Abstract
Attention-deficit/hyperactivity disorder is frequently reported in individuals with Down syndrome, with considerable variation in the expression and severity of the symptoms. Despite growing evidence that gestational age predicts later symptoms of attention-deficit/hyperactivity disorder in the euploid population, this has not been studied in down syndrome. The current study is designed to investigate the influence of gestational age in later symptoms of attention-deficit/hyperactivity disorder in 105 individuals (49 males and 56 females; aged 6–18 years) with Down syndrome who were born at or after 35 weeks gestation. Maternal age at birth, maternal level of education, household income, as well as sex, chronological age, and cognitive level of the participant with Down syndrome were considered in our analysis. Results from this study show that gestational age is related to inattentive and hyperactive/impulsive symptoms in children and adolescents with Down syndrome. Therefore, gestational age should be addressed when considering symptoms of attention-deficit/hyperactivity disorder, as it may have implications for early interventions. More attention is needed toward the advancement of care and follow-up for infants with down syndrome who are born even late preterm or early term.
Similar content being viewed by others
Introduction
Attention-deficit/hyperactivity disorder (ADHD) is characterized by inattention, including increased distractibility and difficulty sustaining attention, poor impulse control, and decreased self-inhibitory capacity, motor overactivity, and motor restlessness1. A mean worldwide prevalence of ADHD of ~ 2.2% overall (range 0.1–8.1%) has been estimated in the general population aged < 18 years2, with a higher prevalence often reported in males3. ADHD is also commonly associated with other neurodevelopmental disorders such as down syndrome (DS), with research indicating a mean prevalence of ~ 36.3% overall (range 31–43.9%)4,5,6 and no differences in prevalence between males and females with DS5. Most of those with DS and a clinical diagnosis of ADHD are diagnosed as predominantly inattentive5. A challenge in interpreting such findings, however, is the extent to which these attention-related symptoms are invariably part of the DS phenotype or are better viewed as secondary comorbid challenges due to ADHD. The high prevalence of comorbid psychiatric conditions in DS7 may further complicate the proper diagnosis of ADHD because of the many overlapping symptoms. We propose, therefore, that it may be best to avoid categorical diagnoses and instead investigate dimensions of attention-related problems, characterized as continuous variables8, in relation to DS.
Considering the variation in ADHD-like symptoms in the DS population and the high prevalence of other comorbid conditions9,10,11,12,13,14,15,16, a key challenge is to identify mechanisms underlying this variability. In this vein, a study of 83 children and young adults with DS found no association between ADHD and age, sex, number of siblings, presence of heart disease, thyroid dysfunction, sleep disorders, or family history of ADHD5. Another study showed that ADHD symptoms in youth with DS were related to the dopamine receptor D4 gene on chromosome 1117 similarly to the euploid population18,19.
Drawing on studies in the euploid population, the association between prematurity and ADHD is well established20. Studies have shown that children born early preterm (delivery at gestational weeks < 34) are rated with more symptoms of ADHD, inattention, and hyperactivity/impulsivity than term-born children21. Various mechanisms explain the observed association between early preterm birth and ADHD symptoms, all based on a lack of brain development in utero relative to full term babies22,23,24,25. Some studies have shown that at gestational week 35, the weight of the brain is around 60% of what it will be normally at term26. In addition, children born prematurely are at higher risk for postnatal complications and are often exposed to factors that can promote neuronal damage27. Even children born late preterm (delivery at gestational weeks 34–36) and early term (delivery at gestational weeks 37–38) score higher on ADHD symptoms later in development compared to children born at gestational week 39 or later22,23. Some studies have shown that the negative association between gestational age (GA) and ADHD may be strengthened by factors such as young maternal age, maternal smoking during pregnancy28, and low levels of maternal education23. Also, sex has been shown to moderate the relationship between GA and ADHD symptoms in euploid preschoolers, with the association appearing to be stronger among girls21. Early maternal age at birth (e.g., teenage) has been associated with ADHD symptoms22. This same study found an incremental risk for ADHD with each declining week of gestation, even after adjusting for maternal age at childbirth22. These findings, which have implications for targeted early interventions in the euploid population, may also have implications for individuals with DS, irrespective of whether they are considered part of the DS-phenotype or a co-occurring condition.
The fetal and neonatal brain in individuals with DS shows deviations from typical development. Whole brain and cerebellar volumes are smaller in DS from 21 weeks gestation, with cortical volumes deviating from that of the typically developing fetus around the third trimester29,30. This raises the possibility of even greater susceptibility to the negative effects of preterm and early term birth. The current study was designed to investigate the association between GA and later symptoms of ADHD in DS. The current study investigated this association in 105 children and adolescents with DS while taking into consideration potential confounding factors such as: chronological age (CA), sex, general cognitive level of participants with DS, maternal age at birth, maternal level of education, and family income.
