Abstract
Our study aimed to explore changes in health-related quality of life (HRQoL) during blood pressure control and blood lipid-lowering therapies. We conducted a 2 × 2 factorial-designed randomized controlled trial in 180 clinical centers in China. At baseline, participants were randomly assigned to an amlodipine + amiloride/hydrochlorothiazide group or an amlodipine + telmisartan group for the blood pressure control treatment and to a statin group or a routine intervention group for the blood lipid-lowering treatment. The allocation ratio was 1:1 for both treatments. Follow-up lasted for 4 years. HRQoL was assessed using the EuroQol five dimensions three levels (EQ-5D-3L) questionnaire every year. Of 13,542 hypertensive patients enrolled in the clinical trial, 9885 were eligible for the analysis. The problems for all dimensions of the EQ-5D-3L descriptive system were slight at baseline and were well preserved in the follow-up period. The EuroQol visual analog scale (EQ VAS) score and the EQ-5D-3L index improved over time (Ptrend < 0.001), with improvements similar among interventions but different between patients who reached the treatment targets or not. Decreases in systolic/diastolic blood pressure and low-density lipoprotein cholesterol and increases in high-density lipoprotein cholesterol were independently correlated with increases in the EQ VAS score and the EQ-5D-3L index. In conclusion, HRQoL is associated with blood pressure/lipid levels but not with specific antihypertensive or lipid-lowering interventions. Blood pressure control and blood lipid-lowering therapies should not be denied to Chinese patients in consideration of their negative effects on quality of life.
Similar content being viewed by others
Introduction
Hypertension and hyperlipidemia are important risk factors and leading causes of cardiovascular diseases (CVDs) worldwide [1]. They are also growing threats to public health in China [2]. The prevalence of both hypertension and hyperlipidemia in China has increased rapidly in the past few decades [3,4,5,6,7]. As estimated by the Global Burden of Disease study, there were 2.04 million deaths caused by hypertension and 0.28 million deaths caused by hyperlipidemia in China in 2010, accounting for 28.0% of the total national deaths [8, 9]. The corresponding disability-adjusted life years caused by hypertension and hyperlipidemia were 37.94 million and 5.91 million person-years, respectively, leading to a high disease burden and a low quality of life among the Chinese population, which necessitates more attention [8, 9].
Blood pressure (BP) control and blood lipid-lowering therapies are necessary to lessen the prevalence and reduce the disease burden. However, the impact of hypertension or hyperlipidemia treatments on patients’ quality of life in China remains unclear. Several BP-lowering studies have reported changes in quality of life through medical treatments or lifestyle interventions [10,11,12,13,14,15]. To date, no data are available on the health-related quality of life (HRQoL) [16] during antihypertensive therapies in Chinese participants. Neither has the joint effect of BP control in combination with blood lipid-lowering therapies on HRQoL been studied. Hence, we conducted a 2 × 2 factorial-designed study among a Chinese hypertensive population to compare HRQoL between two BP control therapies (amlodipine + amiloride/hydrochlorothiazide vs. amlodipine + telmisartan) and two blood lipid-lowering therapies (statin vs. standard management). The aim of our study was to answer the following three questions: (1) Are there any changes in HRQoL over time during the study intervention? (2) Are there any differences in HRQoL between the two antihypertensive treatments and between the two lipid-lowering treatments? (3) Are there any differences in HRQoL between patients who have reached the treatment targets (for either BP or blood lipid) and patients who have not reached the treatment targets?
Since the BP levels were notably decreased in the study period and balanced among groups (Supplementary Table 1), we hypothesized that participants’ HRQoL might improve over time, be similar among interventions, but be different among patients who reached the BP/lipid targets or not [17]. The potential improvements in HRQoL might be mainly attributed to the changes in the dimensions of pain/discomfort and anxiety/depression, rather than the dimensions of mobility, self-care, and usual activities, because the BP control and blood lipid-lowering treatments were mainly aimed to provide comfort and cure [18].
Methods
Study design and participants
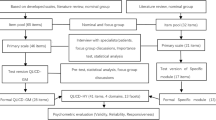
This is a substudy of the Chinese Hypertension Intervention Efficacy (CHIEF) randomized controlled trial, which enrolled 13,542 hypertensive patients from 180 clinical centers in China from October 2007 to October 2008 [19]. The rationale and design of the CHIEF study have been presented elsewhere [19]. In brief, the CHIEF study is a large-scale, multicenter clinical trial that involves two treatments (antihypertensive therapy and lipid-lowering therapy) in a 2 × 2 factorial design to compare the effects of different therapies on the incidence of major adverse cardiovascular events, represented as a composite of nonfatal stroke, nonfatal myocardial infarction, and cardiovascular deaths. Both treatments were prospective, randomized, open-labeled, and blinded-endpoint evaluated, with a 1:1 allocation ratio. For the BP control treatment, all eligible participants were randomly assigned to an amlodipine + amiloride/hydrochlorothiazide group (Group A) or an amlodipine + telmisartan group (Group T). For the blood lipid-lowering treatment, participants with serum total cholesterol levels ranging from 4.0 to 6.1 mmol/L were further randomized to a statin group (Group S) or a routine intervention group (Group R). The flow chart of the CHIEF study is illustrated in Fig. 1.
