Abstract
Study design:
Face-to-face interview.
Objectives:
Pain interference is an important outcome measure in clinical pain trials. However, after spinal cord injury (SCI), interference caused by pain may be difficult to separate from interference caused by the physical impairment. The objective of this study was to determine the ability of the Life Interference subscale of the Multidimensional Pain Inventory, SCI-version (MPI-SCI) to differentiate between pain-related interference and the interference caused by the physical impairments of SCI.
Setting:
VA Medical Center and Miami Project to Cure Paralysis, Miami, FL, USA.
Methods:
The subscales of the MPI-SCI (Life Interference (LI), Pain Interference with Daily Activities (PA), Performance of General Activities (GA)), pain intensity, Pain Disability Index (PDI), Functional Independence Measure (FIM), Beck Depression Inventory (BDI) and demographic/injury characteristics were assessed in persons with SCI and chronic pain (n=180).
Results:
After controlling for age, time since injury and severity of injury, LI subscale was highly correlated with the PA (r=0.58, P<0.001) and PDI (r=0.61, P<0.001) scores. LI subscale was also significantly correlated with pain intensity (r=0.29, P<0.001) and with the BDI (r=0.39, P<0.001). In contrast, LI subscale was not significantly associated with the GA or FIM scores.
Conclusions:
Because of the physical impairments associated with SCI, outcome measures specifically evaluating pain interference may be confounded. This study suggests that the LI subscale administered in an interview format is appropriate for measuring pain-specific interference in the SCI chronic pain population.
Similar content being viewed by others
Introduction
Heterogeneous pain is a common consequence of spinal cord injury (SCI), which often persists and interferes with a person's daily life long after the initial injury. In a recent study in SCI, a high level of pain interference was significantly predictive of a particular pain being viewed as ‘most disturbing’.1 Similarly, the Initiative on Methods, Measurement, and Pain Assessment in Clinical Trials (IMMPACT) group suggested that in addition to pain intensity, measures of physical and emotional functioning including pain interference were important domains to evaluate in clinical pain trials.2 However, measuring pain interference in people with SCI may not be straightforward because of the significant disability associated with the injury, which may complicate and confound the pain report.
In a recent effort to review the utility of pain measures in the SCI population both the Brief Pain Inventory (BPI) and the Multidimensional Pain Inventory, SCI-version (MPI-SCI)3 Life Interference (LI) subscale were recommended as useful measures of pain interference after SCI.4 These instruments have shown adequate psychometric properties in samples of persons with SCI and pain.5, 6 However, recent research in cancer patients suggests that it may be difficult for patients to differentiate between the interference caused by their pain from the interference caused by the functional limitations of their disease.7 Thus, the purpose of this investigation was to determine the ability of the MPI-SCI LI subscale to differentiate between pain-related interference and the interference caused by the physical impairments of SCI. To our knowledge, this has not been examined earlier in a sample with chronic pain and SCI. We hypothesized that LI scores would be significantly associated with pain-intensity ratings, depressed mood and pain-related disability and less associated with general activity or with functional impairment.
Materials and methods
Participants
Individuals (n=180) over 18 years of age with traumatic SCI and who experienced chronic pain participated in the study. Recruitment was conducted by advertisements posted around the Miami VA Medical Center (VAMC) and Miami Project to Cure Paralysis and by word of mouth. Each participant underwent a 2–3 h interview including a set of questionnaires and a neurological examination. The interviewers were trained before independently carrying out the interviews. The Institutional Review Boards of the Miami VAMC and University of Miami approved the study.
Demographic and injury-related characteristics
As part of the structured interview, participants were asked regarding demographic/injury characteristics (for example, age at time of study, time since injury, sex, etiology of injury and ethnic background).
Neurological examination
A physical examination was performed to assess neurological status. The grading of the injury was based on the ASIA impairment scale (AIS): ASIA A (no motor or sensory function in the sacral segments S4–S5) through ASIA E (normal motor and sensory function). AIS scores were calculated by adding the sensory and motor exam scores and were used in this study to reflect severity of injury.