Methods
Data source and study sample
Participants and measures reported in the present study are a subset of a larger multicenter project called The Down Syndrome Cognition Project (DSCP)31,32,33,34, a study of the cognitive and behavioral phenotype of individuals with Down syndrome and the factors influencing phenotypic variability. The study was conducted in accordance with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. Each site obtained their Institutional Review Board’s (IRB) approval to conduct the project. The progress of each site was monitored by the Emory Data Coordinating Center.
Participants were recruited through clinics, community events/referral, conferences, advertisements, internet postings, and participation in past research projects. The participating mother provided written consent and participants with DS provided verbal or written assent (when capable) before collecting the data presented in this study.
105 individuals participated in the present study; 49 males and 56 females; aged 6–18 years (M = 11.1 years, SD = 3.4), all for whom English was the primary language spoken at home. Participants were included in the current study if full trisomy 21 had been verified by karyotype, the biological mother was available for participation, and CA of participants with DS was ≤ 18 years. Participants were excluded if they had other chromosomal anomalies, GA prior to 35 weeks, history of epilepsy or other seizure disorder, history of head injury, history of chemotherapy, accidental poisoning, untreated severe hearing or vision loss, or incident of loss of consciousness > 5 min.
Measures
GA measured in weeks was reported by mothers, as was year of birth of mothers and year of birth of participants with DS. Information about previous ADHD diagnoses, ADHD medication, as well as other comorbid neurodevelopmental disorders, including ASD, was extracted from medical records if available and confirmed by mothers via maternal questionnaire. Maternal age (MA) at childbirth was computed as follows: year of birth of participant with DS–year of birth of mother. We also obtained socio-demographic information via maternal questionnaire as to the self-identified race/ethnicity of the participant with DS (defined by the participating mother), household income, paternal level of education, and maternal level of education.
Symptoms of ADHD were assessed using the Conners Parent Rating Scale, Third Edition (Conners-3)35 which reflects criteria for ADHD in the DSM-IV36 in individuals aged 6 -18. The Conners-3 contains two primary ADHD subscales (inattentive and hyperactive-impulsive) and other behavioral indices likely to co-exist with ADHD symptoms (i.e., learning problems, executive functioning, defiance/aggression and peer/family relations). In a normative sample, test–retest reliability coefficients ranged from 0.71 to 0.98, with strong discriminant validity between children with ADHD and other groups37,38. In a study of 154 children and adolescents with intellectual disability (ID), a Conners Parent Rating Scale total score of 42 provided a sensitivity of 0.9 and a specificity of 0.67 with an area under the curve of 0.84, with strong discriminant validity between children with ID with and without ADHD39. The parent version of the Conners-3 also has been used previously in other studies targeting ADHD symptoms of individuals with DS17,40, with mean T-scores consistent with diagnostic features of ADHD40. For our primary analyses, we used T-scores for the inattentive and the hyperactive-impulsive subscales as the primary symptoms of ADHD, as well as the global index T-score. Higher T-scores for each scale indicate more symptoms of ADHD endorsed by the parent informant.
General cognitive level was measured with the Kaufman Brief Intelligence Test, 2nd Edition41. The KBIT-2 assesses verbal and nonverbal cognition across a wide age range (4–90 years old). Our initial outcome was the KBIT-2 Composite IQ score (see Table 2 for descriptive values). However, floor effects emerged; that is, more than 20% of participants’ composite IQ scores were estimated to fall at or below 40 (the lowest possible derived IQ score). For this reason, we computed age-corrected scores from the KBIT-2 composite raw score [(KBIT-2 verbal raw score + KBIT-2 non-verbal raw score)/ 2] as determined by the KBIT-2 scoring manual41. The formula used for age-correction was as follows: ((KBIT composite raw score/CA) × 100)42,43,44.This method is similar to that done for the Mullen Scales of Early Learning, another test of general cognition45, and, as is true for standard scores, this formula produces different adjusted scores for children of different ages who earn the same raw scores. The KBIT-2 age-corrected score showed no floor or ceiling effects, no correlation with CA (r = 0.1), and a strong correlation with the KBIT-2 IQ score (r = 0.9).
Data analyses
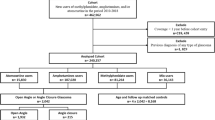
The first step consisted of a descriptive analysis of the sociodemographic and clinical parameters. Results are described using central tendency (mean values) and variability (standard deviation and range) for numeric variables, and absolute and relative frequencies for categorical variables in Tables 1 and 2. Figure 1 shows the frequency distribution of GA.