The Flow Chart of the CHIEF Study. Group A: amlodipine 2.5 mg + amiloride/hydrochlorothiazide 1.25/12.5 mg per day. Group T: amlodipine 2.5 mg + telmisartan 40 mg per day. Group S: oral simvastatin 10 mg per day. Group R: routine intervention managed at the investigators’ discretion. TC, total cholesterol; HRQoL, health-related quality of life; EQ-5D, EuroQol five-dimension questionnaire
Participants were eligible for the CHIEF study if they were 50–79 years of age with at least one CVD risk factor (as listed in Supplementary Method 1) and had a systolic BP between 140 and 179 mmHg and/or a diastolic BP between 90 and 109 mmHg at randomization. Detailed inclusion and exclusion criteria are shown in Supplementary Method 1. In this analysis, we further excluded individuals with missing values in the baseline measurements of HRQoL. The CHIEF study was approved by the ethics committees of all participating centers and was consented to all participants. It is registered with ClinicalTrials.gov, number NCT01011660.
Study intervention and follow-up
The standard procedures of randomization, intervention, follow-up, and measurements of the CHIEF study have been described previously [19]. In brief, participants were allocated to different intervention groups by the minimized randomizing method in the Interactive Web Response System after 2 weeks of discontinuing their previous antihypertensive medications.
During the BP control treatment, participants in Group A received amlodipine 2.5 mg in combination with amiloride/hydrochlorothiazide 1.25/12.5 mg per day. Participants in Group T received amlodipine 2.5 mg plus telmisartan 40 mg per day. The target BP was 130/80 mmHg for diabetes or chronic kidney disease patients and 140/90 mmHg for other participants. If the target BP was not reached at the second week visit, the dose of amiloride/hydrochlorothiazide or telmisartan would be doubled. If the target BP was not reached at the fourth week visit, the dose of amlodipine would be doubled. If patients’ BP was still uncontrolled 2 or 3 months after randomization, other antihypertensive interventions would be added to the groups by the investigators’ determination. After the treatment, we post hoc classified subjects who reached the target BP at both the 12- and 24-month visits into a controlled BP group (Group C) and classified others who did not reach the target BP at either the 12- or 24-month visit into an uncontrolled BP group (Group U).
During the blood lipid-lowering treatment, participants in Group S received oral simvastatin 10 mg per day, while participants in Group R received standard management at the investigators’ discretion. Similarly, we classified subjects with low-density lipoprotein cholesterol (LDL-C) < 2.6 mmol/L at both the 12- and 24-month visits into a controlled lipid group (Group C) and classified others with LDL-C ≥2.6 mmol/L at either the 12- or 24-month visit into an uncontrolled lipid group (Group U) [20].
Follow-up occurred at 2 weeks, 1 month, 2 months, 3 months, and every 3 months thereafter until 4 years after randomization. At every visit, three sitting BP measurements were performed using a standardized mercury manometer with 6-monthly calibration [19]. The average of the second and third measurements was used in the analysis. At the screening visit, baseline demographics and medical histories were recorded through interview-based questionnaires; physical examinations were conducted, and blood samples were taken for the evaluation of CVD risk factors. Serum markers and HRQoL were assessed every year. The follow-up rates of the 12-, 24-, 36-, and 48-month visits were 96.3% (13,036/13,542), 93.6% (12,681/13,542), 85.4% (11,564/13,542), and 74.9% (10,145/13,542), respectively. Owing to the higher loss rates and the greater number of missing values for BP and lipid measurements at the 36- and 48-month visits, we only considered the antihypertensive and lipid-lowering effects at the 12- and 24-month visits to classify subjects as controlled or uncontrolled.
Health-related quality of life
HRQoL was evaluated by the EuroQol five-dimension (EQ-5D) questionnaire, which is a simple and standardized measurement of health status for clinical and economic appraisal [21, 22]. The EQ-5D questionnaire contains the following two parts: the EQ-5D-3L descriptive system for health profiling and the EQ visual analog scale (EQ VAS) for health evaluation.
The EQ-5D-3L descriptive system consists of five dimensions (5D): mobility, self-care, usual activities, pain/discomfort, and anxiety/depression. Each dimension is scaled by three levels (3L): no problems, some problems, and extreme problems. The EQ-5D-3L descriptive system can be transformed into the EQ-5D-3L index, which is a summary value that represents the health status for the general population, with 0 representing death and 1 representing perfect health. We calculated the EQ-5D-3L index according to the Japanese value sets [23], since there is no estimation for the Chinese population yet; Japanese is the most comparable ethnicity with Chinese among the currently available value sets [22].
