Abstract
Asthma is a common non-communicable disease, often characterized by activity limitation, negative effects on social life and relationships, problems with finding and keeping employment, and poor quality of life. The objective of the present study was to conduct a systematic review of the literature investigating the potential factors impacting quality of life (QoL) in asthma. Electronic searches were carried out on: MEDLINE, EMBASE, PsycINFO, the Cochrane Library, and Web of Science (initial search April 2017 and updated in January 2019). All primary research studies including asthma, psychological or physical health factors, and quality of life were included. Narrative synthesis was used to develop themes among findings in included studies in an attempt to identify variables impacting QoL in asthma. The search retrieved 43 eligible studies that were grouped in three themes: psychological factors (including anxiety and depression, other mental health conditions, illness representations, and emotion regulation), physical health factors (including BMI and chronic physical conditions), and multifactorial aspects, including the interplay of health and psychological factors and asthma. These were found to have a substantial impact on QoL in asthma, both directly and indirectly, by affecting self-management, activity levels and other outcomes. Findings suggest a complex and negative effect of health and psychological factors on QoL in asthma. The experience of living with asthma is multifaceted, and future research and intervention development studies should take this into account, as well as the variety of variables interacting and affecting the person.
Similar content being viewed by others
Introduction
Over 235 million people worldwide are living with asthma, which is one of the leading non-communicable diseases worldwide.1,2 Symptoms, exacerbations, and triggers in asthma are associated with lower quality of life (QoL), tiredness, activity limitation, negative effects on social life and relationships, problems with finding and keeping employment, and reduced productivity.3,4,5,6,7 People with asthma are up to six times more likely than the general population to have anxiety or depression,8 and 16% of people with asthma in the UK have panic disorder,9 compared to 1% in the general population.10 People with brittle asthma (difficult-to-control asthma with severe, recurrent attacks) demonstrate even greater comorbidity and maladaptive coping styles.11 Psychological dysfunction is often unrecognized in primary care, despite being significantly associated with poor asthma outcomes, including asthma control and QoL.8,12,13 Indeed, the European Asthma Research and Innovation Partnership has identified understanding the role of psychological factors as an unmet need in improving asthma outcomes.14,15 They propose that anxiety and depression are present at all three stages of the experience of asthma: onset, progression, and exacerbation.14
A recent meta-analysis found that asthma diagnoses significantly increased the risk of psychological and health conditions (such as cardiovascular/cerebrovascular diseases, obesity, hypertension, diabetes, psychiatric and neurological comorbidities, gut and urinary conditions, cancer, and respiratory problems other than asthma).16 In addition, studies have pointed towards an impact on QoL in people with asthma of additional health and psychological factors, such as comorbid anxiety or depression, higher body mass index(BMI), professional status, and feelings of lack of control over health (for example, refs 17,18). Such evidence reinforces the argument that the needs of people with asthma should be approached in conjunction with these additional factors, rather than using a single-illness approach, aiming to reduce the adversity of people’s experience. However, the extent to which psychological and physical health factors interact and impact asthma outcomes is yet to be systematically explored. This systematic review aims to provide a narrative synthesis of the literature exploring psychological and physical health factors that influence QoL in adults with asthma.
Results
Study characteristics
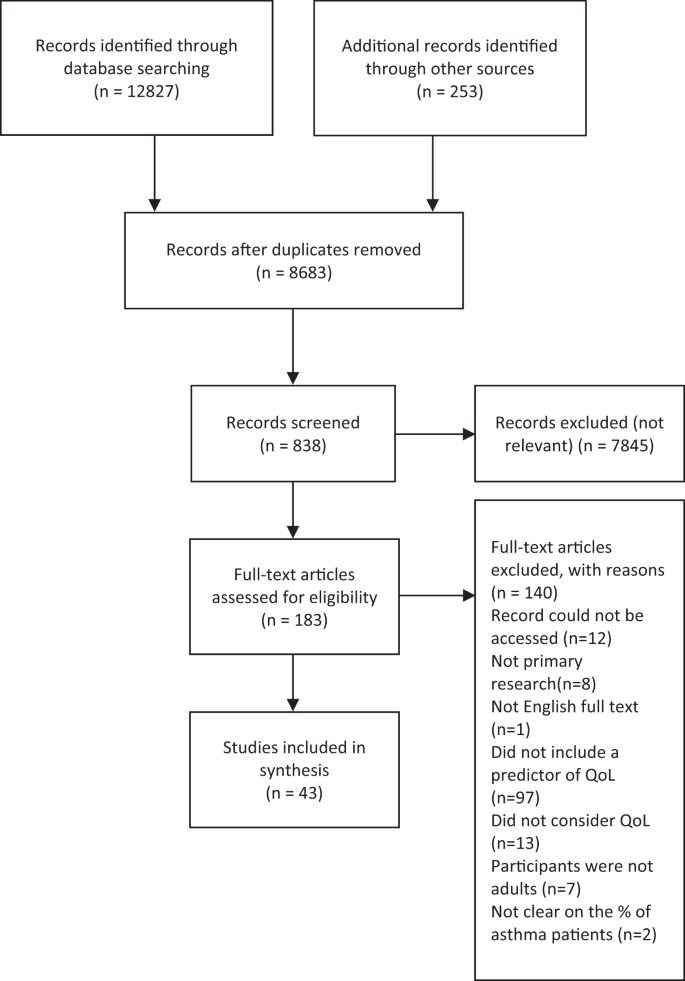
The search and screening process identified 43 eligible papers, published between 2003 and 2019 (see Fig. 1 for PRISMA flowchart19). The characteristics of each study are summarized below in Table 1. Twelve studies were conducted in Europe,20,21,22,23,24,25,26,27,28,29,30,31 17 in North America,12,32,33,34,35,36,37,38,39,40,41,42,43,44,45,46,47 7 in Australia,17,48,49,50,51,52,53 4 in Asia,54,55,56,57 and 3 in Africa.58,59,60 All papers employed a quantitative approach comprising 2 longitudinal studies31,44 and 41 cross-sectional studies. Only 4 studies included a control group.21,28,29,31 Overall, the majority of papers had a large sample size (ranging between 40 and 39,321 participants; 30 papers included a sample size of >100). The majority of studies recruited from primary care or the general population, using self-report to confirm a diagnosis of asthma. Only a few studies recruited from secondary and tertiary asthma clinics.12,27,36,41,44,48,60 There was a high occurrence (n = 14) of