In order to decide whether our analyses needed to adjust for potential covariates, we first examined the association between GA and ADHD outcomes (i.e., Inattentive T-score, Hyperactive-Impulsive T-score, and Global Index T-score) for each of the following potential covariates: (1) CA of participant with DS at time of ADHD measurement, (2) KBIT-2 composite age-corrected score at time of ADHD measurement, (3) sex of participant with DS, (4) maternal age at birth, (5) maternal level of education and (6) family income. The computation of all correlations of interest was done using Pearson’s correlation coefficient for numeric variables and ANOVA models for categorical variables. Correction for multiple tests was performed in order to maintain a familywise alpha rate of p < 0.05. We then examined the contribution of GA to ADHD outcomes (i.e., Inattentive T-score, Hyperactive-Impulsive T-score, and Global Index T-score) in independent linear regression models. Multiple regression models were adjusted, when necessary, for potential covariates (i.e., if a potential covariate was related (p < 0.05) to GA or an ADHD outcome, this covariate was included in the regression model). All predictors were added to each regression model simultaneously. The same analyses were conducted excluding participants taking ADHD medication to see if that impacted our results. Correction for multiple tests was performed to maintain a familywise alpha rate of p < 0.05.
Secondary analyses were conducted to rule out a possible link between CA of the participant and parental response bias on the questionnaires. We examined the association between CA of participant and the positive and negative impression scales from the Conners-3. In addition, in order to confirm that higher scores in the Conners-3 were related to ADHD, a one way-ANOVA was conducted with ADHD diagnosis (yes/no) as the independent variable and ADHD outcomes (i.e., Inattentive T-score, Hyperactive-Impulsive T-score, and Global Index T-score) as dependent variables. All the variables included in the models were normally distributed (e.g., skewness (− 1,1) and (− 2,2) for kurtosis). Correction for multiple comparisons was achieved by using the False Discovery Rate (FDR) procedure46. All analyses were performed using the statistical software package SPSS (Version 18.0; SPSS Inc., Chicago, IL, USA).
Ethical approval
The authors assert that all procedures contributing to this work comply with the ethical standards of the relevant national and institutional committees on human experimentation and with the Helsinki Declaration of 1975, as revised in 2008. Informed consent was obtained from the parent or guardian of each participant before testing.
Results
Table 1 provides the demographical information about our study sample. Twenty of the 105 participants (19%) had a previous diagnosis of ADHD. Of those 20, 17 (16.2%) were taking ADHD medication. See supplementary Table 1 for co-occurrence of other neurodevelopmental disorders.
We found no association of ADHD outcomes or of GA with maternal age at birth, maternal level of education, family income or sex of participants with DS. However, CA of participants with DS at time of ADHD measurement was related to T-scores for the Inattentive subscale (R = − 0.25, p = 0.01) and the Hyperactive-Impulsive subscale (R = − 0.25, p = 0.01), as well as the Global Index of the Conners-3 (p = 0.001, R = − 0.32). CA was not related to the positive (R = − 0.08, p = 0.4) or the negative impression scores (R = 0.008, p = 0.9). In addition, the KBIT-2 composite age-corrected score at time of ADHD measurement was related to the Global Index of the Conners-3 (R = − 0.21, p = 0.04). See supplementary Table 2 for details. After controlling for multiple comparisons, only the relationship between CA and the Global Index of the Conners-3 remained significant. However, for a conservative approach, CA and general cognitive functioning at time of ADHD measurement were both included as covariates in the corresponding regression models reported below.
As seen in Table 3, multiple regression models show that GA is associated with T-scores for the Inattentive and Hyperactive-Impulsive subscales both before and after adjusting for CA of participants with DS at time of ADHD measurement. In addition, GA is associated with the Global Index of the Conners-3, before and after adjusting for CA, and the KBIT-2 composite age-corrected score at time of ADHD measurement. As represented in Fig. 2, lower GA is related to higher T-scores for ADHD measures from the Conners-3. The contribution of GA to T-scores from the Conners-3 excluding those participants taking ADHD medication showed similar results to those reported in the entire sample (see Table 4).
Secondary analyses focused on the correlation between having a diagnosis of ADHD and the Conners-3 total and subscale scores are reported in Supplementary Table 3. Participants with a reported diagnosis of ADHD had higher T-scores for the Inattentive subscale, the Hyperactive-Impulsive subscale and the Global Index of the Conners-3 compared to those who did not have an ADHD diagnosis.
Discussion
The present study is unique in assessing association of GA at birth with ADHD-like symptoms at 6 to 18 years of age in a group of 105 individuals with DS. This retrospective study found that an earlier GA (limited to those with GA of 35 weeks or more) was associated with more symptoms of ADHD among children and adolescents with DS, after adjusting for CA and general cognitive functioning at time of ADHD measurement. Our results are in line with those studies of the euploid population showing that children born early term as well as those born late preterm scored higher on ADHD symptoms compared to children born at gestational week 39 or later22,23. In the general population, various mechanisms have been proposed to explain the association between preterm birth and future neurodevelopmental difficulties. First, the immaturity of the brain relative to full term-expectations observed in the early weeks of gestation (i.e., ≤ 35 weeks) has been proposed as the main mechanism involved in long-term difficulties, including ADHD21,26. However, typically developing infants born even at a late preterm GA are at increased risk for morbidities in the immediate newborn period, including a higher rate of respiratory distress syndrome and transient tachypnea of the newborn when compared with term infants47,48. These problems could, in turn, lead to volumetric losses in specific brain regions and may partially explain the long-term difficulties related to ADHD symptoms21.