The EQ VAS score is graded according to the participant’s self-rated health state, with 0 representing the worst imaginable health state and 100 representing the best imaginable health state [22]. We reported the frequencies of some or extreme problems at each level for each dimension in the EQ-5D-3L descriptive system and presented the values of EQ VAS score and EQ-5D-3L index in every study group and at every visit.
Statistical analysis
Statistical analyses were based on the intention-to-treat approach [24]. Baseline characteristics are presented as the mean ± standard deviation for continuous variables and as the frequency (proportion) for categorical variables. Cross-sectional comparisons among groups were made by analysis of variance for continuous variables and Chi-square test for categorical variables. Trends of HRQoL over time were analyzed using analysis of covariance for continuous variables and Mantel-Haenszel Chi-square test for categorical variables. Longitudinal comparisons among groups were made by repeated measures models, regarding group, time, and group by time interaction as fixed effects [25]. To further understand the relationships between BP/lipid levels and HRQoL, we fitted generalized linear models using generalized estimating equations, adjusting for potential confounders of age, sex, body mass index, and CVD risk factors, and addressing for the cluster effect of repeated measures (considered all yearly measures of BP or lipid in the model and explored the associations at the visit level). A two-tailed P-value <0.05 was considered statistically significant. Given the multiplicity of comparisons in some cases, we used the Bonferroni method to correct the significance level as appropriate. To address the missing values of HRQoL during follow-up, multiple imputation with ten replicate sets was performed in the primary analysis [26]. The monotone discriminant function method was used for imputing the EQ-5D-3L descriptive system (no problems or some/extreme problems), and the monotone regression method was used for imputing the EQ VAS score and the EQ-5D-3L index. Missing values were predicted on the basis of all repeated measures taken from the previous visits. At the same time, a complete-case set was used for sensitivity analysis. All analyses were conducted by SAS 9.4 (SAS Institute, Inc., Cary, NC, USA), and all graphs were depicted by GraphPad Prism 5 (GraphPad Software, Inc., California, USA).
Results
The CHIEF study recruited 13,542 hypertensive patients, of whom 9913 had total cholesterol levels between 4.0 and 6.1 mmol/L and were eligible for both BP control and blood lipid-lowering treatments. Among them, 9885 subjects with baseline HRQoL measurements were included in this analysis.
In the BP control treatment, 4954 (50.1%) participants were allocated to Group A, and 4931 (49.9%) were allocated to Group T. In the blood lipid-lowering treatment, individuals were assigned to Groups AS, AR, TS, or TR, with sample sizes of 2482 (25.1%), 2472 (25.0%), 2459 (24.9%), and 2472 (25.0%), respectively. The baseline characteristics of the intervention groups are presented in Table 1. All variables were balanced among four groups.
During follow-up, HRQoL was available in 9442 (95.5%), 8919 (90.2%), 6605 (66.8%), and 4693 (47.5%) subjects at the 12-, 24-, 36-, and 48-month visits, respectively. Detailed follow-up rates in the four intervention groups are displayed in Fig. 1. Supplementary Tables 2 and 3 explore the association between baseline characteristics and the missing status of HRQoL data, which suggested that baseline features had little impact on the missingness of HRQoL. Therefore, we assumed that missing data occurred at random and performed multiple imputation in our primary analysis. Moreover, we conducted sensitivity analysis by the complete-case set and found consistent results.
Health-related quality of life by time
The changes in HRQoL over time are shown in Fig. 2 (primary analysis) and Supplementary Table 4 (sensitivity analysis). Of the five dimensions for health state description, pain/discomfort and anxiety/depression were most serious at baseline and were much lightened during the antihypertensive and lipid-lowering therapies (Ptrend < 0.001). Problems in mobility and usual activities were slight and almost unchanged over time. Self-care difficulty increased from 1.6% to 2.5% throughout the 4-year intervention (Ptrend < 0.001). The EQ VAS score and the EQ-5D-3L index increased significantly in the follow-up period (Ptrend < 0.001), indicating better health status after the study treatments.
Changes of HRQoL in the study population. HRQoL, health-related quality of life; EQ VAS, EuroQol visual analog scale; EQ-5D-3L, EuroQol five-dimension three-level questionnaire. *Ptrend < 0.05. Comparisons among repeated measurements were made by covariance analysis for continuous variables and Mantel-Haenszel Chi-square test for categorical variables
Health-related quality of life among intervention groups
The changes in HRQoL over time in different intervention groups are shown in Fig. 3 (primary analysis) and Supplementary Table 5 (sensitivity analysis). Both the EQ VAS score and the EQ-5D-3L index were comparable in the four groups at every visit. In consideration of repeated measures, we found that the values of EQ VAS score and EQ-5D-3L index increased over time (Ptime < 0.001), and the trends of all intervention groups were similar without factorial interactions.