Measures
MPI-SCI
The MPI-SCI6 is adapted from the original version of the MPI,8 which is a self-report questionnaire based on the cognitive-behavioral perspective on chronic pain. The items of the MPI are answered on a 7-point Likert scale and assess pain severity, the impact of chronic pain, responses by significant others, and emotional and physical adaptation to chronic pain. The following subscales of the MPI-SCI were used in this study:
Life Interference subscale: The LI subscale of the MPI-SCI includes eight questions relating to interference with social/recreational activities, family-related activities, relationships including friendships, household chores, ability to plan activities and limitations due to pain (Table 1). This subscale has shown an internal consistency of 0.90 and a test–retest reliability of 0.81.6
General Activity subscale: The General Activity (GA) subscale assesses the degree of participation in various types of daily activities: household activities, activities away from home, social activities and outdoor activities (Table 2). This subscale has shown an internal consistency of 0.83 and a test–retest reliability of 0.69.6
Pain Interference with Daily Activities subscale: The Pain Interference with Daily Activities (PA) subscale addresses the degree to which activity levels are decreased specifically because of pain, as distinct from restrictions of activity due to other aspects of the SCI (Table 2). This subscale has shown an internal consistency of 0.94 and a test–retest reliability of 0.78.6
Pain Disability Index
The Pain Disability Index (PDI) is a self-report measure concerning the degree to which pain interferes with functioning in seven broad areas: family/home responsibility, recreation, social activity, occupation, sexual behavior, self-care and life support activity. The format for responses is an 11-point scale with anchors of 0 (no disability) and 10 (total disability). The internal consistency in the study by Tait and colleagues9 was 0.86 and test–retest reliability was 0.44.
Beck Depression Inventory
The Beck Depression Inventory (BDI) is a commonly used measure to assess depressed mood in chronic pain samples including SCI. It consists of 21 items rated on a categorical scale with each response category assigned a number from 0 to 4 with higher scores indicating greater emotional distress. The internal consistency ranges from 0.73 to 0.92 and the test–retest reliability ranges from 0.48 to 0.86.10
Functional Independence Measure
The Functional Independence Measure (FIM) is a reliable and valid instrument designed to assess the amount of assistance required for a person with a disability to perform basic life activities safely and effectively. In this study the motor scores were used, which consists of 13 items concerning mobility and self-care. The interviewers administered the FIM in a standard manner according to the ‘Guide for the Uniform Data Set for Medical Rehabilitation’.11
Pain intensity
Pain intensity was assessed using numerical rating scale (NRS) with anchors of 0 (no pain) and 10 (most intense pain imaginable). Participants were asked to rate the average pain intensity of their present pain. For comparative analysis between the LI subscale, PDI and pain intensity, NRS pain ratings were categorized as mild (1–4), moderate (5–6) and severe (7–10).12
Statistical analysis
All analyses were performed with SPSS 16.0 for Windows. Because interference of any type is likely to be affected by demographic and injury-related characteristics, partial correlation coefficients were calculated to control for the potential confounding influences of age, time since injury and severity of injury (that is, AIS scores). Analysis of variance with Bonferroni post hoc comparisons was used to examine the relationship between pain interference and mild, moderate and severe NRS pain ratings. All tests were 2-tailed and a probability less than 0.05 was chosen to indicate statistical significance.
Exploratory factor analysis
We used exploratory factor analysis to examine multivariate relationships among the LI subscale, NRS, BDI, PDI, PA and GA subscales, FIM and AIS scores. Principal component analysis was used as the method of factor extraction and the analysis was based on the correlation matrix and pair-wise relationships. Only factors with Eigenvalues greater than 1.0 were accepted. The factor loadings were sorted according to size and the oblique rotation method, Oblimin, was used to allow for possible correlation between factors.
Results
Participants
This study was part of a larger study where approximately 230 individuals were approached and 214 individuals completed a face-to-face interview. Of those, 180 individuals (78.3%) had a physical examination to assess neurological status. Of the 180 participants, 155 were men and 25 were women. Detailed demographic and injury-related characteristics are presented in Table 3.
