Abstract
In daily routine, many COPD patients report early onset augmented dyspnea following use of NIV (Deventilation Syndrome, DVS) as a negative side-effect. The aim of this study is the clinical characterization and concrete definition of DVS. This monocenter prospective observational study collected demographic, physiologic and symptomatic data from 67 in-patients with severe COPD Gold III–IV and chronic hypercapnic failure before, during and after use of an established NIV. During their inpatient follow-up, we examined patients during the first hour after termination of nocturnal NIV. DVS was defined by the authors as an increase of ≥ 2 points on the Borg scale during the first 30 min in patients who reported repeated dyspnea after the use of NIV. We monitored cardiovascular and respiratory data and measured diaphragm excursion. Subjective dyspnea was documented by use of the Borg scale and questionnaires. In addition, respirator and demographic data were collected. DVS occurred in 58% of our COPD patient collective, showing predominant emphysema phenotype. Patients with DVS were more severely ill than non-DVS concerning bronchial obstruction (FEV1 0.6 vs. 0.8 l, p < 0.05) and hypercapnia during spontaneous breathing (pre NIV pCO2: 54.5 vs. 49.3 mmHg, p < 0.02). DVS patients showed significantly higher respiratory rates (RR) (20.1 vs. 18.1/min p < 0.05) after termination of NIV. This trial characterizes and defines early onset augmented dyspnea after the use of NIV, referred to as DVS. It is hereby brought to attention as a frequent side effect of long-term home ventilation and possible pathophysiologic mechanisms are elucidated.
Similar content being viewed by others
Introduction
Non-invasive positive pressure ventilation (NPPV, NIV) is a widespread therapeutic option for patients with chronic hypercapnic failure due to COPD1,2. Effectively reducing hypercapnia by high-intensity ventilation can not only lead to improvement of health-related quality of life and lung function status, but has shown to reduce hospital re-admission and prolong long-term survival1. Persistent improvements of dyspnea in the daytime have also been documented3,4.
Aside many positive aspects, there are also negative side effects of NIV. Most commonly described are dryness of the upper airways, abdominal bloating or sleep fragmentation5,6, but also multifaceted fear of therapy7.
This study now describes a further, highly burdening side effect: early onset acute dyspnea following the use of NIV—augmented in the morning, but also after use during the day.
During ongoing NIV, patients experience relief of dyspnea and can breathe without effort. In some patients, termination of NIV within minutes leads to increasing dyspnea and discomfort. This is accompanied by tachypnea with rapid, shallow breathing, increased heart rate, the need to sit upright (coachman's seat) and the feeling of restlessness, sometimes even leading to panic attacks and fear of use of NIV. This state is hereby defined as the Deventilation Syndrome (DVS).
The term "Deventilation Syndrome" in the context of dyspnea after mask removal was first described by Adler and colleagues8.
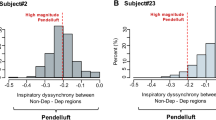
The authors hypothesized that in these patients, progressive hyperinflation, resulting from inappropriate ventilator settings, leads to patient-ventilator asynchrony (PVA) with a high rate of unrewarded inspiratory efforts and morning discomfort and identified inappropriate ventilator settings as a treatable cause of the problem in a group of 8 patients affected. Although this problem is common in clinical practice, there are no diagnostic criteria or recommended actions to address it. The aim of our study was to characterize DVS in patients with COPD and long-term home mechanical ventilation (LT-NIV) in order to better understand the pathophysiological background and by so to develop possible solutions for an improved care of the affected patients in the future.
Methods
Design
In a monocenter prospective observational study demographic, physiological and subjective data was collected from in-patients with severe COPD III–IV and chronic hypercapnic failure before, during and after use of an already established NIV.
Extended routine examinations included cardio-respiratory monitoring during and one hour after the nocturnal use of NIV, including ultrasonic diaphragm measurements. Subjective dyspnea was documented before and after use of NIV by use of the Borg scale and questionnaires were supplemented.
Being an observational study to document the Deventilation Syndrome, no study endpoints were defined. The authors refrained from power calculation due to the observational character of the study.