Changes of HRQoL in different intervention groups*. a Changes in the EQ VAS score in different intervention groups in the factorial treatment. b Changes in the EQ-5D-3L index in different intervention groups in the factorial treatment. Group A: amlodipine 2.5 mg + amiloride/hydrochlorothiazide 1.25/12.5 mg per day. Group T: amlodipine 2.5 mg + telmisartan 40 mg per day. Group S: oral simvastatin 10 mg per day. Group R: routine intervention managed at the investigators’ discretion. HRQoL, health-related quality of life; EQ VAS, EuroQol visual analog scale; EQ-5D-3L, EuroQol five-dimension three-level questionnaire. *Comparisons among four intervention groups were made by analysis of variance for factorial design at every yearly visit and by repeated measures models throughout the entire follow-up period. All time-point P-values were ≥ 0.01, either between the blood pressure control treatments, the blood lipid-lowering treatments, or their interactions. The significance level was corrected by the Bonferroni method. #The upper limit of the 95% confidence interval of the EQ-5D-3L index may exceed 100% because the EQ-5D-3L index obeys a skewed distribution with a median of 100% and an interquartile range of 92 to 100%. More than half of the participants had perfect health at baseline, and we were more concerned about the others whose HRQoL had room for improvement. Thus, we used the mean (confidence interval) rather than the median (interquartile range) to present the results
Health-related quality of life among effect groups
The antihypertensive effects of the two BP control therapies were similar (P = 0.30); 72.0% (3566/4954) of the participants in Group A and 71.0% (3503/4931) of the participants in Group T reached the target BP. The lipid-lowering effect was higher in Group S than in Group R (P < 0.001), as 72.1% (3561/4941) of the subjects using statin had a controlled LDL-C, while only 65.4% (3233/4624) who received standard management had their lipids controlled. In total, 7069 individuals were classified into the controlled BP group and 2203 were classified into the uncontrolled BP group. Meanwhile, 6794 patients were classified into the controlled LDL-C group and 2478 were classified into the uncontrolled LDL-C group. There were still 613 (6.2%) participants who did not enter any group due to loss of follow-up. The baseline characteristics of the effect groups are listed in Supplementary Table 6. Age, sex, body mass index, baseline BP/lipid levels, and several CVD risk factors differed among the groups, suggesting that the effects of BP control and blood lipid-lowering therapies might be related to these factors.
The changes in HRQoL over time in different effect groups are shown in Fig. 4 (primary analysis) and Supplementary Table 7 (sensitivity analysis). The baseline EQ VAS score and EQ-5D-3L index were balanced among groups. From the 1-year visit onward, participants with controlled BP had a significantly higher quality of life than those with uncontrolled BP (Fig. 4a, b). After considering the time effect in a repeated measures model, we found that the EQ VAS score increased with time (Ptime < 0.001) and varied with BP level (PBP < 0.001). For different BP groups, the gains of EQ VAS score by time were also distinct (PBP×time = 0.03) (Fig. 4a). The EQ-5D-3L index showed similar but fewer disparities (Fig. 4b). No evidence of an interaction was detected between target BP and target LDL-C in the groups.
Changes of HRQoL in different effect groups. a Changes in the EQ VAS score in different effect groups in the factorial treatment. b Changes in the EQ-5D-3L index in different effect groups in the factorial treatment. c Changes in the EQ VAS score in different effect groups in the blood pressure control treatment. d Changes in the EQ-5D-3L index in different effect groups in the blood pressure control treatment. e Changes in the EQ VAS score in different effect groups in the blood lipid-lowering treatment. f Changes in the EQ-5D-3L index in different effect groups in the blood lipid-lowering treatment. Group U: uncontrolled BP or LDL-C. Group C: controlled BP or LDL-C. HRQoL, health-related quality of life; EQ VAS, EuroQol visual analog scale; EQ-5D-3L, EuroQol five-dimension three-level questionnaire; BP, blood pressure; LDL-C, low-density lipoprotein cholesterol. *PBP < 0.01; ^PLDL-C < 0.01. Comparisons among four effect groups were made by analysis of variance for factorial design at every yearly visit and by repeated measures models throughout the entire follow-up period. All time-point PBP×LCL-C values were ≥ 0.01, indicating no evidence of an interaction between the target BP and the target LDL-C groups. The significance level was corrected by the Bonferroni method. #The upper limit of the 95% confidence interval of the EQ-5D-3L index may exceed 100% because the EQ-5D-3L index obeys a skewed distribution with a median of 100% and an interquartile range of 92 to 100%. More than half of the participants had perfect health at baseline, and we were more concerned about the others whose HRQoL had room for improvement. Thus, we used the mean (confidence interval) rather than the median (interquartile range) to present the results
The main effects of antihypertension and lipid-lowering on HRQoL are presented from Fig. 4c–f. For the BP control treatment, the EQ VAS score annually increased by 0.98 for Group C (Ptime < 0.001) and 0.79 for Group U (Ptime < 0.001); the group-by-time interaction played a role in deciding the intergroup differences (PBP×time = 0.03). On average, the EQ VAS score was 0.98 higher in participants with controlled BP than in those with uncontrolled BP (PBP < 0.001) (Fig. 4c). The EQ-5D-3L index grew by 0.19% a year (Ptime < 0.001); the average level of EQ-5D-3L index, however, was similar between the controlled and uncontrolled BP groups (Fig. 4d).