exclusion criteria relating to specific demographic or asthma characteristics, as well as mental health conditions and comorbidities, which restricted the study sample without a reason being given. Most studies used self-report measures,17,20,21,22,23,24,25,26,27,28,29,30,32,33,34,35,36,37,39,41,42,43,44,45,46,48,49,51,52,53,54,55,56,57,58,59,60 with a small proportion using psychiatric interviews to screen for mental health conditions.12,31,38,40,50 The majority of studies used asthma-specific QoL measures (n = 29),12,21,23,25,27,28,30,32,33,34,35,36,37,39,40,41,42,44,48,49,50,51,54,55,56,58,59,60,61 17 included an health-related QoL measure (n = 18),17,20,22,23,24,25,28,30,31,34,35,36,38,43,50,51,52,55 and 4 used general measures of QoL (n = 7);26,35,45,46,47,57,62 11 papers used >1 measure of QoL.23,25,28,30,34,35,36,37,50,51,55 The average age across included studies was 42.1 years (and 61.57% were female). Papers report prevalence rates of between 16.8% and 48.9% for depression and between 13.3% and 44.4% for anxiety,20,27,33,38,50,56,58,60 with an average of 28.31% for a diagnosis of anxiety or depression. Across several studies, the prevalence of other mental health conditions was 28.31% on average (ranging between 28% and 80%).12,37,38,40,42 Between 72% and 86.9% of people with asthma had at least one additional physical condition and between 21% and 26.3% had ≥2;25,34,56 26.36% had, on average, at least one other physical health condition. On average, people with asthma were significantly more likely to have a BMI of >30 (and between 61% and 75.1% had a BMI >25).26,45,59 The quality assessment identified that most studies were of a reasonable quality; however, it should be noted that some measures used could be considered inappropriate for the research aim or the population under investigation. Examples include measuring general QoL with an asthma-specific measure or administering a geriatric depression questionnaire to a young adult population.
Narrative synthesis
Narrative synthesis generated three overarching themes: psychological factors, health factors, and multifactorial aspects (see Table 2 for themes and subtheme descriptions). Overall, patients with asthma demonstrated impaired QoL, which was further decreased by psychological factors (e.g. anxiety, depression, emotion regulation, illness perceptions), health risk factors (such as an increased BMI), and the presence of a co-existing mental health or physical condition (such as rhinitis, cardiovascular disease, diabetes, etc.). Having more than one co-existing condition or psychological factor impacted overall QoL even more substantially. Results for each of the aspects found are presented below.
Psychological factors
Within this first theme, four subthemes were generated. These comprised ‘anxiety and depression’, ‘other mental health conditions’, ‘emotional regulation’, and ‘illness representations’.
Anxiety and depression were notably the most commonly considered factors (n = 30). A high prevalence of people with asthma showed symptoms of or clinical diagnoses of anxiety or depression, which appeared to play a key role in understanding the relationship between asthma and QoL. Overall, having a diagnosis of anxiety or depression was associated with poorer QoL across all dimensions (e.g. activity limitation, physical or mental wellbeing, social or role functioning, etc.), as well as health perceptions.24,36,46,50,54 In particular, one study (of undergraduate students aged 18–25 years, with childhood-onset asthma) found that anxiety was significantly associated with asthma QoL, as was the interaction between anxiety and depression,32 while others found that generally anxiety and depression both predicted worse QoL independently (refs 12,29,33,38,42,44,56,60). One study found that the average asthma-related QoL scores for people with asthma and depression were 1.4 times lower compared to people with asthma and no depression.33 Having current depression or anxiety was associated with worse QoL than was having a lifetime diagnosis; this was in turn was greater than having no depression or anxiety.45 Having a history of major depression was also significantly associated with worse physical and mental functioning, compared to those with asthma and no depression.38 There was considerable variability across variance explained, with depression found to account for between 3%40 and 56%30 of the variance in QoL, whereas anxiety was found to account for between 2%40 and 68%.21
In contrast, one study found that having either a depressive or an anxiety disorder significantly impacted asthma QoL but having both was not significantly different than only having one,40 which is dissonant with other studies. Another study of 90 people with difficult asthma found that having anxiety or depression had no significant effect on QoL.48 In addition, although depression was associated with poorer QoL, it did not inflate the relationship between asthma severity and QoL.29 All other studies were significant but showed only small-to-moderate effect sizes. Having a full clinical diagnosis of anxiety or depression was not significantly worse (in terms of QoL) than having only some symptoms of anxiety and depression.
