Abstract
The objective of this study was to compare the efficacy of abiraterone acetate with that of bicalutamide in combination with gonadotropin-releasing hormone (GnRH) antagonist treatment for patients with high-risk metastatic hormone-sensitive prostate cancer (mHSPC). A total of 149 patients with mHSPC who underwent treatment at our hospital and affiliated hospitals between December 2013 and July 2020 were retrospectively identified. Fifty patients were administered abiraterone acetate (1000 mg/day) plus prednisolone (5 mg/day) with a GnRH antagonist (degarelix) (group A), and 99 patients were administered bicalutamide (80 mg/day) with a GnRH antagonist (group B). The prostate-specific antigen (PSA) progression-free survival (PSA-PFS) was significantly longer in group A than in group B. Abiraterone acetate therapy and Gleason score were significant independent factors of PSA-PFS. Using propensity score matching, 56 matched patients were obtained. The PSA-PFS (p < 0.001) and overall survival (OS) (p = 0.0071) of patients with high-risk mHSPC were significantly longer in group A of matched patients. Abiraterone acetate therapy and Gleason score were significant independent factors for PSA-PFS in matched patients. The PSA-PFS and OS of patients treated with abiraterone acetate in combination with a GnRH antagonist were significantly better than those treated with bicalutamide.
Similar content being viewed by others
Introduction
Although prostate cancer today tends to be diagnosed at an early stage due to the introduction of prostate-specific antigen (PSA) screening, some patients with prostate cancer still present metastasis at the time of diagnosis in Japan11,2. The mechanism underlying prostate cancer metastasis remains unclear3. Androgen deprivation therapy (ADT) as systemic therapy is generally accepted as a standard of care for patients with metastatic hormone-sensitive prostate cancer (mHSPC)4. In Japanese clinical practice guidelines for prostate cancer, combined androgen blockade (CAB) therapy, which involves concurrent use of a gonadotropin-releasing hormone (GnRH) agonist and first-generation antiandrogen, such as bicalutamide, is recommended as the standard first-line therapy for metastatic prostate cancer. However, CAB therapy is not recommended in the National Comprehensive Cancer Network guidelines and the European Association of Urology guidelines5.
Recently, hormonal therapy using abiraterone acetate, a next-generation antiandrogen, was reported to improve overall survival (OS) and radiographic progression-free survival (PFS) in men with high-risk mHSPC who exhibit at least two of the following factors: Gleason score ≥ 8, at least 3 bone lesions, and the presence of visceral metastasis6. Although the superiority of abiraterone acetate plus prednisone with GnRH agonist over placebo with GnRH agonist for the treatment of high-risk mHSPC has been reported, there are two concerns regarding its application in clinical practice in Japan. First, as stated above, most patients with metastatic prostate cancer receive CAB therapy as first-line therapy in Japan7. Therefore, the effectiveness of abiraterone acetate plus prednisone with a GnRH analog should be compared with that of CAB therapy using bicalutamide. Second, the GnRH antagonist, degarelix, which does not induce a transient increase in testosterone to aggravate the symptoms, instead of GnRH agonist, is becoming a major component of ADT, especially for those who have a high metastatic burden in Japan8. However, there have been no reports comparing the efficacy of abiraterone acetate with that of bicalutamide in combination with GnRH antagonist treatment for high-risk mHSPC.
The aim of this study was to compare the efficacy of abiraterone acetate with that of bicalutamide in combination with GnRH antagonist treatment for high-risk mHSPC.
Methods
Patients and treatments
We retrospectively identified 149 patients with high-risk mHSPC at our hospital and affiliated hospitals in the KPUM Prostate Cancer Study Group between December 2013 and July 2020. All patients had two or more of the following factors: Gleason score ≥ 8, at least three bone lesions, and the presence of visceral metastasis. Fifty patients were administered abiraterone acetate (1000 mg/day) plus prednisolone (5 mg/day) with a GnRH antagonist (degarelix) according to the clinician’s preference (group A), and 99 patients were administered bicalutamide (80 mg/day) with GnRH antagonist according to the clinician’s preference (group B).