For the blood lipid-lowering treatment, the EQ VAS score increased by 0.98 (Ptime < 0.001) and the EQ-5D-3L index increased by 0.30% (Ptime < 0.001) year-on-year for both groups. The difference in HRQoL between the controlled and uncontrolled lipid groups was not significant (Fig. 4e, f).
The associations of BP/lipid levels with HRQoL are displayed in Table 2. With the decreases in systolic/diastolic BP, patients’ quality of life highly improved. A decline of 10 mmHg systolic BP was correlated with a 0.60 increase in the EQ VAS score (P < 0.001) and a 0.26% increase in the EQ-5D-3L index (P < 0.001). A decline of 10 mmHg diastolic BP showed similar but fewer correlations, with 0.31 higher values for the EQ VAS score (P < 0.001) and 0.12% higher values for the EQ-5D-3L index (P = 0.005). Decreases in LDL-C and increases in high-density lipoprotein cholesterol (HDL-C) were also associated with improvements in the EQ VAS score (0.21 for 1 mmol/L lower LDL-C [P = 0.02]; 0.51 for 1 mmol/L higher HDL-C [P = 0.009]) and the EQ-5D-3L index (0.13% for 1 mmol/L lower LDL-C [P = 0.03]; 0.39% for 1 mmol/L higher HDL-C [P = 0.001]). The linear relationship existed when systolic BP was 130 to 180 mmHg, diastolic BP was 80 to 110 mmHg, LDL-C was 2.5 to 4.5 mmol/L, and HDL-C was 1.2 to 2.4 mmol/L. If BP or blood lipids were out of these ranges, we did not have sufficient data to verify the linearity.
Discussion
Our study used the data from the CHIEF randomized controlled trial and detected the following three major findings: (1) There were significant improvements in HRQoL during BP control and blood lipid-lowering therapies. The problems for all dimensions of the EQ-5D-3L descriptive system were slight at baseline and were well preserved in the follow-up period. The EQ VAS score and the EQ-5D-3L index increased over time, indicating better health status after the treatments. (2) There was no evidence of a difference in HRQoL between the two antihypertensive groups or the two lipid-lowering groups. (3) Patients who reached the BP/lipid treatment targets had better HRQoL than those who did not reach the treatment targets. Decreases in systolic/diastolic BP and LDL-C and increases in HDL-C were independently associated with increases in the EQ VAS score and the EQ-5D-3L index. In addition to the above three findings, we found no evidence of an interaction between BP control and blood lipid-lowering in determining the post-treatment HRQoL.
These findings confirmed our hypotheses that HRQoL would improve over time, be similar among interventions, but be different among BP/lipid-lowering effects. Notably, the evaluation of HRQoL was based on a group of people. Small changes in HRQoL might be statistically significant for populations but have little clinical importance for individuals [27]. We thus calculated the minimal clinically important difference (MCID) to appraise practical significance [28]. The MCID for the EQ VAS score and the EQ-5D-3L index were 6% and 3%, respectively [29, 30], indicating that the increases in HRQoL in our study seemed to be of less clinical importance. As the situations of the CHIEF participants were quite good at baseline, we could at least claim that the BP control and blood lipid-lowering therapies did not impair the patients’ health states, from a clinical point of view.
Generally, disease symptoms and physical/biochemical activities are the main tools to evaluate the effects of drug therapies. These tools, however, cannot reflect patients’ perception of HRQoL. Patients’ perceptions are largely responsible for whether they will adhere to and benefit from interventions [16, 31]. Therefore, it is essential to understand how treatments reduce symptoms and influence quality of life when conducting clinical trials. HRQoL instruments such as the Psychological General Well-Being Index [13, 15], the Subjective Symptoms Assessment Profile [13, 15], the Medical Outcomes Study Short Form-36 Questionnaire [14], and the EuroQol Health Utility Index [15] have been widely used in previous investigations. In our study, we chose another generic instrument, the EQ-5D measurement, for the following reasons. First, the EQ-5D form is short and easy to fill out, avoiding an unnecessary administrative burden for both interviewers and participants. Second, the EQ-5D questionnaire is validated in many countries and diverse populations [32, 33], showing acceptable stability and reliability in health state assessment. Finally, the EQ-5D products include both a descriptive system and a visual analog scale, which are convenient for the description and evaluation of patients’ health conditions.
The main finding of our study was in parallel with those of several investigations that demonstrated an improvement in HRQoL during antihypertensive treatments [12, 15]. Investigators claimed that drug interventions would considerably relieve symptoms, comfort patients’ anxiety, and improved their self-reported quality of life. Other studies, in contrast, have reported no or even adverse influences of BP-lowering therapies on HRQoL [10, 11]. Such controversy might be attributed to the difficulties in measuring and interpreting HRQoL. Since the assessment of HRQoL was relatively subjective, survey results on HRQoL were largely dependent on the interviewers’ expression and the participants’ understanding of the questions. The CHIEF study used centralized training and periodic inspections to avoid investigator biases [19], ensuring that the advances in HRQoL were real but not superficial.