Studies also considered the impact of anxiety and depression on specific subdomains of QoL and asthma-specific QoL. Having anxiety was not associated with physical functioning, mental health or health perception,38 or the physical component of QoL.20 Depression, however, was associated with significantly poorer QoL on physical dimensions and activity limitation,20,21,23,30,38,45,53,55,58 although one study found significant results only for participants with uncontrolled asthma.22 In relation to asthma-specific QoL, depression and anxiety were significantly associated with decreased asthma-specific QoL.17,21,23,27,28,32,33,36,37,40,50,54,55,58,61
Nine studies looked at other mental health conditions, such as panic disorder with or without agoraphobia,24,38,44,57 personality disorders,31 alexithymia,23 somatization,38 mood disorders,12,40,57 schizophrenia, eating disorders, substance use disorders,38 and general occurrence of any psychiatric disorder.12,17 The results in this subtheme were mixed, but overall they suggest that the presence of an additional mental health condition is significantly associated with a decrease in QoL in patients with asthma.12,17 Panic disorder was also shown to be both significantly24 and non-significantly57 associated with poorer mental and physical components of QoL. Alexithymia in people with asthma was not associated with poorer QoL.23 Having asthma and a personality disorder was associated with lower general QoL,31 as well as lower scores for physical health, vitality, pain, general health, social function, mental health, and emotional role (physical function was not significant). This association was not found for people without asthma, suggesting that it is the combination of conditions (asthma and co-existing mental health conditions) that may lead to the negative impact on QoL.31
The emotion regulation subtheme included studies that explored the relationship between emotional states, negative affect (not related to anxiety, depression, or other mental health conditions), or coping and QoL in people with asthma. QoL in asthma was found to be influenced by affect and a predisposition to negative states, as found by four studies.28,39,41,51 For instance, a model of age, gender, negative affect, and medical problems accounted for 20% of symptoms and 23% of activity limitation.39 This was supported by findings that negative mood is associated with poor scores on both the mental and physical components of the Asthma Quality of Life Questionnaires (AQLQ),28 as well as a positive correlation between active coping and asthma QoL.51 Despite heterogeneity, the impaired QoL was associated with impulsive-careless coping41 and avoidant coping.51 Overall, the presence of psychological distress seemed to affect people with asthma more than people without asthma in terms of QoL.
Illness-related cognitions are people’s patterns of beliefs about the characteristics of their conditions, which in turn influence their appraisal of severity and can determine future behaviours.63 A number of illness-related cognitions and perceptions significantly predicted QoL in seven studies.26,34,37,42,43,51,60 For instance, asthma self-efficacy42 was positively associated with QoL. However, decreased QoL was significantly predicted by a series of varied illness perceptions: subjective illness severity, uncertainty in illness, illness intrusiveness,43 perceived disability,60 health beliefs and attitudes,34 perceived severity,34 level of confidence or self-efficacy in managing asthma,51 satisfaction with illness,51 anxiety sensitivity for physical concerns,39 and satisfaction with life.37 In addition, a model of subjective and objective illness severity accounted for 24% of the variance in QoL, further supporting the effect of illness perceptions on QoL.34
Physical health factors
Two subthemes were generated in the physical health factors theme: additional physical conditions and BMI.
Ten papers examined additional physical conditions in relation to QoL in asthma;25,27,34,39,46,47,48,49,52,53 most only referred to ‘comorbidity’ or ‘medical problems’ as a measure of frequency of additional conditions.34,36,39 Some studies looked at both general and individual co-existing conditions25,48,52 and others counted chronic conditions but did not include them in further analyses.33,36,56,59 Of the ones that did explore individual conditions, the highest impact seemed to be provoked by musculoskeletal conditions.25 Similarly, statistically and clinically significant decreases in activity levels were also found for people with asthma and multimorbid conditions.52 Other conditions investigated included respiratory conditions,47 diabetes,25,48 obesity,48 hypertension,25,39 gastro-oesophageal reflux disorder,48 rhinitis,48,49 vocal cord dysfunction,48 sleep apnoea,48 musculoskeletal disorders,25,39 arthritis,39,52 heart disease,25 stroke,39,52 cancer,39,52 osteoporosis,52 dysfunctional breathing,48 headaches,39 and allergic status.27,39 The consensus was that having an additional physical condition significantly decreased QoL in asthma, the effect being amplified with the addition of further conditions.