Relationships between the LI subscale and pain and injury-related disability
After controlling for age, time since injury and severity of injury the LI subscale was significantly correlated with the degree of pain interference with daily activities as measured by the PA subscale (r=0.58) and with the degree of pain-related disability as measured by the PDI (r=0.61). The LI subscale was also significantly correlated with average pain intensity (r=0.29) and with level of depressed mood as measured by the BDI (r=0.39; Table 4).
As the PDI measures pain disability defined as ‘the extent to which chronic pain interferes with a person's ability to engage in various life activities’,8 the relationship between the LI subscale and each of the seven areas of activity assessed by the PDI was examined. Although LI does not evaluate the same domains as the PDI, each domain of the PDI was significantly associated with the LI subscale score: family/home responsibilities (r=0.55, P<0.001), recreation (r=0.53, P<0.001), social activities (r=0.57, P<0.001), occupation (r=0.50, P<0.001), sexual behavior (r=0.35, P<0.001), self-care (r=0.39, P<0.001) and life support activities (r=0.37, P<0.001).
Theoretically, pain-related interference should be more associated with measures of pain-related disability than with injury-related functional impairment in a disabled population. In this study, we hypothesized that the LI subscale would be minimally associated with the GA subscale and FIM motor score as the LI specifically measures interference due to pain. As expected, even after controlling for age, time since injury and severity of injury the LI subscale was not significantly associated with the GA subscale (r=−0.13) or to the FIM motor score (r=−0.17; Table 4).
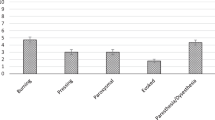
Relationship between average pain intensity and pain interference
As people reporting severe pain would be expected to report higher levels of pain interference compared with those with mild pain,4 the relationship between mild (1–4), moderate (5–6) and severe (7–10) pain intensity levels and pain interference was examined.12 One-way ANOVAs revealed that the average pain interference scores from the LI subscale and the PDI significantly (P<0.05) increased with increasing levels of pain intensity (Figures 1 and 2). Post hoc analysis revealed that the LI scores were significantly (P<0.05) higher in individuals with severe pain compared with individuals who experienced mild or moderate levels of pain. Although the PDI scores were significantly lower in individuals with mild pain compared with those who experienced severe pain, the PDI scores did not significantly differ between severe and moderate pain levels.
Multivariate relationship between pain interference and pain and injury-related factors
To examine the relationship among levels of pain intensity, pain interference, pain-related disability, depressed mood, degree of functional independence, general activity and injury severity, an exploratory factor analysis was performed including the LI subscale and the pain and injury-related variables. Two separate factors emerged in the final factor solution, which accounted for 58.9% of the variance (Table 5). The first factor (that is, pain-specific interference) included the LI subscale along with the PDI, the PA subscale, average pain intensity and the BDI and had factor loadings ranging from 0.46 to 0.85. The second factor (that is, injury-related interference) was composed of the FIM motor score grouped with the AIS and the GA subscale scores with factor loadings ranging from 0.66 to 0.88. These two factors were not significantly correlated with each other (r=0.06).
Discussion
The results of this study suggest that the LI subscale, when administered as a face-to-face interview, effectively measures pain-related interference as separate from the interference caused by the functional impairments of SCI. The multivariate analysis revealed two distinctly different factors, that is, pain-specific interference and injury-related interference. The latter factor is determined by the severity of injury, which significantly influences the functional status and independence of a person with SCI. Our results concur with a study in which FIM motor scores and ASIA motor scores were significantly associated at multiple time points after injury13 and with the idea that these two measures in combination reflect overall functional ability.14 The pair-wise analysis also supported this conclusion.