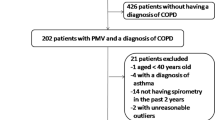
Patients
Between November 2016 and January 2019, 71 patients with severe COPD (Gold III–IV) and established long-term home NIV who presented to our center for elective control of their ventilation at home were included in the study. Sufficient data was collected from 67 patients. Inclusion criteria were: men and women with stable COPD disease, GOLD stage III–IV, regular use (≥ 4 h/d) of NIV (prescription ≥ 1 year) and age > 18 years. Study participation required written consent and patients had to be able to follow the requirements of the project. The study protocol was granted permission by the ethics review board of the University of Heidelberg, Germany (number S-484/2016) and all patients gave their written informed consent. The DVS study was conducted in accordance with the Declaration of Helsinki. During the study any medically necessary concomitant therapy was allowed. Intercurrent diseases were treated according to the clinic standard. Exclusion criteria were: Acute pulmonary impairment (e.g. pneumonia), other acute diseases such as acute pulmonary artery embolism, hemoptysis, internal bleeding, pneumothorax. In addition, serious neurological disorders (e.g. stroke) or cardiovascular diseases with hemodynamic instability (e.g. heart failure NYHA ≥ III, myocardial infarction < 1 month ago) were excluded, as also newly occurring hypoxemia or worsening of hypercapnia ≥ 20% compared to previous values.
Deventilation Syndrome (DVS)
DVS is determined by dyspnea—a highly subjective symptom. Being a novel syndrome, there is no definition of DVS to this date. Patients report recurring dyspnea episodes after the use of NIV, often preventing normal activities in the morning. This is accompanied by tachypnea with rapid, shallow breathing, the need to sit upright (coachman's seat) and the feeling of restlessness, sometimes even leading to panic attacks and fear of use of NIV. Objectification is best done by use of the modified Borg scale9. The minimal clinically importance difference (MCID) for Borg is 1 point10. For this study and further use of this terminology, DVS was defined by the authors as an increase of subjective dyspnea by ≥ 2 points on the Borg scale during the first 30 min after NIV termination—thus stressing the symptomatic and chronologic context after use of NIV. This threshold was determined in intention of clinical reflection of DVS, surpassing MCID of 1 point, but not excluding symptomatic patients who require symptom management.
Ethics approval
Ethics approval by Ethics Committee University of Heidelberg, S-484/2016.
Measurements
Survey examination timeline
During the study, medical history, questionnaires, vital signs, and functional examinations, including diaphragmatic ultrasound, were collected at various time points. The timeline of the study is shown in Fig. 1.
Pulmonary function diagnostics
These were carried out according to the internal standards of the lung function department of the University Thoraxklinik Heidelberg, using MasterScreenBody and PFT Body + Diff. by Care Fusion (Jaeger).
Body plethysmography: Documentation of body plethysmography (functional residual capacity (FRCpleth), specific airway resistance (sRaw), total lung capacity (TLC) and residual volume (RV), airway resistance was calculated by use of sRaw and FRC(pleth)) and spirometric data (vital capacity (VC), forced vital capacity (FVC), forced expiratory volume (FEV1) and percentage value FEV1/FVC index . Furthermore, measurement of diffusion capacity (TLCO) was documented.
Reference values were calculated according to GLI for spirometric parameters and TLCO11,12, while ECSC was referenced for body plethysmography13.
Respiratory muscle strength: capacity of respiratory muscles was measured non-invasively by maximal inspiratory mouth pressure (Pimax). Respiratory drive was measured indirectly by occlusion pressures (P0.1)14.
Ultrasonic diaphragm measurement
Measurements of diaphragm excursion were performed using the Philips Ultrasound Sparq with an abdominal transducer C 6-2. Patients were examined during spontaneous breathing on admission day (T0) and the following morning after termination of NIV (T1). This was done in a dorsal lying position, the torso elevated at approx. 45°. The right diaphragm was located in B-Mode and then excursion measured in M-Mode subcostal, mid clavicular line15,16. Pre and post NIV measurements on one patient were performed by the same examiner, two people in whole performed the exams by standardized procedure.
Measurement of carbon dioxide values and blood gas analysis
Carbon dioxide values were collected by two methods: continuous transcutaneous measurement and capillary blood draw (blood gas analysis, BGA), both examined on the earlobe.