Bone and visceral metastases were assessed using bone scintigraphy and computed tomography (CT). The extent of disease (EOD) score9 was measured using bone scintigraphy. PSA recurrence was defined as two consecutive increases in PSA of 50% compared with nadir and ≧ 2 ng/ml on two consecutive measurement at least 1 week apart. This study was approved by the institutional review board of Kyoto Prefectural University of Medicine (ERB-C-1071-2) and of each affiliated hospital and was conducted in compliance with the Declaration of Helsinki. The institutional review board waived individual written informed consent due to the retrospective nature of this study. Opt-out information was provided to patients on the KPUM website.
Statistical analysis
The chi-square test and Wilcoxon rank sum test were used to compare the two groups as appropriate. Kaplan–Meier analysis was used to estimate the differences in time events between the two groups using the log-rank test. Univariate analysis was performed to determine the association of abiraterone acetate therapy, age, pretreatment PSA, pretreatment alkaline phosphatase (ALP) level, Gleason score, and EOD score with PFS. Multivariable analysis was performed using Cox proportional hazard models to investigate factors associated with PFS. Abiraterone acetate therapy, Gleason score, and EOD score were included as categorical variables. Age, pretreatment PSA level, and pretreatment ALP level were included as continuous variables. Hazard ratios (HRs) and 95% confidence intervals (CIs) were calculated. Propensity score matching was used to adjust the clinical backgrounds between the two groups. Age, pretreatment PSA, pretreatment ALP level, Gleason score, EOD score, and observation period were assessed and matched at a 1:1 ratio in the two groups. Statistical analyses were performed using SAS JMP version 14 (SAS, Cary, NC, USA), and statistical significance was set at p < 0.05.
Result
Clinical background of the patients
Table 1 shows the clinical backgrounds of the patients. Fifty patients were administered abiraterone acetate plus prednisolone with a GnRH antagonist (degarelix) (group A). Ninety-nine patients were administered bicalutamide with a GnRH antagonist (group B). There were no significant differences between groups A and B in terms of PSA pretreatment (p = 0.554). The patients in group A were significantly younger than those in group B (p < 0.001). The pretreatment ALP level, Gleason score, and EOD score of group A were significantly higher than those of group B (p = 0.0411, 0.0439, and 0.0402, respectively), indicating that the patients in group A had more advanced and aggressive disease than those in group B. The significantly shorter observation period of group A (p < 0.001) was probably due to the late approval of abiraterone acetate in Japan. Nine patients (18%) in group A and 77 patients (53%) in group B received life-prolonging subsequent therapy after PSA progression (Supplementary Table S1). Adverse events were uncommon in both groups. Although grade 3 or 4 liver-related adverse events were reported in six patients (12%) in group A, no other serious adverse events were reported in either group.
Prognostic factor of PSA-PFS
As shown in Supplementary Fig. S1, the PSA-PFS of group A was significantly longer than that of group B (p < 0.001). Age, pretreatment PSA level, Gleason score, EOD score, and pretreatment ALP level has been reported as prognostic factors associated with PSA control in mHSPC treatment10,11. Therefore, we performed Cox logistic regression analysis to investigate factors associated with PSA-PFS in patients with high-risk mHSPC using variables of those factors in addition to antiandrogen use (abiraterone acetate or bicalutamide). Abiraterone acetate therapy (HR 7.53, 95% CI 3.48–16.30; p < 0.001) and Gleason score (HR 17.99, 95% CI 3.73–52.10; p = 0.0001) were significant independent factors for PSA-PFS in high-risk mHSPC treatment (Table 2). However, the OS of patients with high-risk mHSPC was not significantly different between the two groups (p = 0.2631) (Supplementary Fig. S2).
Difference of effectiveness of abiraterone acetate and bicalutamide for patients with high-risk mHSPC adjusted by propensity score matching
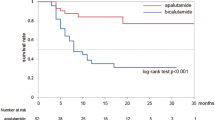
Because several factors associated with PSA-PFS and OS were significantly different between groups A and B (Table 1), we next used propensity score matching to adjust these clinical backgrounds between the two groups to examine the differences in patients with high-risk mHSPC more precisely. A total of 56 matched patients were obtained from the 149 patients. As described in Table 3, the clinical backgrounds were well adjusted between the two groups. The PSA-PFS (p < 0.001) and OS (p = 0.0071) of patients with high-risk mHSPC were significantly longer in group A of matched patients (Figs. 1, 2). Abiraterone acetate therapy remained a significant independent factor for PSA-PFS in matched patients (HR 7.09, 95% CI 2.45–20.56; p < 0.001).