In the fetus with DS, differences in brain development and altered regional brain growth have been detected from 21 weeks of gestation when compared to controls; reduced cerebellar volume apparent in the second trimester, and significant alteration in cortical growth becoming evident during the third trimester, have also been reported29. Thus, we speculate that the effect of early GA on an already altered brain seen in DS may be greater than that for the euploid population. This would partly explain why we still see an effect of GA in long-term ADHD symptoms in our sample of late-preterm to full-term participants. Nevertheless, further longitudinal studies are needed to confirm this association and to examine the consequences of trisomy 21 molecular and behavioral levels. In contrast to the euploid population, the association between GA and long-term ADHD symptoms in DS was not more pronounced with inattention than with hyperactivity21,49,50. One reason for this difference might be the influence of trisomy 21 on brain development and its vulnerability to early GA. It could also be that we are not observing this differential pattern due to a lack of participants born early preterm and very early preterm in our sample relative to previous studies in the euploid population included21,49,50. Future studies should explore whether GA effects on ADHD symptoms in children and adolescents with DS by including those born before the 35th week of gestation.
Interestingly, the CA of the participants with DS was also related to ADHD outcomes. Our results showed that younger participants generally scored higher on inattentive, hyperactive, and general ADHD symptoms when compared to older participants. This finding is in line with previous research in DS51,52 and in the general population53. Taken together, these results suggest that although ADHD is chronic in nature, symptoms may present in different ways or in varying degrees as an individual moves through life stages54. One possible explanation may be that those with ID whose behavioral difficulties have been addressed over the years will have a range of learned strategies to use when ADHD-like symptoms become problematic55. However, it is important to note that our results are based on cross-sectional data and only participants from 6 to 18 years of age are included in our sample. In addition, we have no information on whether these families and their children have interventions to manage behavioral and cognitive difficulties typically observed in DS. Therefore, further longitudinal studies are needed to confirm the hypothesis that ADHD symptoms decrease over time in individuals with DS.
Importantly, the relationship between GA and later ADHD symptoms was still significant after adjusting for CA at time of ADHD measurement, suggesting that GA contributes to the later ADHD symptoms in addition to CA at time of ADHD measurement. Because the effect size of GA limited to 35 weeks and older was small, it remains to be determined whether the contribution of GA to later ADHD symptoms is clinically meaningful. However, these preliminary findings strongly suggest that more studies are needed that include participants with GA below 35 weeks to better to understand the full impact of early GA.
As expected, GA was not related to CA at time measurement, which rules out a potential confounding effect with ADHD symptoms. Therefore, this study adds to the growing body of evidence that indicates more attention needs to be paid toward the care and follow-up of infants born preterm, even those between GA of 35–39 weeks, perhaps even more so for those with DS.
The fact that the degree of cognitive delay was not related to the main symptoms of ADHD suggests that hyperactivity, impulsivity and inattention-related symptoms in those with DS are not a consequence of the ID; therefore, ADHD difficulties may be best conceptualized as comorbid challenges. However, it is important to note that although general cognitive functioning was not related to subscales of hyperactivity, impulsivity or inattention, it was related to the CA of the participants with DS. Indeed, CA explained more of the variance in the outcomes of the Conners-3 than did GA. These results suggest that symptoms of inattention and hyperactivity/impulsivity as reported by parents are more severe in younger individuals with DS. Our results are in line with the statistics reported from the Centers for Disease Control and Prevention (CDC) stating a higher percentage of ADHD diagnoses for children aged 6–11 compared to those aged 12–1756. Note, however, that the CA of participants with DS in our study was not related to the negative or the positive impression score from the Conners-3. Therefore, the link between CA and the Conners-3 rating is not explained by a response bias in the parents. However, further longitudinal investigations are needed to understand the link between CA and ADHD symptoms in DS including different methods and environments of assessment.
Other factors included in the present study that have been shown to be likely to contribute to ADHD outcomes in the euploid population did not show a correlation in our study sample. These include sex and maternal age at childbirth. One reason may be related to the characteristics of our sample. For example, maternal age at birth of the participating mothers was between 25 and 45 years of age, and GA was ≥ 35 weeks. Previous studies have reported a link between younger maternal age at birth and later ADHD symptoms28,57; however, we had few mothers in the younger age range and thus would not have the power to identify this association. In addition, those studies showing a link between maternal age at birth and GA have included babies who were born before the 35th week of gestation58. Another interesting result of our study was the fact that the presentation and severity of ADHD symptoms was not related to sex, which is in line with previous research in DS51,52, but differs from the typically developing population59. In addition, the lack of association between the level of general cognitive functioning and the severity of ADHD symptoms is also in line with previous research conducted in individuals with DS4. Therefore, although attention deficits and the symptomatology associated with ADHD appear with greater frequency in people with DS4,11,60,61,62, ADHD-related symptoms in this population are not better explained by the degree of ID. Taken together, our results suggest the need for similar monitoring of ADHD symptoms in both males and females with DS, regardless of the level of ID, to ensure appropriate health care.