BGA was assessed by arterialized capillary ear-lobe puncture earlobe skin17. The ABL 800 flex from Radiometer GmbH was used as blood gas analyzer. Transcutaneous CO2 measurement was performed using TOSCA transcutaneous monitor TCM 4, Radiometer during the night and 60 min after NIV termination. NIV parameter adjustments were performed when needed according to increased hypercapnia levels.
Monitoring
Nightly monitoring of patients undergoing long term home NIV is an essential part of NIV surveillance, reflecting the respiratory situation and efficiency of ventilation during and after sleep (RR, HR, BP, spO2, CO2). This standardized procedure was performed during nocturnal use and extended one hour after termination of NIV on our ward using Philips IntelliVue MX550 and TCM monitors. (Results spO2/HR/BP see supplementary information).
Questionnaires
Borg perception of exertion CR10 scale
Acquired by modified Borg scale (MBS) with 10-point dyspnea assessment9. An increase of ≥ 2 points after NIV termination was defined by the authors as relevant for DVS.
CAT: COPD Assessment Test
Cut off: < 10 = low impairment to > 30 = very high impairment18.
mMRC: Modified Medical Research Council
Score from 0 ("never breathless, except during intense exertion") to 4 ("too short of breath to leave the house or to dress and undress alone")19.
Statistical analysis
Baseline characteristics are presented for the whole sample and stratified by group (DVS vs. nDVS) by mean and standard deviation (SD) or median and interquartile range (IQR) or frequencies (n, %) as appropriate. Differences between groups were investigated by means of independent t-test, Mann–Whitney U test or chi-square test retrospectively. Continuous variables were explored graphically to justify parametric analysis.
Longitudinal models were applied to test for time × group effects for outcomes measured over time. Except for BORG (ordinal scale), a linear regression model with repeated measures statement was applied for each outcome with the explaining variables time, group, and interaction term. Group and time effects with confidence intervals and p value were presented based on the contrast between groups at each visit and contrasts between the visits for each group.
For Borg, the total score was analyzed descriptively by median (IQR) at the four measurement points in time for each group (DVS and nDVS).
To analyze the relationship of Borg and FEV1, Spearman correlation coefficients were calculated.
This is an exploratory analysis so that p values are interpreted descriptively. A p value < 0.05 was considered statistically significant. All analyses were performed in SAS version 9.4.
Results
Baseline characteristics
Between November 2016 and January 2019, 71 patients were included in the study. One patient was excluded due to double enrollment, three patients did not complete the Borg scale, therefore 67 patients were further evaluated. 39 patients were retrospectively diagnosed with DVS, 28 did not present DVS symptoms.
Enrollment included overall 28 males and 39 females (corresponding to 42% and 58% respectively). The mean (SD) age of all patients was 66.1 ± 6.7 years. Comorbidities were widespread, but severe and/or acute diseases were excluded according to the exclusion criteria of the study protocol. It is noteworthy that our COPD collective requiring NIV showed a predominant emphysema phenotype.
No serious complications occurred during the study, e.g. acute exacerbation of the disease. All patients were compliant with both participation in the study and with their NIV therapy. However, 5 patients did not wish to perform lung function tests. In all, 13 patients were unable to undergo or complete body plethysmography due to their physical constitution and extremely high lung inflation, one further patient had non legible RV rates. Interestingly, 11 of these 13 patients were retrospectively diagnosed with DVS.
Ventilatory setting
Ventilatory settings (VS) were documented (Table 1). The majority of patients was ventilated in ST mode (spontaneous/timed mode), 2 patients of the cohort used an aPCV mode (assisted pressure-controlled ventilation).
Subgroup characteristics—DVS versus nDVS
Subgroup characteristics are presented in Table 1.
Lung function analysis
Subgroup analysis of lung function measurements showed higher bronchial obstruction in patients with DVS and a trend to higher lung inflation. Lung inflation and respiratory muscle drive (P0.1) were elevated and respiratory muscle capacity (Pimax) was reduced in the DVS group compared to nDVS, though not statistically significant (p > 0.05) due to high drop-out rate in body plethysmography (insufficient maneuver). See Table 1, Supplement Fig. 6–7 (SF 6–7).