Discussion
In this study, we retrospectively compared the efficacy of abiraterone acetate with that of bicalutamide in combination with GnRH antagonist treatment for high-risk mHSPC and found that PSA-PFS and OS were significantly better in patients treated with abiraterone acetate than in those treated with bicalutamide. In our hospital and affiliated hospitals, bicalutamide appeared to be administered more frequently than abiraterone acetate to elderly patients with high-risk mHSPC, as shown in Table 1. This may be because clinicians are concerned about possible adverse events in elderly patients. However, six patients older than 80 years in group A complained of no serious adverse events. These results could lead to an increase in the number of elderly patients with high-risk mHSPC treated with abiraterone acetate.
In Western countries, CAB therapy is rarely used as the standard first-line therapy for metastatic prostate cancer, whereas in Japan, it has been widely accepted since several previous reports have suggested that Japanese patients with prostate cancer respond to CAB therapy more effectively than other races12. For example, it has been reported that the adjusted prostate cancer-specific mortality in Japanese patients with prostate cancer who received CAB therapy is less than half of that in American patients with prostate cancer13. Several reasons, such as genetic and dietary/environmental factors, have been discussed to explain the discrepancy between countries14. Furthermore, the difference in typical dosage of bicalutamide (80 mg/day in Japan vs 50 mg in Western countries) has also accounted for the controversial results15. Another report has also suggested that the dose of bicalutamide is associated with PSA response16. In another study, Cooperberg et al. reported that CAB therapy improved survival more significantly compared with luteinizing hormone-releasing hormone monotherapy in men with very high-risk metastatic disease, but not in those with lower-risk metastatic tumors, indicating that CAB therapy may be more effective, especially in high-risk metastatic disease than in low-risk metastatic disease13. One of the most important points in the current study is that we showed the superiority of abiraterone acetate use over 80 mg of bicalutamide in Japan, where these drugs are often selected for the treatment of patients with high-risk mHSPC in a real clinical setting.
Tombal et al. suggested that the GnRH antagonist degarelix may be more effective than the GnRH agonist leuprolide for PSA control17. Furthermore, Kashiwabara and Suda reported that GnRH antagonists were more effective than GnRH agonists for CAB treatment of bone metastatic prostate cancer with pretreatment PSA levels ≥ 50 ng/mL8. There are several hypotheses about why GnRH antagonist treatment results in better outcomes than GnRH agonist treatment. A previous report suggested that GnRH antagonist treatment decreases PSA levels at a faster pace than GnRH agonist17. This rapid effect may result in better tumor control over a longer duration. Currently, almost all patients who have been diagnosed with high-risk mHSPC in our hospital also received GnRH antagonists instead of GnRH agonists. Although this study cannot evaluate the impact of GnRH antagonists for high-risk mHSPC, comparison of PSA-PFS and OS between GnRH agonists and antagonists in CAB therapy may be studied in the future. GnRH receptor expression has been reported in various types of malignant cells, including prostate cancer cells18,19. Both GnRH agonists and antagonists have been reported to decrease the proliferation of prostate cancer cells20. The in vitro comparison of growth suppression effects between GnRH agonists and antagonists may lead to a more profound understanding of the differential effect between the two drugs.
There was a phase III study which compared the efficacy of enzalutamide, other next-generation antiandrogen, with bicalutamide in combination with ADT for mHSPC. Enzalutamide improves overall survival (OS) and progression-free survival (PFS) of men with mHSPC more significantly than bicalutamide21. This is the first report to compare the efficacy of abiraterone acetate with bicalutamide in combination with a GnRH antagonist for high-risk mHSPC patients in Japan. However, it is important to note that the present study has several limitations. The patient cohort was small, and there was a significant difference in patient background because of the retrospective nature of the study. Moreover, the observation period was short, especially in patients treated with abiraterone acetate. Therefore, a further prospective study with a larger cohort over a longer period is required.
In conclusion, we demonstrated that abiraterone acetate with a GnRH antagonist may have advantages over bicalutamide with a GnRH antagonist in terms of OS and PSA-PFS in patients with high-risk mHSPC. The findings in this study could provide useful information when physicians choose a treatment plan for patients with high-risk mHSPC.