The factor labeled ‘pain-specific interference’ included pain-related disability and pain interference with daily activities, depressed mood and pain intensity. This result indicates that an individual who experiences severe pain is more likely to also experience higher levels of pain interference, depression and pain disability even after controlling for injury severity and other functional limitations. These results are also consistent with other studies in SCI where individuals experiencing pain reported higher levels of anxiety and depression than those without pain15 and where more intense pain was significantly associated with greater degree of pain-related disability.16 Recent research shows that levels of depression and anxiety experienced after SCI stay relatively unchanged even after 10 years following injury.17 Therefore, the association between depressed mood and pain-specific variables suggests that the long-term emotional distress experienced by these individuals is significantly influenced by the presence of persistent, unremitting pain. Similarly, earlier research in SCI shows that pain interference is correlated with negative affect even after controlling for the interference with activities and life enjoyment after SCI.18 Thus, persistent pain may reduce long-term life satisfaction over and above the impact of reduced control over one's life, affective distress and lower levels of general activities associated with SCI.6
Outcome measures used in clinical pain trials need to be sensitive to change to reflect small changes in pain severity. In this study, people with severe pain reported significantly higher pain interference levels when compared with those with mild and moderate pain intensity levels. A non-linear relationship between pain intensity and functional interference has been described earlier12 indicating that function is not impaired until the pain intensity reaches a threshold in the severe range. Therefore, the ability of the LI subscale to significantly distinguish between moderate and severe pain intensity is important as individuals with SCI report significantly less interference of pain with activities compared with other chronic pain populations.19
This study further examines the psychometric properties of the LI subscale in the SCI population. Although the LI subscale appears to be a useful measure to evaluate pain-specific interference after SCI, this measure does not directly assess the impact of pain on sleep and mood, which are considered important interference domains.20 In this study there were significant associations between the LI subscale and questions in the PDI relating to sleep and other life support activities (that is, eating and breathing), which are not specifically assessed by the LI subscale. This finding suggests that pain-related interference in different areas are interrelated (that is, when pain is severe it interferes with most daily activities including sleep). However, future studies should determine which specific domains are most relevant to pain interference after SCI.
Methodological considerations
The instruments used in this study were administered via face-to-face interviews to optimize consistency in data collection because some people with SCI are physically unable to fill out a battery of questionnaires. Although some studies suggest that interviews concerning health issues provide more detailed data, others suggest face-to-face interviews may also introduce various kinds of bias such as gender-induced differential responses. To what extent the interview format has influenced the results of this study is difficult to estimate. Future research should examine differences in responses to the different formats.
Finally, all participants in this study were volunteers who agreed to take part in research studies at the Miami VAMC and Miami Project to Cure Paralysis. They may not be representative of all persons with SCI and may present a selection bias. In our sample, 85.7% of our participants were men, 53.0% had a neurologically complete injury and 46.5% had cervical injuries. These frequencies are not substantially different from the National Spinal Cord Injury Database (http://images.main.uab.edu/spinalcord/pdffiles/Facts08.pdf), in which 77.8% of the participants are men, 41.3% have a neurologically complete injury and 52.4% have cervical injuries.
References
Felix ER, Cruz-Almeida Y, Widerstrom-Noga EG . Chronic pain after spinal cord injury: What characteristics make some pains more disturbing than others? J Rehabil Res Dev 2007; 44: 703–716.
Turk DC, Dworkin RH, Allen RR, Bellamy N, Brandenburg N, Carr DB et al. Core outcome domains for chronic pain clinical trials: IMMPACT recommendations. Pain 2003; 106: 337–345.
Widerström-Noga EG, Duncan R, Felipe-Cuervo E, Turk DC . Assessment of the impact of pain and impairments associated with spinal cord injuries. Arch Phys Med Rehabil 2002; 83: 395–404.
Bryce TN, Budh CN, Cardenas DD, Dijkers M, Felix ER, Finnerup NB et al. Outcome Measures for Pain after Spinal Cord Injury: an Evaluation of Reliability and Validity. J Spinal Cord Med 2007; 30: 421–440.
Raichle KA, Osborne TL, Jensen MP, Cardenas D . The reliability and validity of pain interference measures in persons with spinal cord injury. J Pain 2006; 7: 179–186.