We did not find a significant difference in HRQoL between the amlodipine + amiloride/hydrochlorothiazide group and the amlodipine + telmisartan group or between the simvastatin group and the standard management group. This might hint that it was not the specific type of therapy but the BP/lipid decline that was associated with the HRQoL improvements [34]. Some studies have shown that changes in HRQoL vary by antihypertensive treatment [12, 15]. A possible reason for the disagreement is that the sample size of the CHIEF study was not designed according to the HRQoL substudy. Therefore, the power might not be enough to detect the difference in HRQoL among groups.
We found better HRQoL in patients with controlled BP than in those with uncontrolled BP. Similar results are also confirmed by a multitude of studies [12,13,14,15]. Decreases in BP would reduce several clinical complaints and are thus correlated with improvements in HRQoL. Although some researchers have reported that HRQoL is worse in participants with controlled hypertension under drug treatments, the deterioration of HRQoL might not be attributed to the decreases in BP, but to the regular medications and the awareness of disease [35]. Another noteworthy issue that has received increasing attention is the effect of intensive (systolic BP < 120 mmHg) versus standard BP control strategies (systolic BP 130–139 mmHg) on HRQoL. Both the Systolic Blood Pressure Intervention (SPRINT) trial and the Action to Control Cardiovascular Risk in Diabetes (ACCORD) trial stated that HRQoL in the intensive BP control group was similar to that in the standard BP control group [36, 37], which implied that continued lowering of BP after reaching a certain level might not bring additional benefits to patients’ quality of life. Since our study only detected a linear relationship between HRQoL and systolic BP between 130 and 180 mmHg, whether this linearity still exists when systolic BP is lower than 130 mmHg (especially when systolic BP is controlled intensively versus standardly) in Chinese hypertensive patients needs to be investigated in future studies.
Previous studies have reported associations between lipid levels and HRQoL [38]. In our study, we only found that a decline in LDL-C (but no other lipid markers) was correlated with better HRQoL. Moreover, we observed less of a difference in HRQoL related to LDL-C than to BP levels. We speculated that, compared with hypertension, the symptoms of hyperlipidemia were not that conspicuous and did not have too much connection with the patients’ normal life during the study period. Therefore, the decrease in LDL-C might show less of an association with HRQoL. However, an increase in HDL-C showed a substantial correlation with the improvement of HRQoL. This finding suggests that lipid regulation rather than merely lipid lowering is more important for patients’ quality of life.
There is scant information on the joint effect of BP and lipid reduction on HRQoL. Our study found no evidence of an interaction between BP control and blood lipid-lowering. Antihypertensive and lipid-lowering combination therapies would not achieve additional benefits or bring additional risk to HRQoL.
Our study is the first large-scale, prospective, randomized controlled, open-labeled, blinded-endpoint evaluation clinical trial conducted in a Chinese hypertensive population to explore the changes in HRQoL during BP control and blood lipid-lowering therapies. We used a universally accepted tool for the assessment of quality of life, which is essential for demonstrating the overall trend. We found that HRQoL improved over time, and the improvements were associated with BP/lipid levels but not with specific interventions. There is no reason to withhold drug therapies in Chinese hypertensive patients in consideration of the medicines’ negative effects on quality of life.
There are several limitations of our study. First, we did not establish a placebo control arm in our study and thus could not separate the placebo effect from the real treatment effect on HRQoL [11, 12]. In other words, we could not attribute the improvements in HRQoL to the BP/lipid treatments. However, we could at least claim that BP control and blood lipid-lowering therapies did not impair patients’ quality of life and that these therapies should not be withheld in China. Second, we evaluated participants’ HRQoL with a follow-up period of up to 4 years. The short-term impact of antihypertensive and lipid-lowering therapies on quality of life can be appraised and used to guide medical decisions. However, the long-term impact as well as the clinical significance should be examined in further studies. Well-designed investigations for HRQoL with better quality control and lower loss rates in China are expected in the future.
In conclusion, the HRQoL of the CHIEF participants was generally good at baseline and was well preserved during BP control and blood lipid-lowering therapies. Improvements in HRQoL were not associated with intervention groups but with decreases in BP/LDL-C levels. Thus, antihypertensive treatments as well as lipid-lowering treatments should not be denied to Chinese patients to prevent drug harm to people’s quality of life. Moreover, the combination treatment of hypertension and hyperlipidemia will not bring additional risk to HRQoL.
References
Lim SS, Vos T, Flaxman AD, Danaei G, Shibuya K, Adair-Rohani H, et al. A comparative risk assessment of burden of disease and injury attributable to 67 risk factors and risk factor clusters in 21 regions, 1990–2010: a systematic analysis for the Global Burden of Disease Study 2010. Lancet. 2012;380:2224–60.