References
Ferlay, J. et al. Estimating the global cancer incidence and mortality in 2018: GLOBOCAN sources and methods. Int. J. Cancer 144, 1941–1953. https://doi.org/10.1002/ijc.31937 (2019).
Kimura, T. & Egawa, S. Epidemiology of prostate cancer in Asian countries. Int. J. Urol. 25, 524–531. https://doi.org/10.1111/iju.13593 (2018).
Santoni, M. et al. The origin of prostate metastases: Emerging insights. Cancer Metastasis Rev. 34, 765–773. https://doi.org/10.1007/s10555-015-9597-6 (2015).
Crawford, E. D. et al. Androgen receptor targeted treatments of prostate cancer: 35 years of progress with antiandrogens. J. Urol. 200, 956–966. https://doi.org/10.1016/j.juro.2018.04.083 (2018).
Hinotsu, S. et al. Current status of endocrine therapy for prostate cancer in Japan analysis of primary androgen deprivation therapy on the basis of data collected by J-CaP. Jpn. J. Clin. Oncol. 37, 775–781. https://doi.org/10.1093/jjco/hym098 (2007).
Fizazi, K. et al. Abiraterone plus prednisone in metastatic, castration-sensitive prostate cancer. N. Engl. J. Med. 377, 352–360. https://doi.org/10.1056/NEJMoa1704174 (2017).
Akaza, H. et al. Combined androgen blockade with bicalutamide for advanced prostate cancer: Long-term follow-up of a phase 3, double-blind, randomized study for survival. Cancer 115, 3437–3445. https://doi.org/10.1002/cncr.24395 (2009).
Kashiwabara, T. & Suda, S. Usefulness of combined androgen blockade therapy with gonadotropin-releasing hormone antagonist for bone metastatic prostate cancer with pretreatment prostate-specific antigen level ≥ 50 ng/mL. BMC Cancer 18, 619. https://doi.org/10.1186/s12885-018-4541-0 (2018).
Soloway, M. S. et al. Stratification of patients with metastatic prostate cancer based on extent of disease on initial bone scan. Cancer 61, 195–202. https://doi.org/10.1002/1097-0142(19880101)61:1%3c195::aid-cncr2820610133%3e3.0.co;2-y (1988).
Sano, T. et al. Impact of cardiac progenitor cells on heart failure and survival in single ventricle congenital heart disease. Circ. Res. 122, 994–1005. https://doi.org/10.1161/CIRCRESAHA.117.312311 (2018).
Miyoshi, Y. et al. Prognostic value of the bone scan index using a computer-aided diagnosis system for bone scans in hormone-naive prostate cancer patients with bone metastases. BMC Cancer 16, 128. https://doi.org/10.1186/s12885-016-2176-6 (2016).
Onozawa, M. et al. Combined androgen blockade achieved better oncological outcome in androgen deprivation therapy for prostate cancer: Analysis of community-based multi-institutional database across Japan using propensity score matching. Cancer Med. 7, 4893–4902. https://doi.org/10.1002/cam4.1735 (2018).
Cooperberg, M. R., Hinotsu, S., Namiki, M., Carroll, P. R. & Akaza, H. Trans-Pacific variation in outcomes for men treated with primary androgen-deprivation therapy (ADT) for prostate cancer. BJU Int. 117, 102–109. https://doi.org/10.1111/bju.12937 (2016).
Shiota, M. et al. Association of missense polymorphism in HSD3B1 with outcomes among men with prostate cancer treated with androgen-deprivation therapy or abiraterone. JAMA Netw. Open 2, e190115. https://doi.org/10.1001/jamanetworkopen.2019.0115 (2019).
Scher, H. I. et al. Bicalutamide for advanced prostate cancer: The natural versus treated history of disease. J. Clin. Oncol. 15, 2928–2938. https://doi.org/10.1200/JCO.1997.15.8.2928 (1997).
Klotz, L. et al. An open-label, phase 2 trial of bicalutamide dose escalation from 50 mg to 150 mg in men with CAB and castration resistance. A Canadian Urology Research Consortium Study. Prostate Cancer Prostat. Dis. 17, 320–324. https://doi.org/10.1038/pcan.2014.24 (2014).
Tombal, B. et al. Additional analysis of the secondary end point of biochemical recurrence rate in a phase 3 trial (CS21) comparing degarelix 80 mg versus leuprolide in prostate cancer patients segmented by baseline characteristics. Eur. Urol. 57, 836–842. https://doi.org/10.1016/j.eururo.2009.11.029 (2010).