Limitations
This study has several limitations. First, different methods are used to determine GA, for example, prenatal ultrasound or date of last menstrual period63. Bias may have occurred if the source of information to estimate GA is associated with both exposure (GA) and outcome (ADHD symptoms). Second, participants in the present study are part of a larger study (DSCP) in which GA < 35 was an exclusion criterion; including participants with GA < 35 would have increased our ability to examine the broader impact of fetal immaturity for those with DS. Our current results most likely underestimate this impact. Third, we relied on maternal reports of ADHD symptoms, which are not equivalent to a psychiatric evaluation. Finally, the current study is based on a cross-sectional evaluation of ADHD symptoms in relation to CA at time of ADHD symptom measurement.
Conclusion
In summary, findings from the current study are promising but need to be considered as preliminary, suggesting that GA plays a role in the later emergence of ADHD symptoms in children and adolescents with DS. Therefore, more attention must be focused on the advancement of care and follow-up for infants with DS who are born even late preterm or early term. Further longitudinal studies including other perinatal (e.g., fetal lung maturity, biophysical profile, birth weight, Apgar score), other methods of ADHD assessment and behavioral measures (e.g., Behavior Assessment Scale for Children), as well as including individuals with GA < 35, are needed to further explore the effects of fetal immaturity in future development for those with DS.
Data availability
The datasets used and/or analyzed during the current study are available from the corresponding author on a reasonable request.
References
DSM-5 Diagnostic Classification. In: Diagnostic and Statistical Manual of Mental Disorders (American Psychiatric Association, 2013). https://doi.org/10.1176/appi.books.9780890425596.x00DiagnosticClassification
Fayyad, J. et al. The descriptive epidemiology of DSM-IV Adult ADHD in the World Health Organization World Mental Health Surveys. ADHD Atten. Deficit Hyperact. Disord. 9(1), 47–65. https://doi.org/10.1007/s12402-016-0208-3 (2017).
Willcutt, E. G. The prevalence of DSM-IV attention-deficit/hyperactivity disorder: a meta-analytic review. Neurotherapeutics. 9(3), 490–499. https://doi.org/10.1007/s13311-012-0135-8 (2012).
Ekstein, S., Glick, B., Weill, M., Kay, B. & Berger, I. Down syndrome and attention-deficit/hyperactivity disorder (ADHD). J. Child Neurol. 26(10), 1290–1295. https://doi.org/10.1177/0883073811405201 (2011).
Edvardson, S. et al. Attention deficit hyperactivity disorders symptomatology among individuals with down syndrome. J. Policy Pract. Intellect. Disabil. 11(1), 58–61. https://doi.org/10.1111/jppi.12069 (2014).
Oxelgren, U. W. et al. Prevalence of autism and attention-deficit–hyperactivity disorder in down syndrome: a population-based study. Dev. Med. Child Neurol. 59(3), 276–283. https://doi.org/10.1111/dmcn.13217 (2017).
Dykens, E. M. Psychiatric and behavioral disorders in persons with down syndrome. Ment. Retard. Dev. Disabil. Res. Rev. 13(3), 272–278. https://doi.org/10.1002/mrdd.20159 (2007).
Lubke, G. H., Hudziak, J. J., Derks, E. M., van Bijsterveldt, T. C. E. M. & Boomsma, D. I. Maternal ratings of attention problems in ADHD: evidence for the existence of a continuum. J. Am. Acad. Child Adolesc. Psychiatry 48(11), 1085–1093. https://doi.org/10.1097/CHI.0b013e3181ba3dbb (2009).
Visootsak, J. et al. Neurodevelopmental outcomes in children with down syndrome and congenital heart defects. Am. J. Med. Genet. Part A 155(11), 2688–2691. https://doi.org/10.1002/ajmg.a.34252 (2011).
Capone, G. T., Aidikoff, J. M., Taylor, K. & Rykiel, N. Adolescents and young adults with down syndrome presenting to a medical clinic with depression: co-morbid obstructive sleep apnea. Am. J. Med. Genet. A 161A(9), 2188–2196. https://doi.org/10.1002/ajmg.a.36052 (2013).
Visootsak, J. & Sherman, S. Neuropsychiatric and behavioral aspects of trisomy 21. Curr. Psychiatry Rep. 9(2), 135–140 (2007).
Hoffmire, C. A., Magyar, C. I., Connolly, H. V., Fernandez, I. D. & van Wijngaarden, E. High prevalence of sleep disorders and associated comorbidities in a community sample of children with down syndrome. J. Clin. Sleep Med. 10(4), 411–419. https://doi.org/10.5664/jcsm.3618 (2014).
de Asua, D. R., Quero, M., Moldenhauer, F. & Suarez, C. Clinical profile and main comorbidities of Spanish adults with Down syndrome. Eur. J. Intern. Med. 26(6), 385–391. https://doi.org/10.1016/j.ejim.2015.05.003 (2015).