Eleven papers exploring BMI found that it consistently influenced QoL for people with asthma both directly as a multimorbid factor and indirectly by increasing the chance of additional conditions and activity limitation.25,26,28,29,35,42,44,45,48,56,59 In particular, one study found that generic health status decreased for overweight and obese patients with asthma. People with asthma with obesity had on average 5.05 more restricted activity days than people without obesity or without asthma.35 Other studies found that increased BMI was an independent factor in predicting poorer QoL48 and that QoL was two times worse in overweight and three times worse in obese people with asthma.59 In contrast, one study found that overweight BMI made no difference; however, being obese did.27 Almost ½ of obese patients and 25% overweight patients had problems with mobility, pain, discomfort, self-care, and usual activities (compared to <15% people with asthma of normal weight).26
Multifactorial aspects
Seven studies included statistical analyses to explore potential mechanisms for the relationship between asthma QoL and additional physical conditions, BMI, and psychological factors.17,35,42,45,50,56,59 Results from studies in this group are complex, indicating that people with asthma are at a higher risk of adverse outcomes (such as exacerbated symptoms or decreased QoL) if they also have a high BMI and depression.35,42,56,59 People with current depression and asthma are more likely to be obese and 3.9 times more likely to report fair or poor general health.45 A few of these studies have explored the relationship between these factors further. For example, people with asthma and obesity were more likely to have additional physical comorbidities and poorer QoL.59 Significant increases in major depression were associated with dyspnoea,50 and depression and perceived control of asthma significantly mediated between BMI and QoL.35 Higher BMI has also been associated with worse asthma-specific self-efficacy, which was in turn associated with decreased QoL.42
Discussion
The aim of the present review was to synthesise the literature exploring health and psychological factors that influence QoL in adults with asthma. Previous evidence shows that QoL is generally lower in people with asthma and compounded by poor asthma control and severity.13 The narrative synthesis in the present study builds on this by identifying three themes, encompassing a number of factors that substantially explain further impairment in QoL for people with asthma. These were not limited to individual components but also combinations of co-existing conditions, risk factors, and health and psychological factors, which consistently showed a negative impact on QoL.
Anxiety and depression were the most commonly reported psychological factors associated with impaired QoL, but effects were also found for other mental health conditions, illness representations, and emotion regulation. These results are generally consistent with previous research showing not only that among people with asthma there are more people with depression than without8 but also with an increase in depression, the risk of asthma increased.64 Although the relationship between anxiety and depression and asthma-specific QoL were not further considered in the primary sources, they point towards either a link with activity limitation or a cumulative impact of the interaction between these psychological factors, which in turn affect the QoL of people with asthma. In addition, it is argued that people with asthma use more emotion-focused, and generally maladaptive, coping strategies, such as avoidance.65 Despite this, psychotherapy, such as cognitive-behavioural therapy and counselling has had limited effectiveness in improving asthma outcomes.66
Physical health factors, such as high BMI and co-occurring health conditions, were extremely common in people with asthma, consistent with existing literature.16 This affects QoL both directly and indirectly, affecting self-management and illness perceptions. As such, non-pharmacological treatments such as lifestyle change and activity promotion could prove effective. For instance, a higher proportion of people with asthma seem to have overweight or obese BMI67 and weight loss intervention studies have been associated with improvements in asthma symptoms.68
One of the fundamental components of reduced QoL is activity limitation, which is especially relevant to people with asthma, with or without additional conditions or psychological risk factors. This has been widely acknowledged by previous research, to the extent that it has been included as one of the components of asthma-related QoL measures, such as the AQLQ.69 Furthermore, it is not surprising that decreased QoL in adults with asthma is associated with depression or high BMI, both of which have been consistently associated with activity limitation (e.g. refs 70,71). In addition, depression was found to affect QoL on the physical components as well as the mental ones, which has interesting implications for future research and clinical practice.
It is important to note the high prevalence of anxiety, depression, and chronic conditions, despite frequent exclusion of comorbid psychiatric conditions. This was found throughout the included papers and is consistent with previous research (e.g. refs 8,16). This does not only mean that psychological and health factors significantly add to the burden of living with asthma but also that the occurrence of psychological dysfunction and health risk factors seem to be common in people with asthma. In addition, the complex nature of patients with chronic diseases such as asthma, with factors interacting, adds to the negative experience of living with asthma. Results are similar to previous meta-analyses and reviews,8,72 pointing towards conclusive evidence that additional factors (physical or psychological) decrease QoL and functionality in asthma. Finally, these effects were consistent, regardless of the measure of QoL used (asthma specific, health related, or general). This suggests that the identified factors may affect people with asthma more than people without asthma or that the cumulative impact of comorbidities is greater than arithmetically assumed.
The quality of the present review needs to be discussed in relation to the methodology and robustness of the synthesis, determined by the quantity and quality of individual studies included.73 The quality assessment identified that most studies were of a reasonable quality overall, although all papers had one or two elements that were of a slightly lower quality (this included aspects such as recruitment from only one hospital reducing generalizability or self-report vs objective measurement of weight for BMI calculations). However, this was not problematic for the purposes of this review as the focus was to identify potential factors considered in research rather than classify the methodological quality used to measure their impact on QoL. In addition, the search terms in this review could have limited the number and kind of studies included. For instance, not every potential comorbid condition was listed. This could be a focus for future research. Socio-demographic factors were not included, which can be considered a limitation; however, the breadth of the area was deemed too much for the scope of the present review and could also be the focus of future research. The majority of included studies were observational and as such could not be used to determine causal mechanisms. However, the aim of this review was only to identify potential factors involved in decreased QoL in asthma, rather than build a causal model. Similarly, the impact of individual factors was not measured and could be explored in future research.