Limonta, P. et al. GnRH receptors in cancer: From cell biology to novel targeted therapeutic strategies. Endocr. Rev. 33, 784–811. https://doi.org/10.1210/er.2012-1014 (2012).
Angelucci, C. et al. GnRH receptor expression in human prostate cancer cells is affected by hormones and growth factors. Endocrine 36, 87–97. https://doi.org/10.1007/s12020-009-9195-x (2009).
Castellón, E. et al. Effect of leuprolide and cetrorelix on cell growth, apoptosis, and GnRH receptor expression in primary cell cultures from human prostate carcinoma. Cancer Investig. 24, 261–268. https://doi.org/10.1080/07357900600629591 (2006).
Davis, I. D. et al. Enzalutamide with standard first-line therapy in metastatic prostate cancer. N. Engl. J. Med. 381, 121–131. https://doi.org/10.1056/NEJMoa1903835 (2019).
Acknowledgements
This report is based on the results of our hospital and affiliated hospitals. We express our gratitude for the cooperation of the urologists in the affiliated hospitals, including Hiroaki Miyashita, So Ushijima, and Toshiya Takamura, Department of Urology, Omihachiman Community Medical Center; Jintetsu So and Yuta Inoue, Department of Urology, Japanese Red Cross Daini Hospital; Shunji Harikai and Sojiro Hirano, Department of Urology, Kyoto Yamashiro General Medical Center; Yasuhiro Yamada, Kyoto Okamoto Memorial Hospital, Department of Urology; Kento Masuda, Department of Urology, Kyoto Kuramaguchi Medical Center; Tsuyoshi Iwata, Department of Urology, Kyoto Min-Iren Chuo Hospital; Kazuya Mikami and Naruhiro Kayukawa, Department of Urology, Japanese Red Cross Daiichi Hospital; Nobuhisa Hagiwara, Department of Urology, Maizuru Medical Center; Kenji Hiraoka, Department of Urology, North Medical Center Kyoto Prefectural University of Medicine; Hirokazu Ishida, Department of Urology, Uji Takeda Hospital; Kimihiro Yano, Department of Urology, Fujinomiya City General Hospital; Akihisa Ueno, Department of Urology, Saiseikai Suita Hospital; Masakatsu Oishi, Department of Urology, Aiseikai Yamashina Hospital; Motohiro Kanazawa and Asa Nakata, Department of Urology, Kyoto Chubu Medical Center; Naoki Hirahara and Ichiro Takeuchi, Department of Urology, Kyoto Kizugawa Hospital; Hidehisa Boku, Department of Urology, Kyoto Tanabe Central Hospital; Yusuke Gabata, Department of Urology, Ayabe City Hospital. We would like to thank Editage (www.editage.com) for English language editing.
Author information
Authors and Affiliations
Contributions
T.U., T.S. and O.U. wrote the main manuscript text and S.I., M.O., T.M., F.A., F.H. and K.O. prepared figures and tables. All authors reviewed the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary Information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Ueda, T., Shiraishi, T., Ito, S. et al. Abiraterone acetate versus bicalutamide in combination with gonadotropin releasing hormone antagonist therapy for high risk metastatic hormone sensitive prostate cancer. Sci Rep 11, 10094 (2021). https://doi.org/10.1038/s41598-021-89609-2
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-021-89609-2
This article is cited by
-
Apalutamide versus bicalutamide in combination with androgen deprivation therapy for metastatic hormone sensitive prostate cancer
Scientific Reports (2024)
-
Ontwikkelingen in de behandeling van gemetastaseerd hormoongevoelig prostaatcarcinoom
Tijdschrift voor Urologie (2024)
-
Relative search popularity of five advanced prostate cancer medications using Google Trends
Prostate Cancer and Prostatic Diseases (2023)
-
Predictive factors for the efficacy of abiraterone acetate therapy in high-risk metastatic hormone-sensitive prostate cancer patients
World Journal of Urology (2022)
-
Comparison of clinical outcomes between androgen deprivation therapy with up-front abiraterone and bicalutamide for Japanese patients with LATITUDE high-risk prostate cancer in a real-world retrospective analysis
International Journal of Clinical Oncology (2022)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.