Capone, G. T., Grados, M. A., Kaufmann, W. E., Bernad-Ripoll, S. & Jewell, A. Down syndrome and comorbid autism-spectrum disorder: characterization using the aberrant behavior checklist. Am. J. Med. Genet. Part A 134A(4), 373–380. https://doi.org/10.1002/ajmg.a.30622 (2005).
Goday-Arno, A. et al. Hyperthyroidism in a population with down syndrome (DS). Clin. Endocrinol. (Oxf.) 71(1), 110–114. https://doi.org/10.1111/j.1365-2265.2008.03419.x (2009).
Roizen, N. J. Chapter one—overview of health issues among Persons with down syndrome. Int. Rev. Res. Ment. Retard. 39, 2–33. https://doi.org/10.1016/S0074-7750(10)39001-X (2010).
Mason, G. M., Spanó, G. & Edgin, J. Symptoms of attention-deficit/hyperactivity disorder in down syndrome: effects of the dopamine receptor D4 gene. Am. J. Intellect. Dev. Disabil. 120(1), 58–71. https://doi.org/10.1352/1944-7558-120.1.58 (2015).
Gornick, M. C. et al. Association of the dopamine receptor D4 (DRD4) gene 7-repeat allele with children with attention-deficit/hyperactivity disorder (ADHD): an update. Am. J. Med. Genet. Part B Neuropsychiatr. Genet. 144(3), 379–382. https://doi.org/10.1002/ajmg.b.30460 (2007).
Swanson, J. M. et al. Dopamine genes and ADHD. Neurosci. Biobehav. Rev. 24(1), 21–25. https://doi.org/10.1016/S0149-7634(99)00062-7 (2000).
Bhutta, A. T., Cleves, M. A., Casey, P. H., Cradock, M. M. & Anand, K. J. S. Cognitive and behavioral outcomes of school-aged children who were born preterm. JAMA 288(6), 728. https://doi.org/10.1001/jama.288.6.728 (2002).
Ask, H. et al. Association of gestational age at birth with symptoms of attention-deficit/hyperactivity disorder in children. JAMA Pediatr. 172(8), 749. https://doi.org/10.1001/jamapediatrics.2018.1315 (2018).
Sucksdorff, M. et al. Preterm birth and poor fetal growth as risk factors of attention-deficit/hyperactivity disorder. Pediatrics 136(3), e599–e608. https://doi.org/10.1542/peds.2015-1043 (2015).
Lindström, K., Lindblad, F. & Hjern, A. Preterm birth and attention-deficit/hyperactivity disorder in schoolchildren. Pediatrics 127(5), 858–865. https://doi.org/10.1542/peds.2010-1279 (2011).
D’Onofrio, B. M. et al. Preterm birth and mortality and morbidity: a population-based quasi-experimental study. JAMA Psychiatry 70(11), 1231–1240. https://doi.org/10.1001/jamapsychiatry.2013.2107 (2013).
Linsell, L., Malouf, R., Morris, J., Kurinczuk, J. J. & Marlow, N. Prognostic factors for poor cognitive development in children born very preterm or with very low birth weight a systematic review. JAMA Pediatr. 169(12), 1162–1172. https://doi.org/10.1001/jamapediatrics.2015.2175 (2015).
Heinonen, K. et al. Behavioural symptoms of attention deficit/hyperactivity disorder in preterm and term children born small and appropriate for gestational age: a longitudinal study. BMC Pediatr. 10, 91. https://doi.org/10.1186/1471-2431-10-91 (2010).
Farooqi, A., Hägglöf, B., Sedin, G., Gothefors, L. & Serenius, F. Mental health and social competencies of 10- to 12-year-old children born at 23 to 25 weeks of gestation in the 1990s: a Swedish national prospective follow-up study. Pediatrics 120(1), 118–133. https://doi.org/10.1542/peds.2006-2988 (2007).
Gustafsson, P. & Källén, K. Perinatal, maternal, and fetal characteristics of children diagnosed with attention-deficit-hyperactivity disorder: results from a population-based study utilizing the Swedish Medical Birth Register. Dev. Med. Child Neurol. 53(3), 263–268. https://doi.org/10.1111/j.1469-8749.2010.03820.x (2011).
Patkee, P. A. et al. Early alterations in cortical and cerebellar regional brain growth in down syndrome: an in vivo fetal and neonatal MRI assessment. NeuroImage Clin. 25, 102139. https://doi.org/10.1016/j.nicl.2019.102139 (2020).
Baburamani, A. A., Patkee, P. A., Arichi, T. & Rutherford, M. A. Dev. Med. Child Neurol. https://doi.org/10.1111/dmcn.14260 (2019).
Rosser, T. C. et al. associations between medical history, cognition, and behavior in youth with down syndrome: a report from the down syndrome cognition project. Am. J. Intellect. Dev. Disabil. 123(6), 514–528. https://doi.org/10.1352/1944-7558-123.6.514 (2018).