Widerström-Noga EG, Cruz-Almeida Y, Martinez-Arizala A, Turk DC . Internal consistency, stability, and validity of the spinal cord injury version of the multidimensional pain inventory. Arch Phys Med Rehabil 2006; 87: 516–523.
Stenseth G, Bjørnnes M, Kaasa S, Klepstad P . Can cancer patients assess the influence of pain on functions? A randomised, controlled study of the pain interference items in the Brief Pain Inventory. BMC Palliat Care 2007; 6: 2.
Kerns RD, Turk DC, Rudy TE . The West Haven-Yale Multidimensional Pain Inventory (WHYMPI). Pain 1985; 23: 345–356.
Tait RC, Pollard CA, Margolis RB, Duckro PN, Krause SJ . The Pain Disability Index: psychometric and validity data. Arch Phys Med Rehabil 1987; 68: 438–441.
Beck AT, Steer RA . Internal consistencies of the original and revised Beck Depression Inventory. J Clin Psychol 1984; 40: 1365–1367.
Guide for the Uniform Data Set for Medical Rehabilitation (including the FIM instrument), Version 5.1. State Univ New York: Buffalo 1997.
Cleeland CS . The impact of pain on the patient with cancer. Cancer 1984; 54 (11 Suppl): 2635–2641.
Dvorak MF, Fisher CG, Hoekema J, Boyd M, Noonan V, Wing PC et al. Factors predicting motor recovery and functional outcome after traumatic central cord syndrome: a long-term follow-up. Spine 2005; 30: 2303–2311.
Marino RJ, Graves DE . Metric properties of the ASIA motor score: subscales improve correlation with functional activities. Arch Phys Med Rehabil 2004; 85: 1804–1810.
Budh CN, Osteråker AL . Life satisfaction in individuals with a spinal cord injury and pain. Clin Rehabil 2007; 21: 89–96.
Wollaars MM, Post MW, van Asbeck FW, Brand N . Spinal cord injury pain: the influence of psychologic factors and impact on quality of life. Clin J Pain 2007; 23: 383–391.
Pollard C, Kennedy P . A longitudinal analysis of emotional impact, coping strategies and post-traumatic psychological growth following spinal cord injury: A 10-year review. Br J Health Psychol 2007; 12: 347–362.
Summers JD, Rapoff MA, Varghese G, Porter K, Palmer RE . Psychosocial factors in chronic spinal cord injury pain. Pain 1991; 47: 183–189.
Widerström-Noga EG, Duncan R, Turk DC . Psychosocial profiles of people with pain associated with spinal cord injury: identification and comparison with other chronic pain syndromes. Clin J Pain 2004; 20: 261–271.
Widerström-Noga E, Biering-Sørensen F, Bryce T, Cardenas DD, Finnerup NB, Jensen MP et al. The International Spinal Cord Injury Pain Basic Data Set. Spinal Cord 2008; 46: 818–823.
Acknowledgements
This project was supported by the VARR&D (B3070R and B5023R), the State of Florida and the Miami Project to Cure Paralysis. The authors thank Dr Alberto Martinez-Arizala for performing the neurological examinations. We thank all of the participants for volunteering their time; without their participation, this study would not have been possible.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Cruz-Almeida, Y., Alameda, G. & Widerström-Noga, E. Differentiation between pain-related interference and interference caused by the functional impairments of spinal cord injury. Spinal Cord 47, 390–395 (2009). https://doi.org/10.1038/sc.2008.150
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2008.150
Keywords
This article is cited by
-
Prevalence and factors associated with a higher risk of neck and back pain among permanent wheelchair users: a cross-sectional study
Spinal Cord (2018)
-
The reliability of end of day and ecological momentary assessments of pain and pain interference in individuals with spinal cord injury
Quality of Life Research (2018)
-
A prospective study of pain and psychological functioning following traumatic spinal cord injury
Spinal Cord (2016)
-
Psychometric evaluation of the Spanish version of the MPI-SCI
Spinal Cord (2013)
-
Effects of chronic pain on quality of life and depression in patients with spinal cord injury
Spinal Cord (2013)