A strength of the present review is that it uses a novel approach to QoL in asthma, by systematically taking into account additional aspects that influence the experience of living with asthma and impact QoL. Results suggest both a direct association of the identified aspects, as well as indirectly through interactions with other aspects of living with asthma, such as overarching illness perceptions and activity limitation. The present review emphasizes some interesting and novel findings for asthma and QoL research. Three main implications for future research and practice are proposed. First, for future research, the findings of this review should be used to further explore and understand the factors impacting QoL in people with asthma. It is crucial to explore the needs and experience of patients with complex medical problems, in order to unpick the different factors impacting on QoL. Second, the results are relevant for practitioners, particularly in primary care, as they draw attention to the prevalence of various physical and mental health factors that can interact and affect asthma outcomes. This could influence training or guidelines on potential factors to consider during appointments and consultations. Finally, most current non-pharmacological interventions for patients with chronic conditions tend to overlook the complex needs of patients in a multimorbidity context. As such, it is suggested that future intervention development should use a personalized, tailored approach that aims to address the needs of patients with complex medical problems in the wider context of their experience of living with asthma.
This review demonstrates that the themes and factors identified through inductive narrative synthesis illustrate that QoL in asthma cannot be determined in a simplistic way. The findings suggest a complex experience in living with asthma, one that has a stronger impact on QoL than the sum its of parts. People with asthma and their QoL cannot be viewed separately from the psychological and other health elements that they experience. Future research is encouraged to take a function-oriented approach to QoL in asthma, including management of multimorbid conditions when planning studies; clinical practice should also acknowledge the additional and complex needs of people with asthma by offering relevant, person-based tailored interventions.
Method
Search strategy
The initial search was carried out in April 2017 and was updated in January 2019. Databases searched included MEDLINE, EMBASE, PsycINFO, the Cochrane Library, and Web of Science. Search terms used comprised a combination of the following key terms: asthma (MESH term), psychological/psychosocial and factor/determinant/predictor, comorbid, multimorbid, anxiety, depression, illness perception, illness cognition, illness representation, locus of control, self-efficacy, risk factor, quality of life, health-related quality of life, wellbeing, distress, health status, burden. In addition, a hand search of all the references of included papers was performed as well as a grey literature search on Google Scholar.
Study selection
Studies were included if they investigated psychological or physical health factors and included QoL in adults with asthma as primary or secondary outcome. Psychological factors were considered any modifiable factors, including thoughts, beliefs, attitudes, or emotions of people with asthma, as well as the presence of any co-occurring mental health condition. Physical health factors were defined as any physical comorbid or multimorbid condition or risk factor. These were chosen to allow as much inclusivity as possible and to reflect the exploratory nature of this review. Intervention studies were excluded, as they rarely considered the impact of health or psychological factors on QoL but rather investigated how interventions improved asthma outcomes. Studies were excluded if they were conference abstracts, reviews, or not primary research or the full text not in English, German, or Spanish language.
Data extraction and quality appraisal
Data extracted comprised authors, year of publication, study sample, predictors, QoL measurement (outcome), and findings. The AXIS tool74 was used to assess the quality of included papers. This contains questions on study design, sample size justification, target population, sampling frame, sample selection, measurement validity and reliability, and overall methods and does not offer a numerical scale. No papers were excluded or weighted based on the quality assessment.
Data synthesis
Owing to heterogeneity of QoL measures and the range of variables used in the included studies, narrative synthesis was used to describe and group similar findings, explore patterns identified in the literature, and develop a narrative account of the results.73 This is an approach to systematic reviews involving the synthesis of findings from multiple sources and relies primarily on word and text to summarise the findings.
All data generated or analysed during this study are included in this published article.
Reporting summary
Further information on research design is available in the Nature Research Reporting Summary linked to this article.
References
World Health Organization. Chronic Respiratory Diseases - Asthma http://www.who.int/respiratory/asthma/en/ (2018).
ASTHMA UK. Asthma Facts and Statistics https://www.asthma.org.uk/about/media/facts-and-statistics/ (2018).
Pickles, K. et al. “This illness diminishes me. What it does is like theft”: a qualitative meta‐synthesis of people’s experiences of living with asthma. Health Expectations 21, 23–40 (2018).
Goeman, D. P. & Douglass, J. A. Understanding asthma in older Australians: a qualitative approach. Med. J. Aust. 183, S26–S27 (2005).
Juniper, E. F. How important is quality of life in pediatric asthma? Pediatr. Pulmonol. 24, 17–21 (1997).
Accordini, S. et al. The socio‐economic burden of asthma is substantial in Europe. Allergy 63, 116–124 (2008).
Goeman, D. P. et al. Patients’ views of the burden of asthma: a qualitative study. Med. J. Aust. 177, 295–299 (2002).