Edgin, J. O. et al. Development and validation of the Arizona cognitive test battery for down syndrome. J. Neurodev. Disord. 2(3), 149–164. https://doi.org/10.1007/s11689-010-9054-3 (2010).
Channell, M. M. et al. Characteristics associated with autism spectrum disorder risk in individuals with down syndrome. J. Autism Dev. Disord. 49(9), 3543–3556. https://doi.org/10.1007/s10803-019-04074-1 (2019).
Edgin, J. O. et al. The Arizona cognitive test battery for down syndrome: test–retest reliability and practice effects. Am. J. Intellect. Dev. Disabil. 122(3), 215–234. https://doi.org/10.1352/1944-7558-122.3.215 (2017).
Conners, C. K. Conners 3rd edition manual (2008).
Achenbach, T. M., Dumenci, L. & Rescorla, L. A. DSM-oriented and empirically based approaches to constructing scales from the same item pools. J. Clin. Child Adolesc. Psychol. 32(3), 328–340. https://doi.org/10.1207/S15374424JCCP3203_02 (2003).
Gallant S, Conners CK, Rzepal S, Pitkanen J, Marocco M-L, Sitarenios G. Psychometric properties ofthe Conners 3rd Edition. Poster Present Annu Meet Am Psychol Assoc San Fr CA. 2007.
Morales-Hidalgo, P., Hernández-Martínez, C., Vera, M., Voltas, N. & Canals, J. psychometric properties of the conners-3 and conners early childhood indexes in a Spanish school population. Int. J. Clin. Heal Psychol. 17(1), 85–96. https://doi.org/10.1016/j.ijchp.2016.07.003 (2017).
Deb, S., Dhaliwal, A.-J. & Roy, M. The usefulness of conners’ rating scales-revised in screening for attention deficit hyperactivity disorder in children with intellectual disabilities and borderline intelligence. J. Intellect. Disabil. Res. 52(11), 950–965. https://doi.org/10.1111/j.1365-2788.2007.01035.x (2008).
Capone, G. T., Brecher, L. & Bay, M. Guanfacine use in children with down syndrome and comorbid attention-deficit hyperactivity disorder (ADHD) With disruptive behaviors. J. Child Neurol. 31(8), 957–964. https://doi.org/10.1177/0883073816634854 (2016).
Kaufman, A. S., Kaufman, N. L. Kaufman brief intelligence test, second edition. In: Encyclopedia of Special Education. (Wiley, Hoboken, 2014). https://doi.org/10.1002/9781118660584.ese1325
Boer, H. International Handbook of Applied Research in Intellectual Disabilities, vol. 188 (Wiley, Hoboken, 2006). https://doi.org/10.1192/bjp.188.5.496.
Kaufman, A. S. IQ Testing 101 (Springer Publishing, New York, 2009).
Groth-Marnat, G. Handbook of Psychological Assessment. 4th ed. (Hoboken NJW ed. 2003). https://books.google.com/books?hl=es&lr=&id=ldF5oRto-HAC&oi=fnd&pg=PR13&ots=IeVHElmqbC&sig=NaRjiQFQSMv_gIoox977WYofY_I#v=onepage&q&f=false.
Hepburn, S., Philofsky, A., Fidler, D. J. & Rogers, S. Autism symptoms in toddlers with down syndrome: a descriptive study. J. Appl. Res. Intellect. Disabil. 21(1), 48–57. https://doi.org/10.1111/j.1468-3148.2007.00368.x (2008).
Benjamini, Y. & Yekutieli, D. The control of the false discovery rate in multiple testing under dependency. Ann, Stat. 29, 1165–1188. https://doi.org/10.2307/2674075 (2001).
Hibbard, J. U. et al. Respiratory morbidity in late preterm births. JAMA J. Am. Med. Assoc. 304(4), 419–425. https://doi.org/10.1001/jama.2010.1015 (2010).
McEvoy, C. et al. Respiratory function in healthy late preterm infants delivered at 33–36 weeks of gestation. J. Pediatr. 162(3), 464–469. https://doi.org/10.1016/j.jpeds.2012.09.042 (2013).
Johnson, S. & Marlow, N. Growing up after extremely preterm birth: lifespan mental health outcomes. Semin. Fetal Neonatal. Med. 19(2), 97–104. https://doi.org/10.1016/j.siny.2013.11.004 (2014).
Brogan, E. et al. Inattention in very preterm children: implications for screening and detection. Arch. Dis. Child 99(9), 834–839. https://doi.org/10.1136/archdischild-2013-305532 (2014).
Startin, C. M. et al. Health comorbidities and cognitive abilities across the lifespan in down syndrome. J. Neurodev. Disord. 12(1), 4. https://doi.org/10.1186/s11689-019-9306-9 (2020).
Naerland, T., Bakke, K. A., Storvik, S., Warner, G. & Howlin, P. Age and gender-related differences in emotional and behavioural problems and autistic features in children and adolescents with down syndrome: a survey-based study of 674 individuals. J. Intellect. Disabil. Res. 61(6), 594–603. https://doi.org/10.1111/jir.12342 (2017).