National Center for Cardiovascular Diseases. Report on cardiovascular disease in China. Beijing: Encyclopedia of China Publishing House; 2007.
Gu D, Reynolds K, Wu X, Chen J, Duan X, Muntner P, et al. Prevalence, awareness, treatment, and control of hypertension in China. Hypertension. 2002;40:920–7.
Wu Y, Huxley R, Li L, Anna V, Xie G, Yao C, et al. China NNHS Steering Committee; China NNHS Working Group. Prevalence, awareness, treatment, and control of hypertension in China: data from the China National Nutrition and Health Survey 2002. Circulation. 2008;118:2679–86.
Li W, Gu H, Teo KK, Bo J, Wang Y, Yang J, et al. PURE China Investigators. Hypertension prevalence, awareness, treatment, and control in 115 rural and urban communities involving 47 000 people from China. J Hypertens. 2016;34:39–46.
He J, Gu D, Reynolds K, Wu X, Muntner P, Zhao J, et al. InterASIA Collaborative Group. Serum total and lipoprotein cholesterol levels and awareness, treatment, and control of hypercholesterolemia in China. Circulation. 2004;110:405–11.
Yang W, Xiao J, Yang Z, Ji L, Jia W, Weng J, et al. China National Diabetes and Metabolic Disorders Study Investigators. Serum lipids and lipoproteins in Chinese men and women. Circulation. 2012;125:2212–21.
Liu M, Li Y, Liu S, Wang W, Zhou M. Burden on blood-pressure-related diseases among the Chinese population, in 2010. Zhonghua Liu Xing Bing Xue Za Zhi. 2014;35:680–3.
Liu M, Wang W, Ma L, Zhou M. Change on burden of diseases from hypercholesterolemia among the Chinese population from 1990 to 2010. Zhonghua Xin Xue Guan Bing Za Zhi 2015; 43: 802–5.
Van Hoof R, Amery A, Fagard R, Staessen J. Quality of life during treatment of hypertensive patients with diuretics. Acta Cardiol. 1990;45:393–401.
Applegate WB, Pressel S, Wittes J, Luhr J, Shekelle RB, Camel GH, et al. Impact of the treatment of isolated systolic hypertension on behavioral variables. Results from the systolic hypertension in the elderly program. Arch Intern Med. 1994;154:2154–60.
Grimm RH Jr., Grandits GA, Cutler JA, Stewart AL, McDonald RH, Svendsen K, et al. Relationships of quality-of-life measures to long-term lifestyle and drug treatment in the Treatment of Mild Hypertension Study. Arch Intern Med. 1997;157:638–48.
Wiklund I, Halling K, Ryden-Bergsten T, Fletcher A. Does lowering the blood pressure improve the mood? Quality-of-life results from the Hypertension Optimal Treatment (HOT) study. Blood Press. 1997;6:357–64.
Plaisted CS, Lin PH, Ard JD, McClure ML, Svetkey LP. The effects of dietary patterns on quality of life: a substudy of the Dietary Approaches to Stop Hypertension trial. J Am Diet Assoc. 1999;99:S84–9.
Degl’Innocenti A, Elmfeldt D, Hofman A, Lithell H, Olofsson B, Skoog I, et al. Health-related quality of life during treatment of elderly patients with hypertension: results from the Study on COgnition and Prognosis in the Elderly (SCOPE). J Hum Hypertens. 2004;18:239–45.
Testa MA, Simonson DC. Assessment of quality-of-life outcomes. N Engl J Med. 1996;334:835–40.
Liu L, Li M, Song S, Shi A, Cheng S, Dang X, et al. Effects of long-term psychological intervention on blood pressure and health-related quality of life in patients with hypertension among the Chinese working population. Hypertens Res. 2017;40:999–1007.
Zhou T, Guan H, Yao J, Xiong X, Ma A. The quality of life in Chinese population with chronic non-communicable diseases according to EQ-5D-3L: a systematic review. Qual Life Res. 2018;27:2799–814.
Wang W, Ma L, Zhang Y, Deng Q, Liu M, Liu L. The combination of amlodipine and angiotensin receptor blocker or diuretics in high-risk hypertensive patients: rationale, design and baseline characteristics. J Hum Hypertens. 2010;25:271–7.
Robinson JGFM, Krempf M, Bergeron J, Luc G, Averna M, Stroes ES, et al. TERM Investigators. Efficacy and safety of alirocumab in reducing lipids and cardiovascular events. N Engl J Med. 2015;372:1489–99.
EuroQol Group. EuroQol–a new facility for the measurement of health-related quality of life. Health Policy. 1990;16:199–208.