Carbon dioxide levels
When analyzing subgroup data, focus was placed on transcutaneous CO2 measurements. As there was no transcutaneous T0 data, capillary CO2 measurements were alternatively respected.
Patients with DVS had higher CO2 levels than nDVS patients at all times of measurement (Table 2). Hypercapnia was decreased during NIV in both subgroups, but remained higher in DVS. This effect was even clearer after NIV termination at T1 and T2.
Respiratory rate, subgroups
Respiratory rate (RR, breaths per minute (bpm)) was measured by continuous monitoring at four points of time (Fig. 2). It decreased significantly in the DVS group during use of NIV compared to spontaneous breathing. RR increase after termination of NIV was very clear and persisted up to one hour later. There was no significant difference in means between the RR at admission to after NIV termination.
Analysis in the nDVS group also showed a similar pattern with deceleration during and acceleration after use of NIV.
Subgroup comparison (Fig. 2,) of RR on the day of admission and undergoing ventilation showed no significant differences in means (p > 0.1), though a trend towards tachypnea in the DVS group was documented. Subgroup comparison after termination of NIV (T1) showed significant differences: mean RR in the DVS group was higher than nDVS. This effect did not persist at T2, though further marked a trend. See Fig. 2 (and Supplement: Table ST1).
Oxygen
There were no significant differences in oxygen saturation, both as independent variables at the different points in time and in a group as a dependent variable (Supplement: Table ST2, Fig. SF1).
Ultrasonic measurement of diaphragm excursion
The ultrasonic examination of the diaphragm was performed in all patients on day of admittance (T0) and the next morning after NIV termination (T1). In the overall group, T0 mean diaphragm excursion (± SD) was 1269 ± 559 mm, at T1 1069 ± 456 mm. Excursion difference between T0 and T1 (mean −200 mm) was statistically significant (p 0.03).
Inter-subgroup analysis showed a smaller difference of excursion rates between T0 and T1 in the DVS group compared to nDVS, though not statistically significant.
Borg scale CR10
67 patients correctly filled out the Borg scale.
For this trial, an increase of ≥ 2 points on the Borg scale within 30 min after NIV termination was defined as Deventilation Syndrome, based on the patient’s subjective dyspnea.
This criterion was met by 39 out of 67 patients, corresponding to a share of 58.2%. The majority of patients experienced dyspnea immediately after NIV termination (≤ 10 min), only 3 patients showed symptoms between 10 and 30 min. In the DVS group, baseline (T0) median (IQR) Borg score was 3.0 (3.0) points and dropped to 1.0 (3.0) points undergoing NIV (Tn). After NIV termination, Borg value increased to median of 5.0 (4.0) points during the first 10 min, over 90% of the DVS patients experienced greater respiratory distress in this first time segment. Within the next hour, median Borg values dropped continuously and settled after 60 min at 3.0 (3.0) points—thus meeting baseline levels (Fig. 3).
Patients without DVS showed very low variance of dyspnea and overall lower Borg scores (Fig. 3).
Borg scale and FEV1
There was a high correlation of Borg scale rankings and the severity of pulmonary impairment, measured by FEV1. Lower FEV1 levels were associated with more dyspnea (p < 0.01).
CAT
The CAT questionnaire documented a higher mean score in DVS patients than nDVS, reflecting lower FEV1 levels and higher disease burden. This effect was significant p < 0.01 (Table 1).
MMRC
The mMRC questionnaire revealed a significantly higher score in DVS than nDVS (median (IQR) 4.0 (2.0) vs. 3.0 (3.0) points, maximum of 4 points (0–4), p 0.02), reflecting higher respiratory distress in everyday life (Table 1).
Discussion
Acute dyspnea after the use of non-invasive ventilation (NIV) in a long-term setting is a common and stressful symptom in COPD patients. This is the first study to clinically characterize the Deventilation Syndrome (DVS) and suggest routine documentation of patient dyspnea and discomfort after the use of NIV as well as the objectified increase of dyspnea by > 2 points (Borg scale). Despite an abundance of publications on NIV in COPD, many also addressing negative side-effects, DVS has remained widely unaddressed.