Baio, J. et al. Prevalence of Autism spectrum disorder among children aged 8 years — Autism and developmental disabilities monitoring network, 11 sites, United States, 2014. MMWR Surveill Summ. 67(6), 1–23. https://doi.org/10.15585/mmwr.ss6706a1 (2018).
Franke, B. et al. Live fast, die young? A review on the developmental trajectories of ADHD across the lifespan. Eur Neuropsychopharmacol. 28(10), 1059–1088. https://doi.org/10.1016/j.euroneuro.2018.08.001 (2018).
Wilens, T. E. & Spencer, T. J. Understanding attention-deficit/hyperactivity disorder from childhood to adulthood. Postgrad. Med. 122(5), 97–109. https://doi.org/10.3810/pgm.2010.09.2206 (2010).
Danielson, M. L. et al. Prevalence of parent-reported ADHD diagnosis and associated treatment among U.S. children and adolescents, 2016. J. Clin. Child Adolesc. Psychol. 47(2), 199–212. https://doi.org/10.1080/15374416.2017.1417860 (2018).
Chang, Z. et al. Maternal age at childbirth and risk for ADHD in offspring: a population-based cohort study. Int. J. Epidemiol. 43(6), 1815–1824. https://doi.org/10.1093/ije/dyu204 (2014).
Restrepo-Méndez, M. C. et al. The association of maternal age with birthweight and gestational age: a cross-cohort comparison. Paediatr. Perinat Epidemiol. 29(1), 31–40. https://doi.org/10.1111/ppe.12162 (2015).
Loomes, R., Hull, L. & Mandy, W. P. L. What is the male-to-female ratio in autism spectrum disorder? A systematic review and meta-analysis. J. Am. Acad. Child Adolesc. Psychiatry 56(6), 466–474. https://doi.org/10.1016/j.jaac.2017.03.013 (2017).
Capone, G., Goyal, P., Ares, W. & Lannigan, E. Neurobehavioral disorders in children, adolescents, and young adults with down syndrome. Am. J. Med. Genet. Part C Semin. Med. Genet. 142C(3), 158–172. https://doi.org/10.1002/ajmg.c.30097 (2006).
Myers, B. A. & Pueschel, S. M. Psychiatric disorders in persons with down syndrome. J. Nerv. Ment. Dis. 179(10), 609–613 (1991).
Di Nuovo, S. & Buono, S. Behavioral phenotypes of genetic syndromes with intellectual disability: comparison of adaptive profiles. Psychiatry Res. 189(3), 440–445. https://doi.org/10.1016/J.PSYCHRES.2011.03.015 (2011).
Behrman RE, Butler AS, Outcomes I of M (US) C on UPB and AH. Measurement of Fetal and Infant Maturity. 2007.
Acknowledgments
This work was funded primarily by the LuMind Research Down Syndrome Foundation. Additional support was provided by NIH grants P50HD103526, P30HD03352, and U54HD090256. We also want to thank the families who participated in this study and the many members of the Down Syndrome Cognition Project (DSCP) who conducted site recruitment and performance-based testing.
Funding
This study was approved by the Institutional Review Boards (IRB) of each participating site; Emory University (IRB00005100); University of California, Davis (IRB395392-1); University of Arizona (IRB00001751), Johns Hopkins University (IRB00031164), Oregon Health & Science University (IRB00003602), Children’s National Medical Center (IRB:Pro00002478), University of Wisconsin-Madison (IRB:SE-2010-0016) and University of Illinois Urbana-Champaign (IRB#17424).
Author information
Authors and Affiliations
Contributions
L.H.S. contributed to the study conception and study design and was responsible for the analysis of the data. L.H.S. and T.W. prepared figures and tables. L.H.S., L.A., S.S., T.R., D.H. and T.W. were responsible for interpretation of the data, as well as drafting and revising the manuscript. T.R. and D.H. were responsible for the collection and quality control of clinical data. All authors critically revised and approved the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher's note
Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons licence, and indicate if changes were made. The images or other third party material in this article are included in the article's Creative Commons licence, unless indicated otherwise in a credit line to the material. If material is not included in the article's Creative Commons licence and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this licence, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
del Hoyo Soriano, L., Rosser, T., Hamilton, D. et al. Gestational age is related to symptoms of attention-deficit/hyperactivity disorder in late-preterm to full-term children and adolescents with down syndrome. Sci Rep 10, 20345 (2020). https://doi.org/10.1038/s41598-020-77392-5
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41598-020-77392-5
This article is cited by
-
Associations Among Sex, Cognitive Ability, and Autism Symptoms in Individuals with Down Syndrome
Journal of Autism and Developmental Disorders (2024)
Comments
By submitting a comment you agree to abide by our Terms and Community Guidelines. If you find something abusive or that does not comply with our terms or guidelines please flag it as inappropriate.