EuroQol Research Foundation. EQ-5D-3L User Guide: Basic information on how to use the EQ-5D-3L instrument. 2018. Available from: https://euroqol.org/wp-content/uploads/2018/12/EQ-5D-3L-User-Guide_version-6.0.pdf
Tsuchiya A, Ikeda S, Ikegami N, Nishimura S, Sakai I, Fukuda T, et al. Estimating an EQ-5D population value set: the case of Japan. Health Econ. 2002;11:341–53.
ICH Expert Working Group. ICH harmonised tripartite guideline: statistical principles for cllinical trials E9. 1998. Available from: https://www.ich.org/fileadmin/Public_Web_Site/ICH_Products/Guidelines/Efficacy/E9/Step4/E9_Guideline.pdf
Jennrich RI, Schluchter MD. Unbalanced repeated-measures models with structured covariance matrices. Biometrics. 1986;42:805–20.
Rubin DB. Multiple imputation for nonresponse in surveys. New York: John Wiley & Sons; 1987.
Guyatt GH, Juniper EF, Walter SD, Griffith LE, Goldstein RS. Interpreting treatment effects in randomised trials. Brit Med J. 1998;316:690–3.
Beaton DE, Boers M, Wells GA. Many faces of the minimal clinically important difference (MCID): a literature review and directions for future research. Curr Opin Rheuma. 2002;14:109–14.
Jaeschke R, Singer J, Guyatt GH. Measurement of health status. Ascertaining minimal Clin important Differ Control Clin Trials. 1989;10:407–15.
Norman GR, Sloan JA, Wyrwich KW. Interpretation of changes in health-related quality of life: the remarkable universality of half a standard deviation. Med Care. 2003;41:582–92.
Falk M. Compliance with treatment and the art of medicine. Am J Cardiol. 2001;88:668–9.
Greiner W, Weijnen T, Nieuwenhuizen M, Oppe S, Badia X, Busschbach J, et al. A single European currency for EQ-5D health states. Results from a six-country study. Eur J Health Econ. 2003;4:222–31.
Johnson JA, Coons SJ, Ergo A, Szava-Kovats G. Valuation of EuroQOL (EQ-5D) health states in an adult US sample. Pharmacoeconomics. 1998;13:421–33.
Vanmolkot FH, de Hoon JN, van de Ven LL, Van Bortel LM. Impact of antihypertensive treatment on quality of life: comparison between bisoprolol and bendrofluazide. J Hum Hypertens. 1999;13:559–63.
Trevisol DJ, Moreira LB, Fuchs FD, Fuchs SC. Health-related quality of life is worse in individuals with hypertension under drug treatment: results of population-based study. J Hum Hypertens. 2012;26:374–80.
O’Connor PJ, Narayan KM, Anderson R, Feeney P, Fine L, Ali MK, et al. Effect of intensive versus standard blood pressure control on depression and health-related quality of life in type 2 diabetes: the ACCORD trial. Diabetes Care. 2012;35:1479–81.
Berlowitz DR, Foy CG, Kazis LE, Bolin LP, Conroy MB, Fitzpatrick P, et al. SPRINT research group. Effect of intensive blood-pressure treatment on patient-reported outcomes. N Engl J Med. 2017;377:733–44.
Lasaite L, Lasiene J, Kazanavicius G, Gostautas A. Associations of emotional state and quality of life with lipid concentration, duration of the disease, and the way of treating the disease in persons with type 2 diabetes mellitus. Med (Kaunas). 2009;45:85–94.
Acknowledgements
The Ministry of Sciences and Technology of China has awarded a grant to assist in conducting the CHIEF study. We would like to express our gratitude to the doctors and patients participating in the CHIEF study. We thank Dr. Dong Zhang for his important intellectual revisions to this work.
Author information
Authors and Affiliations
Consortia
Corresponding author
Ethics declarations
Conflict of interest
The authors declare that they have no conflict of interest.
Additional information
Publisher’s note: Springer Nature remains neutral with regard to jurisdictional claims in published maps and institutional affiliations.
The Ministry of Sciences and Technology of China has awarded a grant for this study.
Supplementary Information
Rights and permissions
About this article
Cite this article
Yan, R., Gu, HQ., Wang, W. et al. Health-related quality of life in blood pressure control and blood lipid-lowering therapies: results from the CHIEF randomized controlled trial. Hypertens Res 42, 1561–1571 (2019). https://doi.org/10.1038/s41440-019-0281-z
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/s41440-019-0281-z
Keywords
This article is cited by
-
The Impact of Risk Factor Control on Health-Related Quality of Life in Individuals with High Cardiovascular Disease Risk: A Cross-sectional Study Based on EQ-5D Utility Scores in Inner Mongolia, China
Journal of Epidemiology and Global Health (2022)
-
The impact of antihypertensive treatment initiation on health-related quality of life and cardiovascular risk factor levels: a prospective, interventional study
BMC Cardiovascular Disorders (2021)
-
The association of quality of life and personality characteristics with adolescent metabolic syndrome: a cohort study
Health and Quality of Life Outcomes (2021)
-
Variables associated with poor health-related quality of life among patients with dyslipidemia in Jordan
Quality of Life Research (2021)