DVS was identified in 58% of COPD patients with chronic hypercapnic failure in a routine in-patient setting, thus emphasizing the relevance of the subject. Ventilator settings were effective in both groups (DVS and nDVS), leading to significant decrease of CO2 levels and documented reduction of dyspnea per Borg scale undergoing NIV. Both groups were fully adapted to the regular use of NIV and showed no signs of discomfort or asynchronicity undergoing therapy. Nightly cardiovascular and pulmonary monitoring showed no signs of relevant sleep disordered breathing.
Dyspnea is a complex symptom and still not fully understood, though its role as a predictive marker in chronic lung diseases has been acknowledged20,21,22. It is highly subjective in perception and does not necessarily correlate with specific tests (e.g. spirometry, blood gas analysis), but dyspnea can—and should—be measured. Underlying mechanisms and qualities of dyspnea can be categorized in:
elevated work or effort in breathing (elevated mechanical load), tightness of the chest (bronchoconstriction) and intensity of air hunger (increased inspiratory drive, desensitized pulmonary mechanoreceptors)22. Following these main mechanisms can help understanding causes and thus provide therapeutic concepts in DVS. Ultrasonic measurement of the diaphragm showed significant (pre NIV 1269 mm, post-NIV 1069 mm, p 0.03) movement impairment after the use of NIV in the overall group, possibly expressing transient reduction of diaphragm muscle strength due to hyperinflation after use of NIV and diaphragm displacement. Bed-side lung function tests were not performed, but will be added in further trials. Variability of diaphragm movement was overall very high, though pre and post NIV examinations were performed by the same observer. There was no significance between each subgroup, though the differences of diaphragm movement pre and post NIV do strike as noteworthy (nDVS 260 mm vs. DVS 157 mm). Measurements of respiratory muscle strength via Pimax (from RV) were reduced in the DVS group compared to nDVS (4.0 vs. 5.0 kPa, p 0.06). Further assessment of the diaphragm function by ENMG or SNIP was not conducted in this trial but should be considered in further studies.
While diaphragm impairment seems to be well tolerated in some patients, it could pose the fundament of DVS—especially in context of accelerated respiratory rates. Changes of the respiratory rate (RR) provide a further, if not the main key in understanding DVS. Patients in both subgroups showed similar patterns of the RR: a significant drop from baseline to undergoing NIV—then picking up again back to baseline level (and exceeding baseline in DVS) after the use of NIV. Remarkably, dyspnea by Borg scale and RR did not differ in both groups at baseline (afternoon) measurement on admission day or undergoing NIV, thus showing a similar initial patient situation.
DVS shows an impact after use of NIV: in DVS, RR was higher than nDVS patients (T10min: 20.1 vs. 18.1 bpm, p 0.04) and remained elevated during the hour of monitoring (T60min: 20.4 vs. 18.9 bpm, p 0.1, though most DVS patients were subjectively recovered by Borg scale 60 min after NIV termination in this study. RR after use of NIV in DVS patients was higher than at T0 (baseline) although not statistically significant, so time adjusted RR change should be acknowledged. During the short period of 10 min post NIV, DVS patients showed a mean RR increase of 4.3 bpm, in nDVS 2.8 bpm.
Potential reasons for acute RR increase could be reduced diaphragm strength or elevated inspiratory drive due to higher CO2 levels in the DVS group (tCO2 T10min postNIV 54 vs. 48 mmHg, p < 0.01). Also, higher overall bronchial obstruction in DVS (FEV1 25% vs. 32.5% nDVS, p 0.01), furthermore augmented obstruction in the early morning hours (circadian, vagal stimulation, decreased medication levels), increases breathing muscle activity and effort and can trigger dynamic hyperinflation in already severely inflated lungs (RV DVS 6.1 vs. nDVS 5.4 L, p 0.1), thus circling into rapid shallow breathing (RSB). RSB and impaired diaphragm function have been identified as predictors for weaning failure23, reflecting relevant breathing muscle exhaustion. A possible negative influence of DVS on long-term prognosis of COPD patients with NIV is yet to be surveyed. It is also noteworthy that many DVS patients expressed fear of NIV termination in the morning due to experienced dyspnea in the past, posing a further possible cause for RR acceleration.
Furthermore, nocturnal patient-ventilator asynchrony (PVA) can currently not be ruled out as a conceivable trigger, as polygraphy was not carried out.