Thomas, M., Bruton, A., Moffat, M. & Cleland, J. Asthma and psychological dysfunction. Prim. Care Respir. J. 20, 250–256 (2011).
Goodwin, R. D., Fergusson, D. M. & Horwood, L. J. Asthma and depressive and anxiety disorders among young persons in the community. Psychol. Med. 34, 1465–1474 (2004).
Jenkins, R. et al. The national psychiatric morbidity surveys of Great Britain–strategy and methods. Psychol. Med. 27, 765–774 (1997).
Miles, J., Garden, G., Tunnicliffe, W., Cayton, R. & Ayres, J. Psychological morbidity and coping skills in patients with brittle and non‐brittle asthma: a case‐control study. Clin. Exp. Allergy 27, 1151–1159 (1997).
Lavoie, K. L. et al. Are psychiatric disorders associated with worse asthma control and quality of life in asthma patients? Respir. Med. 99, 1249–1257 (2005).
Juniper, E. F., Guyatt, G. H., Ferrie, P. J. & Griffith, L. E. Measuring quality of life in asthma. Am. Rev. Respir. Dis. 147, 832–832 (1993).
Edwards, M. R. et al. Addressing unmet needs in understanding asthma mechanisms. Eur. Respir. J. 49, 1602448 (2017).
Masefield, S. et al. The future of asthma research and development: a roadmap from the European Asthma Research and Innovation Partnership (EARIP). Eur. Respir. J. 49 (2017).
Su, X. et al. Prevalence of comorbidities in asthma and nonasthma patients: a meta-analysis. Medicine 95, e3459 (2016).
Adams, R. J. et al. Psychological factors and asthma quality of life: a population based study. Thorax 59, 930–935 (2004).
Leynaert, B., Neukirch, C., Liard, R., Bousquet, J. & Neukirch, F. Quality of life in allergic rhinitis and asthma: a population-based study of young adults. Am. J. Respir. Crit. Care Med. 162, 1391–1396 (2000).
Moher, D., Liberati, A., Tetzlaff, J., Altman, D. G. & Group, P. Preferred reporting items for systematic reviews and meta-analyses: the PRISMA statement. PLoS Med. 6, e1000097 (2009).
Bohmer, M. M. et al. Factors associated with generic health-related quality of life in adult asthma patients in Germany: cross-sectional study. J. Asthma 54, 325–334 (2017).
Oğuztürk, Ö. et al. Psychological status and quality of life in elderly patients with asthma. Psychosomatics 46, 41–46 (2005).
Lomper, K., Chudiak, A., Uchmanowicz, I., Rosinczuk, J. & Jankowska-Polanska, B. Effects of depression and anxiety on asthma-related quality of life. Pneumonol. Alergol. Pol. 84, 212–221 (2016).
Vazquez, I. et al. The role of alexithymia in quality of life and health care use in asthma. J. Asthma 47, 797–804 (2010).
Sández, E. et al. Depression, panic-fear, and quality of life in near-fatal asthma patients. J. Clin. Psychol. Med. Settings 12, 175–184 (2005).
Wijnhoven, H. A., Kriegsman, D. M., Hesselink, A. E., de Haan, M. & Schellevis, F. G. The influence of co-morbidity on health-related quality of life in asthma and COPD patients. Respir. Med. 97, 468–475 (2003).
Gonzalez-Barcala, F.-J., de la Fuente-Cid, R., Tafalla, M., Nuevo, J. & Caamano-Isorna, F. Factors associated with health-related quality of life in adults with asthma. A cross-sectional study. Multidiscip. Respir. Med. 7, 32 (2012).
Coban, H. & Aydemir, Y. The relationship between allergy and asthma control, quality of life, and emotional status in patients with asthma: a cross-sectional study. Allergy Asthma Clin. Immunol. 10, 67 (2014).
Ekici, A., Ekici, M., Kara, T., Keles, H. & Kocyigit, P. Negative mood and quality of life in patients with asthma. Qual. Life Res. 15, 49–56 (2006).
Al-Kalemji, A. et al. Factors influencing quality of life in asthmatics - a case-control study. Clin. Respir. J. 7, 288–296 (2013).
Kullowatz, A., Kanniess, F., Dahme, B., Magnussen, H. & Ritz, T. Association of depression and anxiety with health care use and quality of life in asthma patients. Respir. Med. 101, 638–644 (2007).
Yilmaz, A., Cumurcu, B. E., Etikan, I., Hasbek, E. & Doruk, S. The effect of personality disorders on asthma severity and quality of life. Iran. J. Allergy Asthma Immunol. 13, 47–54 (2014).
Hommel, K. A., Chaney, J. M., Wagner, J. L. & McLaughlin, M. S. Asthma-specific quality of life in older adolescents and young adults with long-standing asthma: the role of anxiety and depression. J. Clin. Psychol. Med. Settings 9, 185–192 (2002).
Krauskopf, K. A. et al. Depressive symptoms, low adherence, and poor asthma outcomes in the elderly. J. Asthma 50, 260–266 (2013).
Erickson, S. R., Christian, R. D. Jr, Kirking, D. M. & Halman, L. J. Relationship between patient and disease characteristics, and health-related quality of life in adults with asthma. Respir. Med. 96, 450–460 (2002).
