scores on the PMnac by countries, H=15.5, P=0.001.
SOC
There was a significant difference between countries on the SOC scores at 6 weeks after injury, H=18.3, P<0.001.
SCL CSQr
There were significant differences between countries on the SCL CSQr subscales ‘acceptance’ H=10.5, P=0.001 and ‘fighting spirit’ H=12.4, P=0.006.
COPE
There was a significant difference between countries on the COPE subscale ‘behavioural disengagement’ H=17.1, P=0.001.
HADS
There was a significant difference between countries on the HADS depression subscale H=16.1, P=0.001 at 12 weeks after injury.
WHO QOL-BREF
There were significant differences between countries on the physical H=9.4, P=0.024; psychological H=8.1, P=0.045; and environmental H=10.2, P=0.017 subscales.
FIM
There was no significant difference between countries in FIM scores at 12 weeks after injury.
Relationships between coping strategies and outcome measures
To investigate the explanatory contribution of scores on measures of appraisals at 6 weeks after injury and coping strategies at 12 weeks after injury to the variability in outcome measures at 12 weeks after injury, hierarchical multiple regression analyses were performed. Demographic and injury severity variables ‘gender’, ‘age’, ‘severity of impairment’ were controlled for in each regression model with appraisals, SOC and perceived manageability entered in step two and coping variables entered in step three. Because of Cronbach's α scores below 0.70, WHOQoL-BREF social and environmental were not included within these analyses. Results are displayed in Table 4.
The results of the regression models found the model to explain 47% of the variance in Functional Independence and ‘Physical’ QOL scores, 50% variance in anxiety scores, 57% variance in depression scores and 58% variance in the responses to the ‘Psychological’ section of the QOL questionnaire. The most notable predictors were the coping strategy social reliance, which has a significant unique contribution to the variance in all models, and SOC, which was present in all models aside from Functional Independence.
Discussion
This study investigated QOL, appraisals and coping in people with SCI across six European countries during the first 12 weeks of injury. The investigation follows previous work examining psychological aspects of SCI in people living in the community.18
Overall, the sample in this study was found to be psychologically well adjusted, with HADS anxiety and depression at normal levels. Scores on the WHOQoL-BREF were similar to those found in other studies,20 with significant increases in ratings of physical and psychological QOL between the two time points.
Scores on the FIM showed marked improvements from measurement at 6 to 12 weeks and was comparable to that found in the previous study.18
The current sample differed in the mean scores obtained on the appraisal measure compared with the previous research findings.18 Scores on ALE ‘loss’ and ‘threat’ were higher than those obtained in the previous sample, whereas the mean score for ‘challenge’ appraisals were lower than previous findings. However, these results may be due to the time since injury being considerably longer in the community sample (average 21 years).
Similarly, the scores on the coping strategies ‘fighting spirit’ and ‘acceptance’ were lower than those previously obtained18 and higher on measures of ‘social reliance’. As a revised version of the SCL CSQr scale was used in this study, it is possible that differences may be attributed to this change.
Significant differences were found between the countries in terms of the appraisal strategies, coping behaviours and in psychological and QOL outcomes. Participants from Switzerland were found to be the most likely to appraise their injury as a challenge and the least likely to appraise their injury as a loss. Participants from the UK were most likely to use ‘acceptance’ as a coping strategy while those from Switzerland were most likely to use ‘fighting spirit’ as a way of coping with their injury. Results from the COPE measure found that the Irish participants were least likely to use ‘behavioural disengagement’ as a coping strategy, whereas those from Switzerland were most likely. Participants from Switzerland scored significantly higher on measures of SOC; the lowest scored obtained from participants in the UK. On measures of perceived manageability, the Irish participants obtained the highest scores, whereas those from Germany scored the lowest.
Significant differences in outcome measures were found between countries; given the relationship between appraisals, coping strategies, behaviour and psychological well-being,31, 32, 33 these differences may be related to the use of differing styles of coping and in the appraisals made in response to SCI. There has been research to suggest the existence of specific differences in the ways that people from different European countries respond to stressors.34 To fully investigate this possibility, future research would need to explore the stability of these coping strategies and the relationship between these and participants’ long-term psychological well-being and adjustment to SCI.
Results from the regression analyses supported previous research.10, 11, 12, 17 Large proportions of the variance in outcome measures could be explained by early appraisals of injury and subsequent coping strategies. Interestingly, a significant contribution in explaining the variance in functional independence was found in the coping strategy ‘social reliance’. This confirms findings in other research,17 which highlights the often overlooked importance of psychological aspects in physical rehabilitation, and was verified by similar results in the model of physical rated QOL. The coping strategy ‘social reliance’ was present in the regression models of all outcome variables. ‘Social reliance’ refers to the way in which individuals with SCI look towards others for assistance in everyday living; feeling ‘dependent upon others’ and ‘helpless without support’ rather than being able ‘to manage on my own’. However, caution is advised in the interpretation of findings; in the present work, it is difficult to ascertain whether the negative influence of ‘social reliance’ on FIM scores is due to the nature of the individual's injury and greatly assisted hospital environment, or due to the individual adopted a resigned, dependent and unmotivated approach to physical rehabilitation after appraising their injury as a threat. However, in the paper by Kennedy et al.,17 the sample was taken from a community population who were no longer living in institutionalized settings. In this population, cognitive appraisals and coping strategies contributed significantly to the variance in FIM scores over and above demographic and injury variables, suggesting this result to be due to psychological, rather than environmental, factors. Future examination of this sample after discharge from hospital settings will provide some clarification to this issue.