Higher levels of hypercapnia in patients with DVS are probably an expression of higher disease burden, as seen in the lung function tests—though underventilation with NIV cannot be fully ruled out.
Oxygen levels at any time also did not differ in both groups and thereby remain disregarded.
There are limitations in this trial to be discussed. First, assessment of diaphragm function was performed only by ultrasonic diaphragm excursion (DE) and only in two examinations, showing high standard deviation. Initially, DE was only thought an addendum to other focus topics—it now evolved to possibly one of the key features in DVS. In the future, more detailed data (e.g. diaphragm thickening index, repeated measurements) will be needed. Second, there was no guideline in the protocol concerning medication intake. This was intentionally put in the hands of each patient to decide by need, hence heterogenous treatment patterns. Subsequent trials should standardize this procedure. Third, monitoring was only continued for one hour during which some patients did not return to baseline level in terms of dyspnea, respiratory rate and CO2 levels. So, full duration of DVS has not yet been captured. Fourth, polygraphy was not initiated, which would undoubtedly enhance the data and illuminate possible patient-ventilator asynchrony. And fifth, true prevalence was not documented, as not all in-patients were screened for this study.
Despite many limitations in this trial, important data has been collected and helped establish potential key points concerning DVS. Therapy concepts have been established in our clinic and will be the focus of further trials.
Conclusion
In conclusion, DVS is a frequent, but to this day insufficiently regarded side effect of LTH-NIV. The recognition of DVS is of high clinical relevance for health care givers and patients. This trial offers not only definition of DVS, but also documents frequency of occurrence and relevant patient data leading to concepts of factors that presuppose DVS, by this stepping towards prevention and therapy of this often tormenting symptom. Further research is required to substantiate DVS and establish alleviating therapies.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on reasonable request.
Abbreviations
- BGA:
-
Blood gas analysis
- BP:
-
Blood pressure
- Bpm:
-
Breaths per minute
- CHRF:
-
Chronic hypercapnic respiratory failure
- COPD:
-
Chronic obstructive pulmonary disease
- DE:
-
Diaphragm excursion
- DVS:
-
Deventilation Syndrome
- ENMG:
-
Electroneuromyography
- EPAP:
-
Expiratory positive airway pressure inspiratory/expiratory ratio
- HR:
-
Heart rate
- IPAP:
-
Inspiratory positive airway pressure
- kHz:
-
Kilohertz
- kPa:
-
Kilopascals
- LTH-NIV:
-
Long term home non-invasive ventilation
- Mbar:
-
Millibar
- MmHg:
-
Millimeter of mercury
- nDVS:
-
Non Deventilation Syndrome
- NIV:
-
Non-invasive ventilation
- NPPV:
-
Non-invasive positive pressure ventilation
- pCO2 :
-
Arterial partial pressure of carbon dioxide
- PE:
-
Physical exam
- PEEP:
-
Positive end-expiratory pressure
- tCO2 :
-
Transcutaneous measurement of arterial partial pressure of carbon dioxide
- PVA:
-
Patient-ventilator asynchrony
- RR:
-
Respiratory rate
- RSB:
-
Rapid shallow breathing
- SNIP:
-
Sniff nasal inspiratory pressure
- SpO2 :
-
Oxygen saturation of hemoglobin measured by pulse oximetry
- TIMAX :
-
Maximal inspiratory time
- VE:
-
Minute ventilation
- VT :
-
Tidal volume
References
Kohnlein, T. et al. Non-invasive positive pressure ventilation for the treatment of severe stable chronic obstructive pulmonary disease: A prospective, multicentre, randomised, controlled clinical trial. Lancet Respir. Med. 2(9), 698–705 (2014).
Ergan, B. et al. European Respiratory Society guidelines on long-term home non-invasive ventilation for management of COPD. Eur. Respir. J. 54(3), 1901003 (2019).
Windisch, W. et al. Nocturnal non-invasive positive pressure ventilation: Physiological effects on spontaneous breathing. Respir. Physiol. Neurobiol. 150(2–3), 251–260 (2006).
Tsolaki, V. et al. One-year non-invasive ventilation in chronic hypercapnic COPD: Effect on quality of life. Respir. Med. 102(6), 904–911 (2008).