Vortmann, M. & Eisner, M. D. BMI and health status among adults with asthma. Obesity (Silver Spring) 16, 146–152 (2008).
Mancuso, C. A., Peterson, M. G. E. & Charlson, M. E. Effects of depressive symptoms on health-related quality of life in asthma patients. J. Gen. Intern. Med. 15, 301–310 (2000).
Miedinger, D., Lavoie, K. L., L’Archeveque, J., Ghezzo, H. & Malo, J.-L. Identification of clinically significant psychological distress and psychiatric morbidity by examining quality of life in subjects with occupational asthma. Health Qua. Life Outcomes 9, 76 (2011).
Afari, N., Schmaling, K. B., Barnhart, S. & Buchwald, D. Psychiatric comorbidity and functional status in adult patients with asthma. J. Clin. Psychol. Med. Settings 8, 245–252 (2001).
Avallone, K. M., McLeish, A. C., Luberto, C. M. & Bernstein, J. A. Anxiety sensitivity, asthma control, and quality of life in adults with asthma. J. Asthma 49, 57–62 (2012).
Lavoie, K. L. et al. What is worse for asthma control and quality of life - depressive disorders, anxiety disorders, or both? Chest 130, 1039–1047 (2006).
McCormick, S. P. et al. Coping and social problem solving correlates of asthma control and quality of life. Chron. Respir. Dis. 11, 15–21 (2014).
Lavoie, K. L. et al. Association of asthma self-efficacy to asthma control and quality of life. Ann. Behav. Med. 36, 100–106 (2008).
Hullmann, S. E., Eddington, A. R., Molzon, E. S. & Mullins, L. L. Illness appraisals and health-related quality of life in adolescents and young adults with allergies and asthma. Int. J. Adolesc. Med. Health 25, 31–38 (2013).
Favreau, H., Bacon, S. L., Labrecque, M. & Lavoie, K. L. Prospective impact of panic disorder and panic-anxiety on asthma control, health service use, and quality of life in adult patients with asthma over a 4-year follow-up. Psychosom. Med. 76, 147–155 (2014).
Strine, T. W., Mokdad, A. H., Balluz, L. S., Berry, J. T. & Gonzalez, O. Impact of depression and anxiety on quality of life, health behaviors, and asthma control among adults in the United States with asthma, 2006. J. Asthma 45, 123–133 (2008).
Pate, C. A., Zahran, H. S. & Bailey, C. M. Impaired health-related quality of life and related risk factors among US adults with asthma. J. Asthma 56, 431–439 (2018).
Urbstonaitis, R., Deshpande, M. & Arnoldi, J. Asthma and health related quality of life in late midlife adults. Res. Soc. Adm. Pharm. 15, 61–69 (2019).
Tay, T. R. et al. Comorbidities in difficult asthma are independent risk factors for frequent exacerbations, poor control and diminished quality of life. Respirology 21, 1384–1390 (2016).
Powell, H. et al. Rhinitis in pregnant women with asthma is associated with poorer asthma control and quality of life. J. Asthma 52, 1023–1030 (2015).
Goldney, R. D., Ruffin, R., Fisher, L. J. & Wilson, D. H. Asthma symptoms associated with depression and lower quality of life: a population survey. Med. J. Aust. 178, 437–441 (2003).
Adams, R. J., Wilson, D., Smith, B. J. & Ruffin, R. E. Impact of coping and socioeconomic factors on quality of life in adults with asthma. Respirology 9, 87–95 (2004).
Adams, R. J. et al. Coexistent chronic conditions and asthma quality of life: a population-based study. Chest J. 129, 285–291 (2006).
Deshmukh, V. M., Toelle, B. G., Usherwood, T., O’Grady, B. & Jenkins, C. R. The association of comorbid anxiety and depression with asthma-related quality of life and symptom perception in adults. Respirology 13, 695–702 (2008).
Oga, T. et al. Analysis of longitudinal changes in the psychological status of patients with asthma. Respir. Med. 101, 2133–2138 (2007).
Nishimura, K., Hajiro, T., Oga, T., Tsukino, M. & Ikeda, A. Health related quality of life in stable asthma: what are remaining quality of life problems in patients with well-controlled asthma? J. Asthma 41, 57–65 (2004).
Choi, G.-S. et al. Prevalence and risk factors for depression in korean adult patients with asthma: is there a difference between elderly and non-elderly patients? J. Korean Med. Sci. 29, 1626–1631 (2014).
Faye, A. D. et al. Do panic symptoms affect the quality of life and add to the disability in patients with bronchial asthma? Psychiatry J. 2015, 608351–608351 (2015).
Kolawole, M. S. et al. Health related quality of life and psychological variables among a sample of asthmatics in Ile-Ife South-Western Nigeria. Libyan J. Med. 6, 1–5 (2011).
Maalej, S. et al. Association of obesity with asthma severity, control and quality of life. Tanaffos 11, 38 (2012).
Adeyeye, O. O., Adewumi, T. A. & Adewuya, A. O. Effect of psychological and other factors on quality of life amongst asthma outpatients in Lagos, Nigeria. Respir. Med. 122, 67–70 (2017).