The work of Lazarus and Folkman14 was supported by the significant contribution of threat appraisals and maladaptive coping strategies in explaining the variance in outcome measures of psychological well-being and QOL.
This study is part of ongoing research looking at adjustment to SCI. Although the authors acknowledge the relatively short time span during which observations were collected, the relationship found between coping and adjustment during the acute stage of rehabilitation provides a solid base from which to explore the stability of any interactions longitudinally, including the effect of hospital discharge and community living. Furthermore, investigation into the stability of coping and appraisals could provide further support to the importance of such psychological factors during early stages of rehabilitation on long-term physical and psychological adjustment.
Overall, the work of this research group continues to highlight the importance of psychological factors in predicting adjustment to SCI over and above demographic and injury variables, and more recently, have demonstrated the influence of psychological factors on functional independence outcomes.
The relative recency of such findings encourages further research in this field. Although the sample used in this study were measured on two time points, recent reviews15 emphasize the need for more longitudinal designs to investigate the continued influence of appraisals and coping through the life span.
The findings that countries differed in terms of appraisals and coping strategies leads the researchers to recommend further analysis in terms of the processes through which this occurs and the subsequent effect on rehabilitation outcomes over longer time periods.
The influence of coping strategies on outcome measures suggests the need for psychoeducational interventions during early rehabilitation such as the Coping Effectiveness Training programme, which has been found to reduce anxiety and depression in people with spinal cord injuries.33 However, this study found that although reducing distress, most coping strategies did not change, and therefore the intervention may have been targeting earlier cognitive processes such as appraisals and SOC. Recent developments31, 32 looking at Antonovsky's construct SOC, suggests that these factors may precede coping strategies and influence behaviour, ultimately effecting the psychological well-being of the individual. Such proposals are supported in this research by the contribution of appraisals and SOC to psychological regression models, and should be investigated further as a means of clinical intervention.
In summary, the findings from this study show the process of adjustment to SCI begins early in the rehabilitation period; significant changes in outcome measures were observed in the 6-week interval between assessments. The study also suggests that the initial appraisals made at the onset of injury can be important when assessing how an individual may cope with their SCI and how they engage in the rehabilitation process.
Support is given to previous research and highlights the importance of psychological factors in all aspects of SCI rehabilitation.
References
Chase BW, Cornille TA, English RW . Life satisfaction among persons with spinal cord injuries. J Rehabil 2000; 66: 14–20.
Barker RN, Kendall MD, Amsters DI, Pershouse KJ, Haines TP, Kuipers P . The relationship between quality of life and disability across the lifespan for people with spinal cord injury. Spinal Cord 2009; 47: 149–155.
Blanes L, Carmagnani MI, Ferreira LM . Quality of life and self esteem of persons with paraplegia living in São Paulo, Brazil. Qual Life Res 2009; 18: 15–21.
Westgren N, Levi R . Quality of life and traumatic spinal cord injury. Arch Phys Med Rehabil 1998; 79: 1433–1439.
Schwartz SH . A theory of cultural values and some implications for work. Appl Psychol Int Rev 1999; 48: 23–47.
Groce NE . Disability in cross-cultural perspective: rethinking disability. Lancet 1999; 354: 756–757.
Taylor SE, Sherman DK, Kim HS, Jarcho J, Takagi K, Dunagan MS . Culture and social support: who seeks it and why? J Pers Soc Psychol 2004; 87: 354–362.
Clayton KS, Chubon RA . Factors associated with the quality of life of long-term spinal cord injured persons. Arch Phys Med Rehabil 1994; 75: 633–638.
Dijkers M . Quality of life after spinal cord injury: a meta analysis of the effects of disablement components. Spinal Cord 1997; 35: 829–840.
Elfström ML, Kreuter M, Rydén A, Persson LO, Sullivan M . Effects of coping on psychological outcome when controlling for background variables: a study of traumatically spinal cord lesioned persons. Spinal Cord 2002; 40: 408–415.
Elfström ML, Rydén A, Kreuter M, Taft C, Sullivan M . Relations between coping strategies and health related quality of life in patients with spinal cord lesion. J Rehabil Med 2005; 37: 9–16.
Kennedy P, Marsh N, Lowe R, Grey N, Short E, Rogers B . A longitudinal analysis of psychological impact and coping strategies following spinal cord injury. Br J Health Psychol 2000; 5: 157–172.
Craig AR, Hancock K, Chang E . The influence of spinal cord injury on coping styles and self-perceptions two years after the injury. Aust N Z J Psychiatry 1994; 28: 307–312.
Lazarus RS, Folkman S . Stress, Appraisal and Coping 1984. Springer: New York.