Windisch, W. et al. German National Guideline for treating chronic respiratory failure with invasive and non-invasive ventilation: Revised edition 2017—Part 1. Respiration 96(1), 66–97 (2018).
Carron, M. et al. Complications of non-invasive ventilation techniques: A comprehensive qualitative review of randomized trials. Br. J. Anaesth. 110(6), 896–914 (2013).
Ngandu, H., Gale, N. & Hopkinson, J. B. Experiences of noninvasive ventilation in adults with hypercapnic respiratory failure: A review of evidence. Eur. Respir. Rev. 25(142), 451–471 (2016).
Adler, D. et al. Polysomnography in stable COPD under non-invasive ventilation to reduce patient-ventilator asynchrony and morning breathlessness. Sleep Breath. 16(4), 1081–1090 (2012).
Borg, G. A. Psychophysical bases of perceived exertion. Med. Sci. Sports Exerc. 14(5), 377–381 (1982).
Ries, A. L. Minimally clinically important difference for the UCSD Shortness of Breath Questionnaire, Borg Scale, and Visual Analog Scale. COPD 2(1), 105–110 (2005).
Quanjer, P. H. et al. Multi-ethnic reference values for spirometry for the 3–95-yr age range: The global lung function 2012 equations. Eur. Respir. J. 40(6), 1324–1343 (2012).
Stanojevic, S. et al. Official ERS technical standards: Global lung function initiative reference values for the carbon monoxide transfer factor for Caucasians. Eur. Respir. J. 50(3), 1700010 (2017).
Quanjer, P. H. et al. Lung volumes and forced ventilatory flows. Report Working Party Standardization of Lung Function Tests, European Community for Steel and Coal. Official Statement of the European Respiratory Society. Eur. Respir. J. Suppl. 16, 5–40 (1993).
American Thoracic Society/European Respiratory S. ATS/ERS statement on respiratory muscle testing. Am. J. Respir. Crit. Care Med. 166(4), 518–624 (2002).
Matamis, D. et al. Sonographic evaluation of the diaphragm in critically ill patients. Technique and clinical applications. Intensive Care Med. 39(5), 801–810 (2013).
Boussuges, A., Gole, Y. & Blanc, P. Diaphragmatic motion studied by m-mode ultrasonography: Methods, reproducibility, and normal values. Chest 135(2), 391–400 (2009).
Langlands, J. H. & Wallace, W. F. Small blood-samples from ear-lobe puncture: A substitute for arterial puncture. Lancet 2(7407), 315–317 (1965).
Kon, S. S. et al. Minimum clinically important difference for the COPD assessment test: A prospective analysis. Lancet Respir. Med. 2(3), 195–203 (2014).
Mahler, D. A. & Wells, C. K. Evaluation of clinical methods for rating dyspnea. Chest 93(3), 580–586 (1988).
Parshall, M. B. et al. An official American Thoracic Society statement: Update on the mechanisms, assessment, and management of dyspnea. Am. J. Respir. Crit. Care Med. 185(4), 435–452 (2012).
Marin, J. M. et al. Prediction of risk of COPD exacerbations by the BODE index. Respir. Med. 103(3), 373–378 (2009).
Nishimura, K. et al. Dyspnea is a better predictor of 5-year survival than airway obstruction in patients with COPD. Chest 121(5), 1434–1440 (2002).
Khan, M. T. et al. Comparing ultrasound-based diaphragmatic excursion with rapid shallow breathing index as a weaning predictor. Cureus 10(12), e3710 (2018).
Funding
Open Access funding enabled and organized by Projekt DEAL. Specialized funding was not necessary nor initiated.
Author information
Authors and Affiliations
Contributions
First authorship is declared by the submitting author M.S. M.S. concepted study design, acquired participants, collected and interpreted data. S.I. and G.I. collected and analyzed substantial data in COPD patients including questionnaires and diaphragm ultrasound. M.K. analyzed and statistically approved all collected data. F.H. and F.T. analyzed and interpreted lung function and demographic data. All authors read and approved the final manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Schellenberg, M.D., Imach, S., Iberl, G. et al. Clinical characterization and possible pathophysiological causes of the Deventilation Syndrome in COPD. Sci Rep 12, 1099 (2022). https://doi.org/10.1038/s41598-022-05118-w
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-022-05118-w
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.