Deshmukh, V. M., Toelle, B. G., Usherwood, T., O’grady, B. & Jenkins, C. R. The association of comorbid anxiety and depression with asthma‐related quality of life and symptom perception in adults. Respirology 13, 695–702 (2008).
Al-kalemji, A. et al. Factors influencing quality of life in asthmatics–a case-control study. Clin. Respir. J. 7, 288–296 (2013).
Petrie, K. & Weinman, J. Why illness perceptions matter. Clin. Med. 6, 536–539 (2006).
Gerald, J. K. & Moreno, F. A. Asthma and depression: it’s complicated. J. Allergy Clin. Immunol. Pract. 4, 74–75 (2016).
Barton, C., Clarke, D., Sulaiman, N. & Abramson, M. Coping as a mediator of psychosocial impediments to optimal management and control of asthma. Respir. Med. 97, 747–761 (2003).
Yorke, J., Fleming, S., Shuldham, C., Rao, H. & Smith, H. Nonpharmacological interventions aimed at modifying health and behavioural outcomes for adults with asthma: a critical review. Clin. Exp. Allergy 45, 1750–1764 (2015).
Lavoie, K. L., Bacon, S. L., Labrecque, M., Cartier, A. & Ditto, B. Higher BMI is associated with worse asthma control and quality of life but not asthma severity. Respir. Med. 100, 648–657 (2006).
Pakhale, S., Baron, J., Dent, R., Vandemheen, K. & Aaron, S. D. Effects of weight loss on airway responsiveness in obese adults with asthma: does weight loss lead to reversibility of asthma? Chest 147, 1582–1590 (2015).
Juniper, E., Guyatt, G., Cox, F., Ferrie, P. & King, D. Development and validation of the mini asthma quality of life questionnaire. Eur. Respir. J. 14, 32–38 (1999).
Breslin, F. C., Gnam, W., Franche, R.-L., Mustard, C. & Lin, E. Depression and activity limitations: examining gender differences in the general population. Soc. Psychiatry Psychiatr. Epidemiol. 41, 648–655 (2006).
Hassan, M., Joshi, A., Madhavan, S. & Amonkar, M. Obesity and health-related quality of life: a cross-sectional analysis of the US population. Int. J. Obes. 27, 1227–1232 (2003).
Fortin, M. et al. Multimorbidity and quality of life in primary care: a systematic review. Health Qual. Life Outcomes 2, 51 (2004).
Popay, J. et al. Guidance on the Conduct of Narrative Synthesis in Systematic Reviews. A Product from the ESRC Methods Program. Version 1 (Lancaster University, 2006).
Downes, M. J., Brennan, M. L., Williams, H. C. & Dean, R. S. Development of a critical appraisal tool to assess the quality of cross-sectional studies (AXIS). BMJ Open 6, e011458 (2016).
Author information
Authors and Affiliations
Contributions
S.S.—conception of the review, synthesis, wrote the first draft, commented on drafts. B.A. and S.K.—conception of the review and day-to-day conduct of the review, commented on drafts, updated the review, revised the paper. M.T.—conception of the review, commented on drafts. L.Y.—conception of the review, commented on drafts. All authors read and approved the final version of the manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing interests.
Additional information
Publisher’s note Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
Supplementary information
Rights and permissions
Open Access This article is licensed under a Creative Commons Attribution 4.0 International License, which permits use, sharing, adaptation, distribution and reproduction in any medium or format, as long as you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The images or other third party material in this article are included in the article’s Creative Commons license, unless indicated otherwise in a credit line to the material. If material is not included in the article’s Creative Commons license and your intended use is not permitted by statutory regulation or exceeds the permitted use, you will need to obtain permission directly from the copyright holder. To view a copy of this license, visit http://creativecommons.org/licenses/by/4.0/.
About this article
Cite this article
Stanescu, S., Kirby, S.E., Thomas, M. et al. A systematic review of psychological, physical health factors, and quality of life in adult asthma. npj Prim. Care Respir. Med. 29, 37 (2019). https://doi.org/10.1038/s41533-019-0149-3
Received:
Accepted:
Published:
DOI: https://doi.org/10.1038/s41533-019-0149-3
This article is cited by
-
Piloting co-developed behaviour change interventions to reduce exposure to air pollution and improve self-reported asthma-related health
Journal of Exposure Science & Environmental Epidemiology (2024)
-
A Systematic Review of School Transition Interventions to Improve Mental Health and Wellbeing Outcomes in Children and Young People
School Mental Health (2023)
-
Two meta-analyses of the association between atopic diseases and core symptoms of attention deficit hyperactivity disorder
Scientific Reports (2022)
-
Asthma and early smoking associated with high risk of panic disorder in adolescents and young adults
Social Psychiatry and Psychiatric Epidemiology (2022)
-
Health-Related Disparities in the Metropolitan Region Ruhr: Large-Scale Spatial Model of Local Asthma Prevalence, Accessibility of Health Facilities, and Socioeconomic and Environmental Factors
PFG – Journal of Photogrammetry, Remote Sensing and Geoinformation Science (2022)