Chevalier Z, Kennedy P, Sherlock O . Spinal cord injury, coping and adjustment: a literature review. Spinal Cord 2009; 47: 778–782.
Dean R, Kennedy P . Measuring Appraisals following spinal cord injury: a preliminary psychometric analysis of the appraisals of disability. Rehabil Psychol 2009; 54: 222–231.
Kennedy P, Smithson E, McClelland M, Short D, Royle J, Wilson C . Life satisfaction, appraisals and functional outcomes in spinal cord injured people living in the community. Spinal Cord 2010; 48: 144–148.
Kennedy P, Lude P, Taylor N . Quality of life, social participation, appraisals and coping post spinal cord injury: a review of four community samples. Spinal Cord 2006; 44: 95–105.
WHOQoL Group. Development of the World Health Organisation WHOQoL-BREF quality of life assessment. Psychol Med 1998; 28: 551–558.
Jang Y, Hsieh CL, Wang YH, Wu YH . A validity study of the WHOQoL-BREF assessment in persons with traumatic spinal cord injury. Arch Phys Med Rehabil 2004; 85: 1890–1895.
Zigmond AS, Snaith RP . The Hospital Anxiety and Depression Scale. Br Med J Clin Res Ed 1986; 292: 344.
Hamilton BB, Granger CV . Guide for the Use of the Uniform Data Set for Medical Rehabilitation 1990. Research Foundation of State University of New York: Buffalo, New York.
Ferguson E, Matthews G, Cox T . The appraisal of life events (ALE) scale: reliability and validity. Br J Health Psychol 1999; 4: 97–116.
Elfström ML, Rydén A, Kreuter M, Persson LO, Sullivan M . Linkages between coping and psychological outcome in the spinal cord lesioned: development of SCL-related measures. Spinal Cord 2002; 40: 23–29.
Elfström ML, Kennedy P, Lude P, Taylor N . Condition-related coping strategies in persons with spinal cord lesion: a cross-national validation of the Spinal Cord Lesion-related Coping Strategies Questionnaire in four community samples. Spinal Cord 2007; 45: 420–428.
Carver CS, Scheier MF, Weintraub JK . Assessing coping strategies: a theoretically-bases approach. J Pers Social Psychol 1989; 56: 267–283.
Kennedy P, Lowe R, Grey N, Short E . Traumatic spinal cord injury and psychological impact: a cross-sectional analysis of coping strategies. Br J Clin Psychol 1995; 34: 627–639.
Kennedy P, Scott-Wilson U, Sandhu N . The psychometric investigation of a brief and sensitive measure of perceived manageability. Rehabil Psychol 2009; 14: 454–465.
Berry C, Kennedy P . A psychometric analysis of the Needs Assessment Checklist (NAC). Spinal Cord 2002; 41: 490–501.
Antonovsky A . The structure and properties of the sense of coherence scale. Soc Sci Med 1993; 36: 725–733.
Kennedy P, Lude P, Elfström M, Smithson E . Sense of coherence and psychological quality of life in people with spinal cord injury: appraisals and behavioural responses. Br J Health Psychol 2009 (e-pub ahead of print).
Amirkhan JH, Greaves H . Sense of coherence and stress: the mechanics of a healthy disposition. Psychol Health 2003; 18: 31–62.
Kennedy P, Duff J, Evans M, Beedie A . Coping effectiveness training reduces depression and anxiety following traumatic spinal cord injuries. Br J Clin Psychol Med Settings 2003; 12: 93–98.
Gelhaar T, Seiffge-Krenke I, Borge A, Cicognani E, Cunha M, Loncaric D et al. Adolescent coping with everyday stressors: a seven nation study of youth from central, eastern, southern and northern Europe. Eur J Dev Psychol 2007; 4: 129–156.
Acknowledgements
We give their appreciation and thanks to all the patients who participated in the study. We also thank Margareta Kreuter for her help in the planning of the study and Yvonne Lude for her valuable assistance during the research. To those who gave their time to help with the recruitment and questionnaire process, and to all the staff at the specialist spinal injury units involved with this research, we thank them for their support.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Kennedy, P., Lude, P., Elfström, M. et al. Cognitive appraisals, coping and quality of life outcomes: a multi-centre study of spinal cord injury rehabilitation. Spinal Cord 48, 762–769 (2010). https://doi.org/10.1038/sc.2010.20
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2010.20
Keywords
This article is cited by
-
Illness perception of individuals with spinal cord injury (SCI) during inpatient rehabilitation: a longitudinal study
Spinal Cord (2022)
-
Cognitive appraisals of disability in persons with traumatic spinal cord injury: a scoping review
Spinal Cord (2022)
-
Body experience during post-acute rehabilitation in individuals after a traumatic spinal cord injury: a qualitative interview-based pilot study
Spinal Cord Series and Cases (2021)
-
The associations of acceptance with quality of life and mental health following spinal cord injury: a systematic review
Spinal Cord (2020)
-
Effects of a coping-oriented supportive programme for people with spinal cord injury during inpatient rehabilitation: a quasi-experimental study
Spinal Cord (2020)